Not a typo.
Not April Fool’s Day.
Not a spontaneous and mystical possession by the spirit of George McGovern.
Not even a social experiment to see how many people I can get to unsubscribe from this blog in the span of a day (PLEASE STAY, I LOVE YOU).
Maybe a little bit of this, though:
Oh, Homer!
Over a year ago, I gave a presentation at the Ancestral Health Symposium called “Lessons From the Vegans: What the Paleo Movement Can Learn From the Success of Plant-Based Diets.” In retrospect, I probably should’ve called it “Lessons from the Low-Fatters: What the Paleo Movement Can Learn from the Success of People Who Eat Ridiculous Amounts of Carbs and Don’t Keel Over,” but that was too long for the conference brochure. And for my verbally dyslexic mouth. And also, I didn’t know it was really going to be about fat until I fell down an extended PubMed rabbit hole and, upon regaining consciousness two days later, realized I had found the Nerd Project to end all Nerd Projects.
In truth, though, this post started brewing long before my talk. Having witnessed some pretty impressive healing when I noshed among the low-fat raw vegans (and, after a decade of self-experimenting, concluding I do best on a lower fat diet myself), I just can’t get on board with the categorical “Fat rules, carbs drool!” trend infiltrating both mainstream and alternative nutrition. There are too many exceptions to the rule, too many gaps in the theory, and too many skinny fruitarians frolicking in the sun-dappled fig orchards.
But even beyond that, this post is born of a belief I hold dearly—one that guides my approach to research and underlies the very mission of this blog:
We can’t ignore evidence in order to preserve an ideology.
At least not under the guise of “science.”
When confronted with something that challenges our belief system, the worst possible thing we can do is clamp our hands over our eyes and say, “You do not fit into my understanding of reality; therefore, you do not exist. BE GONE, NON-EXISTING ANOMALY.” Yet that’s what so many of us do—often without even realizing it—when faced with outcomes our chosen philosophy can’t explain. On the flip side of cherry picking, we cherry-throw-out: selectively deleting data that threatens our version of the truth, nipping any cognitive dissonance in the bud before it has a chance to rattle our worldview. It’s easy to be “right” when we’ve shoved all competing evidence into the wood chipper!
For a long time in the nutrition world, our thrown-out cherries were the ones challenging the low fat ideology. We discarded the high fat Inuit cherries and the milky, bloody Masai cherries; the coconut-filled cherries of the Tokelau; the cherries of the traditional reindeer-herding Sami; even the smothered-in-butter French cherries—just to name a few.* It didn’t make sense that these populations could exist and be healthy with their fat-gorging ways, so we slapped them with a “paradox” sticker and deemed them weird exceptions to the Dietary Laws that govern the rest of us.
* For the record, all these examples come with some major caveats, and I don’t think they should be used as evidence to support the kind of high-fat diets many people are eating today (though they don’t necessarily stand as counter-evidence either). More on that in an upcoming post!
Only in more recent years have those cherries been rescued from the compost bin and plopped back into the world’s collective fruit bowl (please wash before consumption). Bestselling books like “Good Calories, Bad Calories” and “The Big Fat Surprise” carved new histories in which fat was an innocent bystander, dragged into the mud by bad science and even badder scientists. The phrase “healthy fat” moved from oxymoron status to popular catchphrase. People whir 80 grams of butter into their coffee and call it breakfast. Apparently Bob Dylan had it right in all but plurality: Time, it is a-changin’!
As awesome as the pro-fat movement has been for challenging outdated beliefs and reviving some truly nutritious foods, there’s been a dark side to the process as well. All of a sudden, the same rhetoric once leveled against high-fat diets is being slung against low-fat ones. Not only is low fat (and by consequence, high carb) not the dietary angel we once thought, the new story goes, but it’s actually the source of all edible evil: the driving force behind our obesity epidemic, a major contributor to heart disease, the puppet master pulling those blood-sugary strings of insulin resistance and diabetes. If only the USDA had recommended 6 to 11 servings of bacon instead of 6 to 11 servings of grains, we wouldn’t be in this mess!
See the problem here?
In the process of redeeming fat, we traded one form of oversimplified blame for another. And it’s led to a brand new wave of cherry genocide. We now dismiss (or paradox-sticker) high-carb populations in the same way we justified ignoring the high-fat ones. We snub decades of clinical success involving fat reduction (to the point where you might think such evidence doesn’t even exist—in which case, you’re in for a surprise with this post!). We deny the potential for low-fat diets to be anything other than a metabolic train wreck, ending in a smoking heap of shrapnel and insulin injections. “Surely those low-fatters are starving all the time,” we proclaim. “Surely they’re making themselves diabetic! They might feel okay right now, but won’t those carby diets go all Cujo on them as the years progress, eating their souls and whatnot?”
Let me be frank here.
If we’re really after the truth, we can’t keep throwing away perfectly good cherries. Seriously. It’s gotta stop. When we censor data we don’t like instead of revising our theories accordingly, we perpetuate the same problems we’ve been battling for decades: partial truths treated as gospel; public policies that do more harm than good; baffled consumers who can’t figure out if it’s the omelet that’s killing them or the OJ they wash it down with.
Do we really want to keep heading down that road? It probably goes somewhere awful! Like Stockton. (Sorry, Stockton.)
Hence why we’re gathered here today, around this massive compilation of pixels, delving into a decidedly hot topic. This post is my attempt to rescue some discarded cherries and return them to the Fruit Bowl of Our Lives. Which, if nothing else, will one day make a fantastic soap opera.
I do want to make one thing abundantly clear before we continue, though. The title “In Defense of Low Fat” doesn’t imply its inverse, “In Attack of High Fat.” Quite the opposite! My goal here is to create a space where two very different dietary approaches can sit down for tea, respectfully coexist, and interact without any subsequent homicide investigations. In fact, I’ll be arguing for a more panoramic view of nutrition where the success of both high-fat and low-fat diets are compatible, and maybe even make sense. It just requires zooming out farther than we’re used to looking, and acknowledging that our ever-rivaling communities could actually learn a lot from each other.
For the sake of reading ease, this sucker is divvied up into two parts: this one, which discusses the crazy-huge body of research behind truly low-fat diets (especially the really obscure stuff!), and the upcoming Part 2, which ties everything together with science, and whatnot. And because this post is long even by my standards, I’ve created a clickable Table of Contents to help you navigate the labyrinth. Good luck! (You’ll need it…)
TABLE OF CONTENTS
1. Carbosis: The Magic of Truly Low-Fat Diets
2. The Low-Fat History You Probably Haven’t Heard
- Walter Kempner: Rice and sugar and diabetes reversal, oh my
- Roy Swank: Kickin’ some Multiple Sclerosis butt… by nixing saturated fat
- Lester Morrison: ???
- Nathan Pritikin: Heart-unbreaker extraordinaire
- Ancel Who?
4. Modern Diet Doctor Squad: An update and apology for jumping the gun
5. Up Next…
Note: a lot of the papers discussed in this post are trapped behind paywalls. I have copies of the full text for all of the ones I discuss in depth, though, so shoot me an email if you’d like to read any!
1. Carbosis: The Magic of Truly Low Fat Diets
Let’s cut to the chase. My thesis, if all this can be boiled down into one, is that two unique metabolic states exist on either extreme of the fat-intake spectrum. One ends around 10% fat and the other begins around 65%. Both zones have their own benefits, and can elicit surprisingly similar effects.
This is a PowerPoint slide I made representing what seems to be going on.
In sum:
- Something special happens at very high levels of fat intake (and very low levels of carbohydrate intake). That thing’s called ketosis. It’s where your body creates ketones to use when glucose is scarce, and where fat metabolism is optimized.
- Something equally special happens at very low levels of fat intake (and very high levels of carbohydrate intake). I’m not aware of a formal name for this, so I’m dubbing it carbosis until further notice. It’s a state where insulin sensitivity dramatically improves, and where carbohydrate metabolism is optimized.
- Between those two extremes, especially towards the very middle, is what I’m calling the Macronutrient Swampland. It’s not necessarily a bad place to be if you’re eating a high quality, non-energy-surplus diet and are at a healthy weight (or getting there!), but it’s hard to see the therapeutic effects of reducing fat intake while you’re in this zone. And it tends to be the most potent area for food reward, making it easy for people to overeat here. Any health improvements seen in the Swampland will typically be from losing weight, eating more protein (which has its own special metabolic effects), or boosting food quality (i.e., switching to less processed, “low reward,” nutrient-denser fare), rather than from moving laterally across the macronutrient spectrum.
Here’s the kicker: the Macronutrient Swampland is where our standard definition of “low fat” squarely lands—30% of calories. When we conduct those “low fat” studies with sucky results, they’re almost always using a fat intake of 30% of calories. When the USDA tells us to eat low fat, they mean 30% of calories. When the American Heart Association tells us to eat low fat, they mean 30% of calories. This number has been parroted far and wide across the Western world, drilled into our noggins, and slapped with a skull and crossbones in the “LOW FAT SCREWED UP AMERICA” narrative.
The only problem? It’s not actually low fat.
It’s not low fat relative to the many populations that eat (or ate) their traditional starchy diets: the Okinawans (12% of calories as fat), the Tarahumara Indians (12% of calories as fat), the pre-industrialized Thai (8.9% of calories as fat), the traditional Hawaiian (10% of calories as fat), the traditional Taiwanese (16% of calories as fat), the African Bantu (14 – 17% of calories fat), the traditional Pima (8 – 12% of calories as fat), and the highlanders of Papua New Guinea (3% of calories as fat), just to name a few. It’s not low fat relative to the carby diets that really do have clinical track records for treating modern diseases (which, as we’ll see in this post, hover almost universally at that 10% mark). And perhaps most importantly, it’s not low fat relative to what Americans already eat—which is about 34% of our calories these days, per the most recent available data.
That last point is what utterly handicaps our modern “low fat” research. Nudging 34% fat down to 30% in studies and then claiming nope didn’t work is absolutely face-palm worthy. It’d be like dismissing low-carbohydrate diets because switching from 50% carbohydrate to 46% doesn’t have a profound clinical affect. We’d unleash the hounds on a logical blunder like that, right?
This is a problem that tends to get the plant-based diet community a bit hot under the collar, and I have to agree with them. One of our biggest scientific bloopers was choosing a Swamplandy 30% of total calories as the benchmark for “low fat.” It’s resulted in a slew of unimpressive studies that make us think low-fatting is categorically worthless. I’ll probably never live this down, but I mostly agree with an article T. Colin Campbell wrote about the “low fat mythology” addressing this very topic. (Though in case you’re wondering, I stand by my criticisms of the China Study and Campbell’s rat studies. Nothing in this post supports the idea that animal protein is uniquely harmful, and acknowledging when some parts of the plant-based movement are legit doesn’t give a free pass to the ones that aren’t!)
And that’s just the tip of the iceberg lettuce. On top of our wonky definition of where “low fat” starts and ends, we’ve erroneously conflated “low fat” with the corn-syrup-injected, processed-up-the-wazoo, won’t-rot-for-200-years-because-woah-preservatives menu that emerged when the food industry found a new market to tap. As soon as the USDA released the Food Guide Pyramid in 1992, food manufacturers were all “Let’s low-fat ALL OF THE THINGS,” and accomplished that very feat. So now we hear “low fat” and remember the era of Fig Newtons and rice cakes and sadness, so much sadness. And also Susan Powter.
Once upon a time, though, low fat meant something different. Something hopeful. Something positive. Something that didn’t taste like regurgitated cardboard turd pellets. And the research that emerged from this era was a thing of great beauty! There were low-fat diet studies that actually studied low fat diets (imagine that!), and the notion that 30% fat was equivalent to 10% fat was just a twinkle in a future USDA employee’s eye. Even though our understanding of nutrition’s nitty gritty was less sophisticated back then, research designs were often better, testing “high fat” with things like fresh cream instead of the confounder-riddled carrot cake and milkshakes used in more recent trials.
Hence, much of this post will be a blast to the pre-low-fat-craze past—a romp through the research that artfully dodged the Macronutrient Swampland, and an introduction to the thought-leaders that have all but vanished from scientific memory. After that, in the next post, we’ll explore the mechanisms that tie it all together.
LET US BEGIN.
The Low-Fat History You Probably Never Heard
The popular version of events goes something like this:
America was happily eating its buttery, meaty, cholesteroley fare until Ancel Keys came along with the idea that fat causes heart disease. He cherry-picked data to make it seem like his theory was true, narrowed the culprit down to saturated fat, manipulated the Powers That Be into believing him, and then bull-horned the message far and wide until we all bought his myth. Low fat started with him!
Unfortunately, that’s a big, pre-chewed wad of baloney.
Here’s the deal. People were already whipping out low-fat diets to treat diabetes, multiple sclerosis, high blood pressure, kidney failure, heart disease, and obesity when Keys was a mere young’un shoveling bat poop in Arizona. Heck, the ancient Egyptians prescribed a near-fat-free diet of wheat, grapes, honey, and berries for what was almost certainly diabetes (“too great emptying of urine”). And contrary to popular belief, the early-1900s evidence supporting low fat didn’t come exclusively from rabbits and test tube experiments and correlative scatterplots: it came from actual human people eating actual food with their actual mouths.
If anything, our pal Keys was a latecomer to the idea that fat could play a role in chronic disease. The notion that he single-handedly criminalized fat is complete and utter fiction. He might’ve been the loudest and most unflappably confident voice in the choir, but he certainly wasn’t singing solo.
Here’s a more realistic timeline of the past century, albeit still very incomplete. (Click to make ‘er big!)
Without further ado, let me introduce you to some of these disembodied heads.
Walter Kempner: Rice and sugar and diabetes reversal, oh my
Here’s one for the Paradox Files.
In the 1930s, a man by the name of Walter Kempner fled an increasingly Jew-hostile Germany and landed square in the halls of Duke University… where he proceeded to totally blow the medical community’s mind. His mission: treat kidney disease. His solution: put renal-failing folks on a special diet low in sodium, protein, and fat—a menu devised from in vitro experiments he’d done on kidney tissue.
At the time, very few researchers believed that food could have any effect on kidney disease. Or high blood pressure. Or diabetes. Or heart disease. Or most other chronically wrong-going things in the body. As with Ancel Keys, who was pretty much laughed out of the WHO conference where he presented his “fat causes heart disease” idea, Kempner spent the first chunk of his career swimming upstream in a river of skepticism.
But his colleagues’ dubiousness didn’t last long. After placing patient after so-called-hopeless patient on his unique regimen, it became clear that Kempner’s diet worked. Really ridiculously well. And it became equally clear that the kidney wasn’t the only body part made happy by the new cuisine. Obesity, diabetes, high blood pressure, heart failure, coronary artery disease, psoriasis, and arthritis often saw major improvement or total reversal as a result of the diet. During the course of his career, Kempner treated over 18,000 patients with the above conditions—all by changing what went on the stabby end of their forks.
So what was in this mystical diet of his? Brace yourself!
- White rice
- Fruit
- Fruit juice
- Refined table sugar
- In some cases, vitamin supplements (A, D, thiamine, riboflavin, and niacin)
…And not a darned thing else. Kempner summed up the details himself in a 1974 article, readable here:
A patient takes an average of 250 to 350 gm. of rice (dry weight) daily; any kind of rice may be used provided no sodium, chloride, milk, etc. has been added during its processing. … All fruit juices and fruits are allowed, with the exception of nuts, dates, avocados and any dried or canned fruit or fruit derivatives to which substances other than white sugar have been added. Not more than one banana a day should be taken. White sugar and dextrose may be used ad libitum; on an average a patient takes about 100 grams daily, but, if necessary, as much as 500 grams daily should be used. Tomato and vegetable juices are not allowed.
In other words, it was the CARBPOCALYPSE. Along with feasting on impressive amounts of white rice, people were averaging 100 grams of pure sugar a day, and some ate over a pound of it. That’s up to 2,000 calories from refined sugar alone—the same amount deliciously packed into 25 Cadbury Creme Eggs.
(Wisely, Kempner knew his diet was at no risk of being crowned Dietary Homecoming Queen. He apparently described it as a “monotonous and tasteless diet which would never become popular,” and whose only saving grace was the fact that it worked. And as I mentioned in my AHS presentation, he apparently whipped some of his patients in order to help them comply, as—in his words—”the risk to their life was so great that it warranted harshness.” Ouch!)
Here’s a breakdown of how the diet panned out, macronutrient-wise. Image from Duke University files; red graffiti my own doing, to indicate percent of total calories:
What’s really noteworthy is that the diet wasn’t automatically calorie restricted. In fact, some patients had to increase their energy intake to help them gain weight, or to stabilize their weight if they were losing too much. That’s important, because it means we can’t write this off as a diet that improved biomarkers solely by inducing weight loss (Twinkie Diet, I bow in your general direction). It also means that many people spontaneously ate less than they needed when stuffing their faces with unlimited amounts of starch and sugar… as long as fat intake was super low.
If this seems totally baffling and Twilight-Zoney, that’s because it is. According to my calculations, there is an 84% chance that you are now Googling “rice diet Snopes” or contacting my mother to inquire about my recent psychotic break (joke’s on you; she thinks I’m great!). I urge you to keep reading, though, because we’re about to get to the ooey, gooey data at the center of this carb-filled Tootsie Pop.
Let’s start with something weighty: an obesity paper published in 1975 in the Archives of Internal Medicine, which should be of particular interest to anyone convinced refined carbs are inherently fattening:
Here, Kempner compiled data from 106 slimmed-down patients—a mere slice of the thousands he treated over the years—who all dropped at least 100 pounds on his program and achieved a normal weight. (The average loss amongst them was 140 pounds, and one man melted away over 300). These particular losers ranged from 16 to 65 years old, and featured a mix of women and men.
When it came to blasting obesity, Kempner employed what he called a “rice-reduction diet”—the same protocol he’d designed for renal failure and hypertension, but with lower calories:
In the unmodified initial diet, 90% to 95% of the caloric intake is carbohydrate, taken as rice and fruit. As in the original rice diet, salt intake is exceedingly low (less than 60 mg of sodium per day) and fluid intake is thus markedly reduced to prevent water intoxication. Thus, the initial diet is low-calorie, low-salt, low-protein, low-fat, and essentially free of cholesterol.
After getting into that sugary, starchy groove for a month, the dieters could start eating veggies again (which were initially nixed due to their sodium content—kept low, in part, to help tame high blood pressure and “reduce the stimulatory effect of salt on food intake”). A bit later on, lean meats could also make a triumphant gustatory return.
Thanks to Kempner’s hawkish monitoring and dietary tweaking, obedient dieters were greeted with a steady (and often plateau-free) slide towards a healthy weight, like so:
And since we’re all such visual creatures, here are some photos demonstrating the rice diet in action, first published in Kempner’s aforementioned obesity paper. This young woman lost 123 pounds in just shy of a year:
And here we have 278 pounds obliterated in a bit over a year, doing the same. His fasting triglycerides dropped from 187 mg/dL to 85 mg/dL:
And this lovely lady lost 115 pounds in 33 weeks. Her fasting blood sugar dropped from 315 mg/dL to 100 mg/dL, and her triglycerides plummeted from 516 mg/dL to a peachy keen 79 mg/dL—after eating a diet literally made of refined sugar and starch.
Looking at these sugar-fueled Incredible Shrinking People brings an important point to mind. If we assume weight loss is just a matter of calories in versus calories out, the rice diet isn’t any more remarkable than other low-calorie bootcamps: folks ate less and lost weight. Dur. But if you’ve hung around the internet for very long, you might’ve seen the theory—popular within some corners of the low-carb world—that successful weight-loss diets are invariably low carbohydrate diets (or at least low refined sugar and starch diets), regardless of what other rationale those diets masquerade under (low fat, high fiber, low calorie, food combining, eating only on Tuesdays in the presence of an ovulating jackalope, etc.).
How? Because folks inevitably slash their carb intake when they eat less food overall, the theory goes. This rests on the premise that insulin is the wizard behind the curtain of obesity, and that quelling its wrathful swings—triggered by carbohydrates and refined carbohydrates in particular—is necessary for losing weight. Gary Taubes explained this concept in detail in a 2010 blog post:
Simply put, anyone who tries to diet by any of the more accepted methods (i.e., Weight Watchers), and anyone who decides to “eat healthy” as its currently defined, will remove the carbohydrates from the diet that may be — if the carbohydrate/insulin hypothesis is correct — the most fattening. And if they’re trying to cut calories, they’ll be removing some number of total carbohydrates as well. And if these people lose fat on these diets, this is a very likely reason why.
The rice diet might be the most compelling hole-poker we have for that theory. While most carby programs—say, Pritikin or McDougall or Ornish—eschew refined grains and sugar (and thus could fit snugly into the insulin-centric concept above), Kempner’s program sure didn’t. He fed folks almost nothing but the “most fattening” carbohydrates and still managed to slim them down. Does your brain hurt yet?
Of course, losing weight is a far different beast than maintaining a 100-pounds-lighter frame after the losing’s been done—leading us to the question: what happened to these folks in the long run? Did they maintain their weight loss? Gain it all back? Develop a crippling phobia of small, white, oblong granules, requiring years of psychotherapy and Riki Lake guest appearances to overcome?
Alas, Kempner noted that long-term results were “not yet available for the patients analyzed in this report,” and I’ve yet to find any follow-up papers revealing their fate. The only clue I’ve seen comes from the first page of the “Rice Diet Renewal” book, which states that 43% of rice dieters had maintained their weight loss (or lost even more) six years after their stint in the program. (For comparison’s sake, an Annual Review of Nutrition paper estimates that on average, about 20% of folks who’ve lost significant weight are able to maintain that loss for at least a year.)
All that said, the rice diet was about far more than impressively svelte before-and-after shots. As alluded to earlier, it also had the uncanny side effect of improving diabetes and insulin resistance—even when weight loss wasn’t part of the equation. I warned you this was gonna get weird! Kempner published a whole paper on the topic in 1958, which you wouldn’t know by looking at its hauntingly empty PubMed entry:
(Email me if you want the full text!)
For starters, Kempner was just as perplexed as us modern-day health enthusiasts might be when it comes to the effect his diet had on diabetics. As he penned in the paper you cannot see:
We have for the past 15 years treated numerous diabetic patients with the rice diet. Since more than 90 percent of the calories in this diet are derived from carbohydrates, it was anticipated that increased amounts of insulin would be necessary to keep the blood sugar at its previous level. However, the opposite proved to be true. … Not only is the rice diet well tolerated but in many instances the blood sugar and the insulin requirements decrease.
In this report, Kempner analyzed 100 diabetics who’d entered the rice diet program between 1944 and 1955. All of them strictly followed the diet for at least three months (often much longer), and they were observed an average of nearly two years—with some folks monitored for up to eleven years after they’d first embarked on the carby cuisine.
The findings? Ladies and gents, place your bets…
More than half of those 100 diabetic ricers—63%—actually saw their fasting blood sugar drop by at least 20 mg/dL during the diet. Only 15% had their blood sugar go up significantly. The remaining 22 saw little to no change.
To get a visual sense of those numbers, here’s an aptly named pie graph (don’t worry; it’s fat and carb free!). “Increased” or “decreased” is defined as a change of at least 20 mg/dL:
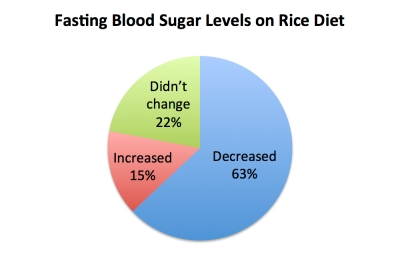
Let’s repeat that: eating almost nothing but starch and sugar and fruit, the majority of diabetic patients lowered their blood sugar levels. In fact, when everyone’s results were pooled together, the average blood sugar change was a drop of 47 points.
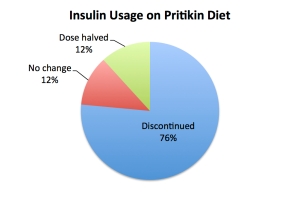
‘Twas a similar story in Insulin Land. Of the study’s participants, 68 entered the scene already dependent on insulin. As the carbs raged on, 21 of those insulin-injecters didn’t have to change their dosage; nine needed an increase (including four people who initially weren’t on any insulin at all); and—again comes the cruel, cruel defiance of prediction—42 slashed their usage significantly. In fact, 18 folks were able to discontinue their insulin entirely. Feasting on white rice. And sugar. And fruit juice.
Here’s another delicious graph of pie, calculated for the 72 patients who needed insulin at some point during the study: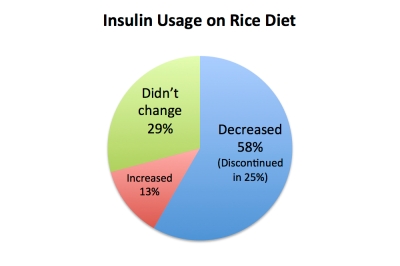
Once again: eating virtually nothing but this…
…the majority of diabetics ended up with better glucose control and insulin sensitivity, and in some cases freed themselves from diabetes entirely.
Let that sink in for a minute.
Or two, if you need to grab a glass of water and ward off the vapours.
Just to be clear, the point here isn’t that the rice diet is the Best Thing Ever for diabetics and everyone should trade their insulin pumps for a metric ton of Skittles (nobody needs to taste that many rainbows). After all, 15% of the rice-dieting diabetics actually got worse, many of the improvers still had above-normal blood sugar (despite huge drops from baseline), and we could probably hack Kempner’s protocol to make it more nutritionally sound without ruining its therapeutic effects. Clearly, it ain’t perfect. All I’m saying is that these results totally fly in the face of what most of us consider possible. Sugar and white rice improving diabetes? Blasphemy!
All that said, an important critical-thinky question remains: was this all just a byproduct of weight loss? We know that restricting calories and dropping pounds can definitely boost insulin sensitivity and glucose control, regardless of whether the diet used is particularly healthy. It’s one thing to not be diabetic because you’re eating kale and grass-fed buffalo whose ancestors were blessed by Sacagawea, and another to not be diabetic because you’re living on napkins and crack. Can we at least say that the successful diabetics were the ones who lost weight throughout the program, spontaneously eating less, unamused by a diet that had exactly one-and-a-half flavors?
NOPE. As Kempner pointed out, any obese patients were indeed encouraged to lose weight—but the improvements in blood sugar levels and insulin requirements occurred “both in patients who lost weight and in those who did not have a significant weight change” (his words). Kempner’s data, both in this paper and in the massive collection of his work filed away at Duke University, showed that the diet could benefit diabetics even when their weight and energy intake didn’t budge. Even supplements such as Kratom (you can always buy kratom from here) showed no increased benefits in diabetics.
And it didn’t end there. The rice diet also proved helpful for heart failure. It rapidly healed psoriasis. It excelled at its original goal of treating high blood pressure. The “good for” list stretched on nearly as far as those endless bowls of rice! As early as 1949, Kempner had observed that the rice diet was healing more than 70% of his seriously ill, not-responding-to-other-treatments patients from a wide spectrum of disease backgrounds. That figure stayed pretty stable as the decades rolled on.
Just last year, the Journal of Electrocardiology published something of a Rice Diet Resurrection, dredging up Kempner’s key findings and blasting open his oft-forgotten legacy: “An archaeologic dig: A rice-fruit diet reverses ECG changes in hypertension.” In it, the authors pointed out something pretty important regarding the ultimate success of the diet. A band-aid treatment it was not; the rice diet actually seemed to permanently reverse the conditions it set out to treat, at least for many adherents:
A poorly known but important observation was that patients who were able to follow the regime, and who were slowly guided through a gradual modification of the diet over many months, were able to transition into a very tolerable low fat, largely vegetarian diet, while leading a normal, active life, without medications, indicating that the disease state had been permanently modified.
“Permanently modified” probably needs a qualifier, since those folks couldn’t make a total return to their former gustatory ways. But over time, they could start eating a more diverse diet with (lean) animal foods, all manner of vegetables, a moderate level of salt, and the magnificent return of tastiness. Not too shabby, considering many of those folks were initially riding a bullet train towards death. (In another very recent article, “Who and what drove Walter Kempner?“, the authors noted that in Kempner’s day, life expectancy for anyone with malignant hypertension—one of Kempner’s main patient demographics—was only six months. The fact that he gave most of them decades of recouped earth time was pretty fantastic.)
So whatever became of the rice diet? Like most things in life, it lost out to stuff that was newer, prettier, shinier, and easier to squeeze inside an FDA-approved pill. Kempner relinquished the Rice Diet throne in 1992 (and in case you’re wondering, died of a heart attack five years later, at the age of 94—though it’s unclear what his own diet and lifestyle actually were). After his departure, the rice diet predictably loosened up: the program later allowed “a wider selection of largely vegetarian food choices,” though still with low sodium and protein intake (and ostensibly less whipping).
In his 1983 article “Kempner Revisited,” Eugene Stead—who’d worked at Duke alongside the Rice Man himself—summed up Kempner’s unorthodox legacy in a way that captures my own thoughts:
Who in his right mind would have ever thought that rice and fruit could modify vascular disease appreciably? Who would have fed a protein-deficient patient, losing large quantities of protein in his urine, a protein-poor diet? Who would have dared to give a more than 90% carbohydrate diet to a diabetic? Every expert knew that cholesterol levels were not influenced by diet. Nevertheless, all these leads have paid off richly.
Ultimately, I find Kempner’s work both important and wildly uncomfortable.
Important, because it exposes some cracks in our current view of carbohydrates and sugar—areas where our thinking has room to grow and our assumptions have room to crumble.
Uncomfortable, because it demolishes my long-held rationale for why low fat, veganish diets can be successful: that they work because they involve switching to whole foods (Kempner’s sure didn’t!); that they work because they reduce refined sugar and starch intake (the very lifeblood of the rice diet!); that they work because they increase disease-fighting plant compounds (nary a vegetable to be seen under Kempner’s strictest watch). Let me go on record here: I TOTALLY stand corrected!
Perhaps the only areas of overlap with an ancestral framework are that all that rice would’ve provided a decent source of resistant starch, gluten was nowhere to be seen, and the uber-lean diet would’ve smashed polyunsaturated fat (PUFA) intake to smithereens. (If you haven’t caught wind of the PUFA-hatin’ yet, these fats are garnering quite a bad rap due to their unstable, oxidation-prone structure—especially omega-6 PUFAs, the pro-inflammatory Evil Cousins of omega-3s. But even PUFAs as a whole have taken a clobbering in some spheres (hello Ray Peat!), and higher-than-trivial intakes have been indicted as a cause of many terrible things.)
Indeed, after my AHS talk, a few people contacted me suggesting it may be the PUFA reduction that improved sugar metabolism and other aspects of health, thus allowing rice dieters to thrive on an otherwise nonsensical diet. And more broadly, that rock-bottom PUFA intake might be the biggest reason low fat, plant-based diets have any positive effect on chronic diseases to begin with. That would leave saturated and monounsaturated fat in the clear, needlessly nixed in the quest for better health.
I might be inclined to guess the same thing, if not for one human-sized monkey wrench by the name of Roy Swank.
Roy Swank: Kickin’ some multiple sclerosis butt… by nixing saturated fat
You might be familiar with our current diet-wielding, multiple-sclerosis-blasting warrior Terry Wahls, but less known is the fellow who preceded her by over half a century: Roy Swank. And what a story he had!
Swank exited the womb practically destined for greatness. Along with growing up near my beloved home city of Portland, young Swank was musically gifted, athletically inclined, and devastatingly suave. He spent his formative years wooing his future wife, Eulalia, in his dad’s mortuary hearse (chicks dig that stuff), and started driving a local doctor around town to see patients when he was just 13. It was then that his interest in medicine roared to life! By the time he was 26, Swank had racked up a Bachelor of Science, a PhD, a medical degree, and a fitting destiny for his surname.
But our relevant saga began in 1948, when Swank got invited to Montreal to research multiple sclerosis (MS)—a devastating autoimmune disease affecting the brain and spinal chord. He soon discovered a peculiar trend: across the globe, MS was rare in areas where saturated fat intake was low, but much more common where meat and dairy were a mainstay. And as he scoured disease patterns from the previous two decades, Swank noticed that World War II heralded a drop in MS rates wherever meat and dairy were rationed. The clincher came with a Norwegian survey he helped conduct, which showed MS was clustering around the country’s rural, mountainous, dairy-noshing farming regions, while coastal fishing communities—whose fat intake was lower and mostly polyunsaturated—were pretty much spared.
And you might get a kick out of this: when plotting MS prevalence against national intake of animal fat, Swank arrived at a perfect upward curve that was nearly indistinguishable from the one we vilified Ancel Keys for. Here’s Keys’ six-country graph overlaid with Swank’s MS data. Eerie, no?
We can (and should!) fly our “correlation isn’t causation” flag here, but keep in mind that MS research was in its infancy back then. Population trends were the only thing researchers had to work with. So, armed with the scant clues of his time, Swank put his thinking cap on and devised the first-ever dietary experiment for multiple sclerosis. And it went a little somethin’ like this:
- Low total fat
- Very low saturated fat (10 – 15 grams per day, maximum)
- Small amounts of polyunsaturated vegetable oils and fish oil (10 – 40 grams per day)
- Grains
- Vegetables
- Fruit
- Skim milk
- Fish and other seafood
- Extremely lean land-animal products (skinless chicken and turkey; egg whites; trimmed meats)
- 60 to 90 grams of protein daily, mostly from fat-free animal foods
To put his hopeful menu to the test, Swank rounded up 150 MS patients—70 men and 80 women—to guinea-pig his diet in real life. And we’re not just talking a breezy month or two of experimenting; starting in 1948, he meticulously followed these folks for 50 years and beyond, keeping track of what each person ate and how much their disease progressed after they entered the study. One of his most detailed papers, “Multiple sclerosis: fat-oil relationship,” documented the 34-year results of that massive undertaking.
As Swank explained in his paper, the patients had to keep detailed food logs of their daily gustatory adventures. They also trekked to a Montreal clinic once every two weeks to get their MS assessed and endure a pop quiz about their eating habits. (Due to humans being sucky remember-ers (and notorious “historical revisionists” of our own mistakes), dietary recalls are often unreliable—but Swank collected so many of them, over such a vast span of years, that he could paint a pretty accurate picture for each patient.) Once their new, Swank-approved eating habits had stabilized, those patients were weaned onto less frequent clinic checkups and did much of their reporting by snail mail.
To gauge how each person’s disease changed throughout the study, Swank used a neurological grading system ranging from 0 to 6, abridged here for reading ease:
0. Remission, more or less
1. Some neurological symptoms, with fatigue and periodic exhaustion
2. Mild physical impairments
3. Severe physical impairments
4. Wheelchair-bound, with memory impairment
5. Confined to bed and chair
6. Dead
From the get-go, the goal was to slash participants’ animal fat intake down from an average of 125 grams per day (pre-Swankification) to a maximum of 10 to 15 grams per day (post-Swankification). Starting in 1951, they could also add 5 grams of cod liver oil and eat between 10 and 40 grams of “fluid vegetable oils” daily, though saturated fat was supposed to stay as low as possible.
Of course, we humans are wont to err, and not all of the patients colored within the low-fat lines. Swank noted that some people “doubled or even tripled the amount of [saturated] fat* recommended,” and that in lieu of a control group, those variations made it possible to see how different fat intakes correlated with MS progression over the decades. Yay math!
* A Swanky disclaimer: although I’m employing more familiar terminology for the sake of this blog post, note that Swank uses the words “fat” and “oil” a bit differently in his papers. “Fat” in his work refers only to saturated fat, while “oil” refers only to unsaturated fats. So if you take a gander at any of his publications (which I recommend you do!), just keep in mind that his “fat” translates to our definition of “saturated fat” rather than “total fat.”
By the 34-year mark, a bit over half of the original group—81 people—had passed away. That’s actually pretty promising: Swank noted that when he first started studying MS, most patients were expected to end up bedridden or wheelchair-bound within a decade or two, and the assumption was that “all would be dead within 35 years.”
But where it gets really interesting is when the Swankers were divided up based on their average saturated fat intake. Of those who didn’t exceed 20 grams per day (70 people), only 31% died over the course of the study (20% specifically from MS). But of those who ate more than 20 grams of saturated fat per day (74 people), a whoppin’ 80% perished in that same time frame (62% specifically from MS). Voila: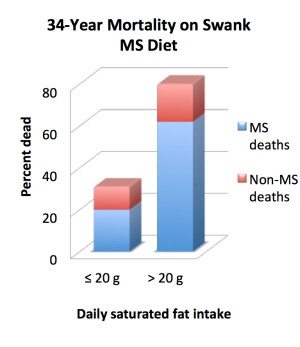 And when we break it down a bit further, something even more interesting emerges: the saturated fat/mortality trend wasn’t linear. Like, at all. Folks eating between 20.1 and 30 grams per day had ridiculously similar mortality rates to those eating 30.1 to 50 grams and beyond. Basically, once people crossed the 20-grams-per-day threshold, it didn’t seem to matter how much saturated fat they were eating: mortality rates rapidly maxed out and then stayed relatively constant. It’s like a saturated-fatty version of the Macronutrient Swampland, where everything outside the “magic” zone is super samey!
And when we break it down a bit further, something even more interesting emerges: the saturated fat/mortality trend wasn’t linear. Like, at all. Folks eating between 20.1 and 30 grams per day had ridiculously similar mortality rates to those eating 30.1 to 50 grams and beyond. Basically, once people crossed the 20-grams-per-day threshold, it didn’t seem to matter how much saturated fat they were eating: mortality rates rapidly maxed out and then stayed relatively constant. It’s like a saturated-fatty version of the Macronutrient Swampland, where everything outside the “magic” zone is super samey!
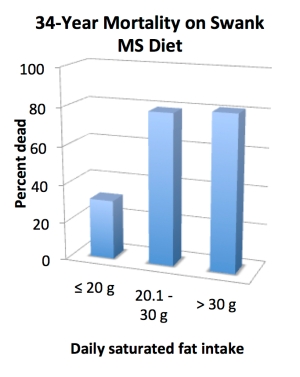
FYI: average saturated fat intake for the lowest bracket was 17 grams per day; for the middle bracket, 25 grams per day; and for the highest bracket, 42 grams per day.
(In case you’re wondering, it didn’t seem to be a matter of having a longer but more miserable, enfeebled life for the low-fat adherents. As Swank noted, “Patients on our low-fat diet have been remarkably free of bacterial and viral infections, ‘colds and flu’ occur rarely, and recovering from urinary and other bacterial infections has been rapid when appropriately treated.” Indeed, quite a few measures of their health improved.)
The Swankers’ disease progression—as tracked by that neurological scale mentioned earlier—followed a similar trend. For the folks eating 20 or fewer grams of saturated fat per day, the disease remained relatively stable, with just over half a grade of progression (worsening) on average. But for the subset of folks eating between 20.1 and 30 grams per day, the disease progressed an average of 2.6 grades. And for those chowing down on more than 30 grams per day, the disease worsened by an average of 3.0 grades. (To help conceptualize that, a three-grade change is the equivalent of going from “mild physical impairments” to “confined to bed and chair.”)
Here are more Smurf-colored bars for the visually inclined:
And because I love me some graphs, here’s another one straight from Swank’s paper, showing the dramatic drop in exacerbation (flare-up) rates before and after folks got all Swanky:
Pretty impressive, no?
In addition to all this fun stuff, Swank commented (again, in his 1991 paper “Multiple sclerosis: fat-oil relationship“), that some patients needed an even steeper slash in their saturated fat intake—down to 10 grams per day, maximum—in order to “gain an improvement in energy and freedom from severe fluctuations of disease.” Swank wrote:
In recent years, this experience induced us to eliminate all meats and other sources of fat from the diet of many patients when first seen. We estimate that saturated animal fat was reduced to ~5 g/day plus the fractional or trace amounts of fat contained in many foods. It is our impression that these patients improved faster than others in whom this was not done.
In the vein of Devil’s Advocation, though, we should give our critical-thinking wheels a whirl and see if there are any alternative explanations for these findings. Could there be some suspicious lifestyle confounders like we see in studies today? Were saturated fats lumped in with hydrogenated ones and mutually given the boot, while only the latter was a true health-harmer? Was the supplementation of cod liver oil, chock full of omega-3 and vitamin-A-rich goodness, enough to explain the mortality patterns? Was the culprit saturated fat itself, or was it just guilty by association—maybe serving as a proxy for generalized I-Don’t-Give-A-Hoot-About-My-Health-itis, as the rebels who ignored Swank’s “eat less saturated fat!” message were more likely to ignore the “sugar is bad” or “vegetables are good” or “don’t run with scissors while chewing arsenic candy” messages as well?
As much as I love wailing my confounder alarms, I don’t think the usual suspects apply in this case. Here’s why!
- Hydrogenated fats were indeed banned from the menu, but not until 1951—two or three years after folks started the diet, at which point they’d already seen profound improvements.
- Likewise, cod liver oil (and other omega-3-rich fluid oils) weren’t allowed during the first couple years of the diet, and again, folks saw an 80% decrease in their MS flare-up rates during that time.
- As for potential bad-guy carbs skewing the results? Remember, Swank developed his diet in the late 1940s—decades before refined grains and sugar joined the Dietary Villain ranks and were widely considered harmful. In fact, his diet didn’t restrict refined grains or sugar to begin with, so it wouldn’t make sense that a “screw it all” mentality would result in folks rebelliously downing processed carbs. (Heck, in Swank’s Multiple Sclerosis Diet book, there are plenty of recipes calling for white flour and sugar, and no indication that his patients—at least during the first few decades—were told to stick to whole-food sources of carbohydrate.)
And lest we wonder if the folks eating more saturated fat were also eating more of those gnarly, high-PUFA vegetable oils we so love to hate (thus obscuring the real relationship between saturated fat and MS progression): no dice! Swank’s data showed pretty clearly that the more saturated fat people ate, the less vegetable oil they were eating—an inverse correlation of -0.62 by the study’s 22nd year. Likewise, as Swank explained in the paper we’ve been discussing, higher unsaturated oil intake went hand-in-hand with better outcomes in terms of disability and mortality. The inclusion of vegetable oils “seemed to make patients feel better, increased their energy, and improved the condition of hair and skin,” even though Swank maintained they weren’t necessary for treating MS itself (since his patients took a fantastic turn for the better before those oils were added back to the diet).
Hence why I called Swank a “monkey wrench” a bit earlier on. In contrast to the theory that rock-bottom PUFA levels are the real reason very low fat diets work (while saturated fat would be an innocent, needlessly reduced bystander), Swank found the opposite to be true—that saturated fat had the strongest relationship with MS progression and mortality, while polyunsaturated fat levels could be scaled up or down without negatively impacting health. At least within that 10 to 40 gram range. And at least for multiple sclerosis (although mortality from other chronic diseases dropped during Swank’s diet as well).
That said, there is another possibility that could maybe, maybe, MAYBE be obscuring the saturated fat trend: Neu5Gc. This is a little sialic acid molecule that humans, rather uniquely, can’t synthesize. We produce a similar molecule called Neu5Ac, but lost the ability to make Neu5Gc after splitting from our last common ancestor with the great apes. Because gene mutations ‘n stuff. Other primates (and almost all mammals) can still synthesize Neu5Gc just fine!
Here’s why it matters: even though we can’t make Neu5Gc on our own, we can incorporate it into our tissues when we ingest it from food. And the prime sources of Neu5Gc happen to be red meat and dairy, the same food-vehicles that deliver most of our saturated fat. Because Neu5Gc looks like a foreign substance to our paranoid human innards, we’re capable of producing antibodies against it (although levels of those antibodies vary widely from person to person), which, in turn, can stir up all sorts of trouble. So far, we’ve got theories about a potential role for anti-Neu5Gc’s antibodies in systemic inflammation, cancer, heart disease, hypothyroidism, and also… WAIT FOR IT… multiple sclerosis. (See: “Why does multiple sclerosis only affect human primates?” and “Missing links in multiple sclerosis etiology. A working connecting hypothesis.“)
I waffled over whether to even include this speculation here, since Neu5Gc research is just a wobbly-kneed babe in the woods right now, and we’d need a lot more data before we could definitively link it to any disease. But, considering that 1) humans are the only primate that develops multiple sclerosis, 2) humans are the only mammal that can’t make Neu5Gc (and that produce antibodies against it), 3) multiple sclerosis tends to cluster around areas with a higher intake of Neu5Gc-containing foods (land meat and dairy), and 4) there’s a plausible mechanism linking Neu5Gc with the development of multiple sclerosis (through the effects of antibodies on the blood-brain barrier and axon-myelin unit)… well, all I’m sayin’ is it seems quite intriguing!
That said, Swank actually had some compelling, research-backed ideas about why saturated fat per se could trigger MS, which we’ll discuss in Part 2 of this post. It’s worth noting that he didn’t believe saturated fat causes multiple sclerosis, just that it “precipitates or accelerates it in susceptible individuals,” as he wrote in 1954. It’s not outside the realm of possibility that Neu5Gc somehow plays the role in the development of MS, while saturated fat, under specific conditions, aggravates it. So, even if this Neu5Gc stuff pans out, it doesn’t necessarily pardon saturated fat!
At any rate, we’re not quite at the end of Swank’s research rope. In 2003, he published the 50-year results of his never-ending study: “Review of MS patient survival on a Swank low saturated fat diet.” By that time, after 16 years of letting them do their own thang, he’d managed to track down 15 of his surviving participants and pull them in for interviews and in-person visits. They were all between 72 and 84 years old. (Swank himself was 94, and in case you’re wondering, was still goin’ strong until he passed away in 2008 at the age of 99). Amazingly, only two survivors needed help walking and had any sign of their disease; as for the others, Swank described it thusly:
The remaining 13 patients were remarkably well. They were very active, could care for themselves, could walk as necessary, and were normal mentally. … [They] stood and were active and unusually youthful looking, with very smooth facial skin devoid of wrinkles due to good subcutaneous circulation. They were all in friendly, good spirits, had joyful laughter, and generally quite youthful behavior. This study also indicated that patients with MS, if they rigorously follow the extremely low-fat diet proposed by Swank, which contains no more than 10 to 15 g/d of saturated fat, can expect to survive and be ambulant and otherwise normal to an advanced age.
Take note of that “good subcutaneous circulation” comment, because it’s at the crux of Swank’s theory about why saturated fat is harmful for MS patients (hint: it has to do with blood cell aggregation and oxygenation). More on that in the next blog-post installment! We’ll be coming back to some of Swank’s research and ideas when we discuss the science behind why low-fatting works, because he’s just that awesome.
In the meantime, we’re hardly done with our historical saga. Next up is another obscure figure from the dusty, carb-encrusted pages of science’s past: Lester Morrison.
Lester Morrison is a man of mystery. A mystery, in part, because he was using low-fat diets to treat heart disease years before Ancel Keys supposedly introduced the idea to the world. A mystery also because for a guy who did some neat stuff, he’s totally not Google-stalkable. Nary a pixel of his face could be found in my sleuthing efforts, and the only bio-esque document seems to be his obituary.
Here’s what we do know. A rather precocious and multitalented individual (along with being a physician, he was an accomplished violinist, historian, symphony concertmaster, novelist, and maybe also Spiderman, and won his first research award when he was a sweet 16), Morrison plunged into the research field with an initial focus on gastroenterology. His first taste of Fat Suspiciousness came in the 1940s, after noticing heart disease and stroke mortality dropped hand-in-hand with wartime food rationing—which curbed, among other things, dietary fat. As he explained in his 1955 article, “A nutritional program for prolongation of life in coronary atherosclerosis,” World War I saw the first parallel dance between food rationing and heart disease, with the British blockade of Germany; World War II was fat-jà-vu all over again:
During World War II … the various Scandinavian governments supplied the information that, when fat in the diets of the population had to be reduced to a minimum because of the scarcity of dietary fats, the death and sickness rate from atherosclerosis was likewise reduced to a minimum. As soon as the war ended and dietary fat once again became plentiful, the mortality rate and morbidity rates from coronary and cerebrovascular disease promptly soared to prewar levels and even began to surpass them.
If you’ve read my critique of Forks Over Knives—a documentary that cited the same wartime stats as evidence for low-fat-plant-based superiority—then you already know I have some bones to pick with those correlations. As I explained in my critique, the rationing-induced changges involved far more than tanking total dietary fat: during World War II, seafood consumption doubled; sugar intake halved; vitamin K2 intake rose; trans-fat-containing-margarines all but exited the table. Not to mention, any situation of food restriction tends to boost vascular health, at least initially.
Nonetheless, the link between war rationing and mortality seemed to catch a lot of eyes, and Morrison’s were two of ’em. Cardiovascular disease had slayed a hefty portion of family (including his mom and dad), so the issue was quite near to his heart (literally!). Thus, he was inspired to investigate the matter in a more controlled setting.
In 1946—years, again, before Keys was hot on fat’s trail—Morrison launched a dietary study involving 100 people who’d recently survived a heart attack. For 50 patients, he left their menu as-is: fairly high in fat (80 – 160 grams per day) and high in cholesterol (200 – 1800 mg per day). For the other 50, he prescribed a war-rationing-inspired diet limited to 20 – 25 grams of fat per day—with continual supervision for both the patients and their families to ensure they stuck with it (and the boot given to anyone who couldn’t promise total compliance). He then followed everyone for eight years to see how many folks perished from each group.
In his papers “Arteriosclerosis: Recent advances in the dietary and medicinal treatment” (1951) and “A nutritional program for prolongation of life in coronary atherosclerosis” (1955), Morrison gave a detailed outline of his experimental diet, which was designed specifically to lower folks’ cholesterol. (Worth noting: the diet didn’t limit sugar or other sweeteners, and didn’t reduce animal protein intake, as a variety of lean meats and dairy were allowed. In fact, it prescribed 60 – 100 grams of mostly animal-based protein per day, and folks ended up eating closer to 120 grams on average—well above the 5% threshold deemed toxic by T. Colin Campbell. Just sayin’!)
The encouraged edibles:
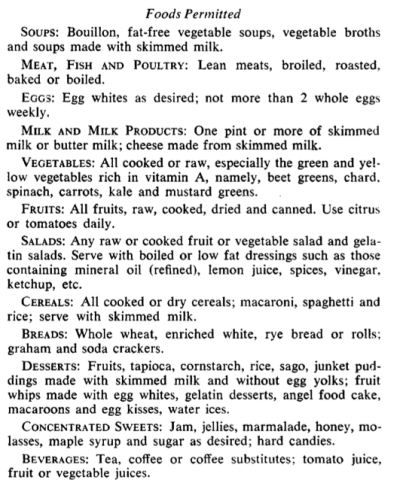 And the no-nos:
And the no-nos:  (Patients were also encouraged to take a multivitamin containing vitamin A.)
(Patients were also encouraged to take a multivitamin containing vitamin A.)
The results? You can probably guess where this is headed! As intended, the diet tanked people’s total cholesterol—by an average of almost 100 mg/dL, in fact. But that’s just the beginning. At the three year mark, 15 people from the control group had died of heart disease, compared to only seven from the low-fat group. (That’s a difference of 70% versus 84% survival.) By the eight year mark, the survival rates had whittled down to 24% of the control group versus 56% of the low-fat group (again, most deaths being from heart disease). And by the study’s 12th year? A whoppin’ nobody was alive from the control group, whereas 34% of the low-fat group was still roaming this lovely green earth.
(Along with the whole “dying less” thing, Morrison noted that his fat-restricted patients frequently reported “a sense of optimism, well-being, and good spirits” after adopting the diet—a sentiment Swank echoed as well, though without either of their studies being blinded, it’s hard to say how much was just a placebo effect.)
As with the other old research we’re resurrecting in this post, the beauty of Morrison’s study is that it gracefully dodged some confounders that muck up science today. Back when he conducted his fat-slashing experiment, nobody was telling the public that sugar and refined carbs were bad along with fat. No one had an inbox full of Meat’s gonna kill ya news headlines. No one had nutrition labels on their food, or a reason to fear egg yolks, or retinas permanently emblazoned with the image of the Food Pyramid. Heck, even smoking wasn’t widely considered a health hazard yet (the Surgeon General didn’t officially declare a causal link between smoking and lung cancer until 1957). Americans’ minds were clean slates, and prescribing a shiny new dietary change (like reducing fat) didn’t invoke the same confounder cascade we see today. How grand!
All that said, in Morrison’s case, there were two potential caveats we should take note of. One, the low-fat group saw some initial weight loss—an average of 21 pounds for men and 17 for women during the first three years, but with no additional changes during the rest of the study—whereas the control group remained weight-stable the whole time. And two, the low-fatters appeared to spontaneously increase their protein intake, making it hard to know what macronutrient change—the uppage of protein or downage of fat—was really driving the results. Could these be the true wizards behind the better-survival curtain?
It’s certainly possible, though I’m hesitant to say they could fully account for 12 years of dramatically lower death rates. Protein doesn’t seem uniquely beneficial for heart disease patients, and there’s a dearth of research looking at intentional weight loss on post-heart-attack survival—so we really have no way of knowing how big a factor that was for Morrison’s patients. (Oddly enough, population studies show that being overweight rather than normal-weight actually predicts better long-term survival for people who have heart disease—and what’s more, losing weight after having a heart attack is counter-intuitively associated with higher mortality rates. Researchers call this the “obesity paradox“: carrying extra weight tends to increase people’s risk of getting heart disease, but for folks who already have the disease, it seems to prolong life. Of course, there could be quite a few alternative explanations for that trend, which are thoroughly discussed here. Interesting, nonetheless!)
At any rate, Morrison was excited (but wisely cautious) about his study’s results, and ended up penning a book called “The Low-Fat Way to Health and Longer Life,” which he published in 1958—the same year Ancel Keys launched the Seven Countries Study. But, refreshingly non-gun-jumping scientist that he was, he also called for “similar surveys utilizing larger numbers of cases for statistical evaluation” in order to deepen and replicate his findings.
And as luck would have it, those surveys eventually came from one of his very own patients: Nathan Pritikin!
Nathan Pritikin: heart un-breaker extraordinaire
 (NOTE: unless otherwise referenced, the background info in this section comes from the memoir, “Pritikin: The Man Who Healed America’s Heart,” which is actually one of the most interesting biographies I’ve ever read!)
(NOTE: unless otherwise referenced, the background info in this section comes from the memoir, “Pritikin: The Man Who Healed America’s Heart,” which is actually one of the most interesting biographies I’ve ever read!)
Small world gettin’ smaller, eh?
Nathan Pritikin is probably best known for two things: 1) promoting an uber-low-fat diet (and running a longevity center dedicated to such); and 2) being downright chummy with George McGovern—the senator in charge of the 1977 Dietary Goals for the United States. (As I detailed in “Death by Food Pyramid,” McGovern ate a quasi-Pritikin diet for many years, delivered Pritikin’s eulogy, and drew a fair bit of inspiration from the man while crafting America’s new low-fat food recs.)
Pritikin’s dietary saga started with the same World War II trends that inspired so many of his fat-slashing contemporaries. Thanks to some work he’d done on bombsights for the Air Force (he was a prolific inventor and engineer by trade), Pritikin had free-for-all access to classified military documents—including the mortality data being churned out for civilians and prisoners. His puzzle-loving mind was intrigued that heart disease rates were dropping in areas plagued by intense stress and low food availability, when most health authorities expected the opposite to occur.
In 1955, an increasingly health-interested Pritikin made a trek to visit Mystery Man Morrison. The two nerded out about heart disease theories, and at the good doctor’s urging, Pritikin had his cholesterol tested for the first time—revealing a borderline-high level of 280 mg/dL. Although he started making some minor dietary tweaks after that, it wasn’t until an official heart disease diagnosis in 1958 that Pritikin kicked his nightly-pint-of-ice-cream habit and got serious about healing himself.
And we’re talking serious serious. For the next ten years, Pritikin guinea-pigged his body with every dietary permutation imaginable. He’d go for weeks eating almost nothing but lentils, or brown rice, or brown rice plus beef; he’d make slight or dramatic adjustments to his vegetable-grain-meat ratios; he’d experiment with eating ten dates after dinner (fruit, not women; this was before Tinder). And in true scientist fashion, he got his blood tested after each new food stint—meticulously documenting changes in his cholesterol levels, triglycerides, fasting and non-fasting glucose, red blood cell count, white blood cell count, hemoglobin, platelets, carbon dioxide, electrolytes, free thyroxine, and pretty much everything else he could cajole his docs into measuring. Be still, my nerd heart!
Although he managed to whittle his cholesterol down to 155 mg/dL with a lowish-fat menu (including a daily helping of nuts, tiny amounts of oil, and some fish and meat), his next EKG didn’t show a lick of improvement. But the man was not deterred! Pritikin low-fatted harder. He nixed the nuts and oil and meat. He pounded his total cholesterol down to 120 mg/dL. And at his next EKG six months later, the report was music to his ears (and a shock to his diet-skeptical doctors): “Definite improvement since the [last] tracing … Normal electrocardiogram.”
Ensuing stress tests over the next few years confirmed that his once-diseased ticker was, for all intents and purposes, healed.
By the 1970s, Pritikin had not only dialed in his own diet to his strict standards of perfection; he’d also amassed hundreds of low-fat devotees—family, friends, friends of friends, and eventually word-of-mouthers—whom he counseled over the phone for free. And in 1976, the real fun began: Pritikin opened the doors of his first Longevity Center in California. Riiiiight here:

The Casa Del Mar building, later transformed into Pritikin’s healing grounds. From Santa Monica Library Archive.
It was in this magical palace, wringing patients through a 26-day diet overhaul and hawkishly watching their food intake, that Pritikin could document the effects of his program on a large-scale basis.
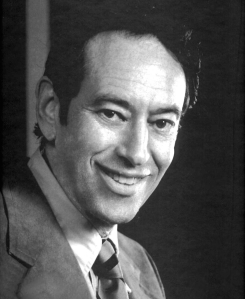
And document he did! Although his reputation was that of a heart-healer, Pritikin’s diet did far more than assuage troubled arteries. Just as Kempner saw, the uber-fatlessness had the fortunate side effect of rapidly—and often permanently—healing diabetes. The earliest PubMed-able record of Pritikin’s success with diabetics came in 1976, with this little gem:
(FYI: Pritikin’s name isn’t on this paper, but it darn well should be. Scandalous tidbit alert! In 1974, Pritikin divulged the details of his diet to a Dr. James W. Anderson—an internationally acclaimed diabetes researcher at the time—and proposed an official study to test the uber-low-fatness on diabetics. Pritikin designed every detail of the study, drummed up $10,000 to fund it, created meal plans, and then received a grand total of zero credit for any of his contributions once the study was completed and published. In fact, Anderson proceeded to repackage Pritikin’s diet under a different name (the “HFC Diet,” standing for the “High Fiber, High Carbohydrate Diet”) and claimed it as his own invention—conducting a number of additional studies so successful that, in 1979, the American Diabetes Association was inspired to downsize its recommended fat intake. Despite years of haranguing Pritikin for more funding money (and thanking him profusely in their private correspondences), Anderson never publicly mentioned his collaboration with Pritikin or credited him for originating the diet. Buuuurn.)
So what was this study all about? For one week, 13 diabetic men—all who needed either insulin or oral drugs to control their blood sugar—ate the standard American Diabetes Association diet of the time: 34% fat and 43% carbohydrate, the rest made up of protein and wishful thinking. After that, they spent at least two weeks in Carbsville, eating a diet of only 9% fat and 75% carbohydrate. (The two diets were isocaloric, meaning they had the same number of calories, and were designed to help folks maintain their weight rather than lose or gain any.)
Surely that carb palooza sent their blood sugar into a frenzy! …Except it didn’t. After switching from the ADA diet to Pritikin-hijacked-by-Anderson one, nine patients had their insulin and oral drugs completely discontinued—at which point their fasting blood sugar was actually lower than it had been when they were still on medication. (The cutoff for drug discontinuation was a fasting blood sugar of 120 mg/dL.) It only took nine days of low-fatting to make that happen! Another patient’s insulin needs dropped from 28 to 15 units per day. As a further head-scratcher, fasting triglycerides, contrary to what we might expect, dropped significantly for ten men. The only folks who didn’t see any benefit from the 9% fat diet were the three who had the most advanced diabetes at the study’s onset—needing 40 to 55 units of insulin per day.
A tabular and graph-ular representation of changes in fasting blood sugar, in case you’re curious:
Even more intriguing, those results weren’t just a result of weight loss. Only five patients dropped more than three pounds, and there was no difference in fasting blood sugar and triglyceride levels between them and the weight-stable folk. And most importantly, the results seemed to stick: after the study, the nine most successful patients were weaned onto more flexible diets—60 to 65% carbohydrate instead of 75%. And after at least four months of followup, the researchers noted their blood markers hadn’t changed and the “control of the diabetes has been satisfactory without any drug therapy.” Pretty neat, huh?
Okay, okay: this study was tiny and used only men and we could find plenty of things to complain about (more womenfolk! Longer time frame! More Instagram pictures of the researchers’ feet overlooking exotic and envy-inducing locales!). Those are fair criticisms, to be sure. But this study does offer something we hardly ever see: a direct comparison between a Swampland menu (34% fat) and a Carbosis menu (9%), with the subsequent revelation that Oh hey, they actually have totally different results!
Again, as I’m trying to hammer home in this post, most of our “low fat” studies are actually only comparing different shades of Swamplandness—without ever hitting that fantastical 10% that brings a dramatic metabolic shift. And that makes us think that low fat is just a sham that does nothing except make our food taste like rabbit chow. So finding a study-gem like this, where fat intake actually does dip into the magic zone, and where the impressive results challenge our “low fat is bunk” narrative, is a rare and valuable find—even if it could be better designed.
That said, we’re in luck because Pritikin actually published some of his own studies on diabetics, and they were bigger and longer. Two of those papers came out in 1982 and 1983, respectively:
- Response of non-insulin-dependent diabetic patients to an intensive program of diet and exercise.
- Long-term use of a high-complex-carbohydrate, high-fiber, low-fat diet and exercise in the treatment of NIDDM patients.
The first paper looks at how 60 diabetics fared during the 26-day program; the second paper looks at how they did once released back into the scary, high-fat-food-filled ‘real world.’ In the latter, Pritikin described the in-house program as such:
During the 26-day session, the patients were served and taught to prepare the Pritikin high-complex-carbohydrate, high-fiber, low-fat diet. The diet consisted of unprocessed natural food with no supplements, e.g. guar. Less than 10% of the total calories were obtained from fat, … 13% from protein, and the remainder from carbohydrate (90% complex—whole wheat grain, rice and bread, beans, peas and other vegetables, and fresh fruit). … Protein was derived primarily from vegetable sources, except for nonfat milk, which was served daily, and small amounts of fish or fowl, of which 85 g/wk were provided.
Right off the bat, we can see the study wasn’t free from animal protein, as folks were allowed to drink a fair amount of skim milk, chock full of that awful casein vilified in The China Study. It also contained very small (but not irrelevant) amounts of poultry and fish—about this much per week:
On top of that, the Pritikinites who started out overweight had their calories restricted, but everyone else could eat as much as they wanted (ad libitum). And all the participants were encouraged to go on short walks each day.
So what happened? At the end of their 26-day bootcamp, their pancreases exploded! Just kidding. They did super well. Of the 23 patients who’d entered the program needing to take oral hypoglycemic drugs, all but two had ditched them by the end of the program:
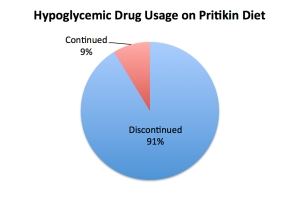 And of the 17 folks who’d been taking insulin (with dosages ranging from 14 to 75 units per day), all but four were released from its needly shackles:
And of the 17 folks who’d been taking insulin (with dosages ranging from 14 to 75 units per day), all but four were released from its needly shackles:
 (After crunching the numbers, it turned out people’s reduction in fasting blood sugar was not correlated with weight loss, or with the amount of walking they did, or other changes that we might suspect played a role. Dietary adherence reigned supreme!)
(After crunching the numbers, it turned out people’s reduction in fasting blood sugar was not correlated with weight loss, or with the amount of walking they did, or other changes that we might suspect played a role. Dietary adherence reigned supreme!)
Okay, I know what you’re thinking. Those results are nice and all, but 26 days is nothing in the span of a person’s disease history. Heck, I’ve had hold-sessions with Comcast last longer than that! What happened afterwards? Did Carbjo cometh?
Luckily, Pritikin wanted to know the answer to those questions too. Between two and three years after their romp at the Longevity Center, the patients got a phone call quizzing them on how well they’d stuck with the diet, how much they were exercising, and whether their medical status had changed. They also had to answer dietary recall surveys and food-frequency questionnaires, and got a fasting blood-sample kit in the mail, which is kind of weird but probably a lot more exciting than bills and MasterCard offers.
The results? Compared to when they were freshly released from their low-fat boot camp, seven more people were taking oral hypoglycemic drugs, and four more people were taking insulin. Does that mean the diet failed?! Can we sling a big, fat “I told you so!” to the low-fat warlords and reassure ourselves that the diet is bogus? Actually:
… the main difference between those patients who went back on medication at follow-up compared with those remaining off medication was the percent of calories derived from fat.
Basically, those who stuck with the diet kept reaping the initial rewards, but those who gallivanted back into the Swampland paid dearly!
Of course, all that’s a mere smidgen of the data that got churned out from the Longevity Center over the years. R. James Barnard, who’s served as Research Director at the Pritikin Center (among quite a few other professional feats), published over 100 studies on the Pritikin Program, looking at everything from cancer to diabetes to heart disease.
And while part of me would love to sit here and write about EVERY SINGLE ONE of those studies in attempt to explode the internet with Literally the Longest Blog Post Ever, another part of me—the part that realizes even the most patient of my readers have sanity limits and day jobs—has vetoed that plan in favor of a briefer sampling. Behold!
ESCAPE HATCH FOR THE FATIGUED OF BRAIN: what follows is a pretty long and sciency scroll of scientific scienceness. I know this blog post is big. I know your brain is turning into soup. CLICK HERE if you want to bypass the study summaries and get back to Pritikin’s life narrative!
Note: the Pritikin Program involves both the Pritikin diet and an hour of daily walking. Although we could definitely consider exercise a confounder (since it can independently improve metabolic and hormonal markers), studies of walking alone haven’t demonstrated anything nearly as dramatic as what’s been achieved with the Pritikin Program. At best, we could wager that walking probably boosts the results of the program, but only contributes to a fraction of its overall effects.
Another note! Unless otherwise mentioned, all the studies below allowed an ad libitum (non-calorie-restricted) energy intake. The participants could eat as much as their hearts desired out of any Pritikin-friendly item except for fish and poultry, which were capped at three servings per week (combined).
Prostate Cancer Protection
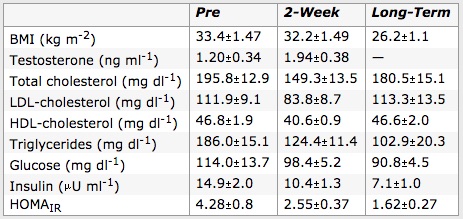
- Long-term adherence to the Pritikin Program was a major boon for squashing out insulin resistance and reducing prostate cancer risk. Folks who followed the diet between 1 and 28 years reduced fasting insulin by 52%, fasting glucose by 20%, HOMA IR (a measure of insulin resistance) by 62%, and fasting triglycerides by 45%. And in a group of overweight men, even a quick jaunt on the program (two weeks) reduced fasting insulin by 30%, fasting glucose by 14%, HOMA IR by 40%, and fasting triglycerides by 33%. Not impressed yet? Blood from the Pritikin-fed fellows (both two-week and long-term) drastically slowed the growth of prostate epithelial cells, suggesting benefit for the prevention of prostate cancer.
From “Effect of diet and exercise intervention on the growth of prostate epithelial cells.” Barnard, 2008.
- In a similar study of both short-term (11 days) and long-term (average 14.2 years) Pritikin followers, more evidence of prostate cancer protection emerged. The short-termers saw a 20% drop in insulin-like growth factor 1 (IGF-1) levels and a 53% rise (that’s a good thing!) in insulin-like growth factor binding protein 1 (IGFBP-1); the long-termers saw a solid 55% drop in IGF-1 and 150% rise in IGFBP-1. (IGF-1 has been strongly associated with cancer due to its role in regulating cell growth and death, and and IGFBPs are proteins that bind insulin-like growth factors and neutralize some of their unsavory activities.) Likewise, the short-term group saw a 25% drop in fasting insulin levels and the long-term group saw a 68% drop. As with the previous study, both groups’ Pritikin-ified blood was particularly awesome at fighting cancer: the serum from the short-termers caused a 30% decrease in the growth of LNCaP cells (a line of human prostate cancer cells) and serum from the long-termers caused a 44% decrease, compared to baseline. Both groups’ blood also increased the rate of death for those cancer cells.
- Yet another study of Pritikin dieters (27 obese men) showed the program may be an excellent defense against the disease: the men saw a 28% increase of sex hormone-binding globulin (which binds androgens and appears to help protect against prostate cancer) and a 43% drop in fasting insulin; for three men who started out with slightly elevated PSA (prostate-specific antigen) levels, the diet also reduced that. According to the researchers, “The increase in SHBG would result in more testosterone being bound and, therefore, less of the androgen available to act on the prostate. The decrease in insulin might also decrease mitogenic activity in the prostate.”
- One more on the prostate front! An analysis of post-Pritikin-Program blood shed light on the mechanisms behind the aforementioned anti-cancer effects: apparently, the Pritikin Program reduced tumor cell inflammation and resulted in lower NFκB activation in LNCaP cells. (NFκB, or “nuclear factor kappa-light-chain-enhancer of activated B cells” if you want to be fancy about it, is a protein complex involved in DNA transcription, cell death, and cytokine production.) The program’s results also seemed to hinge on reducing IGF-1 levels, because when the researchers added back IGF-1 back to the participants’ squeaky clean, post-Pritikin-Program serum, the results were completely reversed:
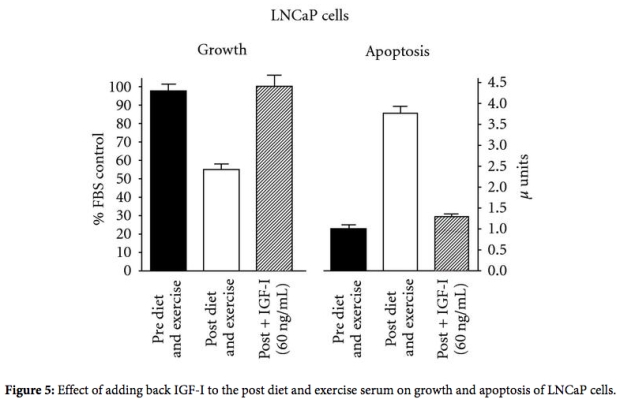
From “Analyzing serum-stimulated prostate cancer cell lines after low-fat, high-fiber diet and exercise intervention.” Barnard, et al., 2011.
Reduced LDL Oxidation and Spiffed-Up HDL
- Three weeks on the Pritikin Program resulted in LDL particles that, even by paleo- and low-carb-advocate standards, were much less likely to oxidize and promote heart disease. In a group of 80 Pritikinning men and women, average LDL particle size increased (with larger LDL considered less atherogenic), and 27% of the folks who’d started out with LDL pattern B switched to LDL pattern A (again, considered less atherogenic). In vitro, the participants’ LDL also became more resistant to copper-induced oxidation—with a 21% drop in initial oxidation, 13% increase in lag time (the delay before oxidation happens, as the LDL’s antioxidants become depleted), a 20% reduction in peak diene formation (a way to measure oxidation), and a 17% reduction in maximal rate of diene formation. All of that jargon basically means the LDL had become far more resistant to oxidation—at least based on this particular assay (there’s always some uncertainty about how well in vitro (outside the body) studies translate to in vivo (inside the body)).
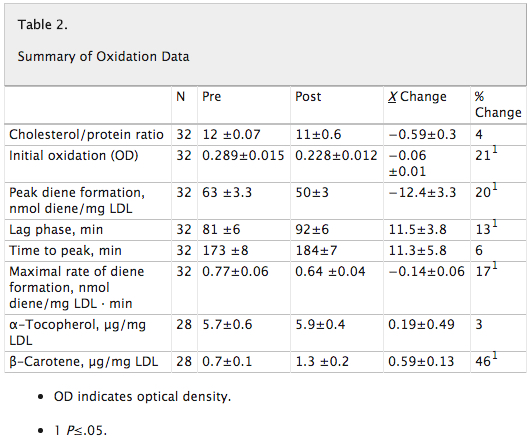
From “Effects of diet and exercise on qualitative and quantitative measures of LDL and its susceptibility to oxidation.” Barnard, 1996.
- Similarly, a study in postmenopausal women found that the Pritikin Program led to more oxidation-resistant LDL particles.
- Even though the Pritikin Program often reduces HDL (the so-called “good cholesterol” lipoprotein), it makes the existing HDL that much awesomer. A study of obese men found that after three weeks in Pritikin Land, the HDL inflammatory index (AKA the ability of HDL to prevent LDL from oxidizing) changed from “pro-inflammatory” to “anti-inflammatory.” The activity of platelet activating factor acetylhydrolase also increased, LDL decreased by 26%, and triglycerides decreased by 29%. Basically, even though HDL was lower than at baseline, its function was mucho improved—”suggesting increased turnover of proinflammatory HDL,” according to the researchers.

From “Effect of a short-term diet and exercise intervention on inflammatory/anti-inflammatory properties of HDL in overweight/obese men with cardiovascular risk factors.” Barnard, et al., 2006.
Breast Cancer Protection
- In postmenopausal women, the Pritikin Program fantastically improved the major metabolic and hormonal risk factors for breast cancer: on average, insulin dropped 29%, insulin-like growth factor 1 (IGF-1) dropped 19%, insulin-like growth factor binding protein 1 (IGFBP-1) increased 32%, estradiol (among women who were on hormone therapy) dropped 34%, and estradiol (among women who weren’t on hormone therapy) dropped 37%. In vitro, serum from those Pritikinettes dramatically slowed the growth (and induced apoptosis, or programmed cell death) in three breast cancer cell lines (MCF-7, T-47D and ZR-75-1) compared to blood from the same ladies before they’d started the diet.
- In a study of pre-menopausal women, two months of the Pritikin diet led to some fun breast-cancer-protective hormonal changes: serum estrone and estradiol (types of estrogens) fell during the women’s early folicular and late luteal phases (with decreases ranging from 18% to 26%), with no negative impact on ovulation. (Exposure to ovarian hormones, especially estrogen, appears to increase breast cancer risk, so these changes could be expected to reduce it.)
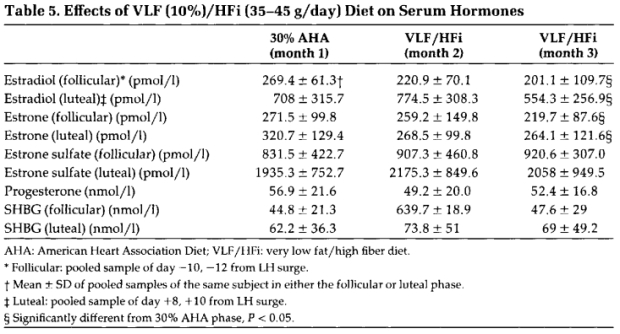
From “Effects of a very low fat, high fiber diet on serum hormones and menstrual function. Implications for breast cancer prevention.” Barnard, et al., 1995.
Colon Cancer Protection
- In women, a 26-day Pritikin diet improved some risk factors of colon cancer by reducing fecal secondary bile acids (which are linked to the promotion of colon cancer).
Heart Disease, and Related Adventures
- Here’s a goodie called, “Effects of an intensive exercise and nutrition program on patients with coronary heart disease: Five-year follow-up.” (There’s no link because for some awfully frustrating reason, this paper is nonexistent online, and I was only able to track it down via the library. Email me if you want a PDF copy!) This study followed the progress of 64 Pritikin adherents with coronary heart disease, five years after they left the sheltered, intensive clutches of the residential program. Prior to entering the program, 59% of the patients had experienced a heart attack and 80% had angina (chest pain). During that five-year follow-up, four people died (one of cancer, two of a heart attack, and one of heart failure during a mitral valve replacement), and two additional folks had non-fatal heart attacks. Reports of angina dropped from the initial 80% to only 32%. Fascinatingly, despite the fact that this was a highly diseased group with the odds stacked against them in terms of morbidity and mortality, their annual death rates ended up being close to that of the “regular” population after they Pritikinized their lives! (At the time the paper was written, post-heart-attack mortality was around 10 to 15% for the first year following the event, and as high as 50% by the third year.)
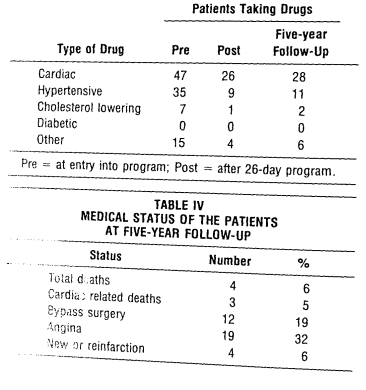
From “Effects of an intensive exercise and nutrition program on patients with coronary heart disease: Five-year follow-up.” Barnard et al. J Cardiac Rehab 1983;3:183-190.
- In 31 obese men, the Pritikin Program brought awesome improvements in a huge range of risk factors for heart disease—including blood lipids, oxidative stress, inflammation, and cell adhesion. After just three weeks, there were significant drops in LDL (25% lower), triglycerides (28% lower), fasting glucose (12% lower), insulin (30% lower), HOMA IR (33% lower), C-reactive protein (39% lower), soluble cell adhesion molecules, inflammatory cytokines, and monocyte adhesion. And to sweeten the deal, nine out of the 15 men who entered the program with an official diagnosis of metabolic syndrome no longer met diagnostic criteria by the time their three weeks of low-fatting was up.
- In 15 hyperlipidemic men, two weeks of the Pritikin bootcamp improved a number of risk factors for heart disease: it lowered the men’s blood pressure, slashed triglycerides, reduced the aggregation velocity and maximum aggregation of platelets, and reduced the formation of thromboxane (which is made by platelets and promotes blood clotting and constriction of blood vessels).
- Combined with daily aerobic exercise, the Pritikin diet facilitated major improvements in myocardial blood flow. After six weeks, resting blood flow decreased by 12%, and hyperemic blood flow increased by 9%—leading to an improved myocardial flow. (It’s impossible to know how much diet versus exercise played a role in these results, though!)
- In postmenopausal women on hormone replacement therapy, the Pritikin Program heralded some promising changes on the heart-disease-protection front. After just two weeks, 20 women saw significant drops in their BMI, glucose levels, insulin levels, all serum lipids, and HOMA IR. The researchers conclude that these “rapid improvements may reduce the risk of acute myocardial infarction (MI), and if sustained, these changes may mitigate the risk for atherosclerosis progression and its clinical consequences.” Not too shabby.
- In a small study of 11 men, the Pritikin Program appeared to be uber protective against atherosclerosis progression. In the span of 21 days, the program dropped LDL by 23%, triglycerides by 41%, fasting insulin by 46%, and fasting blood sugar by 7%. Serum 8-iso-PGF 2 alpha (a product of lipid perodixation) also sank, whereas nitric oxide availability rose. In Barnard, et al.’s words: “The present study is the first to show that unrestricted consumption of a low-fat, high-fiber diet and daily exercise can mitigate oxidative stress, improve NO availability, and normalize BP in obese men within 3 weeks.”
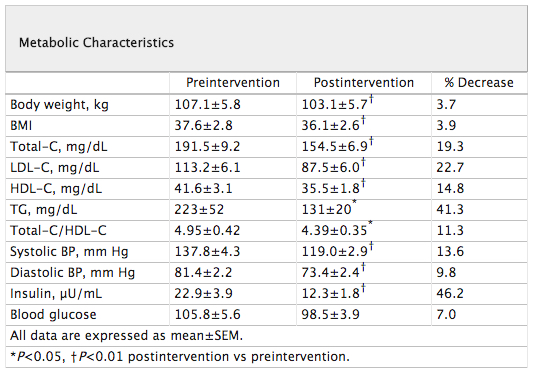
From “Effect of diet and exercise intervention on blood pressure, insulin, oxidative stress, and nitric oxide availability.” Barnard, et al. 2002.
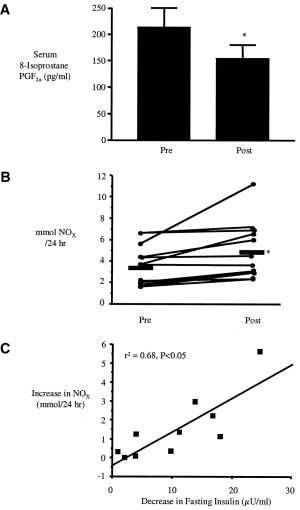
From “Effect of diet and exercise intervention on blood pressure, insulin, oxidative stress, and nitric oxide availability.” Barnard, et al. 2002.
Diabetes Damage Control!
- For 70 diabetics, a 26-day jaunt in the world of Pritikin led to all sorts of disease-blasting perks: fasting blood sugar fell by 24%, blood pressure dropped by 10%—and even better, 71% of the folks who’d been taking oral hypoglycemic drugs pre-Pritikin were able to ditch their prescription (ditto for 44% of the folks taking insulin and 61% of the folks who’d been taking blood pressure medication)! Also, VO2max (“functional maximum oxygen uptake) improved by 41%.
- In diabetic men, a three-week Pritikin Program reduced heart-disease risk factors associated with diabetes: the program whipped down fasting glucose by 20%, dropped fasting insulin by 30%, and totally clobbered markers of oxidative stress, inflammation, and monocyte-endothelial interaction (a major part of the heart disease process). Boom!
- Among 652 non-insulin-dependent diabetics, three weeks of the Pritikin Program significantly improved their condition: fasting glucose dropped by 16%, and 71% of folks taking oral hypoglycemics (and 39% of the folks taking insulin) were able to discontinue those medications. Triglycerides and blood pressure also fell to delightful new lows.
- In diabetics, the Pritikin Program reduced fasting insulin in diabetics by an average of 33% in just three weeks, and restored normal fasting insulin levels in 59% of insulin-resistant folks in the same time frame. (Triglycerides also dropped across the board!)
In the Elderly
- Among 70 folks aged 70 and older (average age of the group being 78.7), 26 days of the Pritikin Program totally spiffed up their health: they lost an average of five pounds, total cholesterol and triglycerides fell significantly, their treadmill performance increased by 49%, the type II diabetics of the group reduced their fasting blood sugar by 27%, and half of the patients taking blood pressure medication were able to discontinue it.
But What About the Children?!
- In overweight and normal-weight children, two weeks of the Pritikin Program yanked down multiple cardiometabolic risk factors: insulin levels fell (by 28.1% in overweight kiddos and 52.5% in normal-weight kiddos, respectively), HOMA-IR fell (28.4% and 53.1%, respectively), leptin levels fell (44.1% and 69.3%, respectively), and a variety of proinflammatory cytokines were reduced (molecules that increase inflammation in the body). LDL went down by 24.5% and 29.4%, while HDL hardly budged. Those changes didn’t correlate with weight loss, either!
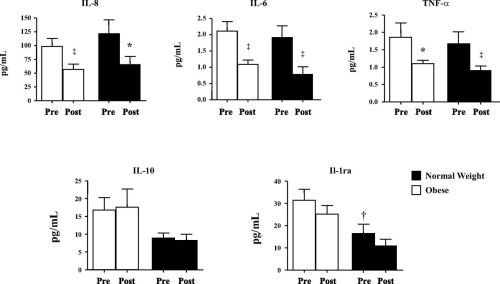
Effect of Pritikin Program on inflammatory cytokines. From “Effects of an intensive short-term diet and exercise intervention: comparison between normal-weight and obese children.” Barnard, 2013.
- Also in children, two weeks on the Pritikin Program (for 19 overweight kiddos) massively improved factors associated with heart disease: the program tanked LDL by 25.3% and triglycerides by 39.5% (HDL didn’t significantly change); 8-isoprostaglandin F2 alpha (a marker of lipid peroxidation) fell by 81%, CRP fell by 41%, and MMP-9 (a measure of plaque stability and progression) fell by 49%. Markers of endothelial cell activation (ICAM-1 and sE-selectin) also went kerplunk! As the researchers summed it up:
“The primary findings of this study provide evidence that even a short-term lifestyle modification program may (1) improve the lipid profile; (2) decrease production of the reactive oxygen species superoxide and hydrogen peroxide and increase NO production; (3) decrease endothelial cell activation and adhesion; (4) decrease inflammation; (5) decrease monocyte chemoattraction; and (6) decrease MMP-9, a marker of plaque destabilization, all of which may contribute to a reduction in atherosclerosis progression.”
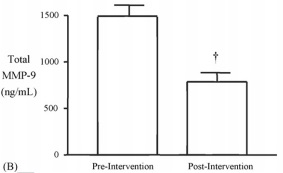
From “Effect of a short-term diet and exercise intervention in youth on atherosclerotic risk factors.” Barnard, et al., 2007.
- WE’RE NOT DONE WITH YOU YET CHILDRUNS. Yet another study on overweight youth found, again, a massive drop in insulin (33%), HOMA-IR (29%), triglycerides (40%), systolic blood pressure (10%), diastolic blood pressure (10%), and LDL (27%), with no change in HDL. All seven of the kiddos who were classified with metabolic syndrome at the start of the study had reversed their diagnosis by the end of it!
And that’s just a freakin’ handful of the research out there. Seriously. A handful. If you want to venture into the full-on Pritikin Research Safari, I recommend bringing snacks and water, ’cause you’ll be gone awhile!
Just to be clear, I’m not trying to say that the Pritikin Program is wildly successful for everyone who jumps aboard, or that it’s unequivocally the best treatment for the diseases it’s been used for. The point I want to make is more conceptual than anything. Contrary to the belief that low-fat, high-carb diets raise insulin levels, muck up glucose control, encourage obesity, and promote inflammation, the overwhelming majority of studies published on the Pritikin diet have shown the polar opposite. That doesn’t mean there isn’t a range of outcomes within each study; indeed, some participants do well, some do really well, and some don’t do well at all, even when the collective effect is positive. But seriously, the Pritikin Program yields impressive results, and it’d take a whole lotta’ somersaults of logic to conclude otherwise.
I know your brain is probably maxed out on scienceness now, so let’s resume our narrative of Mr. Pritikin’s life! First up, an interesting parallel between his way of thinking and that of the modern Paleo community.
In the early ’70s, Pritikin wrote a three-volume opus compiling his theories—dotted with hundreds of scientific references—about every major condition of the time: atherosclerosis, angina, high blood pressure, gout, arthritis, gallstones, kidney stones, diabetes, lung cancer, colon cancer, prostate cancer, breast cancer, as well as hearing and vision diseases. He was convinced they were all, essentially, manifestations of a huge mistake called “What Americans Typically Eat.” In fact, Pritikin had a fascinatingly ‘ancestral’ approach to nutrition (back at a time when linking diet to chronic disease period was considered cuckoo for Cocoa Puffs), which he discussed in the introduction to his three-volume work:
Such a postulation linking diet and the scourge of degenerative diseases may seem far-fetched, until one reflects upon some basic biological facts. All animals, man included, have a diet that emerged from the long-term experience of the species in nature over many thousands of years. Now, man no longer eats foods his body was designed to eat, but has created a synthetic diet—the penalty of which is to endure the adverse effects of short-term experience. The more man’s diet departs from foods to which he is biologically suited, the more the adverse effects.
Whereas the modern incarnation of Paleo has drawn heavily from higher-fat-eating societies (the Inuit and Masaai are particularly cherished), Pritikin found dietary consistency among the starch-based populations: the Tarahumara Indians, the Bantu, and the natives of New Guinea, whose traditional low fat intake and virtual freedom from heart disease fed into his overarching philosophy about food. Just keep that in mind if you find the idea of low-fat eating to be ancestrally preposterous!
For what it’s worth, Pritikin certainly walked his talk. Before his mortal departure, he’d requested an autopsy be performed so the world could have an honest look at his once-diseased heart. The results were published in a New England Journal of Medicine article called “Nathan Pritikin’s heart,” where the state of his ticker blew the pathologist away:
The epicardium was smooth, and no scars were visible. The endocardium and all valves were normal. … The coronary arteries were soft and pliable … there were no raised plaques and no compromise of the lumens. No clots were present. … No infarcts of any size, or other finding referable to vascular disease, were present in any organ.
The report concluded, “In a man 69 years old, the near absence of atherosclerosis and the complete absence of its effects are remarkable.”
Important note on Pritikin’s death: Critics of Pritikin (Priticritics?) often point to his departure from the world—death by suicide, amidst a painful battle with leukemia—as evidence that his low-fat diet either pulverized his mental health (suicide) or gave him cancer (leukemia). Those are both pretty bold claims, so let’s take a moment to assess them.
In the 1950s, Pritikin went through a series of high-dose radiation treatments for a skin condition, pruritus ani, that was stubbornly resisting all the pills and ointments he tried. Over the course of two months, he got blasted with a total of 220 rads (“radiation absorbed doses”) of unfiltered x-rays—the equivalent of getting 3700 chest x-rays or 22 million dental x-rays. Not surprisingly, it wreaked havoc: he soon ended up with a blood condition he’d battle for the rest of his life, later diagnosed as a rare form of leukemia. That all happened before he embarked on a low-fat diet.
Pritikin actually managed to keep his disease in remission for almost three decades, but in late 1984, saw an unfortunate resurgence of symptoms—including leg swelling so severe that he had to stop going on his beloved daily runs. His docs ushered him onto some experimental chemotherapy, telling him it was the only way he could ever resume jogging. Not only did the chemo not help, it also left Pritikin with crippling anemia, kidney failure, diabetes, all-consuming pain, and 30 pounds stripped off his already slender body. In February of 1985, he flew out to New York for a second opinion, was told his case was hopeless and he would certainly die within the next six months, and proceeded to take his own life in a hospital bed in Albany.
As George McGovern reflected, “He was always in charge of his life. It rather followed he’d want to be in charge of his death.”
With all that in mind, can we implicate Pritikin’s diet in his sad demise? With enough mental gymnastics and anti-low-fat bias, sure—but I don’t think it’s particularly logical or fair. Did his diet shorten his life, or lengthen what was originally a grim prognosis? And if we make an automatic diet-death jump, should we do the same for the recent passings we’ve seen in the high-fat community (low-carb guru Barry Groves, saturated-fat-redeemer Mary Enig, or “Carbohydrates Can Kill” author Robert Su)?
As drawn as our human brains are to stories and anecdotes, I think it’s wiser to look at bigger, statistically stable data instead of case studies. Everyone has to die of something, and food isn’t the only tool of the grim reaper.
The one who allegedly pulled the low-fat theory out of thin air, manipulated the American Heart Association into believing it, and took the world by storm with his Machiavellian wiles?
The one who cherry-picked his way into a groundless theory?
The one whose very countenance makes us tremble with rage, as we thrust our butter-encrusted fists in the air in defiance?
Yeah… him.
Let’s get real here for a minute. When it comes to evidence supporting low-fat recommendations, Keys was more like the ending caboose than the engineer driving the train. He was far from the first person to think that fat could play a role in chronic disease. We didn’t need his suspiciously curvilinear six-countries graph, we didn’t need his Seven Countries Study, and we didn’t need his can’t-prove-causation epidemiological utterings to form our “low fat movement.” Those things certainly played a role in pushing low-fat theory into the realm of public policy, but holy massive research pile Batman, there was plenty of evidence already there before he made his own contributions! Heck, Keys was clearly aware of his low-fat predecessors by the time he hit the scene: he even referenced the Rice Diet in his now-infamous 1953 paper “Atherosclerosis: A Problem in Newer Public Health” (PDF), where his six-country graph made its grand debut.
Even if you exit this blog post still believing “low fat” is an awful sham, we can’t keep spreading the myth that Keys was its originator. Every time we place the low-fat movement squarely on his shoulders, a kitten gets ejected from a machine gun and blasts a hole through the ozone. Do you really want to destroy the planet? Do you? I didn’t think so! Let’s just agree right now to put this whole myth to rest, and fill our alotted “hatin’ on Keys” time with more important matters, such as how to invent prosthetic goosebumps for people who cannot feel fear and/or coldness.
Modern Diet Doctor Squad: An update and apology for jumping the gun
Although this post isn’t diving into research by the modern “Plant-Based Diet Doctor Squad” (Caldwell Esselstyn, John McDougall, Dean Ornish, Neal Barnard, and by some definitions Joel Fuhrman), I do want to comment on the first gentleman in that lineup—the heart-disease-bustin’ Esselstyn of the renowned Cleveland Clinic.
If you aren’t already familiar with him, Esselstyn is a super cool cat who I want to adopt as my grandpa, and who’s been treating death-bed-borderline heart disease patients for decades. In my Forks Over Knives critique, I criticized his fat-shunning program on account of the high triglycerides and low HDL it produced in some of his patients, while also pointing out the inconclusiveness of his published work due to its tiny sample size. Allow me to awkwardly quote my self of four years ago:
Holy triglycerides, Batman! Although Esselstyn’s diet helped lower most of his patients’ triglycerides, a couple still have values in the major danger zone (362?). Some of those HDL numbers are looking pretty sorry as well.
All in all, Esselstyn’s study shows that a whole-foods, plant-based diet is probably infinitely better for cardiovascular health than the junky cuisine many folks eat. But it’s far from conclusive evidence that this diet is the best we can do for reversing heart disease, or that it would generally be effective in a population beyond his 11 self-selected subjects. A diet that reduces triglycerides and increases HDL more than his did, for instance, might have an even better outcome.
I’ve written a lot of things in my life. Some of those things have been wrong. This is one of them.
While I still suspect Esselstyn’s diet could be unveganized without harming its therapeutic effect (perhaps through the addition of gelatin, seafood, and whole-grain unicorn flour), I’m no longer convinced that low HDL and high(ish) triglycerides are bad in the context of unprocessed low-fat diets. I’ll explain why that’s the case in Part 2! But in a sneak-peek nutshell, it has to do with the improved quality of HDL (which we saw with one of the Pritikin Program papers) and the fact that higher trigs are typically a marker for insulin resistance, and when that’s absent, a heftier number probably isn’t pathological (which you can read more about in this paper yonder). We also have plenty examples of non-Western cultures that remain virtually free from heart disease, despite having triglycerides we’d consider too high and HDL we’d consider too low (hellooooo there Kitavans!)
As for the issue of Esselstyn’s statistically wobbly sample size (only 11 people who stuck with the diet through its 10-year follow-up): it was a fair criticism at the time, and one that’s been echoed by plenty of others. But it’s time to put that quibble to bed, preferably with enough sleeping pills so that it never again rouses. Why? It just so happens that in July of 2014, Esselstyn published a bigger, badder, bodacious-er study of 198 people instead of his original handful. The prescribed diet was the same oil-free, animal-food-free, whole foods regimen he’d been using for decades—with no confounding elements from exercise, meditation, psychosocial support, or yoga to be had. And the results were just as impressive—if not more so—than the ones he achieved in his earlier work:
- Among the 177 folks who stuck with the diet (for an average length of 3.7 years), there was only one cardiovascular event related to disease progression: a stroke. That’s a recurrent event rate of 0.6%.
- Among the 21 folks who strayed from the program, 13 had cardiac events. That’s a recurrent event rate of 62%.
- (The five other deaths in the adherent group included three cancers, one pulmonary embolus, and one case of pneumonia.)
For sure, there’s still plenty of stuff we could nitpick about this study (and his previous ones): there was no control group; the patients were abnormally motivated and self-selected (rather than reflective of the general heart-disease population, who might not be so inclined to give up steak forever); the study wasn’t randomized; and some level of self-fulfilling prophecy could’ve been at play, since the patients were told initially how awesome the diet was and how stupendously it was going to scrub out their arteries.
But even with those shortcomings, I’ll say it loud ‘n clear: I’m impressed. The study documents true heart disease arrest, and actual reversal for some. We don’t yet have any published studies of that sort on ketogenic, low-carb, or paleolithic diets (as far as I’ve seen!). And in my old age, I’ve come to appreciate the fact that real-world outcomes (i.e., whether or not someone keels over and dies) are more valuable than intermediate risk markers (like specific blood lipid ratios). It doesn’t matter that your health looked good on paper if you still end up in the ER!
And now, for an apology.
For the past few years (five? six? seven ate nine?), I’ve asserted that the success of plant-based diets is due to their whole-foodsness (eliminating processed junk, refined sugar, and refined flour), their low PUFA intake regardless of total fat (with the implication that higher non-PUFA fat consumption would be hunky dory), and the increase in other health-promoting behaviors that come with making a big change in the foods you eat (more exercise, less drinking and smoking, less couch-potatoism, etc.). I still think those things are relevant. But I now believe I dismissed the role of low total fat intake before I gave the data a fair and thorough analysis. This is a breach of the standards I hold myself to as a science blogger, which involve impartially examining all evidence before drawing conclusions.
So, I’d like to take this opportunity to say, HEY GUYS: I’m sorry.
To the aforementioned doctors: I’m sorry for jumping the gun with your research and being snarky when I reference you. I don’t always agree with the way you interpret your own work; I’m often unsettled by your debate tactics; I worry that the co-mingling of animal rights activism and nutritional research is toxic for remaining scientifically objective. But good heavens, I sure dismissed y’alls results before digging as deep as I should have—and in the process, missed out on some amazing opportunities to broaden my understanding of diet (and communicate those findings to my readers). Thanks for being on this planet and helping broken people heal.
To my readers: You guy are the best, seriously. Somehow you put up with these sporadic and unreasonably long blog posts and say nice things to me and wish me a happy birthday, sometimes with the inclusion of cat pictures, which is very wonderful. I don’t take your readership, your trust, or my quasi-position in the public eye lightly. And while I can’t guarantee that every word I write in this blog will be totally accurate, or that the ideas I present now and in the future will stand the test of time, I can promise that I strive to question my own biases just as rigorously as I question others’. That process of questioning will result in errors coming to light, which I see as a very good thing indeed: science (and its interpretation) should be self-correcting! Thanks for hanging in there with me. I’m honored for your readership.
Hopefully by now, some things have become clear:
- We can’t categorically blame low-fat, high-carb diets for heart disease and diabetes and obesity. We just can’t. NOT EVEN A LITTLE BIT. This needs to go away.
- We probably can’t even blame refined sugar for that stuff (at least not in isolation). Oh, the pain of shattering assumptions!
- We can’t ascribe the effects of low-fat, plant-based diets to their lack of animal products. Quite a few of the uber-low-fat studies here still allowed a fairly high animal protein intake, and still managed to whip people into diseaseless shape. Sorry, vegans!
- Ancel Keys did not invent low-fat.
- Ancel Keys did not invent low-fat.
- Once more, with feeling! Ancel Keys did not invent low-fat.
- I need to employ the “delete” button a little more rigorously. (Can you imagine how computer-crashy this blog post would be if I hadn’t split it into two parts?)
Admittedly, I’ve gone pretty easy on some studies in this post and—had I decided to devil’s-advocate from the other side—could’ve critiqued certain ones far more aggressively. But there’s a reason I didn’t go into BAD SCIENCE INCINERATOR MODE, and it’s not because I got bought off by the garbanzo bean industry (they’re gonna have to try a lot harder than 43 cents). For one, the sheer volume and consistency of the research here points to something very real, something totally non-under-the-rug-sweepable—and analyzing each individual study in search of holes and inadequacies wouldn’t change that fact. And secondly, there’s a whole universe of scientific mechanisms explaining why the diets discussed here work: the ability of dietary fat to reduce insulin sensitivity, the effect of different fats on tissue oxygenation and blood flow, the little-known ways that saturated fat can make LDL more likely to get incorporated into plaque, and all sorts of other fun stuff. That’s what the next post is about, so stay tuned!
In sum, there comes a point where it’s more of an intellectual stretch to rationalize something away than to accept that it may have merit. My friends, we’ve reached this point on the issue of low-fat diets. Let’s face it: they can actually do some good. And it’ll make a whole lot more sense why after you read Part 2!
Guess what? You made it to the end! Please remove of your pixel-dizzy eyes from the computer screen and get some fresh air. You freakin’ earned it!
ONE LAST THING. I want to give the stickiest, gooiest hug and eardrum-shattering shout-out to the amazing folks who donated to this blog over the course of the last year. You guys single-handedly made this post (and the one that’s coming next!) possible to finish, and your support allowed everything in here to reach a much wider audience than just the inanimate objects in my office-room. Thank you, thank you, thank you. If we meet in person, I’ve got a hug with your name on it; if we don’t, here’s a whole tray of Internet Bonus Biscuits! Mwah!


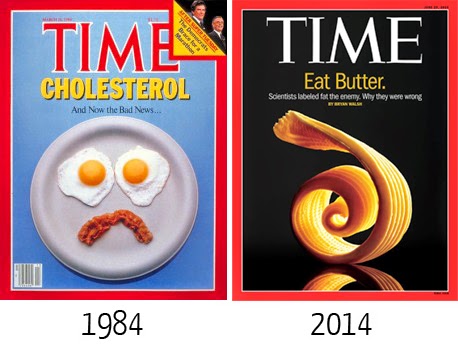

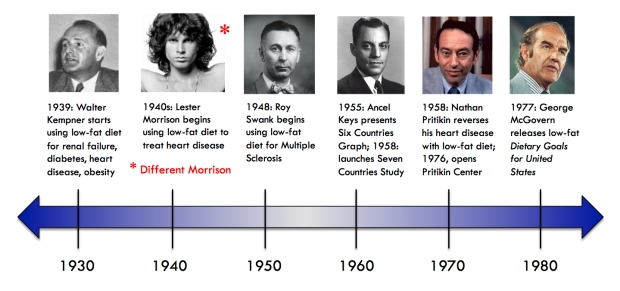

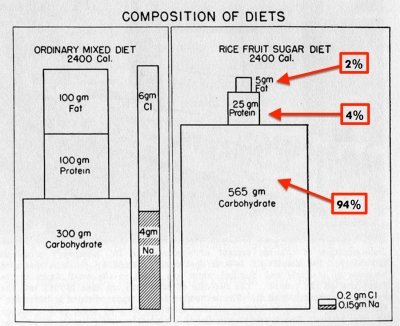
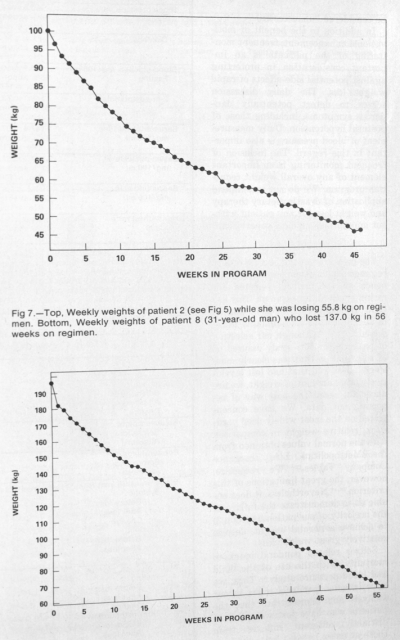
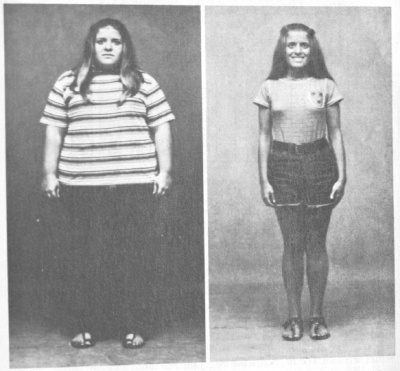
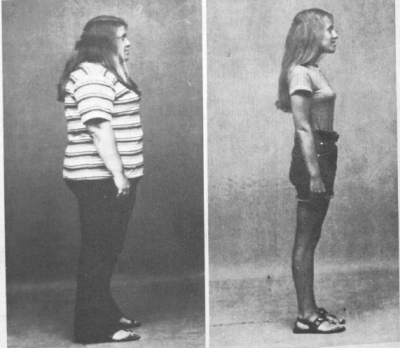
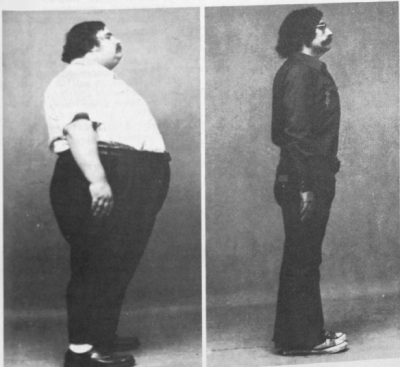


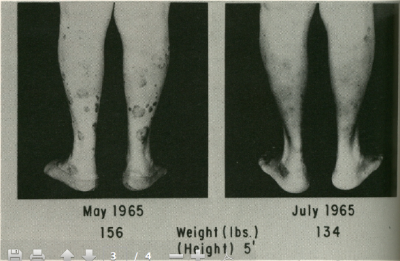
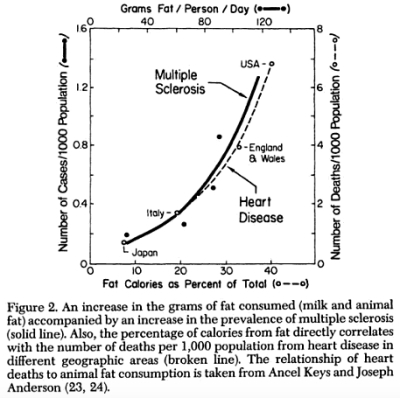
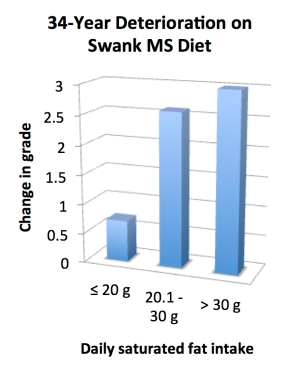

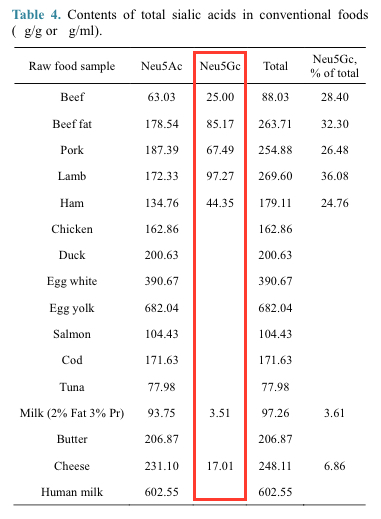

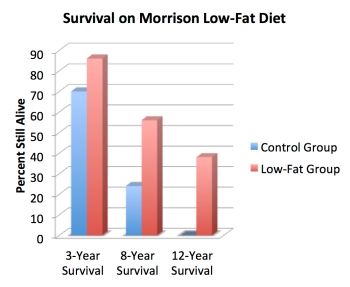
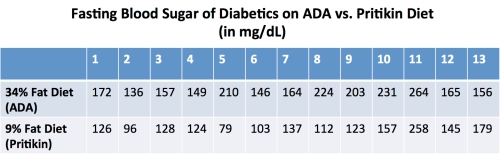
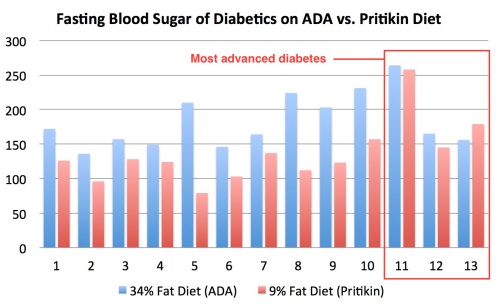

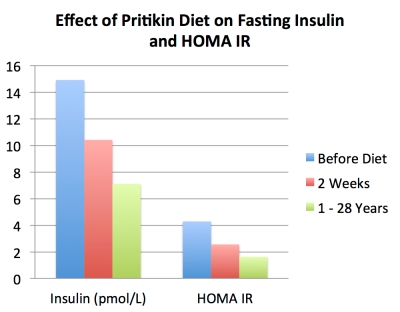
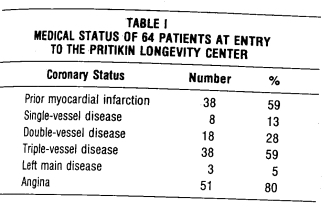
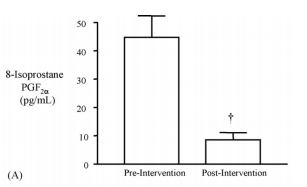
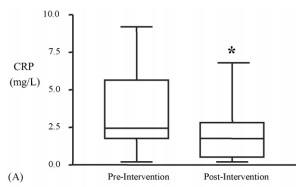

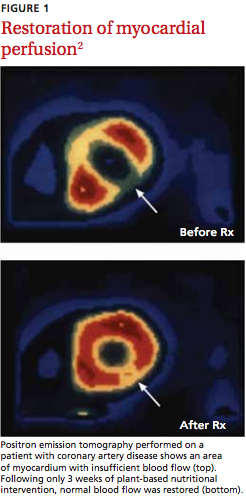
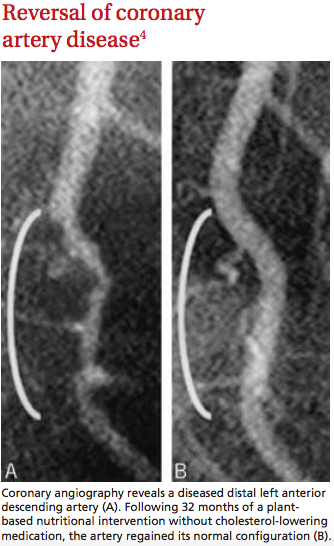

This is an excellent review of importance of fats, protein and carbohydrates on the prevention, treatment and reversal of major chronic diseases in the United States.
I highly recommend this post to traditional and integrative physicians, as well as their patients.
I just yesterday returned from a (Dr. John) “mcDougal 3-day weekend” that included Drs. Colin Campbell, Caldwell Esselstyn ( your grandpa wanna be, Denise), Michael Greger (author of How Not To Die), John McDougal, and several other like minded souls. Denise, these folks all follow a whole grain, plant based diet that you describe in your blog about Dr. Esselstyn and they are all strict vegans. Surely you know this so can you make the leap that yeah, there are more roads to Dublin, and a whole food plant based (WFPB) diet is one of them? Even if your analysis, for arguments sake, of The China Study is correct, Colin Campbell’s conclusion is to eat a WFPB diet, in his case a strict vegan diet. Can you declare that while his study had many faults yet his diet is in fact one road to Dublin?
Ps you should come to one of Dr. McDougals events, with a disguise, maybe, but an open mind, which your discussion in this blog in general, and about Dr. Esselstyn in particular, convince me you have in spades. I love to read your blog, even if I come from the dark side (vegan), because I want to read both sides of this issue, health.
Denise does not need a disguise as she has given her apology. She should come as she is. I applaud Denise for this superb article. There is a Turkish proverb that reads: “No matter how far you have gone on the wrong road, turn back.” Denise has done that and I give her kudos to admit some of the earlier faults and now become more of the writer she has become.
I make one exception. Dr. Keys wasn’t low fat, he was low saturated fat. He was a big proponent of olive oil and lived what he believed.
One more exception: “After getting into that sugary, starchy groove for a month, the dieters could start eating veggies again (which were initially nixed due to their sodium content”. It wasn’t the protein he wanted to limit in the first month that kept veggies out. It was the chloride that he wanted to keep under 200 mg per day. If you review the chart showing the Macro content of his diet you’ll see in the lower right hand column the long term requirements of his diet. It was 150 gm of sodium and 200 mg of chloride during the healing period. In the first 30 days he wanted also to keep the sodium to under 60 mg per day.
There is something in all of this. Of course not everyone does well on high fat, low carb, high carb or low fat. We are all unique individuals. For people with metabolic syndrome who fail to lose weight on any diet, the scientific evidence seems to report better results with low carb high fat. But I am sure there are exceptions to this. Only the individual person can decide what diet is best for them. I had metabolic syndrome and the very low carb high fat diet did wonders for me, I am now a normal sized person, my diabetes has improved immensely. But I cannot digest fat very well, no gallbladder. I have since moved to eating lots of fruit and very little animal products and am continuing to lose weight without any negative impact on my blood sugars. So there are two extremes and they both had a purpose for me, but at different times, and they both worked well. There is no reason to think that one philosophy of eating is the only way to eat forever. We change. I believe as long as your diet is not full of processed foods, the unhealthy fats, and sugars – either low fat or high fat could be appropriate.
OMG, I love that you wrote this post. I can’t wait to delve into this. But I first wanted to say how much I appreciate that you are on the scene. Finally, something that ties together the success of super low-fat plant-based diets and LCHF diets. Thank you Denise!!!!
You are missing one key point. Not all fats are bad. In fact, essential fats are essential for cell homeostasis and cannot be made by your body. They are called essential fatty acids. Your low fat diet will starve your body for these essential fats causing a host of symptoms and facilitate over 60 chronic diseases according to the National Academy of Science. Your program is sound for trans, saturated and monounsaturated fat. It is dangerous for ignoring the need for essential fat which can easily be verified.
And how much of these “essential fatty acids” does one need to get these alleged benefits? Nowhere have I seen it to be more than a couple of grams per day, which can covered by only a couple of eggs.
I wish the answer to your question was simple. But it isn’t because each person responds to nutritional inputs differently for a number of reasons. For example, genetics is a huge wild card in fatty acid metabolism. That is why the “one size fits all” numbers you quote are incorrect and dangerous for some people.
Thankfully there is a simple affordable pin prick serum mail-in test that will generate a comprehensive 3 page report of your complete fatty acid profile. Based on gas chromatography, it provides research-level accuracy that is certainly appropriate for consumer use. You can read about the technology here:
https://en.wikipedia.org/wiki/Gas_chromatography%E2%80%93mass_spectrometry
Exactly!
You obviously haven’t heard that there is no such thing as an essential fatty acid. Once again, scientific fact becomes scientific false. Maybe Denise will do a blog post on this.
I refer you to:
The National Academy of Sciences which links 60 chronic diseases to Omega 3 essential fatty acid deficiency.
The National Lipid Association that states the deficient Omega 3/6 ratio of the general public impacting all chronic diseases.
https://www.lipid.org/communications/reachmd/3942
The International Society for the Study of Fatty Acids and Lipids position papers
http://www.issfal.org/statements/pufa-recommendations
Behind each statement are hundreds of studies supporting essential fatty acids.
Please cites your studies that conclude “there is no such thing as essential fatty acids”.
https://pranarupa.wordpress.com/2012/12/25/pufa-because-this-wouldnt-be-a-ray-peat-themed-blog-without-at-least-one-post-on-pufa/
In 1938, a biochemist William Brown volunteered to go six months eating an extremely low-fat diet. He consumed a diet of defatted milk and cottage cheese, sucrose, potato starch, orange juice and some vitamin and mineral supplements. His blood lipids became more saturated and their concentrations of linoleic and arachidonic acids were cut in half. He experienced an absence of fatigue, his high blood pressure returned to normal, and migraines he had suffered from since childhood vanished, his metabolic rate increased and he lost weight, his respiratory quotient increased suggesting greater carbohydrate oxidation, lower respiratory quotients are associated with diabetes. The diet produced no deficiency, and likely corrected a PUFA excess. Six months on a specially prepared laboratory diet, no deficiency, if these fats are essential they’re essential in such tiny amounts that its almost meaningless to call them essential.
Click to access 511.full.pdf
EFFECTS OF PROLONGED USE OF EXTREMELY LOW-FAT DIET ON AN ADULT HUMAN SUBJECT
Our bodies can store a full winter’s worth of vitamin D in fatty tissues. Storage of six months worth of essential fatty acids would not be surprising.
1 day’s supply of Vitamin D3 is ~125ug. ∴180 days’ supply of Vitamin D3 is ~22.5mg.
1 day’s supply of EFAs is ~2g. ∴180 days’ supply of EFAs is ~360g. That’s a lot to store!
Hi, Certain conditions, related to fat assimilation, prevent vitamin D storage, as Dr Trevor Marshall discusses in one or more videos on YouTube.
Your cited review references classic studies and is very interesting in that, even though it dates to 1938, nothing in it is directly contradicted by the voluminous contemporary science I’ve read to date. But the INTERPRETATION of study results has changed greatly from yours. And there are some curious anomalies.
For starters, the title includes the phrase “prolonged use” of the extremely low fat diet and yet the study is only over a few months and the conclusions specifically warn, “it cannot be assumed that the human subject could subsist indefinitely on a diet completely devoid of the unsaturated fatty acids”.
All the observed good results you cite are due to reducing saturated fat in the subject diet, which is a really good thing on which we can all agree. But your interpretation that, “The diet produced no deficiency, and likely corrected a PUFA excess.” is dead wrong in light of new findings.
Here is what is happening. Some of the stored fats in the human body are the essential ones which it draws on when the subject does not consume them. That is why immediate deficiency symptoms did not occur. Yet your study reports serum level of essential fats dropped by almost HALF. So the subject was in significant deficiency of essential fats and his body made up for it by drawing down on stores it had accumulated.
A further complication is that the stored essential fat is mostly omega 6 because there is a huge amount of it in the modern diet. But a quicker major deficiency of omega 3 fat is inevitable. Since both level and ratio of these fats are deemed to play a role, reducing the excess omega 6 in fat stores is probably good as you claim. But the major problem is a GROSS DEFICIENCY of omega 3s. This is why the ISSFAL recommendation I cite posts no safe limit on omega 3 fat intake but a likely limit to omega 6 fat.
The easy solution for consumers is to do the simple serum test which embraces contemporary science to determine their essential fatty acid status and then be guided by test results.
,
I’m not discounting the deficiency in EFAs, as I’ve read about a rare case of it, but I just wonder how one, living a modern lifestyle would be unfortunate enough to develop such a deficiency. EFAs in all their forms are either added to our foods or naturally occur in fish and some plants. Even on an intentionally low PUFA diet like Peat’s it’s nearly impossible to go under 4g without compromising calories and nutrient density.
And by the way, out of pure ignorance, what would constitute a deficiency? I’m not sure if the FDA/ AMA has made recommendations regarding the minimum daily value. Would such a deficiency stem from intentional avoidance or a genetic/ physiological malfunction?
I also think the term “essential” is loaded with meaning. The public would understand essential as “necessary (for health) when in the original scientific terminology essential described fatty acids that, unlike cholesterol, cannot be produced by the body.
I think Ray Peat’s argument (and his proponents) raise the question: If our body cannot produce them on its own, we must be able to survive without them? (The human body is often programmed to be able to sustain itself.) I’m not settled on this since I can’t see a logical reason to avoid fatty (and tasty) things like avocados, fish and olive oil. But I don’t know… I’m trying it out!
“If our body cannot produce them on its own, we must be able to survive without them?”
Big fat(-insoluble) counter-example: vitamin C. Another: most of the B vitamins. Yet another: histidine. Being unable to synthesize something is a terrible marker for not needing it. More likely, as is the case with vitamin C, our ancestors were so used to getting enough of it in their diets (which were not completely herbivorous, as another of Denise’s posts points out) that they no longer needed genes for the enzymes to make it and were free to let the gene decay via mutation and save the protein synthesis.
“If our body cannot produce them on its own, we must be able to survive without them?”
By that logic, we don’t need to eat or drink anything because our bodies can magically produce whatever they need to survive. Hallelujah!
Forsythia, salbers12 is right, omegas 6 and 3 ARE essential. Check out Susan Allport’s book “The Queen of Fats” for a great case example of someone suffering from too little Omega-3
The proof is in the pudding. My experience on a low-fat diet for 1.5 years gave me low mental energy and bad memory. I’m not sure William Brown ‘s 6 months study is long enough to override the benefits of his previous diet (which isn’t explicitly stated). I did not eat EPA and DHA before this diet so I suppose a low-fat diet made the symptoms of this nutritional deficiency worse.
A low-fat meal doesn’t have the same satiety feeling as a medium-fat meal, even during intermittent fasting meals in which I ate a great deal of low fat food. Prolonged hunger sensations to me are a warning sign that my body desperately needs fat.
It may be different to others but I sure as hell won’t go back to a low-fat diet.
It is actually very difficult to avoid “essential fats”. You can go without nuts and seeds and olives and avocado, but all fruit and vegetables have some pufa!
Your ignorance is dangerous. All pufa are not essential. It’s almost impossible to avoid the w6 essential fatty acid, linoleic acid found in seed oils, but the w3 essential fatty acids – linolenic acid or the elongated versions EPA and DHA – are simply not found in the diets of 25% of Americans according to William Lands. Since the same enzymes process both families and the prostaglandin progeny of w6 fatty acids are overwhelmingly inflammatory, while the prostaglandins derived from w3 fatty acids are anti-inflammatory, we are more or less likely to suffer chronic inflammation according to the w6/w3 ratio of our diets. Japan wins, we lose. “The potential attributable burden of disease ranged from 20.8% (all-cause mortality in men) to 99.9% (bipolar disorder)” https://www.ncbi.nlm.nih.gov/pubmed/16841858. Read and salve your ignorance.
That paper assumes that differences in dietary percentages of “essential” fatty acids are responsible for mortality differences between Japan and the US!
It also assumes that the ratio of n6 to n3 should be at lower.
It then makes recommendations based on those assumptions.
The best advice from that paper is to consume fewer n6 fats.
http://www.bmj.com/content/346/bmj.e8707 is an RCT which found raising w6 increased both all cause mortality and heart death quite dramatically
https://circ.ahajournals.org/content/99/6/779.full.pdf is an RCT which showed that raising w3 halved heart deaths – I believe this is the most successful dietary intervention ever studied
An excellent citation that agrees with my extensive reading. I’m not entirely clear on several statements that may be worth exploring. The National Academy of Science now links over 60 chronic diseases to omega 3 deficiency. So it seems a pretty safe correlation whether it is justified by this paper or not. The the optimal cellular-level target appears to be equal amounts of LC omega 3 & 6 FA. How best to achieve this is the question? Two serum measurements that bear on this are the LEVEL of LC omega 3 and the RATIO of LC omega 3s to 6s. Both need to be addressed. For example, if the ideal ratio of 1 to 1 is achieved but the level of omega 3s is too low, there is not enough present for optimal cellular function. Additionally, if the optimum level of LC omega 3s is present but the ratio is too high the the omega 6s swamp cell receptors so that the 3s are not absorbed. The best plan is a personal blood test and be guided accordingly.
I think you’ve nailed it!
I have begun sprinkling flax seeds and chia seeds, both excellent sources of 3’s, on one or two of my meals each day. I’ve cut out all animal products so have reduced my 6’s. Wanna make sure you actually use the stuff and don’t leave it in a container in the fridge? Go to the store ( I found it at Bed Bath and Beyond) little containers that you put the seeds in and are really easy to access and pour. Makes a big difference in how readily you use the stuff. I do it every day without thinking now. Experiment with different containers until you find the easiest. I did.
The root source of DHA is algae: fish eat the algae and the DHA climbs up the food chain. The ALA that is in plants CAN be converted to DHA, but some people do it better than others. Seems to have to do with your genetics … people who lived inland have better ability to convert plant omega-3’s into the longer ones that people need. Anyway, if one does not want to eat fish for whatever reason, the next-best source is algae. supplements.
“By now, everyone has heard that omega 3s are good for your brain. However, omega 3 is a generic name for a family of fats. Docosahexaenoic acid (DHA), a specific type of omega 3 found in fish, krill and algae, is what your brain is made from. While humans have the ability to convert the type of omega 3 in walnuts and seeds into DHA, new research has shown that the degree to which these omega 3s are converted is dictated by your genes.”
http://thatnutritiongirl.com/tag/omega-3-2/
I think this is particularly important for vegan women that are planning to have children. The development of the brain is very much dependent on the amount of DHA in the mother … if the mother is not genetically able to convert flax seeds to DHA, the baby will suffer.
Um, Jonathan, YOU need to learn what you’re talking about before you start shooting off your arrogant piehole. First, learn what “essential” means in the context of nutrition. An essential nutrient is a nutrient required for normal human body function that the bod either can’t synthesize at all, or not enough for good health. The 18C omega fats linoleic acid and alpha-linolenic acid ARE indeed essential–we have to ingest them. As far as longer-chains, EPA and DHA, we can make them from ALA, but conversion rates are low enough (~8–21% to EPA, 0–9% to DHA) as to make them conditionally essential. You are correct that we can easily obtain w6 from our diet, but we don’t really know the minimum levels for w3. Nor the ideal 6:3 ratios: 2:1? 4:1? Read that “Queen of Fats” book and you’ll see a test case that went for years without any w3 before starting to suffer overt systems. Some people eating ancestral diets, e.g. the Pima Indians in Arizona and their Tarahumara cousins in Chihuahua State, were plenty healthy before Euro intervention even though these inland desert and arid land dwellers ate diets rich in beans and corn and got far less EPA and DHA than the Japanese, Inuit, and other peoples living near cold-water seas rich in high-w3 marine life. Leafy greens do include small levels of ALA because they need that w3 in the thylakoids for photosynthesis so Richiebogie is at least partially correct when he says “… vegetables have some pufa.” As far as that PubMed study you tout, that’s just one more of the zillions of meta-studies out there, completely correlative, nothing clinical about it, confirming nothing at all. The study leads even make that clear, putting “estimations” in the title. Correlation does not imply causation. Get off your high horse.
Umm, feelings run high! Every word you say is true. I chose Lands’s pdf because it was to hand and because it gives a good overview. However …
http://www.bmj.com/content/346/bmj.e8707 is an RCT which found raising w6 increased both all cause mortality and heart death quite dramatically
https://circ.ahajournals.org/content/99/6/779.full.pdf is an RCT which showed that raising w3 halved heart deaths – I believe this is the most successful dietary intervention ever studied
This one cut all-cause mortality too. So we have RCTs in which more w6 increased all-cause mortality, and more w3 reduced all-cause mortality. Yes, they’re secondary prevention trials, and, yes, Sydney probably ate more trans fats but this is the best data I can find to justify my dietary choices. My coronary artery calcium score is zero after 15 years of lowcarb (because I’m Type I, not because of dietary convictions), taking fish oil and avoiding seed oils.
Had I been lulled into complacency by advice like richiebogie’s “It is actually very difficult to avoid “essential fats””, I think it likely I’d now have rampant atherosclerosis. Which is why I say it’s dangerous bollocks.
Jonathon, is it this from richiebogie you reacted to?:
“It is actually very difficult to avoid “essential fats”. You can go without nuts and seeds and olives and avocado, but all fruit and vegetables have some pufa!”
If so, I think you may have read too much into his comments. I don’t see him advocating using seed oils or other w6 bombs.
btw, I interpret this as him saying you get pufa in a great many foods. Do you think he’s wrong?
In any event, you should have sought clarification from him before you adopted your high and arrogant tone. Just saying.
He said its very difficult to avoid “essential fats”, no explanation, no references – seemed pretty arrogant to me – perhaps he can clarify that?
All I know is that doctors have been selling me variations on the theme for 15 years and I’m hale and hearty while one of them retired prematurely with Parkinson’s, and a second died with dementia blind from ARMD, all conditions for which lchf has been found to help. Had I taken their advice, I’d probably be with them now.
When people come on cocksure with what I know to be untrue, then I feel I must oppose them since this may help people who find themselves in the position I found myself in 15 years ago, fighting the conventional medical wisdom – which is turning out to be more and more wrong.
If I come off as arrogant, then maybe it’s because I’ve got something to be arrogant about, like being alive
Jonathan, again, what *exactly* did Richiebogie you took such issue with? Please quote it, thanks.
He wrote: “It is actually very difficult to avoid ‘essential fats'”. It’s not true. Why do you ask?
Jonathan, I do mainly what you’re doing, only I don’t get pufa (or anything else) through supps, just through food (mainly canned salmon and sardines). I try to keep ALL pufas low because pufa is the most oxidizable of the fats, esp w3, I init did the spreadsheet work on those to make sure I was getting enough w3 (Mary Enig of “Know Your Fats” gives 3–4g/day), and obviously no seed/nut oils and limit fatty grain-fed meats.
About the RCTs. The first one you cite, the Sydney Diet Heart Study, doesn’t test w3 at all, merely subs w6 with SFA. The Lyon Diet Heart Study does look at w6/w3 balances, but where’s the sample rate? Can’t seem to find it, maybe just overlooking it.
Finally, your CA calcium score, Vit A/Vit D/Vit K balances can also greatly affect that. Those fat-solubles work together to transport serum ca to bone.
Yes! I think your strategy has the best chance of lengthening healthspan.
“Saturated fat protected the livers of rats given alcohol, but replacing the saturated fat with corn oil resulted in oxidative stress and severe liver damage (Ronis 2004). Moreover, there’s a robust inverse association between saturated fat intake and ischemic stroke in both American (Gillman 1997) and Japanese men (Yamagishi 2010) – the more saturated fat eaten, the less the likelihood of a stroke” from an essay I wrote.
Ramsden’s meta-analysis concludes “Advice to specifically increase n-6 PUFA intake, based on mixed n-3/n-6 RCT data, is unlikely to provide the intended benefits, and may actually increase the risks of CHD and death” http://www.ncbi.nlm.nih.gov/pubmed/21118617
I take the fish oil because I tested low in cell-wall w3’s, thought to be a diabetic trait where w3’s are burned for energy preferentially over glucose when insulin is high, causing insulin resistance. I do take K2, but I started after I got the zero calcium score.
As you point out, the RCT evidence is woefully inadequate but what the hell we’ve got to eat something!
Therese Dolacek found among about 6,000 middle-aged men with lousy risk factors for heart disease in the MRFIT Usual Care group that 20% of them reported zero intake of conditionally-essential w3 fatty acids. She went on to say “Analysis of the combined fatty acids predominantly found in fish … demonstrated significant inverse associations with CHD, CVD, and all cause mortality groups but not for cancers … The benefit … [at] 664 mg/day … [was] … 40, 41, and 24% lower [incidence respectively when compared to zero intake]” http://tinyurl.com/p7jt9fh
So I’d amend your gnomic utterance to: “It’s actually very difficult to avoid eating the pattern of ‘essential fats’ associated with heart health and less death if you eat fish”
Pardon me for being a little insane on this topic, it’s the legacy of my 30-year fight against the conventional medical wisdom that diabetics should eat lfhc and avoid saturated fat. The way you put it implies you can’t help getting your “essential fats”, don’t worry about them – dangerously misguided advice IMO
This is the medical wisdom my conventional MD handed me in 2007 when I was diagnosed Type 2 diabetic. It is anything but “lfhc and avoid saturated fat”.
Click to access CountingCarbandMeal_EG.pdf
After two weeks of following this protocol my fasting blood glucose dropped from 200 to 100 without any other medication.
Any doctor that would recommend lfhc to treat diabetes with lfhc is insane, certainly not conventional by 2007 Illinois standards.
Wow! They advocate more than 50% carb calories, what were you eating before?? Dr Richard Bernstein suggests 6% as an upper limit of carb calories. Allick 2004 points out that such a low carb intake depletes liver glycogen by about half which prevents the liver from raising the blood sugar via glycogenolysis, allowing the diabetic to have normal fasting blood sugar http://www.ncbi.nlm.nih.gov/pubmed/15579777. Being Type I, I have to keep to that level to prevent high fasting blood sugars – you must have beta cells producing enough insulin to get away with such a high carb intake
There’s no advocacy of carbs at any level (you don’t have to use the sample meals), and you could construct it VLC if you so desired. It’s biased against high glycemic carbs, and set up so typical SAD dieters will use it.
My problems were overeating high glycemic carbs and fats and being sedentary. Specifically I was eating huge amounts of frosted mini wheats and raisin bran. I suppose that my carbs were 70% of total calories diabetic at 2500 total calories per day and no exercise, dropped to 40% of total calories at 1500 total calories per day and 350 calories per day exercise with the carb exchange system. After I’d controlled blood sugar and lost 25 lbs, I increased the exercise to 700 calories per day, the food to 1800 calories per day and started putting the high glycemics back in. I was able to maintain a 2 lb/week weight loss rate for 6 months doing this, stopping it after 50 lbs lost. Since then I’ve continued to increase the exercise. I aim for Cordain’s 1000 calorie per day historic Paleo exercise by walking and biking. I eat to maintain weight, typically 2300-2500 calories per day, on ca 50% carb, 35% fat, 15% protein, and have stayed at target weight for 8 years.
VLC Paleos have called me asymptomatic in the past. However, I couldn’t eat this way without all the exercise or if I hadn’t lost the weight. I’m certain that I stopped what I was doing, my trigs would go from 35 back well above 100, my blood sugar would go from under 100 back to 200 fasting, my CRP from below 6 back to 8, and my HDL down from 70 to 30.
thhq, what is the “non-inflammatory” range for your CRP measure? 1–3?
My Dr. wanted it under 6.
Sent from my iPhone
>
My Dr. recommended getting CRP below 6, and the test shows a healthy range 4.8%-5.6%, so I don’t think this is the high sensitivity test. I started at 8.2% in 2/07, and by 8/07 was below 6% (after 6 months of the carb counting and 50 lbs weight loss). I’ve been at that level until the last test in 2/14. I moved in 2014 and my current Dr. doesn’t run it.
Wow, that’s impressive! Congratulations!
Thhq, I agree with Jonathan here. If I stayed on this high-carb diet that Novo Nordisk proposes, I’d be injecting insulin by now. And I ask you the same question as Jonathan: What percent carb diet did you eat before?
Bear in mind your BG levels don’t tell the whole story. With such a diet, you may have near-normal BGs but chronically high serum insulin levels, esp if you have insulin resistance. Chronically high serum insulin may also harm you in various ways, e.g. promote growth of amyloid plaque in the brain that lays the groundwork for Alzheimer’s. E.g. the same enzyme that dismantles insulin also dismantles the amyloid plaque, but works on insulin first. So chronically high insulin may mean never enough enzyme left over to break down the plaque. You can get an inkling of your insulin levels with the C-peptide test, but to really put a fine point on it, you need the euglycemic clamp, and expensive and involved test not regularly done.
This proposes another mechanism for how chronically high insulin levels promotes brain plaque development:
http://www.medicaldaily.com/alzheimers-may-be-late-stage-type-2-diabetes-relationship-between-insulin-amyloid-plaques-and-enzyme
Wow, just WOW. Talk about cherry picking, dismissing anything that can, god forbid, brake the fabric of the little pattern we are trying to build, and leap frog from diet to MS with several other subjects in between to overcome reading sharpness with a totum revolutum devoid of unbiasedness.
The agglutination of causalities without a minimal effort to look beyond the obvious first impression is flabbergasting, The dismissal with the wave of a hand of historical data is insulting.
I will be honest, I did not read the very few last paragraph, cause though you write very well, your style is, simply put, chaotic, you are very capable of giving a headache to an aspirin.
But with that said, the article is pseudo science, yes it is. It’s obvious that you don’t have a scientific background, you don’t challenge the methodology, you don’t provide articles where the testing hypothesis has being duplicated following the same program, and I don’t mean 10 or 15, but hundredths, that is how peer review works. You do make a half hearted attempt to play Devil´s Advocate, but excuse me if I am not overly convinced or satisfied by it.
But let me address the first shortcoming. The P. diet, is a diet which is first and foremost high in fiber, then high in carbo and almost lacking fat and animal protein. It requires strict adherence to it for life, AND relies heavily on exercise. Of course you gonna get the improved body, of course you gonna get rid of type 2 diabetes, you are exercising. You just barely brushed aside the whole core of the diet like if it were an innocent passer jaywalking onto your fine article. Then you don’t address the number of maladies caused by a diet deprived of fat or with very low fat intakes, liver cancer, brain malfunction, cell membrane integrity, hormonal imbalance, etc. All of that without going into the trivial detail that not all fats are created equal, and the same goes for carbohydrates.
You also take as example people from indigenous tribes, as role models for the diet benefits, since they don’t have heart disease, well yeah, but they suffered from severe malnutrition, anemia, are susceptible to viral infection and have a high incidence of certain types of tumors associated with low fat and animal protein intakes. The bantus don’t have that diet by choice, they have it by geography, and by the way, their infant mortality is enormous, cuz somewhat carbos are not sufficient to provide synthesis of mother’s milk.
So stop pandering your neo sophism, reading nutrition books and science papers is not a magic wand to turn you into a scientist, or an expert on the matter. I read many books in quantum physics and relativistic theory, it does make me a physics expert either, because although I have the math background to understand the theory, I don’t have enough of it to propose hypothesis using a few cherry picked articles.
Regards
Hilarious. The high carb cheerleaders sounded exactly like you when the China Study article was released here!
3 paragraphs on how she’s not a “scientist” (even though she never claims to be one) and then more condescending babble about nothing.
Get a life, dude.
Please do more research into efa’s. Especially R. Peat’s. They are NOT essential. I feel making a statement like that without really researching will harm and may kill a lot of people.
At last- -!! But I’m not going to read this tonight- – I shall waken in the morning but stay in bed and read and digest until I’ve ‘got it’. I’ve been wondering when it was going to appear, ever since you prematurely hit the ‘Publish’ button some months ago. Good night, from the South of Africa
1. Thank you / this is great / you’re awesome.
2. I have absolutely no idea what to ever eat anymore…..like, ever.
3. Do you happen to have some sort of magical machine that gives you more time in the day than the rest of us?!?!?!?
4. Thank you!
Eric
Eric, my reaction exactly (and I’ve written a diet book!). Thanks, Denise!
Brian
P.S. I would add a 3b: I wish I also had a time machine to do a few N=1 trials, repeated with washout periods, of high-fat, low-fat (really low-fat), and a couple variants of in-the-middle-fat diets.
I was a Registered Dietitian working in Marin County, California, at a very large cardiology group when low fat diets were popular. I am still an advocate of low fat eating and controlled, careful fat eating–I have not fallen for the “high fat, high protein” way of eating. (I see too many impaired renal function patients and colon/breast/prostate cancer patients to feel excess protein and fat are good for people.)
What I find “hilarious” about the movement to blame “carbs for the obesity epidemic and the explosion of Type 2 diabetes” is that for that statement to be true, EVERYONE in the population would have needed to be eating a very low fat, very high carbohydrate diet–all the time for that to happen (if it was even true.) The truth was (and is) that it was very difficult for people to eat a very low fat diet–AND VERY FEW PEOPLE ACTUALLY DID IT–even those who were cardiac patients. It has always struck me as ironic that no one ever really checked to see if people were really eating low fat and high carbohydrate diets before they were blamed for the health disasters. The association was too “theoretical” without sufficient data to back it up. People self-identified with a low fat diet and would say they ate that way–but that did not mean they ate that way all the time.
Keep up the good work–you are a brave soul. I envy your dedication.
One of the good responses. Thanks for your story.
Like Denise was saying, the still are whole populations who eat very high fat and have very little cardiovascular disease – the Maasai, the Eskimo, some populations in China, etc. An idea is that it probably has to do with other factors, too – like level of physical activity and place of living (the Eskimo live in very cold weather most of the time, so fat is probably necessary for them anyways). The thing is, nobody even thinks of the fact that air is a nutrient too – so maybe, if you breath clean air, you can eat more fat and still not get sick – or something of the sort. Since most of the diseases are plurifactorial, fat cannot be the only one causing – or curing – heart disease…
Not only that, but there is still no proof that dietary fat even causes heart disease in the first place- (or the corollary, that low fat “cures” heart disease). If any of these diets DO cure heart disease, then it could likely be due to any number of factors, not the low fat element. Based on all I’ve read, it still seems a bit unclear exactly what causes heart problems. There are a lot of theories out there, but nothing has been scientifically proven. And there are so many “paradoxes” as well……
Ditto.
To be clear, impaired renal function does impair your ability to get rid of protein that you aren’t using as protein, and all of those cancers are an insulin thing (so any diet that reduces insulin will help with them).
But there’s a reason even I, lay keto ideologue of the highest order, hate overdoing protein and endeavor to frontload an energy nutrient (in my case fat for the mood stability effects, though I am considering upping the carbs a bit from fruit and rice because of the excellent work the fire in a bottle guy has done with saturated fat, as well as the fact that I’m not really holding onto my self-perception of fatness very well – I’m getting “mentally emaciated”). And that’s that a high protein diet is toxic if you do end up going too high, even without impaired renal function – there’s this thing called rabbit starvation.
Denise, YOU ARE MY HERO!!! #thatisall
Chapeau!
Very detailed post, must have been a lot of work! I know it might seem mysterious or surprising to some why low fat vegan works so well. Our bodies are natural starchivores (low fat plant based), just Google ‘omnivore vs frugivore’ and look at the chart – from teeth, to stomach, intestines, etc. Even Denise does a low fat diet. So it makes perfect sense when we eat our natural human diet why our bodies would perform so well, reverse heart disease, etc. But humans are uniquely able to adapt to lack of carbs by going into ketosis – an emergency state during starvation or illness. When no glucose is available (emergency state) our body switches to using fat to survive. Not something we want to do on a regular basis in a healthy state. We avoid all the nutrients, fiber and phytochemicals that plants have to offer. It’s fairly simple to understand.
I know people here probably don’t accept the china study links between protein and cancer, so here are 5 other ways meat causes cancer that you may not have heard about https://www.youtube.com/watch?v=PlhJU57KUd for example estrogen, IGF-1, hydrogen sulfide, Neu5Gc. Sure we can scavenge some meat for calories and survival but it’s not going to help us thrive and live to 100+. People jumped all over your china study critique because they like to hear good things about their bad habits.
The success of LCHF is usually based on short term weight loss (assuming caloric deficit and includes loss from glycogen stores and associated water depletion) which creates associated reductions in say blood pressure, but it’s not able to reverse heart disease such as with Dr. Esselstyn’s studies. They have bad breath, constipation and revert to caffeine or laxatives to stimulate the bowels. Check out the longest living populations in Okinawa and 7th day adventists they blow away the masai and eskimos (why we use small isolated tribal populations who didn’t live as long and were shown to have atherosclerosis is a question for another day). 🙂
Keep up the great work!
That’s peculiar since my bowel works much better when I stop eating fiber and eat only meat.
My system also runs much more smoothly when I reduce my fiber intake. In fact, I can’t do a high carb diet anymore, since I am intolerant to so many of the foods; there would be nothing left for me to eat.
And- in response to Will- I eat LCHF, but I am underweight, and therefore am not even trying to lose weight. But I’ve seen massive improvements in my health since I started eating this way about 4 years ago. I had pretty massive health issues when I ate a plant based, low fat diet; (I also went through a phase of eating a very low fat diet, of exactly the kind that Denise describes). So my first point is that the benefits of LCHF- for many of us, anyway- are NOT solely due to “temporary weight loss”. My second point is that no one particular diet is the “absolute correct one” for all people.
I lost 150+ pounds on LCHF, so I’ll assure it was not water weight alone. I have excellent bowel function. I think you miss her point, BOTH diets seem to work. Some people do well on one or the other, if vegan suits you great, go for it, but stop spreading the lie that LCHF doesn’t work for people like me, it’s simply not true.
Exactly. I’m pretty sure Denise is not on a diet with less than 10% of calories from fat, either.
Exactly
Vegan nonsense at its finest. Posting that in the comment section of a blog that clearly states how BOTH diets are perfectly fine show how narrow-minded you guys are. Shaking head really
Then there is the notion that neither diet is ideal. And that swampland is only swampland when carbs and fats are combined in the one meal.
My bet is Denise will have something to say in terms of following both diets, but not a mix of the two.
We will see…
If you cannot have roast potatoes with your roast then please kill me now!
“They have bad breath, constipation and revert to caffeine or laxatives to stimulate the bowels.”
Is that so? I don’t know any LCHF eaters who have had bowel problems. I assume you must have access to a large database to make this assertion with such confidence.
Many low-carbers who convert from the SAD find they actually consume more vegetables than before. Often their fiber intake increases substantially.
I’m unaware of studies showing that LCHF is incapable of reversing heart disease. There are certainly studies that shows it reverses metabolic markers “associated” with heart disease, but these are questionable indicators. LCHF hasn’t been studied in depth, and in most cases the LCHF diets that have been trialed are in the “swampland” Denise has described.
I think Denise is presenting objective analysis. And she didn’t prove anything regarding the superiority of low-fat diets (or try to), She is pointing out there is “magic” at both ends of the spectrum.
And I might add that the “magic zone” at the LCHF end is far, far larger.
I disagree. I run a Facebook group with LCHFers and that is a huge complaint, either they have very loose stools, or constipation. Either way, it is a common complaint. I have myself had extremely loose and often stools on LCHF. I eat higher carb, and the problem instantly disappears. In both diets, I am eating a lot of veggies/starches. The only difference is the amount of sugar and fat.
Will . whey you aré in Ketosis you do not avoid all the nutrients because you can still eat as much as vegetables you want with all the micronutrients and phitochemicals
Will, you simply fail to offer rigorous evidence for the claims you make. Nor can you. And your vid link is broken.
What do you consider “short term”? I’ve lost 65 pounds in the last six months (30 pounds disappeared in the first 30 days) eating LCHF. I am no longer pre-diabetic, my LDL is down, my VLDL is way down, my HDL is up, etc, etc…. Oh, and I’m not friggen hungry all the time, which for a weight loss diet is VERY important to insure compliance. To drive that last point home, I even fast two days a week. That’s how “not hungry” this diet makes me feel. BTW, I had never been on a diet before more than two or three days in my entire life, and I had put off doing this diet on my doctors advice, as I didn’t want to have the severe hunger pains I had on my three day diet stint in high school 33 years ago.
If your doing LCHF and have constipation, then your not doing the diet correctly (hint, your eating too much protein, and not enough low starch vegetables & fiber). The most common mistake people make on this diet is thinking that it is high fat AND high protein diet (it’s not). It is a high fat, very low carbohydrate, & MODERATE protein diet. Too much protein and two things happen. First you stop loosing weight, because your body tries to turn the excess protein into sugar. The other thing that happens, and yet another reason you stop losing weight, is that ya can’t poop anymore 8^].
I DO think that the author may be onto something though, when speaking about the “magic” that happens on the extremes of fat & carbohydrate dietary intake levels, and the macro-nutrient swamp that is the Standard American Diet.
I watched a Horizon (BBC’s version of NOVA) episode on weight loss and diets a few months ago, where they had taken two identical twins who were about the same weight, and fed them different diets. One was high fat & protein, almost no carbs. While the other was almost all Carbs, lowerish fat, minimum protein. What was interesting were the results. Both gained a little bit of weight, because neither was following a truly LCHF or VLF diet (too much processed foods, etc). Here’s the interesting part… Although allowed to eat as much as they wanted, both tended to eat about the same amount of calories. Hmmmm…..
Near the end of the program, another scientist shared the results of a feeding study he did on 3 sets of rats. The 1st set of rats he fed a high carb very low fat diet. The 2nd set he fed a high fat very low carb diet. Neither of those two sets of rats gained any significant amount of weight, or had any significant disease problems. The 3rd set of rats gained weight like crazy, and were having various health problems, and way higher mortality rates… He fed the 3rd set of rats “cheesecake” exclusively. The cheesecake would be akin to a Standard American Diet (SAD). The scientist’s theory of why this was, is because the 3rd set of rats ate WAY more calories than the other two sets of rats.
His example of why goes like this: Take a bowl of heavy cream, a spoon, and start eating. You’ll soon quit, as it won’t take much to have your fill. Now (sometime later), do the same thing, but this time with a bowl of sugar. Again, it won’t take long for you to stop eating spoonfuls of sugar. NOW (again, sometime later), pour the bowl of sugar into the bowl of heavy cream, mix them, and get out your spoon again. This time you’ll most likely consume the entire bowl… Why? Because when you add sugar and fat together at a certain ratio (something not found often in nature), it kind of turns off your brain’s satiety switch, and hence causes you to over eat. BTW, sugar+cream+cold=ice cream…. At a certain ratio of sweetness to fat, we can’t help but want to have more.
They tested this hypothesis by giving out free donuts to random strangers. Of the 3 types of donuts they gave out (glazed, chocolate frosting, & powdered sugar), one type was consistently chosen the most. It was the glazed doughnut, as it has the same sugar to fat ratio as ice cream does.
Now that’s food for thought ;-).
Please refer to nourishingtraditions dot com on Okinawan and 7th day Adventist diets. Buettner gave lots of disinformation. Okinawans fry their food in lard. They eat more pork than other Japanese. Unfortunately I can’t open the link which claims 12% of their diet calories is fat.
Not all 7th day Adventist are vegans. In fact 7D vegans have more cancer and certain diseases than 7D non vegans. Again refer to nourishingtraditions. Many blue zone diets are found to feature meat and animal fat, contrary to popular notions.
@Z – “Many blue zone diets are found to feature meat and animal fat, contrary to popular notions.”
That is correct. I extensively showed the evidence in an article I wrote. I included every source of info I could find over years of research, including recent updates.
The thing that’s missing in this whole discussion is protein. Of the ways we get calories, there’s pretty good evidence that protein is a better plan than either fat or carbohydrates. Indeed, one could argue that the success of low-carb diets is largely due to the fact that they are high-protein diets: Atkins’s own argument was that the fat was in the diet to make you less hungry, not because it was inherently good for you. Weightlifters and other health types have been advocating high-protein diets for years, and having generally good health with them.
I think you are doing a disservice to your readers if you paint the diet question as “high fat vs. high carbs.” The most credible evidence I’ve seen favors diets featuring lots of protein, plenty of fruits and vegetables, enough fat to reduce food cravings, small amounts of sugar and simple carbohydrates, and less total food intake. I’m guessing you wouldn’t find any of that controversial?
PO8:
Sorry but a high (animal) protein diet is a disaster for someone like me who has high uric acid levels. I eat way less meat than most people and I can bring on a gout attack at will simply by upping my protein intake from fish, beef, poultry and pork. Through trial and error I do best on low fat. Vegetable protein doesn’t seem to have any effect on my uric acid/gout nor does dairy and eggs (as demonstrated in studies).
The human liver simply cannot process enough protein to meet our energy needs. For that reason, we need to get more than half of our calories from some combination of carbohydrate and fat. This article suggests it should be one or the other, but not both.
People keep saying the low carbohydrate diet is high protein. A properly formulated low carbohydrate diet supposed to be moderate protein, high fat and very low carb. This is like Atkins and what the other low carb gurus out there say it should be moderate protein.
So basically if you had listened to me you’d have been right all along.
lol
Fascinating! Excellent work. I’ve been checking your website for months looking for updates. I can only imagine the amount of research and work that went into writing this. Can’t wait for part 2 and wondering if genetics will help make sense of it all.
I will be at the Anaheim conference in November. Looking forward to meeting you there.
Am I really the first commenter or has it been so long in reading that a page refresh would show a different truth?
Anyway, it’s post like this that show why I read your work and trust you. I don’t have a lot of time left over in life to read about nutrition science. Thank goodness for you thorough review and overall entertaining presentation. Can’t wait until part 2!
Wonderful and amazing article. What I wonder is what you ate yesterday.
“… we could nitpick about [Esselstyn’s studies]: … the patients were abnormally motivated and self-selected (rather than reflective of the general heart-disease population, who might not be so inclined to give up steak forever)”
These issues may be relevant to the prospects for widespread adoption of the dietary regimen, but they do not confound the results of the studies.
One of the largest impediments to widespread adoption is the conviction of medical professionals that it’s impossible for almost all patients to change the way they eat.
Michael Greger (nutritionfacts.org) analogizes thus, mimicking a hypothetical M.D. saying, several decades ago something like, “I’d try harder to get my patients to quit smoking, but I know how they love it so!”
but it is so much fun running with scissors while chewing arsenic candy!
Wow! It is an incredibly good read, so far only read until the end of the Walter Kempner – Rice diet part, its great results was definitely what made me question the low carb ideologies. Now I think its effectiveness is due to its ability to increase the metabolic rate, by completely eliminating PUFA and fats, along with amino acids like tryptophan which supports Ray Peat’s work as you mentioned aswell.
Have to go to bed to get some sleep gains, (living in EU) but can’t wait to wake up tomorrow and finish the rest of it, thank you so much for this Denise!
Tremendous! Thank you! I have not read part two yet so am at this point a confused but open-minded paleo adherent. Always looking to optimize the program based on new information.
You are awesome.
“We can’t ignore evidence in order to preserve an ideology.”
So fucking awesome to read this. Thank you.
Brilliant!
Harold Himsworth never used a word where a paragraph would do, you fall asleep reading him – but he noticed in 1935 that giving carbohydrates increased insulin sensitivity in rabbits, which is to say that more carbohydrates can be tolerated on a high-carbohydrate diet, and confirmed the effect in humans http://www.ncbi.nlm.nih.gov/pmc/articles/PMC1394223/pdf/jphysiol01610-0047.pdf
Perhaps the first low-fatter?
I LOVEEE how you put science behind everything you say!!
Excellent post: shows once again one size does not fit all. Hard to understand how Pritikin had some heart issue, yet clean coronary arteries. And yes, genetics do count. Many tout Jack LaLanne, and yet I believe he had a brother who was not health oriented who lived in to his 90’s.
Many on a very low fat diet will have their LDL size shrink and an increase in Ldl_P and yet not be insulin resistent ( much to the chagrin of the paleo crowd) which appears to be contrary to the data you cite in your piece. Krauss and others say that 1/2 the population will experience it and perhaps those on the very low fat diet who did not have a positive outcome might fit in to this profile.
Hi Steve,
Thanks for your comments! As for your point here —
“Many on a very low fat diet will have their LDL size shrink and an increase in Ldl_P and yet not be insulin resistent ( much to the chagrin of the paleo crowd) which appears to be contrary to the data you cite in your piece. Krauss and others say that 1/2 the population will experience it and perhaps those on the very low fat diet who did not have a positive outcome might fit in to this profile.”
Indeed, there’s generally (but not always, as we saw in this post) a decrease in LDL size on very high-carb diets. I’m no longer convinced LDL particle size is as significant as some health figures are claiming. Large, fluffy, supposedly ‘protective’ LDL predominates in people with familial hypercholesterolemia, who develop atherosclerosis as early as their 20s and 30s (or even earlier for homozygotes!); likewise, low-fat doctors like Ornish have reversed heart disease in patients even when their LDL particles are small. I suspect in Western populations, LDL particle size is part of a cluster of hallmark elements for metabolic syndrome rather something inherently harmful, and that its association with heart disease diminishes in the context of non-SAD diets. I’ll be going into more detail about that in either the next blog post or the one after it!
Denise, looking forward to your LDL post and how it relates to the consumption of saturated fats and dairy.
thanks.
Tim Steele’s “Potato Diet” is what shifted my belief in the powers of a near-zero fat diet! If anyone who is having a hard time losing weight on low carb wants to see dramatic results, just eat nothing but potatoes for a week! You’ll see. Read about it here:
http://www.vegetablepharm.blogspot.com/p/the-potato-diet_14.html
This post made me think of Tim’s potato diet too! I’m glad Denise mentioned the RS content of the rice diet, because I was curious about that.
Denise, this was such an awesome read! Reading things you write is always an enjoyable experience, and makes me feel like I’m getting a brain massage. I’m also a sucker for myth-busting and paradigm-destruction, so that made it even more fun to read. I can’t even imagine how long this must’ve taken you to research and write.
Now that you point it out, it is funny how so little attention is paid to some of the extremely high-carb/low-fat ancestral diets. And when attention is paid, it’s to defend “safe starch,” with little discussion of the accompanying low fat intake.
I’m also glad you mentioned Ray Peat, because the rice/sugar diet made me think of him. I’ve been meaning to make myself understand his dietary recommendations for ages, and just haven’t gotten around to it. I’m super excited to read part 2!
Revisiting cherished theories? Admitting that you were wrong? What a rare thing to find in the diet world. My hat goes off to you. Keep up the good work.
You are brave, girl! It took guts and grace to do this piece–somewhere between a call-out to Thomas Kuhn and a confession to Pope Francis – :).
I’ve followed your writings from the China Study on, agreeing and disagreeing here and there, but admiring your stamina, civility, smarts, good humor, inventiveness, insight and analytical prowess.
I’ve followed even longer Pritikin (since his first book); Ornish (since before his publication of his study showing that a low-fat/et al ‘program’ can reverse heart disease); McDougall (since his first book) and Roy Swank via my first exposure to McDougall. Both McDougall and Pritikin have written about Kempner’s work & I read numerous of his earliest research studies on the Rice Diet website (not sure they’re still available at this site.)
McDougall was/is one of Swank’s biggest fans and was instrumental in funding and designing a Swank-ish MS study in collaboration with OSHU about which one can read here: https://www.drmcdougall.com/2014/07/31/results-of-the-diet-multiple-sclerosis-study/
One has to wonder if the patients in the McDougall ‘arm’ might have done a bit better with a bit more PUFA, as per Swank…but that arm did get randomly assigned the sickest patients in the study. Love McDougall for his helping SO MANY PEOPLE but he’s not the first person I recommend to someone suffering from heart disease (or any of the other diseases that appear to improve, as you so ably demonstrate in your review of the low-fat research, in a significant majority of folks who stick to these low-fat diets). He’s dogmatic to a fault…and his recent coloring book for children borders on the offensive in so many ways (and I am a semi-vegan–for health and environmental reasons) that it makes it really difficult for me to send those in need to his website.
Love Esselstyn too despite the similarities he shares with McDougall. He’s a kinder, gentler, more avuncular McDougall–and his latest study keeps adding to his cred.
But my biggest thanks are for the intro to Lester Morrison! Must have read about him in one of Pritikin’s books but it’s been at least thirty years and it was really fun and educational to be re-informed and enlightened if in fact I had already been exposed to his work and then forgotten about it.
I’m looking forward to part 2. And to the good news on HFLC diets.
I’m sure you’ve seen the recent study by Kevin Hall et al purporting (by others…and Hall) to disprove the carbohydrate-insulin hypothesis in a head to head study of a low carb vs a very low fat diet- http://www.cell.com/cell-metabolism/abstract/S1550-4131(15)00350-2
“Highlights
•19 adults with obesity were confined to a metabolic ward for two 2-week periods
•Cutting carbohydrates increased net fat oxidation, but cutting fat by equal calories had no effect
•Cutting fat resulted in more body fat loss as measured by metabolic balance
•Mathematical model simulations predicted small long-term differences in body fat”
Stephen Guyenet has two nice takes on this study: http://wholehealthsource.blogspot.com/2015/08/a-new-human-trial-seriously-undermines.html
http://wholehealthsource.blogspot.com/2015/08/more-thoughts-on-recent-low-fat-vs-low.html
Both Hall and Guyenet ‘guess’ that an even lower carb diet might show more positive results.
Here’s Hall’s response to the Taubes and Teicholz-like critics: http://www.weightymatters.ca/2015/08/guest-post-dr-kevin-hall-asks-is.html
Hall notes that he’s already finished a study that responds to the many complaints his team has received from the low-carb groups re the first study: https://clinicaltrials.gov/ct2/show/NCT01967563
He’s hinting…but the results haven’t been published yet. Love the suspense!
I am sure I am one of many who truly appreciate the enormous amount of time you have spent on your newest endeavor….and I am really looking forward to whatever comes next: paradox, spoiler, or whatever! Sock it to us! 🙂
Just for people who look at the magic of the rice diet, this extreme part of the program was not long term – just like atkins 20g/day thing was not long term. The rice diet contained extremely low levels of protein, and largely rice protein. Rice protein is great and all, but low in many amino acids, especially lysine, and even more so once you adjust for actual available lysine rather than just total. This is not a diet that is to be consumed for a long time.
The diet was followed for as long as the patient needed to follow it. That might be 6 months in certain cases!
Accomodation is not your friend.
Well, haven’t read all 1.2 million words of Part ! yet…, but I did catch a great mixed metaphor possibility:
BACON-SCENTED rainbow farts from flying, floating, or even incorporeal unicorns, as catechism may demand.
Interesting read. But is there any practical application? Who is going to eat less than 10% fat as a lifestyle? Would be more useful to see an analysis of food combinations for realistic living. If you have a meal high in carbs, that is ok, just ensure its low in fat, etc. These are entertaining post and kudos on your dope writing style… but clinicians are left with the job of actually guiding patients to make realistic changes, which 65% fat or 10% fat are neither for most people.
There are a ton of people already eating this way. Anyone following McDougall, Pritikin, Ornish, Barnard (forgetting any), and possibly Fuhrman are all eating a whole foods plant-based (i.e. vegan) diet. They also feed it at True North Health, the fasting center in northern CA, but it is inspired largely by McDougall as well.
The ATOZ study showed that while Ornish says to eat less than 10% of calories from fat, people who follow (or think they are following) Ornish actually eat about 20-30% of calories from fat – too much for the benefits cited in this article.
There’s also a ton of people eating at the other extreme: moderate animal source foods, low carb, high fat, who are doing very well indeed. Check out Mark’s Daily Apple, for multiple examples. Some people do well as vegans, others – with different biochemistries – don’t. Success on any diet depends far more on factors like the enzymes that our bodies are able to produce than adherence to ideology, at any position on the continuum. For every triumphant vegan story, there’s an equally triumphant ex-vegan story, just as there are people who trumpet their success on their paleo diet and others, once staunch disciples, who now call it the fail-eo diet.
There never was any single ancestral diet, and humans don’t even have a clear ancestral line! More and more DNA work shows that early Homo sapiens interbred (in different times and in different places) with Neanderthals, Denisovans, and a species so far called Species X that some researchers think may prove to Homo erectus. Adding to the excitement, Neanderthals and Denisovans may have interbred. I look forward to the day when babies are food-typed at the same time and as routinely as they’re blood-typed.
…unless also Esselstyn and Campbell, et al
Thanks for your comments! My hope is that by understanding the mechanisms behind macronutrient interaction, we’ll be able to apply the relevant concepts to less rigid diets and create something sustainable. That said, there really are plenty of people out there eating less than 10% fat — folks following the McDougall program, etc. — so it’s not impossible. My own diet falls around 15% fat on many days, and I find it both easy and enjoyable.
“My hope is that by understanding the mechanisms behind macronutrient interaction, we’ll be able to apply the relevant concepts to less rigid diets and create something sustainable.”
+1, though I’m totally down with obtaining 90% calories from maple syrup.
I’m very curious to hear what your research suggests on the topic of potential mechanisms. Your post above seems to foreshadow greater attention paid to the cellular environment, e.g. in your references to quality of blood flow and the levels of O/CO2 available to individual cells. A related theme concerns how the very low fat diets (VLFDs) above may affect electrolyte balance. Do you have any pet theories about the role that cellular metabolism plays in human health? Or whether or not VLFDs provide an “optimal” environment for cellular metabolism?
Yours is my favorite nutrition blog. I’m staying tuned.
Denise
Have you seen these studies that use low fat high carbohydrate macrobiotic diets to reverse diabetes?
http://www.medscape.com/viewarticle/832732
The Effect of the Macrobiotic Ma-Pi 2 Diet vs. the Recommended Diet in the Management of Type 2 Diabetes
The Randomized Controlled MADIAB Trial
http://www.hoajonline.com/internalmedicine/2052-6954/2/3
Ma-Pi 2 macrobiotic diet intervention during 21 days in adults with type 2 diabetes mellitus, Ghana 2011
http://onlinelibrary.wiley.com/doi/10.1002/dmrr.2519/pdf
Ma-Pi 2 macrobiotic diet and type 2 diabetes mellitus: pooled analysis of short-term intervention studies
Click to access Hindawi_MaPi2_2012.pdf
Medium- and Short-Term Interventions with Ma-Pi 2 Macrobiotic Diet in Type 2 Diabetic Adults of Bauta, Havana
http://www.wjgnet.com/1948-9358/full/v6/i3/403.htm
Gut microbiota and Ma-Pi 2 macrobiotic diet in the treatment of type 2 diabetes
Click to access mr_119.pdf
Ma-Pi 2 Macrobiotic Diet Intervention in Adults with Type 2 Diabetes Mellitus
With regard to Dr Morrison
Click to access 358.full.pdf
Prevention of Atherosclerosis in Sub-Human Primates by Chondroitin Sulfate A
By Lester M. Morrison, M.D., Katsumi Murata, M.D., Ph.D., J. Joseph Quilligan, Jr., M.D., O. Arne Schjeide, Ph.D., and Leon Freeman, Ph.D.
https://www.dropbox.com/s/17vsix1d1qbctft/morrison1973.pdf?dl=0
CORONARY HEART DISEASE: REDUCTION OF DEATHRATE BY CHONDROITIN SULFATE ALESTER M. MORRISON, M.D., F.A.C.A., AND NORBERT L. ENRICK, PH.D
AMAZING. Please post part II soon!!!
Fascinating! Those of us who’ve been around quite a spell (I’m 66) already know that reality is far more complex than our dearly-held beliefs would have it, but we so effortlessly forget that, as we slip into dietary dogma (and political dogma, etc., ad infinitum). I’ve just been thinking deeply about just this issue in regard to feeding the cats. Of all the dozen or two cats, and seven or eight dogs, I’ve had in my time, Tibey is the first one I had to take to the vet (UTI). Brought him home today, $6,000 in the hole. We have a first-rate vet who gave excellent medical care, but she gave a bag of kibble labeled Urinary Health. Ingredients? Chicken, corn, corn gluten, soybean oil, and on and on to pukedom. I’ve fed him and his brother a species-appropriate diet, based upon Kymythy Schultze’s recommendations, for about six years, since weaning. I also have Dr. Becker’s book, and, in rereading it I noticed that she says the diet of wild felines includes only 7% fat! So I’ve been giving them too much (they are lean, sleek, incredibly athletic, and, of course, lovable) I assumed that the negative effects of excess dietary fat would result partly from the displacement of other essential nutrients, but the studies you’ve discussed sound largely like starvation, junk food diets, so what gives? Food for a great deal more thought, a great deal. Thank you so much for this fine piece of work. It is good for us to shatter our myths from time to time-keeps us properly humble.
my husband lived in taiwan from ’63 to ’97. yes, he was very thin on a traditional, low-fat, mostly rice diet in taiwan before the economic boom hit in his middle school years. he was thin because he was poor and went to bed hungry every night. he does have beautiful teeth, though. when i lived in taiwan off and on for 7 years i got a lot thinner, but my body i believe canabalized my muscle. i had been very athletic before the move to taiwan. living in taiwan i only walked a lot of exercise. when i got home and took a hike in the woods with a friend, my fingers swelled up i believe because my heart wasn’t pumping the way it should have been. i was only 24 at the time.
Thank you for sharing your experience. I suspected the HCLF diet is only useful as a 6 month diet. People who need muscles probably can’t handle it. Though I’ve seen stick thin people with incredible strength so who knows. Nutrition is complicated
So “eat anything in moderation” is out then!
Well, technically, ‘paleo’ can encompass high carb diets as well as low carb ones while still maintaining its’ core tenants. I wonder if I should try a high carb diet? It sounds pretty insufferable though…
Dear Denise:
Thank you very much for writing this. I really appreciate that you are willing to publicly change your mind and admit you were wrong about something. I really appreciate how you mostly refrained in this article for advocating for a new replacement theory to explain everything and allowed yourself instead to dwell on evidence against a current theory. And I really appreciate that you forced your attention onto uncomfortable evidence, and that in doing so you forced me to do likewise. I do indeed find these results surprising and discomforting, and I’m glad to be forced to think about them.
I do have two objections, but before I launch into them I want to emphasize that these objections do not give my weary brain an “out” and let me shove this uncomfortable evidence out of sight and forget about it.
The first objection is that these results are all from an earlier era, not randomized, and so it’s hard for me to know how this kind of treatment would compare to alternative treatments tested under better-controlled, randomized conditions. I did a quick bit of googling and hit upon this updated, randomized trial from McDougall:
https://www.drmcdougall.com/2014/07/31/results-of-the-diet-multiple-sclerosis-study/
Apparently the results were so disappointing that it didn’t get written up into a paper but was instead merely a poster: http://www.neurology.org/content/82/10_Supplement/P6.152 . The actual results aren’t all there (it says “Click to enlarge” but it doesn’t enlarge for me). The excuse from McDougall at the end of that web page about randomization resulting in too many more-sick patients going into the test group doesn’t make any sense. They could still have reported improvement in those patients, if they had improved, or if their rate of decline had been lower than expected.
So my first objection is that as far as I know (which isn’t far), these phenomenal results have failed to replicate when attempted under better-controlled conditions.
My second objection is this: “We can’t categorically blame low-fat, high-carb diets for heart disease and diabetes and obesity. We just can’t. NOT EVEN A LITTLE BIT. This needs to go away.”
No, that’s wrong. Earlier in your post you argued that reducing fat from 34% to 30%, and finding no improvement, shouldn’t be used as an argument that reducing fat to 10% wouldn’t be beneficial. That’s a good argument! And for the exact same reason, the fact that increasing carbohydrate to 90% was beneficial (in these non-randomized experiments) should not be used as an argument that increasing carb from 48% to 54% is not a chief cause of our current health crises.
Sincerely,
Zooko
i think the takeaway lesson from this is that this writer is not, and should not be regarded as, a health authority. you’re doing the right thing in doing your own research; she has no credentials, she simply reads a lot about nutrition. as do i, and as you do as well, i take it.
Dear Denise: if you could delete this comment, which is a slightly earlier version of my comment below, that would be cool. I don’t see a way to delete it myself.
Hey Zooko,
Thanks for the great comments! Those are some excellent points. In response —
1) The lack of robust study design is definitely the biggest problem with studies from that era. Ideally, I would LOVE to see a “true” low fat diet and a “true” low carb or keto diet go head-to-head with a great study design, relatively large sample size, and sufficient follow-up period. Maybe one day the Funding Gods will descend and grant such a thing. Until then, I appreciate the older studies because, despite weaker designs, they’re free from other notorious forms of confounding plaguing research today (especially healthy user’s bias).
That said, I’m very familiar with that McDougall study and will talk about it a bit in the next post. What I find fascinating is that the biggest difference between the two men’s studies is that McDougall used a strict vegan diet for his, and Swank allowed a wide variety of animal products (and considerably higher protein intake), so long as they were lean (trimmed meats, skim milk, egg whites, plenty of seafood). That raises the possibility that the vegan component was actually harmful (or less beneficial), that something in the lean animal products in the absence of saturated fat was also helpful, or any other of a variety of options; the mens’ diet were similar in fat intake but not identical elsewise. Relapse rates had already dramatically improved for the Swankers by one year, so I’m hesitant to suggest McDougall’s study just wasn’t long enough for the results to start manifesting, but I suppose that’s a possibility as well (seeing as Swank’s 50-year monitoring of some patients allowed a much fuller view of their disease progression than one year for the McDougall study).
It also raises the intriguing possibilities about MS symptoms improving independently of improvements in brain lesions/MRI scans. Swank didn’t use MRIs in his study or measure brain lesions; he only went by objective changes in the patients’ physical capabilities and their number of relapses over the years. So we can’t even say for sure that his study improved MS on the basis of lesions. McDougall’s study does show a trend of improvement in FSS score and MFIS score between 0 and 12 months, especially a pretty dramatic jump when they first started the diet from baseline — so the patients WERE improving in some measure. Why did they improve without concurrent improvements in MRI scans? Could it be possible that the diet alleviates MS symptoms in a different way and sheds light on a different element of MS etiology? I find it fascinating as a possibility, though certainly inconclusive, and I’m not as well versed in MS as I’d need to be to know if that theory could even hold water.
Anyway, Swank’s results (and rationale) will make a lot more sense after Part 2. He conducted (and drew from) a lot of additional research on both animal models and humans, showing some very specific changes in blood and tissue oxygenation from dairy fat (meals of nothing but pure cream — and in the 1940s, before dairy was largely crap). Anyway, stay tuned for that, as it does add more credence to Swank’s findings.
2) “”“We can’t categorically blame low-fat, high-carb diets for heart disease and diabetes and obesity. We just can’t. NOT EVEN A LITTLE BIT. This needs to go away.”
No, that’s wrong. Earlier in your post you argued that reducing fat from 34% to 30%, and finding no improvement, shouldn’t be used as an argument that reducing fat to 10% wouldn’t be beneficial. That’s a good argument! And for the exact same reason, the fact that increasing carbohydrate to 90% was beneficial (in these non-randomized experiments) should not be used as an argument that increasing carb from 48% to 54% is not a chief cause of our current health crises.”
Ah, I disagree. We can’t blame low-fat, high-carb diets for heart disease and diabetes and obesity because the nations (America, etc.) suffering from these conditions have NEVER eaten low-fat, high carb diets. We’ve eaten moderate-fat, moderate-carb diets, which may be the worst of the worst. 🙂
It would make sense that the well balanced proteins from lean meat, which tend not to be allergenic, would be much better with respect to an autoimmune disease like MS than plant proteins, which tend to induce immune system reactions.
I think it’s ridiculous to assert that a 15% fat 80% carb diet isn’t “low fat, high carb”. 20% carb, 60% fat diets – typical strict paleo – are always referred to as low carb, high fat, after all. People who go below 10% carbs are usually referred to as being on “very low carb”, “ketogenic”, or in some cases, for those on 0% carbs, “zero carb”. Similar wording should be used for the other end of the spectrum.
Heart disease has been with us for a while, but we can absolutely blame low fat, high carb for the obesity epidemic. What we can’t blame is VLF (very low fat) or no-fat diets.
”We’ve eaten moderate-fat, moderate-carb diets, which may be the worst of the worst.”
Even worse yet, Denise.
We have eaten mostly a moderate (SFAs, refined PUFAs, and trans-fat) fat, and moderate (sugar and refined carb) diets. That’s the SAD. Lots of meat, refined carbs, and junk. No wonder we’re in the state we’re in. Anyone blaming the low-fat diet for our current health state is not being honest. As you have shown, lots of population ate successfully a truly low-fat, high unrefined carbs diet with excellent health.
Thanks for your article.
” We’ve eaten moderate-fat, moderate-carb diets, which may be the worst of the worst. :)”
What about Ancel Keys Med Diet? It lies in the middle of Swampland, yet it allows the eating of all foods…in moderation. As a result it is the best of the worst, at a minimum.
Pushing macronutrient extremes in search of a perfect health diet is an interesting game to play. But it takes extreme motivation, a flexible schedule and an open wallet. Most people can’t sustain these diets for more than a few months, so their usefulness is confined to emergencies like weight loss, celiac, and IBS.
Dear Denise:
Thank you very much for writing this. I really appreciate that you are willing to publicly change your mind and admit you were wrong about something. I really appreciate how you mostly refrained in this article for advocating for a new replacement theory to explain everything and allowed yourself instead to dwell on evidence against a current theory. And I really appreciate that you forced your attention onto uncomfortable evidence, and that in doing so you forced me to do likewise. I do indeed find these results surprising and discomforting, and I’m glad to be forced to think about them.
I do have two objections, but before I launch into them I want to emphasize that these objections do not give my weary brain an “out” and let me shove this uncomfortable evidence out of sight and forget about it.
The first objection is that these results are all from an earlier era, when randomization was not practiced, and so it’s hard for me to know how this kind of treatment would compare to alternative treatments under better-controlled, randomized conditions. I did a quick bit of googling and hit upon this updated, randomized trial from McDougall:
https://www.drmcdougall.com/2014/07/31/results-of-the-diet-multiple-sclerosis-study/
Apparently the results were disappointing — no improvement in brain imaging or in disease burden for the low-fat diet arm. So disappointing, apparently, that they didn’t get written up into a paper but instead merely a poster: http://www.neurology.org/content/82/10_Supplement/P6.152 . The actual results aren’t all there (it says “Click to enlarge” but it doesn’t enlarge for me). The excuse from McDougall at the end of that web page about randomization resulting in too many more-sick patients going into the test group doesn’t make any sense. They could still have reported improvement in those patients, if they had improved, or if their rate of decline had been lower than expected.
So my first objection is that as far as I know (which isn’t far), these phenomenal results have failed to replicate when attempted under better-controlled conditions.
My second objection is this: “We can’t categorically blame low-fat, high-carb diets for heart disease and diabetes and obesity. We just can’t. NOT EVEN A LITTLE BIT. This needs to go away.”
No, that’s wrong. Earlier in your post you argued that reducing fat from 34% to 30%, and finding no improvement, shouldn’t be used as an argument that reducing fat to 10% wouldn’t be beneficial. That’s a good argument! And for the same reason, the fact that increasing carbohydrate to 90% was beneficial (in these non-randomized experiments) should not be used as an argument that increasing carb from 48% to 54% is not a chief cause of our current health crises.
Sincerely,
Zooko
Two follow-ups to my own comment:
1. I realized that I didn’t find that McDougall trial through Google — I found it by reading admgm’s comment. Sorry to have forgotten that, admgm.
2. There’s another way that trials from this era are unreliable, and that’s selection effects by the experimenter after the beginning of the experiment. For each subject who did well under their care, the experimenter would take credit for it, and for each subject who did badly, the experimenter would investigate and find some way that the subject was not following the protocol and blame the subject for it. Then they would write up a report showing that their treatment had a nearly perfect track record. To prevent such shenanigans is why nowadays we require Intention To Treat analysis.
Some of the parts of your post about just counting the results in adherers reminded me of this, and so did the part about whipping the patients, because those experimenters who blamed patients for their failure would also tend to be the ones who bullied patients.
(As an aside, I think that *both* Intention To Treat *and* adherer analysis should be standard instead of just ITT, but that’s a topic for another day.)
Denise – beyond this post being, honestly, the most interesting thing I’ve read in the health-o-sphere this year, it’s inspiring.
It takes big stones to backtrack on your beliefs and admit they were short/wrong/misguided/whatever – something that so few in this biz are willing to do (or are even capable of doing).
Well done. Way to set the bar high. Looking forward to part 2.
My thoughts exactly!
I respect how Denise is slowly and politely Denise is removing herself from the wacko paleo community she found herself involved with. Just have a look at the first few AHS talks she did. They must be pretty embarrassing to watch, especially considering the type of people she found her associated with. Leaving the Raw food wacko’s and jumping into the wacko paleo camp was probably a pretty big move for her.
Finding out that the paleo sect that she jumped into is just as wacko or even worse than the raw food cult she left was involved in must of been pretty brutal.
Actually what the article is saying is that it’s the wackos at both ends that have it right, and the people who preach moderation that are wrong.
Courageous angel!
Personally I’ve tried both ends of the dietary spectrum. Both require an adjustment period. And while both may be magical in their own way, intuitively I’ve leaned toward the high carb pole.
This diet war has raged for a good while now, but a clear and rational evaluation such as this represents a major push forward for the high carb camp.
Essential fats and carbs don’t mix well. One option is to cut the fat, the other to cut the carbs. Cutting fat is evidently a health inducing option, whereas high fat has its issues longer term.
Essential fats and carbs mix very well indeed, and have for millenia. The problem for millenia has been finding enough fat, at a price that the average person can afford. It’s only recently that people have had a problem with being in the middle of the swamp. That’s where I live, and eat my daily 1000 calories carb, 1000 calories high fat, 400 calories protein, and maintain healthy weight. You cannot overeat for what you do, and I get the 1000 calories a day Cordain recommends for a minimal level of Paleo exercise. Ditch the car/subway/bus, ditch the chair, and walk bike or run to the nearest bakery for the donut you need to get your needed calories for the day. They’re not empty calories if you metabolize them.
Believe me the middle of the swamp is the sweet spot. Not an Atkins/Taubes/Eades/Jimmy Moore CVD risk-land, nor a Jobs/Pritikin wrecked liver-land. Every food every day, within reason.
Wow, this was an amazing read, thank you for pulling this all together. It’s left me confused not really knowing if there is a way forward. I do wonder at the effect of all these extremes on the gut biome, and wonder that the restricted nature of some of these diets actually promote healing and remission by improving the gut health. I got diagnosed with Hashimotos this February, prior to the blood tests (out of desperation with ballooning weight), I went on the HCG diet which is virtually no fat. My symptoms improved amazingly (mainly the pain and fatigue), even though I didn’t loose as much weight as I hoped. It wasn’t until I started taking thyroid medication that the weight slipped away. I follow a restricted paleo diet. I look forward to reading part 2, is there going to be any help with a way forward?
I appreciate your hard work in pursuing the truth, I lost 50Kgs and got rid of diabetes through low fat diet only to afterwards change my mind and admit publicly that a high fat diet is superior so I can definitely appreciate your humility and your science based rather than ego based approach. But I do have five comments/questions here –
1) To get below the magic number of 10% fat – one has to reduce consumption of animal products and with that to reduce the consumption of DHA, EPA, B12, Iron, Zinc, Iodine, Glycine, etc, etc. What is the impact of such a diet on the *brain’s health*? What is the impact on our hormones? On our sex drive? On Homocysteine levels? On the activation of so many genes in our body. I am aware that you said that many of these low fat diets do allow some consumption of animal products – but the question is how much and whether that is enough. Health is not only about cardio vascular health and cancer prevention. I would love it if your part 2 (or part 3) will take that into consideration. Let’s see the whole picture.
2) I wasn’t aware that we humans can’t synthesize Neu5GC and that actually we have antibodies against this thing. I was under the ancestral approach impression that whatever we were evolutionary accustomed to eat – was good for us – this is why we survived so far and so based on this understanding if really there was a problem with the Neu5GC then we would all become vegans by natural selection process. We know that this is not true because never ever has there been a vegan society lasting more than several generations.
3) How easy it is to live one’s life on the low fat diet? I think you have to be quite the masochist to adhere to such a regime. So yea, suppose that after you answer points (1) and (2) above and indeed low fat diet is even a bit better than high fat diet – which diet should one pursue? How much can a person sustain such a harsh low fat diet and convince himself that he feels great? I would choose the easier diet, the one that I can pursue for the rest of my life.
4) Why is it that you are focusing only on the extreme diets? Either very low fat or very high fat? Doesn’t it make sense that humans, throughout the last 2.5 million years ate a diet that is somewhere in the middle?
5) Does this blog post mean that you now moved from advocating high fat to low fat? Or is it that you merely indicate that there’s a viable low fat diet option?
Hi Aviel,
Thanks for the great questions! I’ll address them as best I can, in order:
“1) To get below the magic number of 10% fat – one has to reduce consumption of animal products and with that to reduce the consumption of DHA, EPA, B12, Iron, Zinc, Iodine, Glycine, etc, etc. What is the impact of such a diet on the *brain’s health*? What is the impact on our hormones? On our sex drive? On Homocysteine levels? On the activation of so many genes in our body.”
— I’d say, first of all, that 10% of calories as fat is an average and not necessarily the goal of every single meal of every single day. I’ll be covering this in Part 2, but for folks who aren’t trying to reverse their diabetes or advanced heart disease, occasional (2 – 3 times per week) higher fat meals with nutrient-dense animal foods is unlikely to ruin the carbosis benefits and will make for a more nutritionally complete diet.
That said, a low-fat diet doesn’t necessarily reduce intake of those micronutrients, apart from DHA and EPA. Liver (rich in vitamins A, D, E, K, B12, iron, copper, etc.) is only 25% fat, and can easily be integrated into a low-fat diet without pushing the macro averages above 10%. Clams are only 9% fat and also very high in B12; other shellfish like oysters supply a lot of animal-based nutrients as well and are relatively low in fat. Bone broth is low fat and rich in glycine. Insects are mostly protein, for those daring to go there! 😉
As for DHA and EPA, the need isn’t particularly high if omega-6 intake is low, so small amounts of seafood will probably be sufficient here. Interestingly, it seems fat restriction actually increases omega-3 status — see http://jn.nutrition.org/content/131/2/231.full: “Consumption of a low fat diet alters fatty acid patterns in a manner similar to that observed with feeding of (n-3) long-chain fatty acids. This change is likely related to decreased competition for the enzymes of elongation and desaturation, with reduced total intake of 18:2(n-6) favoring elongation and desaturation of available (n-3) fatty acids.”
As for the impact of very low-fat on brain health, sex hormones, etc., I’d love to see more research delving into that using non-vegan diets. Considering that many populations have successfully subsisted and reproduced on diets in the 10 – 15% fat range, I doubt it harms reproductive functions as long as energy intake and micronutrient content is sufficient. Neurological health deserves more attention, and my guess is that there will be a range of response due to individual variation and ApoE status. Homocysteine is unlikely to be a problem as long as folate and B12 status are good.
“2) I wasn’t aware that we humans can’t synthesize Neu5GC and that actually we have antibodies against this thing. I was under the ancestral approach impression that whatever we were evolutionary accustomed to eat – was good for us – this is why we survived so far and so based on this understanding if really there was a problem with the Neu5GC then we would all become vegans by natural selection process. We know that this is not true because never ever has there been a vegan society lasting more than several generations.”
— Per evolutionary theory, we only need to survive until reproductive years in order to keep our DNA in the gene pool. The problems associated with Neu5GC (in theory, anyway) wouldn’t show up until later in life, after reproduction; and historically, the biggest killers were immediate things like acute infections, traumatic injury, etc. before chronic disease had a chance to take hold. Also, if Neu5GC really is an issue (still highly speculative!), it involves interaction with bacteria that may be a more neolithic phenomenon.
“3) How easy it is to live one’s life on the low fat diet? I think you have to be quite the masochist to adhere to such a regime. So yea, suppose that after you answer points (1) and (2) above and indeed low fat diet is even a bit better than high fat diet – which diet should one pursue? How much can a person sustain such a harsh low fat diet and convince himself that he feels great? I would choose the easier diet, the one that I can pursue for the rest of my life.”
— I disagree here! I actually very much prefer a low-fat diet to a high-fat one (although my only experience with low carb, high-fat on a personal level was only a 6-week experiment a few years ago — I experienced no detectable advantages and had a few problems worsen). There are thousands (? I’m guessing) of followers of the McDougall program, Ornish, Pritikin, etc. who appear very content with their diet. Apart from my six-week experiment, my diet has been pretty low fat for the past 10 years and I actually prefer it taste-wise and texture-wise to higher-fat eating plans. If you’re interested, Angelo Coppola has a “Plant Paleo” diet plan that fits into the low-fat bracket but is very nutritionally replete and looks delicious: http://www.humansarenotbroken.com/about/plant-paleo/
“4) Why is it that you are focusing only on the extreme diets? Either very low fat or very high fat? Doesn’t it make sense that humans, throughout the last 2.5 million years ate a diet that is somewhere in the middle?”
— I’m focusing on the extreme diets as a way to explore macronutrient interaction and its impact on human health. I’ll explain more in Part 2 why I think we can isolate some of the effects from these extreme diets and apply them to more flexible eating plans. To get there though, we have to study what exactly is happening on a biological level — which is why these studies (and the more mechanistic research I’ll go through in Part 2) are valuable!
I’d say it’s historically much more likely that we swung between macronutrient extremes than ate a diet in the middle: warmer seasons would feature abundant fruit and plant foods (high carb), winter would have lower high-energy plant food ability but perhaps more large game; and even in the shorter term, times of gathering (plant foods, small lower-fat/higher-protein mammals and insects and reptiles) would be punctuated by sporadic successful kills, in which case gorging on meat was likely. Even geographically, tropical areas tend to produce more sugary and starchy foods (fruits, tubers/roots) and polar regions are lower carb with more animal-derived nutrition.
“5) Does this blog post mean that you now moved from advocating high fat to low fat? Or is it that you merely indicate that there’s a viable low fat diet option?”
I’ve never advocated high fat (or any specific diet, for that matter), so I guess the technical answer is no. I’ve defended high fat when the science used to discredit it is bad, and I’ll continue to do so when the occasions arise — as well as recommend it when it seems the best choice for someone’s specific situation. But I’d be quite a hypocrite to advocate a high-fat diet when my own experience with it was unimpressive and I’ve been eating a low-fat diet for the last decade! 🙂
We need to keep in mind that the body fat composition of the wild game, even the hooved mammals, that our Paleo ancestors ate was a far cry from that of today’s typical feedlot-fattened, selectively bred cattle and grain-fed poultry. Outdoor Life lists the fat content for various types of wild game commonly hunted today, and many of these animals have less than 10% fat in their meat. These include mule deer, elk, antelope and several others. So even during seasons when our ancestors consumed a fair quantity of red meat, it probably wasn’t hard for them to keep their intake in the 10-15% fat range. History buffs have probably encountered the term “rabbit starvation” in the diaries of early explorers, a situation where a person’s body fared poorly because the meat he was consuming was so lean.
Wild game is about 10% fat by weight. That comes to about 50% fat by calories – more after accounting for bones and such. Our livers cannot handle more than about 40% of calories from protein – thus rabbit starvation – so at those times we ate meat, we were getting most of our calories from fat.
I don’t think it’s a coincidence that the whole body body fat percentage of wild game is very similar to the fat percentage to which steaks are typically trimmed. Most of the extra fat on feedlot animals is trimmed and discarded.
No. As a scientist, organic foodie, and math nerd, I DO know the pitfall of comparing calories on a weight vs. calorie basis. The Outdoor Life analysis was based on calorie percentages, NOT on weight. For example, 3.5 oz. of elk meat at 0.9 g fat, total 137 calories. See http://www.outdoorlife.com/photos/gallery/hunting/2013/02/wild-game-nutrition-guide-organic-meat/?image=3
Wild game is very different from “trimmed steaks” from grain-fed beef, and one reason people complain of elk as being too “dry”. Most of the fat on beef cuts in grocery stores is NOT trimmed. Even when I buy grass-fed beef, I end up trimming a huge amount of fat from it. At certain seasons, yes, the fat in wild game is higher. The protein handling problem is likely just what was causing a problem for the folks suffering from rabbit starvation. And please remember that fat and protein are only two of the macronutrients — our Paleo ancestors ate a lot of carbs — root veggies and tubers and fruit and such. Despite what some bacon-addicted “modern Paleos” will tell you.
That Outdoor Life analysis does not reflect the whole animal. It reflects a trimmed 3.5 oz serving. And most of the fat absolutely is trimmed off of beef cuts in grocery stores. To see what a steak from a feedlot animal looks like if it really isn’t trimmed, have a gander at the picture here:
http://cavemanforum.com/diet-and-nutrition/how-to-get-more-healthy-tasty-affordable-animal-fat-in-my-diet/msg67510/#msg67510
Yes, that’s more than half an inch of fat most of the way around the steak.
Now, wild animals do not have that much fat, which in domestic cattle can be up to 40% of total carcass weight. However, even wild ungulates do have substantial amounts of fat in deposits in the belly and in the rump at the base of the tail, amounting typically to around 10% of the total carcass weight. That’s more than half of the total carcass caloric value. Paleolithic humans would have had no problem getting fat to eat.
Yes….and I was under the impression also that early humans, and many modern hunter-gatherers, ate plenty of fat. Animals with fat were sought after; and though some wild animals are lower in fat, there are plenty that have fat on them. Early humans used to eat brain marrow, also high in fat, and Inuit and other native people ate fatty fish and sea mammals. Many hunter-gatherers processed the fat of certain animals, to be used later- (ever heard of oolichan grease? Not sure if I spelled it right….And then of course there’s pemmican….) So, yes; I agree with Psychohist.
yes. Plus Paleolithic and Paleolithic-style cultures also selectively hunted the older animals late in the season who had really good stores of fat on them. Modern day “theorists” don’t ever consider these sorts of details.
The idea that they selectively hunted old fat animals is also a theory and quite the generalization.
No it has been observed in Paleolithic style cultures.
There is no such thing as a paleolithic style culture. There are hunter gatherer style cultures but even then, little to none that do not also utilize some sort of agriculture or animal husbandry. Gathering data from these cultures no not in any way validate any theory of our paleolithic ancestors. And please don’t mention Inuit cultures, they are a very young culture and are about as far removed from any ancestors that have any influence on 99.99% of modern humans.
Zach: I believe you are talking about modern day hunter-gatherers. However, many of these observations were made in the 1800’s and early 1900’s, the time of the explorers. Back then, there were not only more hunter-gatherer cultures in existence, but they were also living a more “pure” hunter-gatherer lifestyle. Since you don’t want anyone to mention the Inuit, I won’t, but let me give another example: the Sioux Indian (as well as other Plains Indians). The Sioux lived mainly from buffalo meat, and it was noted that when they hunted, they did indeed choose the fatter animals.
Generally, since hunting expends a lot of calories, it has been noted by observers that hunting cultures tend to try to seek out the most nutrient dense foods; in other words, preferring to kill a bigger animal over a smaller one, or choosing the animals with the most fat on them- (at least they did this whenever possible. I may also hasten to add that modern day hunter-gatherers have fewer choices, due to encroachment, being pushed off their lands and into more marginal territory, etc.) It is theorized that Paleolithic people probably behaved in a similar manner, though I guess we don’t know this for sure. But it makes sense, seeing as we somehow survived through the ice age.
I’m not saying that all hunter-gatherers *have* to eat lots of fat.Those that have access to more plant foods and other carbohydrates could probably get by with less fat. But the “low carb” hunter-gatherers- and there were quite a few- would have had to have eaten adequate fat.
I spent some time on this site. That area had a rich history dating back centuries. There are links to a diary of white explorers living off of game, who reported eating currents they found made them sick, but they mentioned there was nothing really wrong with the currents. Perhaps due to a change in gut bacteria(my theory ). It may have been on this site that I read certain berries were added to the meat and fat to preserve them.
http://www.history.alberta.ca/headsmashedin/default.aspx
This book was at one time available to read free online.
http://www.aupress.ca/index.php/books/120137
I have never tried a diet of just meat and fat.
Zach, what you say makes no sense. People can argue the semantics of “paleo,” now a highly co-opted and abused word. But the fact that a society following an ancestral lifestyle, like the Hadza, even if they also practice agriculture and/or animal husbandry, doesn’t necessarily alter how they pursue their hunting and gathering, nor does it necessarily make it different from dedicated hunter-gatherers past or present. As far as “validating any theory” not sure what you mean by that either. It’s unlikely we’ll ever know in detail what pre-agricultural societies ate. We need to use the evidence at our disposal. This includes what direct evidence we do find (e.g. bones showing cut marks), analyses of bone and dentition, and, yes, examining the lifestyles and foodways of modern day hunter-gatherers. And absolutely we need to include Inuit cultures who migrate to the NA Arctic in ~900AD, and who come from the same common ancestors as nearly all of us only 40,000 yo. That’s only 2000 generations ago–time for a handful of successful SNPs to survive, like lactase persistence–but not for the very many conditions that are are determined multifactorially, such as Type 2 diabetes, driven by MNPs locvated on at least six genome sites.
Good points, wbryanh. And I’ll repeat one of the comments I made earlier above, that there is very good evidence that early humans broke open the brains of the animals they killed and sucked on the brain marrow. (Very high in fat). Some even theorize that this is what made our brains become bigger.
Excellent overview, thank you Denise!
For me, the problem with all of these studies is that they focus on the same type of person. Either they’re all overweight or they all suffer from some kind of disease. It would be very helpful if, at the very least, studies were designed that tested how overweight people and those with normal weight, or how sick and healthy people react to the same type of diet.
My point is, there are basically two different kinds of people who, for simplicity’s sake, can be put in one of two categories – heat sensitive or cold sensitive. It’s actually a bit more complicated than that and environmental factors are tied to this as well, but in general these groups’ reaction to the different types of food is inherently different and they develop altogether different types of diseases when they eat the wrong diet for their type. Simply put – their bodies are unable to maintain a certain elemental balance and diseases develop because of that.
Thus, when the same type of diet is tested on people from both groups, the results might be markedly different. While one group may do well on a certain diet, the other might actually develop all kinds of problems. To find out which diet is good for a person, one has to find out to which group the person belongs, without ignoring environmental factors and other individual differences in the person’s lifestyle, all of which have an effect on their metabolism and ultimately their health. For example, it makes a huge difference if a person does primarily physical or primarily mental exercise.
Yes, I think that is the point. Denise is showing that there is not just one kind of diet that can help people. Frankly if you live long enough and have tried a great number of diets yourself for various purposes and at various times in your life and spoken with a number of other people who have done the same, you don’t need elaborate research or studies begin to understand that ( beyond eating real, well produced and fresh food) there is not one best way of eating. We need to better understand why some diets work best for specific conditions and specific people. The point is to get beyond trying to win the LCHF/HFLC wars and to collaborate on trying to discern how to target diets for individuals, healthy ones and sick ones. My bet is that there will be numerous variations.
Hello,
I think you have a typo. Search for “changges” which I think should be “changes” with only one ‘g’ letter.
V/r,
Bryan
The sooner people lose their obsession with macronutrient ratios, the better. Carbs, fats & proteins can be obtained from:-
1. Minimally-processed animal & vegetable produce.
2. Over-processed crap-in-a-bag/box/bottle.
We should be basing our diets on 1.
The Food Product industry wants us to base our diets on 2 and uses every marketing trick in the book to “make it so”.
Did you miss the part where the successful very low fat diets had milled rice and refined sugar as major elements?
No. In what way does your comment contradict the fact that we should be basing our diets on 1.?
Just because it’s possible to be healthy on a diet of milled rice and refined sugar for *one* *year* doesn’t mean that it’s the optimum diet for *life*.
Do you have any evidence that 1. isn’t a better choice over a lifetime? Kempner’s trial only lasted for one year, so there would have been no long-term health problems caused by micronutrients missing from his diet.
The actual evidence Denise presents is that 1. doesn’t matter if you are on a very low fat diet.
There is also evidence that whole grains are worse from an autoimmune perspective than refined white flour. In general, for nonpaleo foods, processed versions seem if anything healthier than unprocessed versions.
Whole grains contain oils in the outer coat that can go rancid. Consuming rancid oils from stale whole grains is definitely not good for optimum health. Refining grains removes these oils, which is a good thing. However…
Refined grains are lower in certain minerals (copper & manganese, for example). If this is compensated for by eating other foods that are high in those minerals, it’s not a problem. A diet comprising milled rice, refined sugar & fruit juice will be lacking in the above minerals.
A very low fat diet comprising veggies, root veggies & tubers, legumes, whole grains and whole fruits will be high in the above minerals.
Please provide evidence showing that fresh whole grains are worse from an autoimmune perspective than refined white flour.
“Please provide evidence showing that fresh whole grains are worse from an autoimmune perspective than refined white flour.”
It’s because whole grains have more toxins like gluten and wheat germ agglutinin. These toxins lead to more leaky gut and then trigger autoimmune responses due to molecular mimicry.
As someone with an autoimmune disease, I’m perfectly happy avoiding both whole and refined grains. Doesn’t hurt anything, and I’ve got both bases covered.
“It’s because whole grains have more toxins like gluten and wheat germ agglutinin. These toxins lead to more leaky gut and then trigger autoimmune responses due to molecular mimicry.”
You’ve got it the wrong way round. Whole grains have an outer husk which *doesn’t* contain gluten, so the relative gluten content of whole grains is lower than for refined white flour. Also, despite thorough chewing, whole grains have a much smaller surface area than refined white flour, reducing absorption through the gut wall.
As you have gut permeability issues & AI disease, you’re better-off sticking to meat & veg!
The opposite is the case. There is much more missing in refined grains than just copper and manganese (althouth those trace minerals are crucial for phase II enzymes). We always have to be wary of the fallacy of reductionism when evaluating the health effects of a complex, natural food. There are many more differences between whole and refined grains, all being at least as significant as the content of micronutrients:
1) Fiber, of course, but the term “fiber” is as much an overgeneralized umbrella term as the term “fat”. Both comprise a huge variety of compounds with very different health effects. While in contrast to fatty acids, all known types of fiber seem to have beneficial effects (well, except a well known side-effect from large doses), some excert their effects simply by increasing the mass of the intestinal lumen, some have probiotic effects, and some excert potent physiological effects even beyond acting as a prebiotic. Whole grains – particularly oats and barley, but also wheat and rye – contain large amounts of β-glucans in the bran – a type of fiber that is also found in fungi but fruits an vegetables are generally devoid of – that is partially absorbed and partially metabolized by gut bacteria. It excerts powerful immune-regulating effects, not only on the intestine (which we now know to be crucial on a systemic level) but also systemically through intestinal absorption of the β-glucans and their bacterial metabolites. Here is a comprehensive review on β-glucans done by a hobby researcher.
2) An abundance of seconary plant metabolites concentrated in the bran, phenolic compounds such as simple phenolic acids and tannins, compounds related to B-vitamins such as PABA, and – probably most importantly – significant amounts of inositol hexaphosphate or phytic acid. The very compound that paleo lore has painted as a villain of whole grains may in fact have highly beneficial effects in well nourished Westerners, as it has a high binding affinity to iron and does chelate iron not only in the intestinal lumen but is also absorbed through passive diffusion and acts as an chelator of free iron in the blood stream, as testified by many people who suscessfully lowered their iron overload by taking supplemental IP6. Ironically, Paleo dieters who avoid phytic acid like the plague would probably derive the most benefit from it, given the high heme iron and saturated fat load of such dietary patterns and their well-known inflammatory effects.
3) Last but not least: structure. Whole grains ain’t whole grains. The aspect that usually gets lost first when engaging in reductionist methodology of nutritional science is the three-dimensional, cellular structure in which nutrients are delivered within a whole food matrix. Usually it accounted for only as a factor in bioavailablity (e.g. carotenoids), but it may have effects far beyond this aspcect. By legal definition, whole grain products are all products made out of unrefined grains. However, the literal meaning would be a grain that is not milled to flour but still intact or coarsely cracked. Bread baked from grist instead of flour has a significantly lower glycemic and caloric load, because much of the starch that remains tightly contained within the cellular structure is indigestible and thus acts as a prebiotic fiber in the large intestine similar to resistant starch, further improving gut health.
Of course, eating some refined grain know and then won’t hurt – it’s simply a wasted opportunity to eat something much more healthy. I’m the first to admit, though, that I sometimes happily waste this opportunity in exchange for a delicious, crispy croissant. 😉
1. & 2. If someone’s diet consists entirely of grains, then what you say would have a significant effect. Who eats a diet of rice and nothing else whatsoever?
3. I totally agree. See http://nigeepoo.blogspot.co.uk/2010/02/problem-with-whole-grain-cereals.html
I don’t like orthorexia a.k.a. “clean” eating. As long as the diet is *based* on whole, minimally-refined animal & vegetable produce, there’s some wiggle-room for refined foods. 😀
Actually a huge number of people around the world DO live off mostly grains, sometimes for their entire lives. With very little in the way of vegetables. That is why the IIRC developed “golden rice” … to save the sight and lives of millions of children.
Oddly though, some of those grain-eaters are actually surprisingly healthy. Like this guy:
He’s from a culture that eats mainly sorghum, 3 meals a day. Other places in Africa eat mainly millet, or their own version of corn, or yams. Or peanuts or milk. One of the first questions one asks when meeting a stranger is, “What is your staple?” … I guess they define the culture by the main food. When you see the pictures though, the people are typically tall, with straight teeth and wide smiles … even when they are living at a barely subsistence level.
I haven’t yet seen a culture with healthy people living mainly off wheat or barley though. Even in the ancient Egyptian and Roman days … skeletons of the rich and the poor were both pretty bad. Even Oetzi, with all his exercise. The French are healthier than Americans, but not nearly as robust as your average Japanese mountain villager who lives off yams.
Well, in chapter 3 of Dr. Price’s “Nutrition and Physical Degeneration” he found the Swiss in perfect health eating mainly whole rye.
Major-General Sir Robert McCarrison’s “Studies in Deficiency and Disease” he found the Hunza eating mainly whole wheat, barley, maize, apricots and milk. He describes them as “unsurpassed in perfection of physique and in freedom from disease in general, whose sole food consists to this day of grains, vegetables, and fruits, with a certain amount of milk and butter, and goat’s meat only on feast days.” His findings are documented in Guy Wrench’s “Wheel of Health.”
Egyptians and Otzi had the unfortunate dental abscesses from millstone grit and sand which destroyed their teeth and their health. Difficult to know how they would have done without that issue.
Rice is so low in protein that I think of it as a “filler”, rather than a staple. Eating beans with rice improves the AA profile a lot. Tubers are good.
In the 1st world, the problem is over-consumption. For nearly 100 years, the 1st world masses have been manipulated to over-consume, as it keeps them happy & docile and it’s good for the economy.
Have you seen http://www.dailymotion.com/video/x2d29tf_the-century-of-the-self-part-1-of-4-happiness-machines_school ?
I agree, white rice is totally nutrition-less. Which is what makes the Kempner studies so amazing. Even more amazing to me is that the Chinese railway workers were noted as being MORE healthy on a diet of mainly rice and vegetables and dried octopus, than the Irish beef and potatoes guys. OK, the Chinese boiled their water and did less whisky! But still … they worked 10-11 hour days at hard labor on mainly rice, lived in hard conditions, and were noted for being “healthy”.
Billions of people live off mainly rice. They DO get nutrition problems if they don’t also get some vegies and protein too. But given that, they do fine and tend to be healthier than the people getting the Western diet.
I think the idea that scarcity protected people is mostly a myth. Comparisons have been done calorie-for-calorie with Westerners, for the same exercise levels. The Chinese often eat MORE calories for the same exercise level, and yet tend to be skinnier and healthier. Your average Japanese doesn’t go to bed hungry either, and is likely more healthy than the average American.
However, the Chinese have *less* tolerance for “The Western Diet”, whatever that is .. and get diabetes with less weight gain. It seems to have something to do with the actual food choices.
Asians appear to have limited Sub-cutaneous Adipose Tissue (SAT) hyperplasia, which limits fat storage capacity below the skin. As a result, Visceral Adipose Tissue (VAT) stores are filled prematurely, leading to the Metabolic Syndrome, as VAT deposits are much more metabolically-active than SAT deposits. This is a.k.a. “Skinny-fat”.
See http://nigeepoo.blogspot.co.uk/2012/06/adipocyte-hyperplasia-good-or-bad.html
The SAD/SED combination of refined carbs + fats results in fats being stored, as carbs are burned preferentially. A high-carb, low-fat diet suits Asians much better!
Having re-read what I wrote about Adipocyte Hyperplasia and the comments from June 2012, the following thought processes occurred:-
Adipocyte Hyperplasia occurs mostly during childhood, as that’s when rapid hyperplasia of other cells occurs a.k.a. growth.
A slim child which becomes a slim adult has few SAT adipocytes, predisposing said adult to get excess VAT rather than SAT if chronic over-eating occurs during adulthood.
A fat child which becomes a fat adult has lots of SAT adipocytes, allowing said adult to get rolls of SAT rather than VAT if chronic over-eating occurs during adulthood.
heathertwist said: “I haven’t yet seen a culture with healthy people living mainly off wheat or barley though. Even in the ancient Egyptian and Roman days … skeletons of the rich and the poor were both pretty bad. Even Oetzi, with all his exercise.”
Indeed there were healthy grain eating cultures that were observed in the early 1900s when various of prominent doctors were researching nutrition, at the time. The idea that grains are not a good food for humans comes from the “porotic hyperostosis” study of ancient skeletons. The bones of early farmers were found to have lesions which were thought to be due to iron deficiency as a consequence of eating grains instead of meat.
However, it only became clear a few years ago (2009) that the lesions were not due to iron deficiency, making the original hypothesis flawed.
The causes of porotic hyperostosis and cribra orbitalia: a reappraisal of the iron-deficiency-anemia hypothesis (2009)
So, the original hypothesis is obsolete—yet it is still used to claim that grains are problematic. The skeletal lesions were perhaps due to episodes of starvation or something else. We don’t really know. But, I’m not sure why grains would be assumed to be the only culprit of causing such lesions and skeletal issues. Now that the original hypothesis has been deemed obsolete, another explanation is needed.
Keep in mind that societies became larger, infections were more rampant, and food was scarce at times. Societies were adapting and there was a lot of turmoil. Mass starvation was also said to have happened as early farming practices depleted the soils to oblivion. Some say this turmoil and social stress is evident at archaeological sites like Göbekli Tepe and Caynou, where mass death, genocides or sacrifices appear may have happened.
Also the high levels of cavities in early Neolithic skeletons has been attributed to the wearing down of teeth from poor milling standards. Attrition broke the enamel, which led to dental abscesses and promoted cavities.
See: Teeth and Bread in Ancient Egypt (1972)
This is very different from the sugar-promoted cavities we have today. (Honey was their main sugar, but honey is believed to be protective of dental caries). Arteriosclerosis has been linked to dental infections. If we wanted to, we could probably link all of their health issues to poor dental health and starvation, but that too would be highly speculative. Incidentally even Paleolithic teeth have also been found to have significant wear and tear.
The point being is that it’s very easy to create a narrative both vilifying and defending grains by using ambiguous archaeology.
“Indeed there were healthy grain eating cultures that were observed in the early 1900s when various of prominent doctors were researching nutrition, at the time. ”
I would really like to see such a study! I’ve been looking. There are loads of healthy skeletons of “grain eaters” in general, just not wheat-eaters. Hard bran and everything, their teeth might wear down, but they didn’t have the soft enamel that has become common now. If you combine the soft enamel with sugar, it causes cavities. But most cultures don’t have soft enamel: just a few do, and those ones also have significant skeletal changes (crooked teeth, narrow mouth etc) which one associates with vitamin malabsorption.
It’s also not clear what the “prominent doctors” considered “healthy”. Price was rather specific: he counted cavities and took pictures of the dental arches! But the cultures he considered “healthy” were oat-eaters. And the Swiss, who ate barley bread. The Swiss also drank a lot of raw milk though, and it turns out that raw milk interferes with one of the factors in wheat that is a problem. Also, it turns out that the Swiss had gone through a big problem with goiter not long before Price studied them. The Swiss government started trucking in iodized salt because so many of the recruits failed their physicals because of goiter.
He did notice that English poor folk got healthier when supplemented with whole wheat bread, raw milk, and cod-liver oil. Which may show that whole wheat is better than white wheat, or that raw milk really does help, or that the vitamin involved happens to be in cod-liver oil. Anyway, the Chinese did fine on white rice and vegies and fish, for the most part, without extra raw milk or cod-liver oil.
The main reason I got curious about this was my daughter. Until she was 6, she ate a normal US diet, and her tooth enamel was really soft. “Sticky” as the dentist put it. She got cavities constantly. Then we switched from wheat to rice, and her next visit … no sticky teeth. Didn’t get any more cavities from that point, even though she ate (and eats) plenty of sugar.
So for some people, at least, it turns out that wheat messes with vitamin absorption and also with the gut biota, which is where Vit K is produced. I don’t know if it’s Vit K or Vit D or what else, but I think something is going on that interferes with skeletons and teeth.
It could well be that this happens a whole lot less with whole boiled or parched grains … those digest slower and feed bacteria less. The whole grains … of any type … also interfere with iron absorption but in general I think that’s a good thing (as was some level of hookworm!).
Anyway, sure, one can skew history, and skew statistics. But it’s a weak argument. Anyway, I’ve never made the argument that “grains” caused anything bad: just one or two particular grains which have weird effects on humans.
heathertwist said: “I would really like to see such a study! I’ve been looking.”
Are you not familiar with McCarrison’s observations on the Hunza? They ate a lot of whole wheat and milk and a few other foods, of course (even the bible says one cannot live on bread alone). McCarrison also did experiments on rats where he gave one set of rats a British diet (white flour, margarine, etc) and another set of rats the Hunza diet of whole wheat and milk. The rats eating a Hunza diet had no discernable disease. His study was done to prove that the success of the Hunza diet had nothing to do with genes.
Sir McCarrison presented his findings before the Royal College of Surgeons and his observations are summarized in the 1938 book, “The Wheel of Health,” by Dr. Guy Wrench. (Free on Google Books).
In his lectures, McCarrison remarked:
He was their doctor for 7 years and described them as one of the finest and physically fit races he had ever seen. The Hunza are no longer healthy now eating a modern diet.
heathertwist said: “There are loads of healthy skeletons of “grain eaters” in general, just not wheat-eaters.”
Well, if you dig into the history books, you’ll see that wheat was considered the healthiest and most revered of all foods. The word cereal comes from the name for the ancient Roman goddess, Ceres—the goddess of grains and agriculture. Ceres was said to have discovered wheat, and given the gift of agriculture to humankind.
Hippocrates not only recommended wheat bread, but experimented heavily with different preparations.
If wheat was so deleterious, you’d think that Hippocrates would have noticed it and warned against its consumption instead of recommending it for the prevention of disease.
Avicenna recommended bread as a key staple of the diet. Paracelsus believed that wheat had mystical properties, and Aristotle thought foods made from wheat suits our bodies best. A 19th century encyclopedia says that wheat is the most nutritious and most important edible plant in the entire vegetable kingdom. Surely if wheat was so terrible, we would see evidence in the history books.
Over 250 years ago, Swedish biologist Carl von Linné, the father of modern taxonomy and modern ecology, wrote two texts—Ceres noverca arctoum and De pane diaetetico—that were wholly devoted to bread and bread-making. Citing his own observations as well as those of the greatest medical authorities of antiquity, he wrote.
Von Linné also provided examples of how bread could prevent or cure specific diseases. Although rye was popular in his home country of Sweden, von Linné considered wheat bread to be “the most excellent of all.”
In the 19th century, Thomas Hodgkin, the prominent English physician and first to observe Hodgkin’s disease, wrote:
heathertwist said: “Price was rather specific: he counted cavities and took pictures of the dental arches! But the cultures he considered “healthy” were oat-eaters. And the Swiss, who ate barley bread.”
Actually, Price said the Swiss ate whole rye bread and milk. Price wrote:
“Anyway, sure, one can skew history, and skew statistics. But it’s a weak argument.”
I’m mainly pointing out that people often use the Neolithic skeletons to demonize grains when in fact nobody actually knows what actually caused the bad skeletons. If wheat were so problematic, you’d think somebody would have noticed this before white flour triggered the dyspepsia epidemic in the 19th century. Yet, everyone who wrote about wheat seemed to think it was the best thing since, well, sliced bread.
OK, some people say the Hunzas are awesome. I don’t see a lot of evidence for that … unlike the Okinawans, Sardinians, Japanese mountain people, Masai … where are the studies? One visitor did write a book about them and noted:
“As their diet is deficient in oils and vitamin D, all Hunzas have soft teeth, and fully half of them have the barrel chests and rheumatic knees of sub-clinical rickets.”
As paleoedge noted:
“But there is a problem with this climate theory; why did the Inuits maintain their darker tone? The reason is theorized to be because northern Europeans switched vitamin D rich meat for low-fat vitamin D deficient grain, while the Inuit maintained a vitamin D rich meat based diet without grains. It turns out, Dr. Cordain found out that wheat contains an anti-nutrient called WGA, a lectin that binds to cellular glycoproteins. Once in the gut, WGA binds to a cell receptor, and then a nuclear pore found in every cell in the body that blocks the transport and absorption of vitamin D. According to Dr. Cordain, WGA has a half-life of four hours, which means if you are sunbathing while consuming wheat, the vitamin D is most likely being blocked from the sun. Whoa!”
However, my grandmother grew up in Germany, and lived to be 96. Her diet included wheat, but really not that much … like the Hunza, there were a lot of other vegetables, lots of dairy, and limited meat. The grains tended to be mainly oats. They rarely got wheat growing up (it was for rich people) and it was a lower-quality wheat at that.
http://paleoedge.com/how-much-meat-plants-and-dairy-did-farmers-consume/
Actually there is a theory that white skin actually developed in the Middle East, as an adaptation to eating wheat. The white skin people eventually moved North, and I guess the people that live there now are better adapted (or just sickly: what are the caries rates in the Middle East?).
http://news.sciencemag.org/archaeology/2015/04/how-europeans-evolved-white-skin
“Then, the first farmers from the Near East arrived in Europe; they carried both genes for light skin. As they interbred with the indigenous hunter-gatherers, one of their light-skin genes swept through Europe, so that central and southern Europeans also began to have lighter skin. The other gene variant, SLC45A2, was at low levels until about 5800 years ago when it swept up to high frequency.”
Interestingly, Sardinia, which was one of the wheat-exceptions, appears to be no longer:
http://paleoedge.com/how-much-meat-plants-and-dairy-did-farmers-consume/
“According to Sarah Wilson who visited Sardinia with National Geographic, “the longevity phenomena seems to have come to an abrupt halt, even reversed. It’s almost like as soon as money came to the island (which it did about 50 years ago) the locals went from famine to feast, taking on the health consequences that come with abundance. Young Sardinians are incredibly overweight. And Sardinia has one of the highest incidences of celiac disease, I’m guessing from eating so much bread and pasta where the gluten content has shifted due to the more processed wheat strains available today.”
heathertwist, Duck Dodgers: I have also read that the health of the Hunza was not all that awesome, though it was better than most people’s health today. Like most native cultures, they did have an absence of diabetes, cancer and heart disease; however, compared to other native groups, they did have goiter, and a reasonable number of cavities.
heathertwist, I believe in another post you mentioned that you are a celiac? Me too! “Welcome to the club”. In researching celiac disease years ago, I remember reading that most of those cultures that did eat wheat traditionally also ate many more other grains, mostly gluten free, like millet or teff, buckwheat, etc. In other words, they varied their grains. It was stated that we as a culture today eat far more wheat than most cultures of the past, because we eat almost exclusively wheat. (For instance, I’m pretty sure I’ve read that the Hunza also eat buckwheat and millet). Some of these other types of grains have become obsolete, and few people in the West even know about them. (Apparently, wheat is more convenient to grow and transport). And my guess is that if the Swiss were eating lots of rye bread, it was most likely fermented sourdough; this would remove some of the anti-nutrients and make it more digestible- (I don’t know: Weston Price didn’t mention that they fermented it. However, wheat was traditionally fermented, so maybe he didn’t feel the need to mention it?) It could also be possible that drinking full fat milk, and/or eating meat (or cod liver oil) helps mitigate some of the harmful effects of wheat by replacing nutrients. So in other words, eating wheat in a traditional culture would be different from eating lots of wheat and sugar with low fat milk in a modern day culture.
In any case, wheat bread of the past was very different from modern wheat bread. Not only was the wheat different- (it was lower in gluten; the bread would have been flat, dense, and not “fluffy”)- it might have been fermented, and, nowadays, there are many shortcuts to bread making. Rather than relying on a long process of letting the dough rise, there are many additives that are used today to speed up the process. Not only are some of these additives questionable for human health, but also, in not using a slow, traditional process, it might make the wheat more deleterious.
Finally, I don’t think we can have a discussion about wheat without mentioning that which interests me the most: the opioid effects! Duck Dodgers, I wonder if many of these historical figures praised the benefits of wheat because it makes people “feel good”? It is definitely, absolutely addictive, like sugar; I see many people who are addicted to it, all around me. (I was addicted to it even while it was killing me). Some have even suggested that the widespread shift from hunting and gathering to farming may have had something to do with opiates and addiction. I find that theory very interesting……
“heathertwist, I believe in another post you mentioned that you are a celiac? Me too! “Welcome to the club”. In researching celiac disease years ago, I remember reading that most of those cultures that did eat wheat traditionally also ate many more other grains, mostly gluten free, like millet or teff, buckwheat, etc”
Well thanks! An interesting time to be part of that club … !
There is something interesting going on with the heritage wheat too. One of the aid organizations sent some wheat berries to a town that traditionally ate mainly wheat. But the kids developed celiac symptoms from the American wheat. It probably shouldn’t be toooo surprising … heritage corn and beans are sure different from the modern ones. But the heritage wheat didn’t seem to help the Egyptians or Romans, so it’s hard to say.
“And my guess is that if the Swiss were eating lots of rye bread, it was most likely fermented sourdough; this would remove some of the anti-nutrients and make it more digestible- (I don’t know: Weston Price didn’t mention that they fermented it. However, wheat was traditionally fermented, so maybe he didn’t feel the need to mention it?)”
I haven’t seen that rye and barley are anywhere near as harmful as wheat though. It is true that celiacs cross-react to rye and barley, but would a culture that ONLY ate rye and barley have the same issues? Celiac is a very specific kind of auto-immunity, but there doesn’t seem to be a similar kind of illness that is triggered by, say, millet or quinoa.
The “healthy Swiss” weren’t all that healthy either. They had a super-high rate of goiter until the Swiss government started trucking in iodized salt circa 1920.
Click to access idd_aug13_growth_and_iq.pdf
Now, my grandma grew up in a German village and she did live to a grand old age (96) with no heart disease, high blood pressure, tooth loss, etc. She didn’t get white wheat much as a kid (they got a slice per week as a treat) but she certainly ate it a lot, esp. cookies, when she came to America. But further, she was somewhat sun-phobic and kept the shades drawn, and covered herself from head to toe with long sleeves, high necklines, thick stockings, hat … which was traditional for her growing up. So I always wondered why she never got rickets? Or goiter, for that matter.
The answer appears to be that in her day, one of the favorite foods were fish. Pickled herring was big, and river eel, and even salmon. Another favorite food was mushrooms, which they gathered themselves in the local forests. Mushrooms dry and keep very well, and guess what? They are an incredible source of Vit D, esp. if they are sun-dried, and actually high in protein too. Cheap food for anyone who wants to gather them. Otzi was found with a string of dried mushrooms!
“Placing regular mushrooms in direct sunlight for an hour (winter) will generate your daily needs of vitamin D in a serve (100g or three button mushrooms – See more at: http://www.powerofmushrooms.com.au/health-nutrition/health-nutrition/vitamin-d/#sthash.SLdZIjq4.dpuf”
Price used cod liver oil as a magic cure of sorts, which would provide Vit D and Vit A (the two that tend to be problematic), and, I think, iodine?
So maybe that is part of the reason the Egyptians had more issues with wheat … it was too hot and dry there to have a lot of mushrooms!
” It is definitely, absolutely addictive, like sugar; I see many people who are addicted to it, all around me. (I was addicted to it even while it was killing me).”
Amen to that! I think this is one reason that there is such a strong reaction to the “anti-gluten” people. I mean, in our culture, we have people who won’t drink milk, won’t eat sugar, won’t eat meat, won’t eat chocolate unless it’s fair trade … I’ve gone on my share of food experiments. But the “no wheat” food experiment had people talking to me like I’d joined an evil cult and they got seriously angry.
Also though when kids stayed overnight at our house, they would start going bonkers at the end of day 2. Got headaches and had anger fits. One, her Mom reported, started screaming on the drive home “I have to have spaghetti!” so they stopped for food. There was not spaghetti so the girl had a meltdown. Mind you we DO have spaghetti and bread, and these kids were too young to understand that our spaghetti was missing the gluten part. But they definitely were going through withdrawals.
heathertwist- I had a look at the link you posted about the Swiss. They mention that some “alpine villages” had problems with goiter, but there was no mention of the specific valley that Weston Price visited, where the people were so healthy: the Loetschental Valley. It was a very remote part of Switzerland where the people still ate only traditional, natural food, whereas in most other parts of Switzerland the people ate very differently. As I recall, he made the distinction that the people in this valley were much healthier than the average Swiss elsewhere. So I’m still not sure about that; unless there is a link somewhere that states specifically that those people had goiter?- (but even if they did, it may be hard to find the evidence). So, who knows?
That was very interesting what you wrote about people getting sick when their heritage wheat was replaced by American wheat!
There is also the theory that in some African countries, where the people are starving and are fed government rations of wheat, some of those children who still look emaciated may be suffering form celiac disease rather than actual starvation. I think there was no proof of this, just speculation, but I hope someone is looking into this possibility. When people suddenly eat lots of wheat when it’s not part of their traditional diet, celiac is likely to occur.
Also, I guess that was a good point about rye and barley. Although they both have gluten, they are most likely not harmful in the way that wheat can be. I guess it’s possible that a culture eating just rye and/or barley may not have the same problems as wheat eating cultures.
Last thing about wheat: Denise Minger, in her “China Study” rebuttal, noticed there seemed to be a correlation between wheat eating groups of Chinese and heart disease.
The bit I read about the wheat berries in food aide was an actual report, not just an anecdote. But it was years and years ago!
Yes, Denise did an amazing job of analyzing The China Study in terms of wheat, rather than meat. It is the case worldwide that the places that grow wheat tend to also be the places that have cows or goats … they are the inland people! The coastal people can get food more easily by eating fish, and rice grows better in warm or wet places (wheat gets moldy easily). Inland people have other confounding issues too, notably lack of iodine and lack of fish. The more fish people eat, the statistically more intelligent they tend to be.
Cordain is saying that the WGA in wheat is what blocks the Vit D … not the “gluten” (gluten is a total misnomer, but the term has stuck!). WGA stands for “Wheat Germ Agglutinin” Barley and Rye have something similar, but I don’t know that it is the same thing. Try baking bread from barley or rye and you get the idea … they are really different.
I also don’t know to what degree raw milk blocks the process. Apparently it DOES block a lot of it, which might be one reason why raw milk got suck kudos as a health food. Drinking raw milk with your wheat might be the magic bullet-dodger!
“On another note, not only does wheat contain gliadin, which upregulates zonulin, which increases intestinal permeability, it also contains an obscure compound (thaumatin like proteins) which also increase intestinal permeability. Hence wheat represents a triple time bomb (gliadin, WGA and thaumatin like proteins) which maintain physical and physiological characteristics that almost certainly impair gut function, interact with our immune systems to produce low level inflammation, and impair vitamin D metabolism (not a vitamin at all, but a hormone having receptors in virtually every cell in the body).” (Cordain)
http://thepaleodiet.com/wheat-the-triple-time-bomb/#.VldSl3arTME
Interesting link! There’s a lot about wheat there.
I have also read about wheat and vitamin D, in other sources. (As well as the idea that white skin might be a recent adaptation to grain eating). It’s all very interesting.
There’s also some evidence that wheat eating might interfere with magnesium absorption.
Oh yeah, and I forgot to mention, that was totally fascinating about the children going through wheat withdrawal! Yes, I can believe it too. I’ve seen this kind of thing; (with sugar too). As wheat and sugar often appear together in foods, that’s a double whammy.
heathertwist said: “Dr. Cordain found out that wheat contains an anti-nutrient called WGA, a lectin that binds to cellular glycoproteins.”
Matt LaLonde, and many others, have questioned Dr. Cordain’s overlooking the fact that people do not eat raw wheat…
Even Dr. Ayers, an actual glycobiologist, says that cooked lectins are fine (see his user comments, below the post, where he discusses WGA).
heathertwist said: “On another note, not only does wheat contain gliadin, which upregulates zonulin,”
Actually, certain ancient types of tetraploid wheat (e.g.; Graziella Ra, Khorasan wheat/Kamut) have even greater amounts of total gliadin than modern accessions. Interestingly, during the 1800s, gluten (and gliadin) were considered to be the most nutritious vegetable compound. This may explain why cultures preferred wheat varieties with higher levels of gluten. For instance, Einkhorn was the least reactive wheat, and more reactive wheats were preferred by cultures, even during the Neolithic.
In the 19th century, doctors recommended gluten bread for diabetics. 6th century Chinese actually added wheat gluten to their foods as a protein source. It’s only been since about 1950 that people began to have problems with gluten. Of course, everyone blames “modern wheat varieties” but few seem to notice that wheat is now heavily processed (fumigated, reconstituted and sometimes bromated). Also, the protective oils often removed to improve shelf life. It’s a bit like adulterating, fumigating and removing the Vitamin E from a mongongo nut and wondering why someone eating those heavily processed nuts would have health issues.
heathertwist said: “which upregulates zonulin which increases intestinal permeability, it also contains an obscure compound (thaumatin like proteins) which also increase intestinal permeability. Hence wheat represents a triple time bomb (gliadin, WGA and thaumatin like proteins) which maintain physical and physiological characteristics that almost certainly impair gut function,”
Those who make this insinuation—that a temporary upregulation of zonulin promotes health issues—are often the same people who recommend using liberal amounts of coconut oil for cooking and eating. Ironically, these individuals don’t seem to realize that lauric acid, found concentrated in coconut oil, is known to upregulate zonulin and causes the same intestinal permeability that gluten does.
There’s little evidence that a temporary upregulation of zonulin is problematic in a healthy individual. For all we know, it may plat a role in oral tolerance.
Even celiac researcher Alessio Fasano explains that it’s no big deal for healthy people:
He goes on to explain that people with celiac secrete too much zonulin and their tight junctions stay open longer than it should.
Anyhow, it’s probably unhelpful wise to scare healthy people into fearing these normal processes, particularly when other popular foods, like coconut oil, have the same likely normal effect.
Uh oh….I do eat raw peanuts from time to time. But I don’t notice myself having issues with them at all. In fact, I’m normally quite sensitive to foods; I have trouble digesting most other legumes, even if they are soaked and cooked. Could it be that it’s personal, and our bodies react differently to lectins and other anti-nutrients?
Yeah, some groups have spent thousands of years adapting to wheat (and to milk!) and some groups have not. And some people don’t think they have any much reaction at all. There is just this amazing coincidence that the healthiest cultures are the ones with the least wheat, and that a lot of people drop wheat and suddenly feel a whole lot better. And things like the China Study. My prediction is it will be like say, “Sugar of Lead” … the rich Romans added it to their wine and no one could see any problem with it. Except rich people kept going crazy.
Anyway, lectins are not always destroyed by heat. Gluten for sure isn’t … the whole point of gluten is to get bread to rise. WGA maybe could be destroyed by cooking it enough, but apparently it is not:
“.whilst variable amounts of agglutinin were found in wholemeal pasta probably as a consequence of thermal inactivation during food processing..”
http://www.sciencedirect.com/science/article/pii/S095671350300104X
“The concentration of WGA in white flour is about 3 to 4 milligrams per 100 grams, whereas in whole wheat it’s 10 times that, it’s an order of magnitude higher. But at physiologic levels, we’re only talking nanogram concentrations in bloodstreams. We know from tissue studies, these in vitro studies, that cells respond at nanogram concentrations, so nanogram concentrations can easily be achieved by consuming 4 to 7 milligrams per 100 grams.”
So they are working with WGA as a drug-delivery system and it works it seems in really tiny amounts. There aren’t many lectins in canned beans, but there are some left in homemade beans, and it’s fairly common for people to get sick (and even die) from home-cooked kidney beans. Cooked bread has “variable amounts” of WGA in it, and some of it is inactivated by other foods with it. Or not. So the effect likely has to do with how it’s cooked, what you eat with it, and what your genes are. Hardly a glowing recommendation for a highly wheat-based diet.
Fasano is Italian, and hardly a health-food person. He’ll probably live a normal Italian life and get arthritis and heart disease at the usual age, like all the other Italians, who are in fact the most wheat-adapted. He likely takes Vit D pills or eats Vit D enriched foods too, and has his cavities filled like everyone else. He’ll get osteoporosis as expected as he gets older and likely a few root canals. So he’ll live longer than a celiac would who was eating wheat, and won’t live with a constant stomach-ache … and he’ll be able to eat Big Macs and pizzas, which is important to him. But will not live as long or be as healthy as the average Japanese mountain villager.
But what would his life be like if his Big Macs did NOT have wheat in them? (or added iron, for that matter). That is the question. The experimenters who are trying it out … the no wheat lifestyle … are beginning to answer that question. Maybe it’s just another odd dietary fad. Or maybe the non-wheat people will end up being quite a bit healthier. Right now we have these massively parallel food experiments going on with fat, sugar, meat, GMO, fish, and grains. I say the more the merrier … try something out, see how it works for you, and share with the rest of us.
“Could it be that it’s personal, and our bodies react differently to lectins and other anti-nutrients?”
It’s definitely personal, but our flora are likely responsible for much of our adaptations.
We find indigenous cultures take steps to minimize wild plant toxins, but wild plant toxins often make our domesticated foods look quite tame (domestication is a kind of toxin reduction). Their gut flora adapts to their diet.
This is a key point to understand because while on the surface we often don’t have the ability to digest certain foods, like dairy, seaweed, or grain toxins, our gut flora can quickly adapt to break down those foods. For instance, most Masai are lactose intolerant, but their flora adapts to their high dairy diet. Japanese individuals possess the genes for the consumption of the algal polysaccharide porphyran in their microbiomes, which are rarely found in North American and European individuals. We cannot digest phytate, but our flora can.
Plus most lectins and antinutrients are also known to have beneficial properties:
The dreaded kidney bean lectins have anti-fungal and anti-viral activities and lectins in general have anti-cancer properties too. Phytates have anti-cancer functions and therapeutic properties against diabetes mellitus, atherosclerosis, coronary heart disease and reduces kidney stone formation. Toxic glycoalkaloids, found in potatoes and nightshades, have been shown to offer antiallergic, antipyretic, anti-cancer and anti-inflammatory effects; blood sugar-lowering effects, and anti-pathogenic effects against viruses, protozoa, and fungi. Cyanogenic glycosides have anti-cancer properties. Phytosterols, polyphenols, flavonoids and tannins, alkaloids, phytates all have anticancer, antioxidant or endocrine normalization properties as well.
Notice a pattern? Antinutrients are not so black and white after all. They aren’t always bad. In the context of adapted gut flora, I suspect they help maintain homeostasis (i.e. a proper balance of what we might consider “good” or “bad”… yin/yang).
Duck Dodgers- thanks for the clarification about lectins (and other anti-nutrients. Actually, I had read that about phytates before, but I didn’t know it applied to the others). This explains why I feel fine with peanuts (though I eat them in moderation), as well as nightshade vegetables, of which I eat a lot of! Not only do I digest them well, but they don’t seem to be causing me any harm and I feel very healthy when I eat them. However, I’m not sure about the “adaptation” theory; though I had exposure to foods like wheat and soy for a good part of my life, I never “adapted” to them. I think it probably has to do with more than just damaged gut flora- (if anything, I think those foods might have caused damaged gut flora, in my case). And there are so many vegetables and fruits that most people think of as being benign and even healthy, that I can’t digest at all! Basically, I just go by how I feel, and screw all those conventional “recommendations”.
“There is just this amazing coincidence that the healthiest cultures are the ones with the least wheat”
Yes, an amazing coincidence that those who eat the most white flour are unhealthy. Like most anti-wheat sentiments, this statement conflates the difference between white flour eating cultures and traditional whole wheat. It should be obvious that any refined food is problematic, and wheat is the king of refined grains in the modern world.
The problem with that conflation is that it ignores the cultures that thrived on, revered and worshiped wheat. Prescribed by Hippocrates, Paracelsus, Avicenna, Aristotle, favored by the Spartans, the Greeks and the Romans, and observed by countless scholars who wrote about its health effects. In every single instance, throughout Western history, wheat was unanimously considered to be the healthiest of all foods by the most prominent medical authorities—and this sentiment existed until the industrial revolution.
Furthermore, gluten was discovered in 1742 and even through the 19th century was believed to be the most nutritious plant compound. Not only did most cultures prefer higher gluten wheats, but it’s only since the 1950s that many people began to have trouble with gluten.
Anyhow, the “amazing coincidence” would be like condemning all meats without recognizing that processed meats are completely different from eating whole animals. It’s misleading. If you’ve never seen how modern flour is made, it’s extremely processed.
Let’s not pretend that modern wheat milling is indicative of traditional wheat consumption. It’s common knowledge that bread is broken.
Good points. Qualitative, mostly-opinion statements like “the healthiest populations eat the least wheat” are problematic for many reasons: their qualitative nature; their failure to define what “healthiest” is; their failure to present any quantitative analysis; their dependence on apparent correlations, rather than establishing causative relationships; their failure to deal with confounding factors; and many others. Of course, the statements in support of wheat suffer the same shortcomings. And many of the assertions are made without any backup from the historical record. For example, sea vegetables are not a food that only the Japanese began to eat in quantity, and then only in recent times. Coastal peoples throughout the world have used them for many centuries.
Annie, yup. You wrote what I was thinking. So much assertion of unknowable things.
Qualitative? In terms of say, the Hunzas … there isn’t much data. But in terms of the China Study … it is much more studied. Also the Japanese mountain people. They exist NOW and aren’t hard to find or hard to study.
In terms of ancient peoples … we are getting good data now too. The plaque off Neanderthal’s teeth, or the contents of Oetzi’s stomach … yeah, we are understanding exactly what they were eating. The Romans kept records of what they fed their slaves, and we have the bones of the slaves to compare to. And of the nobles (a lot of them are full of lead!). The railroads in the 1800’s have exactly what they fed to their workers too, and loads of data about illnesses.
It’s basically an exciting time, I think. A lot of research is finally coming to a kind of “universal field theorem” of human nutrition. I’m not sure anyone knows where it will lead. Like Denise, I’ve gone down a lot of tracks in studying this, and I’m certainly not going to say “Hey, but THIS TIME I’m right!”. We should share though, because that’s how we get to the next step.
Absolutely, the statement I flagged as qualitative is exactly that. There are reams of data on many populations, but that does not make the statement. “the healthiest populations eat the least wheat” any less qualitative. Healthiest in terms of what criteria? Which populations were evaluated and by what criteria? Is there a positive correlation between quantity of wheat consumed and “healthiness”? If so, is it statistically significant? Is there a tabular or graphic illustration of the correlation? If such a correlation exists, what confounding factors may have influenced it? The statement as it was made is a classic illustration of a qualitative statement on the subject of diet and health.
“Is there a positive correlation between quantity of wheat consumed and “healthiness”? If so, is it statistically significant? Is there a tabular or graphic illustration of the correlation? If such a correlation exists, what confounding factors may have influenced it?”
And the problem is that the discussion around the qualitative statement usually goes like this:
Person A: Studies and published observations show that whole grains are considerably healthier than refined grains and refined grains tend to promote degenerative diseases.
Person B: There is evidence that wheat promotes chronic disease.
Person A: No, you found evidence that refined white flour promotes chronic disease. But we already knew that.
Repeat ad nauseam.
“Which populations were evaluated and by what criteria? Is there a positive correlation between quantity of wheat consumed and “healthiness”? If so, is it statistically significant?”
I’m basically pointing you to Denise’s excellent (and detailed) analysis of the China Study. There are books and studies that say more or less the same thing, though yes, most of them are not so detailed. The China Study though was of a large population, eating largely homegrown foods, in towns where the population typically ate the same kinds of foods day in and day out. Denise crunched the numbers. She does have the results.
“Wowza! By the way, wheat flour also correlates significantly with hypertensive heart disease and stroke, but I’m mainly going to look at coronary heart disease in this post. (And although wheat looks like it could have a nonlinear relationship with heart disease, with the highest wheat eaters having disproportionately steeper rates than non-wheat eaters, I’m going to treat it as linear for the sake of this analysis. That way, the worst that’ll happen is we’ll underestimate the potential effect of wheat, which—for now—is better than overestimating it.)”
http://rawfoodsos.com/2010/09/02/the-china-study-wheat-and-heart-disease-oh-my/
http://rawfoodsos.com/the-china-study/
I expect there will be a lot more hard data in the next decade or so, esp. as so many people are doing their various “diet experiments”. All those n=1 experiments do add up eventually. There have been some interesting studies though, done on correlations between, say, anti-gliadin IgA and the prevalence of certain diseases. Or the percentage of people whose symptoms get better on a non-wheat diet even though they are not celiac. Anyway, they are detailed and there are dozens of them.
http://www.ncbi.nlm.nih.gov/pmc/articles/PMC4015193/
Click to access Parrish-June-15-2.pdf
Duck, you say to Heathertwist: “…One could easily create any narrative they wanted to with such vague clues. I’ve often wondered if the whole point of Paleo™ is to base a particular diet on extremely ambiguous data.” This to sum up your words on Oetzi, how there are many factors, not just diet, that affected his health…”
We can say the same about early grains! Even early grains may well have been much less healthy for us than a hunter-gatherer diet.
In an earlier post, you say: “…cultures that thrived on, revered and worshiped wheat…” Duck, we don’t need to fact-check your comment to know that the “thrived on” assertion is unknowable at best. And certainly suspect.
No question, the Ag Rev allowed humans to civilize. Our planet’s population explored 2500x since then. But because calories became much easier and more reliably available doesn’t mean they made us *healthier.* We have evidence for the opposite:
http://www.ncbi.nlm.nih.gov/pubmed/21507735
“…empirical studies of societies shifting subsistence from foraging to primary food production have found evidence for deteriorating health from an increase in infectious and dental disease and a rise in nutritional deficiencies…”
And this from Pulitzer-Prize winning anthropologist Jared Diamond (http://www.ditext.com/diamond/mistake.html):
“…The farmers gained cheap calories at the cost of poor nutrition, (today just three high-carbohydrate plants — wheat, rice, and corn — provide the bulk of the calories consumed by the human species, yet each one is deficient in certain vitamins or amino acids essential to life.)…”
Duck, about this you say:
“… Prescribed by Hippocrates, Paracelsus, Avicenna, Aristotle, favored by the Spartans, the Greeks and the Romans, and observed by countless scholars who wrote about its health effects. In every single instance, throughout Western history, wheat was unanimously considered to be the healthiest of all foods by the most prominent medical authorities—and this sentiment existed until the industrial revolution…”
Even if fact-checking bore out your high-flown assertions, should anyone be surprised if early prominents did extol wheat’s virtues? If you had a choice to eat nutritionally inferior food or to starve to death, which would you choose? That quickly became the option in many places after the Ag Rev when human population started exploding and developing large permanent communities, creating an absolute need for the most abundant reliable easiest-to-obtain calories. No government could possibly recommend against wheat–even to the current day. And of course the medical authorities from Hippocrates on up to the 1970s when the McGovern Committee developed the US’s disastrous dietary guidelines, they all lacked sufficient data on wheat to make properly informed pronouncements on it. Back in the day, they lacked blood serum tests to measure inflammation biomarkers, they lacked sophisticated IT to do large epidemiological studies, they lacked the basic nutritional biochem we know today. People usually didn’t live long enough for chronic disease to clearly manifest–until the past century. I submit to you that, over the 10–12k years from the Ag Rev, only now are we able to begin to properly assess wheat’s true health effects–even apart from all the processing such as fortification–which you so correctly point out.
heathertwist said: “or the contents of Oetzi’s stomach … yeah, we are understanding exactly what they were eating”
I think the problem is concluding skeleton/health conditions based on mainly diet when other factors are known to have a significant, or even greater, effect on bone and joint health. Many ancient civilizations and cultures had to deal with famines and plagues, and dental attrition which promoted abscesses and infections, and poor growth, etc. all of which may have had a significant effect on their skeletal remains and health. To link those problems to mainly diet alone can be more than a little misleading.
Case in point, it’s been insinuated that Otzi’s poor health and skeletal remains may have been due to his diet. However, Otzi was known to have dental attrition, was genetically pre-disposed to heart disease, and a rather serious infection (possibly the oldest known case of Lyme disease) that may be linked to poor skeletal and joint status. His diet was the least of his problems. He was a very sick individual.
One could easily create any narrative they wanted to with such vague clues. I’ve often wondered if the whole point of Paleo™ is to base a particular diet on extremely ambiguous data.
“We can say the same about early grains!”
Of course. I only pointed out the historical and written evidence to show that the anti-grain evidence is inconclusive at best, and misleading at worst. Nobody can ever really prove anything one way or the other. Though, I doubt it helps anyone to only have an anti-grain sentiment given the extremely vague data we are dealing with.
“Even if fact-checking bore out your high-flown assertions”
Please. I’ve already given the sources here.
Do note the references showing that bread, and specifically wheat, was considered to be the healthiest of all foods right up until the mid-19th century when plenty of other foods were available. The idea that grains are an ideal food is not just an ancient belief. The belief lasted right up until the industrial revolution when prominent scientists like Carl von Linné (1757) and Thomas Hodgkin (1841) documented the well known health promoting effects of (wheat) bread. It hardly seems like something we should easily dismiss—we’re talking about actual written opinions based on actual observations, all spanning thousands of years.
“People usually didn’t live long enough for chronic disease to clearly manifest–until the past century”
Let’s not conflate life expectancy at birth with life span. Hippocrates lived to between 83 and 90 years of age. Aristotle lived to 62. Von Linné lived to 70. Medieval scholars had an average lifespan of 59–84.3 years in the Middle East and 69–75 in Islamic Spain. New England colonists had lifespans of 62-65 years. Is that not long enough for chronic disease to clearly manifest? Spoiler alert. Eventually we all die. 🙂
Duck, very interesting observations on wheat, thanks for your comments. A few questions if you have some time.
1. Do you think that white flour is a problem and whole wheat is ok, or it doesn’t matter, any wheat flour is ok? Perhaps the milling process is what makes the difference?
2. I’m curious, do you have any theory on why americans are getting fatter and fatter and more and more people world wide are having Diabetes? If it’s not wheat, then what? Do you blame sugar or simply too much calories? and if it’s increased caloric intake, why did it happen?
Thanks.
It should be painfully obvious by now that unsaturated oils are the driving factor in the obesity AND disease epidemic. Secondary would be added food fillers such as fortification, lecithins, gums, dyes, etc.
Bottom line, if you eat real food and real food ingredients, life will be ok.
Zach, what is real food? is sugar real food? is flour real food? Is broccoli real? And if whole grains that are milled are real food, then why oil extraction from grains is not real food?
Hi Anna. I surfed through the forum (yet again) this time to revisit your other comments, including your exchange with Neisy. So I’m smiling in the possibility you include rhetorical elements in your questions to Duck’n’Zach 🙂
In any case, why don’t I take a crack at your Qs?
About your Zach Qs, it’s hard to know exactly what he means when he says “unsaturated” oil. Does he include the monounsaturates which, after all, qualify as “unsaturated?” Including that Mediterranean Diet darling, olive oil? From my reading and tracking my food and health numbers for the past nine years, I’m quite disposed to the idea that an overabundance of omega-6s polys you usu find in the SAD (Standard American Diet) could be raising systemic inflammation and setting the table for chronic disease. Legume/nut/seed oils (e.g. from soybean, peanut, corn, and sunflower seed) are exceptionally high in omega-6 (w6) and these are products most people consumed till researchers devised cost-effective ways to extract these oils in the late19th c and turn of the last century. Before then, people mainly used lard and suet (tallow). In this sense, what Zach may mean by “real food” is a food that has not undergo novel refinements, such as those hexane-processed high w6 oils which he may consider to not be “real foods.” But of course Zach should answer for himself. Back to olive oil, it has a long history and it is relatively low in w6. I used it almost every day. I get extensive blood panels every three months and check my blood sugars throughout the day, and all my number remain quietly in the normal zone, and I’m now 55. Many of my numbers were well out of whack when I was 46 and was diag’ed T2D. These have since steadily improved, most of all my BGs, which are now normal (mostly 75–95 mg/dL), and my C-Reactive Protein, a popular biomarker for systemic chronic inflammation, which steadily dropped over 3 years from from 4.6 (inflammatory) to 0.6 (anti-inflammatory). In fact, all my blood panel numbers are now normal.
As for your Duck Qs, my take is that we should regard warily *all* wheat flour. White flour, for the very fast carbs/gluten/lectins and loss of nutrients replaced by fortification plus chemicals introduced in its processing, the potential downsides of which Duck amply covers through the forum (search on “fortification”) Whole wheat includes the bran and comes with its own concerns, e.g. phytic acid that, in your GI, can steal essential minerals from your food. Though some will argue that, in the case of iron which we too often get too much of, phytic acid could be a *good* thing. You can find detailed explorations of this here: http://www.marksdailyapple.com/why-grains-are-unhealthy/ and of course in Wheat Belly and Grain Brain. For my part, I quit grains early on (2007) simply because grains are high in carbs–long before I faced the additional health questions of gluten, hemoagglutenating lectins, and phytic acid. I wrote a spreadsheet to track my meals, keyed detailed nutrient data into it from the USDA Nutrient Database (a tremendous resource if you get a chance to play with with it: http://ndb.nal.usda.gov/ndb/foods), and found I could easily get all my micronutrients (vits + mins) without eating a single grain. Again Anna this is just my n=1. Please get as many health checks as you can, as often as you can. I can make specific suggestion for you on that if you want.
Finally your Q on why Americans are getting fatter and fatter and more and more people around the world are developing diabetes. I suspect this is very multifactorial, going way behind wheat and the threadbare “too-much-food/too-little-exercise” trope. We live in an unprecedented bewildering era of change. America was already well on its way to becoming sedentary in the 1950s/60s, and still much slimmer then. HFCS arrived to the US in 1975, and we kept upsizing sugar water esp since HFCS was so cheap. Chemical companies also keep creating new compounds, many of which are estrogenic and so promote metabolic syndrome–I can give you the proposed mechanistic chain for that for you if you want. Then there’s widespread use of antibiotics which can profoundly disrupt our microbiome, more and more violation of our circadian rhythms through working night shifts, and many many many other factors. Mark’s Daily Apple does an excellent job discussing these elements, http://www.marksdailyapple.com. And of course, I look forward to Zach and Duck’s answers, should they decide to respond to your questions.
Hi, Anna. To respond, I suppose real food would constitute foods that we can consume and get a net positive in terms of nutrition and also that are unadulterated with man made substances, i.e. they came from nature and required little to no preperation to eat. I would say that use of fire for cooking, rocks for pulverizing, water for soaking, etc is probably as far as one should go for prep.
So to answer your questions, no I don’t think that refined sugar or refined grains should be considered food, yes they are edible and give us calories but in terms of health, they are a net negative. Natural sources of sugar however (honey, cane, maple, etc) are probably healthy, same for whole grains which require little more than a rock, water and heat to eat.
Oils are anempty calorie and net negative. Before the industrial age, oil was hardly ever consumed and rendered fats were the norm. Of course it’s not completely black and white and not all oils are created equal. I would take an expeller pressed oil from a whole real food (coconut, olive) over a machine and chemical solvent extracted oil from a non edible food any day. (Cotton seed, rape seed, canola, etc)
Zach, your definition of real foods is very subjective and biased.
I think if one would eat a lot of honey and maple syrup, it will have a similar effect of eating a lot of table sugar. Btw, one can make sugar with water, flame and rocks.
it’s highly debatable what “net positive” is in terms of nutrition. We can’t possibly know how to calculate this.
Most of the veggies we eat are modified and bread by humans and required much more then water flame and rocks.
You can have expeller pressed canola oil, would it make it healthy? It has lots of omega-3s and some people consider it healthier then olive oil:
http://www.rd.com/health/the-great-olive-oil-misconception-dr-ornish-responds/
Whatevers clever, you can worry and fret, I’ll eat the grains and sugars and be lean, energetic and happy.
Done with this blog till the next post, love the carb love!
Zach, all the best to you. Too bad you avoided the discussion.
Bryan, thanks for your reply 🙂
To your point about fats, Zach doesn’t seem to like detailed discussions and precise definitions. It’s easier to debate this way.
You can see my view of why the world is getting fatter and fatter in my reply to Duck. It’s somewhat similar to yours. I’m not convinced about antibiotics because I’ve met many people who basically eat them for food, yet are very thin.
Thanks for sharing your health history, my experience was very similar, although I didn’t have diabetes or major health issues. I certainly feel healthier and more energized eating LC, even compared to whole soaked sprouted grains/nuts and freshly milled oats ala dr. Price. And I have objective markers to back it up. My fasting insulin is 1.8, triglycerides are 40, down from 135, CRP is 0.4. So high fat diet hasn’t increased my inflammation markers.
What other tests or health checks do you routinely do? Have you ever tested your leptin level?
As you’ve seen from my previous posts, thanks for reading btw, I’m leaning towards thinking that
CR and protein restriction matters more then the type of nutrients for the most part and if one has a metabolism that’s not damaged. But subjectively I enjoy LCHF diet more then HCLF (I prefer bacon to beans) and it’s easier for me to maintain it. For me LCHF is naturally CR and hunger is very rarely present compared to HC, when I felt the need to snack all the time.
How many carbs do you eat normally? And what do you think about ketosis long term?
Thanks!
Hi Anna, you’re very welcome. I like your style 🙂
About Zach, if you search for my handle in this forum, you’ll see the exchanges I had with him earlier and then finally put an end to, concluding it was a sheer waste of time. I find it’s pointless to argue with anyone who’s long on religious fervor and testosterone and short on science. Zach doesn’t want an genuine discussion and sharing of ideas that don’t jibe with his own. He just wants to beat into you how great HCLF is and how everyone should do it.
About what you say: “I’m not convinced about antibiotics because I’ve met many people who basically eat them for food,…” When you get a chance maybe clarify that? At the moment I’m picturing waifs honking down handfuls of Cipro caps 🙂
Once I left grains (July 2007) I left them totally, not even trying things like fermented teff which seems to work well for Ethiopians. That’s not because I harbor an anti-grain dogma–I don’t–as I’ve explained in posts to Duck and others. It’s only because I’ve never felt a compelling need to seek out fermented heirloom grains. My grain-free LCHF foodway, mainly organic and pasture-raised locally produced foods, satisfies me utterly. But I’m certainly open to trying fermented heirloom grains and see how I fare with them. I completely agree that CR transcends the HCLF/LCHF debates–esp for people who are not yet deep into metabolic syndrome.
About my carb intake, I usu eat ~40–80g per day. Some days it’s zero (fasting), Occasionally up to 100-120 grams during the summer when the high-sugar fruits ripen. In the latter case, I just put up with my higher BGs (110–135 post-prandrial)
About ketosis long-term, I simply haven’t seen a compelling argument against it.The only reason to eat carbs is for the glucose, and our bods make plenty for our needs, esp from excess protein. ~ 75% of the excess protein we eat, our liver makes glucose out of it. The only exception is when doing extended resistance training, like free weights at the gym, working out regularly to fail, trying to put on muscle mass. In that case I found I needed to chow a high-fast-carb meal within 45m after the workout in order to continue to grow muscle mass. In those cases, my post-meal BGs would often be in the 60s, even after a 100+ g carb meal! But this post-resistance recovery meal is the ONLY exception I’ve found for me for eating carbs.
Most of all, Anna, I’m very glad you get plenty of health tests. I truly feel that’s our best shot to learn what actually works for us. There’s so little true science out there, and of course it can’t account for individual metabolic diffs. I’m still eager to read research papers and listen to people steeped in the field, be they formerly credentialed folks or autodidacts. But ultimately it is for the ideas, for things to investigate further and to try. You also find plenty of caveats and shortcoming in the tests, but you learn to cross-ref your results, not to read too much into any one result. In this fashion we straggle and crawl toward something that might resemble the truth 🙂
For my tests, at home I check weight/BF%/BP/HR in the morning, and test BGs 4x/day, including at peak post-meal times. For blood panels, beyond the usual CBC, lipid panel, liver and kidney enzymes, etc. lineup, I get these:
– C Reactive Protein. Which you get. Congrats on your anti-inflamm 0.4!
– Hemoglobin A1c. Avg blood sugar over 60–90 days. Useful because you can have a normal FBG and still too-high post-prandrial BGs. Ideally <5.0%
– C Peptide. Proxy for basal serum insulin. S/b <1 ng/L adj
– Iron panel (TIBC, Transferrin, etc), since systemic iron overload *is* a common prob, and I eat meat and cook in cast iron
– T3 and T4 for Thyroid. TSH can give a false reading.
– Mercury. Get one to check, then repeat IF you eat a lot of fish high up on the thophic scale, e.g. tuna, king mackerel.
– Consider for other heavy metals too, e.g. lead, cadmium, selenium. If you eat lots of shellfish and esp if you eat lots of Brazil Nuts, you may want to check selenium.
About Lipid testing: the current standard is woefully inadequate and uninformative. It measures just total trigs and c'stol, and gives no idea of the number of size of the lipoproteins these lipids travel in though serum. Many researchers consider certain of the lipoproteins–not their lipid cargos–to be the actual atherogenic elements coursing through our blood. Esp older, smaller more highly oxidized LDL and–yes–HDL–lipos. The current direct-lipo measure tests like VAP and NMR may still not be ready for prime-time. Mark Sisson discusses them here: http://www.marksdailyapple.com/how-to-interpret-advanced-cholesterol-test-results His post is already a few years old, but it's a good starting point.
Finally about leptin. I haven’t been able to wheedle this out of my doc, but I admit I haven’t pressed that hard either. I fast frequently (18h–3d) and almost never feel an acute desire to eat. At this point I can go pretty much as long as I want without eating, and feel fine, though I don’t see a point to go beyond three days. –Bryan
Bottom line bro is that you feel the need to writ short story sized posts that I bet are directly inverse to how healthy you are. I have great health and don’t feel the need to argue or post a mountain of studies yo get my point across.
I have read mountains of information and none of it makes a hill of beans compared to achieving true health. True health comes from being able to utilize carbohydrates, plain and simple. One can never be truly healthy restricting calories or carbs. Sorry but that’s the plain truth. You guys and girls restricting macros, fasting, searching out heirloom fermented teff (lol) will never experience true health until you get to the root issue of being under carbed.
Sure Zach. How you feel, etc.
Zach, my carb deprived brain can’t handle your comments full of assumptions, vague statements and lack of coherent thought process or quality references. May be my brain doesn’t have enough glucose to truly understand your point. So I hope you forgive me that I will not reply any further to your comments. Let’s agree to disagree.
Bryan, thanks for Zach warning 🙂
To clarify my antibiotic point, it was a gross exaggeration on my part. I meant to say that they take antibiotics so often, it’s almost like food. I think the gut flora influence on our health is grossly exaggerated as well. It’s a new FAD. I’m not saying it doesn’t matter, I’m saying it doesn’t matter as much for the vast majority of people compared with other abuses they take, especially metabolic syndrome.
My concern about ketosis is the lack of test subjects, so to speak. Inuits being a strange genetic exception, no population has subsisted in a constant ketosis for a prolonged amount of time, so we simply don’t know. That’s why I try to stay on the edge of it, coming out of it periodically with protein and carb binges, which are fun anyway.
I’ve noticed similar results to yours after my resistance training, although I’ve never had BG in the 60th!
I used to test my BG often, I’ve kind of relaxed and stopped it now for the most part and test occasionally after a carb binge to see it around 135-145.
I did ferritin testing as well, love cooking in cast iron! and had to do a few blood donations to bring it down to 80 from 140. I’ve heard lots of bad thing about iron, so trying to keep it at a lower range point.
I eat lots of sardines, salmon, shrimp, so not much large fish at all, thanks.
Also, how do you check for selenium? do you mean too much of it? I don’t eat much nuts, but take selenium 1xweek.
I agree on cholesterol testing, I don’t put much faith in it at all.
Thanks!
Hi Anna. Glad to save you some time and frustration 🙂
About antibiotics, those are one of the very many novel inputs in our lives that came along post WWII. Starting ~ decade ago, researchers started showing great interest in it as shown here: http://hmpdacc.org/ Michael Pollan wrote a compelling piece on it too:
There’s some though that gut microbes help mediate insulin response and blood sugars though it’s mostly correlative at this point, such as what you read here:
http://www.the-scientist.com/?articles.view/articleNo/41033/title/Sugar-Substitutes–Gut-Bacteria–and-Glucose-Intolerance/
Mechanistically flora mediating BGs and insulin response is a plausible idea because so much of proper blood sugar regulation is about proper *signaling.* You can have plenty of insulin output and even decent insulin sensitivity, and still have BG issues.
You can think of our bods as a large corporation and those trillions of microbes as little temps workers which our bod gives room and board and “hires” and “fires” at will depending on the specific and ever-changing tasks it needs done.
About persistent ketosis, you’re right we haven’t seen much of it in the Ag Age starting ~12k years ago. We have many questions, many of which research may never be able to answer. E.g. can we all still thrive in persistent ketosis? If not, did some of permanently lose the ability to thrive in persistent ketosis since the dawn of Ag, e.g. through one or several SNP mutations? Or can those Ketosis intolerant people become tolerant once their gut microbiome adjusts. As for the Inuit’s genetic exception, I hope people don’t read too much into that. The Inuit may be much closer to us than some believe. Just because the Inuit have SNP variants that *may* (and I emphasize *may* since we have not directly tested this) preferentially direct dietary fat to skeletal muscle and brown adipose tissue doesn’t means the rest of the world will fare poorly on a high fat diet. E.g. it could be we have evolved more robust ways to vet dietary fat in the GI and send the excess to the exit, i.e. not bring it systemic. Bottom line, again, keep observing your own experience. I’ve been in steady ketosis almost nine years. I still regularly get as many tests as I can and monitor myself, and have been doing and feeling terrific.
About my low post-resistance-training BGs, they may have been a combo of keen insulin sensitivity brought on by my intense 90–120 minute workouts and my unstable sugar control due to my early and mild diabetes. It’s not uncommon for early diabetics to get slight hypos even without taking meds. Again, that could be due in part to bad signaling, possibly from unbalanced gut biome. Fortunately, I never get the “feak and weebles” unless my BG dropped below ~44 mg/dL, which happened only a handful of times. When I stopped taking supps, including chromium picolinate, I stopped getting those super low BGs.
About the fish you eat, excellent! Funny how many fish low on the food chain are also high in Omega-3, like the salmon and sardines you eat, herring, smelt, and other cold-water species. I eat shrimp too when I can find it (and afford it) wild. I totally avoid farmed raised shrimp as those ponds are often polluted, sometimes with heavy metal laden effluent from factories, esp in China. See Taras Grescoe’s book “Bottomfeeder” for scary details on that.
About serum selenium, I don’t check for it because I stopped taking all supplements in 2009–I could fill a book with the reasons why I stopped supps!–and I limit the only food source that’s outrageously high in selenium, which are Brazil Nuts. Selenium’s one of the easier minerals to overdose on, and supp makers occasionally flub up the formulations with tragic results:
https://www.lawyersandsettlements.com/legal-news-articles/case/total-body/ –Bryan
Regardless of how you interpret their SNPs it would be at least worth pointing out that the Inuit have never been observed to be in ketosis.[1][2][3][4]
The one exception was Heinbecker showed in his follow-up experiments (in 1931 and 1932) that even (non-Pregnant/lactating) Eskimos who regularly ate carbohydrates had difficulty making ketones.*
Before their unique genetics were discovered, it was stated by the researchers that they were not in ketosis due to a high protein diet. However, the genetic evidence on CPT1a now explains why they had difficulty producing ketones and why Inuit children have difficulty fasting. (aka “hypoketotic hypoglycemia”).
Anyhow, I think it’s worth pointing out to Anna that the Inuit are not an example of a population in perpetual ketosis. They clearly metabolize fats differently than we do and they do not exhibit ketosis as we do.
* Pregnant/lactating women have exaggerated ketone production and the pregnant/lactating Eskimos in Heinbecker’s experiments made more ketones, while fasting, but were still well below what we would expect from pregnant/lactating women.
Hi Duck. What you say here: “I think it’s worth pointing out … the Inuit are not an example of a population in perpetual ketosis.” So far I’m left with a much different impression. That 1972 paper suggests the test subject Inuit *are* indeed ketotic.
It’s important to note someone could be in ketosis *at relatively low serum ketone levels.* Just like certain lucky folks can be in glycolysis and still enjoy low blood glucose levels. It’s possible that, due to his/her genetic variants and/or other adaptations and conditions, an Inuk may well be in ketosis even when serum ketone levels appear relatively low–low enough to show negative on test strips.
For the record, here’s a couple of ketosis defs: WebMD defines it as “…a normal metabolic process… your body … burns fat instead [of carbs]…”
http://www.webmd.com/diabetes/type-1-diabetes-guide/what-is-ketosis. The Wiki (http://en.wikipedia.org/wiki/Ketosis) says: “Ketosis is a metabolic state where most of the body’s energy supply comes from ketone bodies in the blood…”
OK, back to that 1972 paper. It has the most recent research of your links. http://ajcn.nutrition.org/content/25/8/737.full.pdf I started with it with the idea that study results are the most accurate due to ongoing improvements in medical testing and diagnostics.
Duck, the paper never mentions “ketosis” or “glycolysis.” But the authors sure do imply ketosis. They say “…[The negative ketone body test result] does not preclude an increase in ketone body production during this time…” and “…the Eskimos had high serum FFA and low glucose levels (approximately 65 mg/100 ml) indicated that free fatty acids played a major role in body energy production…” Reading this, given their high level of serum FFAs, the subjects sure don’t seem glycolytic. What else could they be then except ketotic? –Bryan
Bryan, I’m well aware that they burn a lot of FFAs in other areas of their bodies. And I’m aware of ketoadaptions. But the genetics clearly explain how they could not burn much FFAs in their livers like we do—they literally have a deficiency of the liver enzymes to do this—hence their known tendency for hypoketotic hypoglycemia.
wbryanh said: “Reading this, given their high level of serum FFAs, the subjects sure don’t seem glycolytic. What else could they be then except ketotic?”
No one denies that they burn a lot of fat for heat. But the point being that their livers appear to be protected (or at least spared) from metabolizing a lot of FFAs due to their CPT1a mutations. They just don’t do ketosis like we do. And the studies show this as well. They evolved differently than we did, due to their harsh climate.
Duck, let’s be clear. Your evidence, however interesting, in NO WAY indicts persistent ketosis. Your assertions “the Inuit have never been observed to be in ketosis…” and “…the Inuit are not an example of a population in perpetual ketosis.” are misleading at best, and most likely wrong. Inuit on VLC foodways most likely *are* in persistent ketosis. You even lean toward that in places. E.g. in your previous post you appear to contradict yourself by saying: “…[The Inuit] just don’t do ketosis like we do.”
Persistent ketosis may well remain a terrific option for Inuit and non-Inuit alike. Here’s why:
In their 1972 report–by far the most relevant of the five links you supply–fully describes ketosis, however “hypoketotic” it may be. http://ajcn.nutrition.org/content/25/8/737.long
Ho et al observed in the serum of those 168 Inuit “high FFAs” [free fatty acids], and “low BGs.” Sorry, Duck, but that’s ketosis. The only other energy-burning option is glycolysis, and given the high serum FFAs in these healthy test subjects, it sure isn’t glycolysis. Even the authors allow their results “do not preclude an increase in ketone body production during this time. Again, Duck, someone can be in ketosis even *at relatively low serum ketone levels* so long as glucose is not their primary fuel at that time.
What you say here: “…their livers appear to be protected (or at least spared) from metabolizing a lot of FFAs due to their CPT1a mutations…” You imply that that CPT1a mutation somehow evolved with the aim to prevent overloading and burdening the liver with FFAs. Please remember Duck this implication reflects your opinion. *It is not fact*. Even for folks lacking the CPT1a variant, you’ll find little evidence that a ketotic diet, even long term, burdens and harms their livers. There’s plenty of evidence to suggest a long-term ketotic diet does not harm the liver at all: e.g. here: http://www.hopkinschildrens.org/high-fat-ketogenic-diet-to-control-seizures-is-safe-over-long-term.aspx Duck if you can present strong evidence to the contrary, I’ll gladly stand corrected. The Inuit CPT1a variant may have evolved for reason having nothing to do with purported liver sparing. Many ancestrally-living Inuit lived on subsistence VLC foodways in intensely cold environments requiring huge amounts of calories just to generate enough thermal energy to survive. It’s quite plausible that CPT1a may have stuck in order to direct more FFAs to the skeletal muscle and brown adipose tissue. We simply can’t say for sure what specific selection pressures drove the spread of this variant in the Inuit.
Bottom line (again!): Whatever foodway–HCLF, HFLC, “Swampland,” whatever–get regularly tested and see how you are doing. If anyone happens to have any qualms about persistent ketosis, please regularly test your liver enzymes and your blood for FFAs and ketone bodies. Get a ketone testing meter or ketone test strips. Easy enough to do. You absolutely shouldn’t let these Inuit studies dissuade you from exploring any foodway, including VLC. The still meager, poorly understood, and caveat-filled results we see from the Inuit studies–many from 70 or more years ago–no way confirms or even strongly suggests any danger of persistent ketosis for us. –Bryan
Relax, Bryan.. Nowhere in my comment did I ever say that the Inuit didn’t burn FFAs. And nowhere in my comment did I ever say this proves anything good or bad about ketosis. I could care less.
All I said is that they don’t do ketosis like Westerners do.
Do you deny that most Inuit have CPT1a deficiencies? Do you deny that a CPT1a deficiency tends to cause hypoketotic hypoglycemia?
That’s just what the research says about the Inuit. That’s all I’m pointing out. They do ketosis differently from the way we do. That’s all.
Duck why do you ask me these two questions?:
“Do you deny that most Inuit have CPT1a deficiencies? Do you deny that a CPT1a deficiency tends to cause hypoketotic hypoglycemia?”
If you had read my post carefully, you’d know I don’t deny either one.
What is your point? How are these relevant to the main message. That we should feel free and safe to experiment with persistent ketosis?
Bryan said: “Duck why do you ask me these two questions? If you had read my post carefully, you’d know I don’t deny either one.”
Ok.. just wasn’t sure if you were acknowledging it or not. Understood.
Bryan said: “What is your point? How are these relevant to the main message. That we should feel free and safe to experiment with persistent ketosis?”
Yes, people should feel free to experiment, if they wish. They just shouldn’t be doing it under the pretense that they will be burning fats like the Inuit do. The Inuit are not an example of what happens in Western metabolisms.
…Also, many studies point out that the Inuit also ate considerable quantities of protein, and apparently have enlarged livers (which happens to be a symptom of CPT1a) with increased capacity for gluconeogenesis, which is originally why the old researchers did not believe they were in ketosis, despite burning lots of FFAs throughout their bodies. As multiple studies have pointed out, the ratios of fatty-acid to glucose were observed to be well below the generally accepted level of ketogenesis. [1][2][3][4]
But, I agree, people should experiment if they want to. They should just understand that they are going to burn FFAs differently from the Inuit. That doesn’t make ketosis good or bad, of course.
Maybe many/most non-Inuit can handle a persistent ketogenic diet *better* than the Inuit. As ironic as that sounds, given the ancestral Inuit’s VLC foodway.
There’s little evidence to show that ketosis burdens the livers of people in the Western developed world. Even though we generally lack the CPT1a variant that appears to be more common in the Inuit.
Bryan said: “Maybe many/most non-Inuit can handle a persistent ketogenic diet *better* than the Inuit. As ironic as that sounds, given the ancestral Inuit’s VLC foodway.”
lol.. That’s certainly a perspective I’ve never heard before. 🙂
Bryan said: “There’s little evidence to show that ketosis burdens the livers of people in the Western developed world.”
I wouldn’t know. Has it really been that well studied? I do remember Tolstoi in 1936 tested Stef and Andersen’s glucose response after their year-long Bellevue experiment and found they had a “false diagnosis of diabetes” that tends to happen after a long fast (i.e. very poor glucose control and/or physiological insulin resistance). That seems to be a temporary and normal response to fasting/ketosis as far as I know.
Perhaps it’s no big deal and soon reverses after some time on a varied diet. But, I’m not sure anyone really knows the long term consequences of it. Probably something people should at least be aware of.
I just (superficially) tried to find a link about this, but couldn’t find anything off hand- (it takes time, which I just don’t have right at this moment). However, I do know that Dr.’s Phinney and Volek have done some long term testing with low carb diets, and found no harm. They write about some of this in their book “The Art and Science of Low Carbohydrate Living”. In addition, there are several doctors who have been in long term ketosis; I know Dr. Phinney himself, and I believe Dr. Volek also. And, Dr. Eric Westman has been on a long term ketogenic diet- (he mentions it in his debate with Dr. Colin Campbell, which is on You Tube). These people seem to be in pretty good health, and they are doctors, so they must be aware of their health markers. There is also a book called “Ketopia” (which I haven’t read, though it sounds interesting). This is also about ketogenic diets, all the health benefits, and long term effects I believe.
Having said all that, I will admit that constant ketosis may not be the best thing for everyone. Children can generally make metabolic adaptations pretty quickly, but some adults may have difficulty if it’s not what they’re used to. However, it does appear that many people thrive on a ketogenic diet.
The modern evidence we have for ketogenic diets are clinical studies which are overwhelmingly either positive or neutral on them. We don’t have epidemiological studies on them, but not sure how much that even matters. Epidemiological studies have debatable value given their inherently correlative nature and issues of self-reporting.
Most people who want to try a persistent ketosis foodway should have no compunctions whatsoever! Go for it!
Duck, right? That’d be funny if we (assuming you are not Inuit) *did* handle ketosis better than those far Northern peoples. But the more we discuss and analyze this issue, the more I’m thinking it’s plausible. We may have the advantages, e.g. adequate persistent ketone levels, with no apparent downsides, at least none broadly documented. I can’t speak to the 1936 Stef and Andersen experience, but I can speak about my own in 2015. I am in persistent ketosis and even then, my BGs can start to float stubbornly higher, likely due in part to my marginal insulin output. In such a case I fast anywhere from 18h to three days, however long it takes to push me back onto the “right side of the metabolic divide.” Fasting always corrected my BGs, and it appears to be getting more effective. When I first started fasting in 2009, for a few years I used to have to occasionally do 2- and 3-day fasts to get the desired effect. But since ~2012, 18h fasts has been reliably doing the trick, and even these I need to do less and less. –Bryan
Duck,
I know the whole Inuit/ketosis thing has been in the spotlight and is very controversial, so I’m not putting all my stakes on them being in ketosis.
Having said that, it’s their protein that they metabolize differently, that I find interesting. They have so much brown fat and are able to decouple lots of ATPs as free heat, so they could eat much more protein then us and still be in ketosis.
And if ketosis defined simplistically as burning and using mostly fat for fuel, they certainly were in ketosis. Their mutations may just affect how they get in and out of ketosis, not how they “do it” or stay in it.
I’d say there are more similarities then differences between how we and inuit burn FFA, after all we both evolved and have mitochondrion that can burn only carbs or fat for fuel. We burn most of the fat not in the liver anyway, so I think it’s very similar how we and inuit burn fat.
Morgana,
thanks for reminding me about Dr. Phinney, I meant to read his stuff and forgot.
Bryan,
what is the longest modern study of people in ketosis have you seen? preferably not epileptic kids, because their disease will screw the results anyway.
Anna said: “And if ketosis defined simplistically as burning and using mostly fat for fuel, they certainly were in ketosis. Their mutations may just affect how they get in and out of ketosis, not how they “do it” or stay in it.”
Well, according to Wikipedia, “Ketosis /kɨˈtoʊsɨs/ is a metabolic state where most of the body’s energy supply comes from ketone bodies in the blood.”
Wikipedia also defines “ketone bodies” are defined as, “Ketone bodies are three water-soluble molecules that are produced by the liver from fatty acids during periods of low food intake (fasting) or carbohydrate restriction”
The article goes on to say, “Ketone bodies are produced from acetyl-CoA (see ketogenesis) mainly in the mitochondrial matrix of hepatocytes (liver tissue) when carbohydrates are so scarce that energy must be obtained from breaking down fatty acids”
So, no, I don’t believe that’s the actual definition of ketosis. The Inuit don’t do it like that.
Duck, technically you are correct, “Ketosis is a metabolic state where *most* of the body’s energy supply comes from ketone bodies”. Although I’m sure it’s debatable how “most” it is.
But ketone bodies are made mostly from FFA, some call ketones a byproduct of FFA metabolism. So in ketosis state our mitochondria uses ketones (made from FFA) and FFA (directly), so as I was saying in general terms, mitochondria is “using mostly fat for fuel”.
So I’m not sure what’s the argument here.
Anyway, if most of ketones are made in the liver, may be that’s why inuits’ liver is so enlarged? To produce more ketones? Idk.
But I still fail to see how they “do it” differently? both, us and them, burn ketones and FFA for energy while in ketosis. They may be able to get in and out easier, meaning their liver is more adapt at producing them, for example, or they have some other mechanism for additional ketone production, possibly.
But on a deep mitochondrial level we are exactly the same while in ketosis – we burn the same ketones and the same FFA to live.
“Anyway, if most of ketones are made in the liver, may be that’s why inuits’ liver is so enlarged? To produce more ketones? Idk.”
No. They do not produce more ketones. They struggle to produce ketones. As the research on CPT1a explains, the Inuit have difficulty producing ketones and this is why the Inuit can have difficulty fasting—particularly their children who tend to die of SIDS without regular breastfeeding around the clock. We don’t have difficulty fasting like that.
The mutation promotes “hypoketotic hypoglycemia” (low ketones, low blood sugar).
Anna said: “But I still fail to see how they “do it” differently? both, us and them, burn ketones and FFA for energy while in ketosis. .”
No.. the difference is that we burn “mostly” ketone bodies (acetoacetate and β-hydroxybutyrate) while they are known to have “extremely low levels of ketones”.
Anna,
I think Bryan had a rather accurate way of looking at it… Westerners appear to be “better” at ketosis than the Inuit.
It seems paradoxical, but I think Bryan is technically correct. The Inuit aren’t very good at producing ketones. But Westerners are quite good at it.
Duck, Anna–Anna I saw your recent comment and was thinking along your lines–this does seem like a distracting semantical snarl on “ketosis.” What does “ketosis” truly mean anyway? Duck, you pulled the def from the Wiki–not an unimpeachable source. But can I blame you? We can’t even find agreement on the def in the medical dictionaries. Many of those sources still imply it’s something pathological. Even doctors still confuse “ketosis” with “ketoacidosis.” We need to get past the surprisingly vague names of these metabolic states, which we use sloppily anyway. We often say “ketotic” to distinguish from the absence of the primacy of glycolysis. Maybe instead we should say “glycolysis” and “aglycolysis?”
In ant event, all that takes us away from the main question that triggered all the Inuit diet discussions. In search of what many of us want to know: Can we thrive on persistent LCHF? Even VLC?
The Inuit appear to do just that (with certain restrictions like freq child feeding) on VLC. Great. That’s a perfectly valid starting point for rest of us. Fellow humans being who diverged from us not so many thousands of years ago are up there in the Wild Blue North making VLC work. The Inuit are not from Mars. Genetically speaking we are still very very very very closely related. The fundamental mechanisms of energy production remain just the same. Our mitochondria oxidize glucose and beta-oxidize fats in just the same ways. It doesn’t at all mean we can’t take meaningful macronutrient lessons from the Inuit that we can effectively apply to our own lives. Their SNP variants appear to merely tweak the ketone body/FFA balance likely due to the Inuits’ special environment. So what if then that *may* make the Inuit not strictly “ketotic?”–whatever that means. So what if those with the CPT1a deficiency variant derive a greater proportion of their energy directly from the free fatty acids than non-variant VLCers? Our plasma albumin tows FFAs directly to the many types of cells that need the energy. Bypass the liver! Collect 200 ATPs!
Finally, let’s remember the idea that the Inuit with the CPT1a deficiency variant are “hypoketotic” Not “aketotic.” They are obviously producing *some* ketones. Plus that Wiki says the liver is the main but not the *sole* source of ketone bodies.
If anything, my recent discussions with you Duck makes me think that those of without the SNP variant may actually fare *better* on VLC than the Inuit. We have very little evidence that persistent VLC overloads and injures the liver. My little n=1 redux, I’ve been doing VLC it for over eight years. My extensive blood work has consistently improved in that time. Liver enzyme levels (AST, ALT, ALP) are always normal. –Bryan
What I haven’t heard here is any discussion of gluconeogenesis. Discover has a nice article about a lot of the issues with the Inuit:
http://discovermagazine.com/2004/oct/inuit-paradox
At one point I was in a group where a researcher with a zoo chimed in. She was saying that true carnivores are NOT “in ketosis” at all … they convert protein to glucose. Which isn’t efficient, but it works. If a lion or bobcat in a zoo is throwing ketones … it is ill and needs treatment.
She said the same is true for the Inuit. You maybe could find some other researcher and see if they agree. It may well be true that Europeans don’t have that ability so much, but the low-carb hunters probably would. Same as a lion.
Heathertwist said: “What I haven’t heard here is any discussion of gluconeogenesis”
Yes, exactly (actually I did mention it briefly). As I had mentioned in an earlier comment, all of the researchers who actually studied the Inuit firsthand (not talking about those who just wrote about them) believed that they were relying too heavily on gluconeogenesis to be in “ketosis”. They were eating far too much protein.
Their enlarged livers were believed to assist in gluconeogenesis beyond what Westerners can do. And their significant excretion of urea was also seen as evidence of this.
Actually there was a paper that was just published this past September that summarized all of the available Inuit research, and it too explained how they were a high protein culture that relied heavily on gluconeogenesis.
As you can see, they handle their food differently than we do. When white Arctic explorers lived with the Inuit, the white men had to eat a lot of fat and limit their protein to stay in ketosis. However, the Inuit were known to eat enormous quantities of meat, preferably dipped in fat. The point being that the Inuit did not limit their protein intake—they ate it constantly throughout the day to avoid fasting.
Interestingly, Stefannson never claimed that the Inuit ate 80% fat. In fact, his Inuit recipe for pemmican (when based on caribou rather than bison and the standard recepie was 2/3 lean caribou meat to only 1/3 melted fat) was relatively lean. LCHF Magasinet not only explained the Inuit/ketosis myth but they calculated the fat content of the Inuit pemmican would be less than 60%. You might get into mild ketosis if the fat content exeeds about 2/3 of calories, but but 60% wouldn’t achieve it even if the inuits ate 100% pemmican year around.
So, again, all of the evidence points to a high protein diet in the Inuit. They just weren’t eating enough fat to be in “ketosis”.
Duck, just curious, where’s the actual clinical proof that supports what you say about the Inuits’ “…enlarged livers…” and “…their significant excretion of urea…”?
I’ve been googling “Inuit liver autopsies” and “Inuit urine output” which so far turns up nothing except those comments from Harold Draper in Discover Mag and replicated elsewhere “recalling his 1970s studies.” Trouble is, I can’t find links to Draper’s actual studies. I’m not saying they don’t exist. Just saying I haven’t so far been able to find them.
Duck if you have links that prove what you assert, it’d be great if you post them here for us.
In the meantime, Duck, that new paper from Hardy et al is very interesting! Ever since I read Wrangham’s excellent little book “Catching Fire,” I’ve been following the research on the role starchy roots/tubers may have played in our pre Ag Rev evolution. Looking forward to digging into Hardy’s work. It’ll be a while till I have much to say on it. Most of the refs therein are books or stuck behind paywalls. At the moment, I’m ordering what cited pubs I can. Thanks –Bryan
Well, the Hardy paper references Kaleta, et al. 2012. But Harold Draper mentions increased urea in his 1977 paper. Both should be freely accessible.
I don’t know if Draper ever saw an Eskimo liver, but in his paper he just talks about urea clearance and high water intake with high protein.
CPT1a deficiency is known to cause enlarged livers, so I don’t doubt that they have them.
Of course, at the time, Draper didn’t know about their CPT1a mutations, but I’m sure he would have found that fascinating.
Draper mentions lack of fiber, but actually glycans in (raw?) animal tissue can be broken down by some bacteria (how meat is tenderized, for instance), so I imagine they had biomes similar to a carnivore might. They also ate rotting meats, a traditional delicacy which was claimed to offer health benefits.
???
Duck these don’t answer the question at all!
In the Draper paper, he says *nothing* about enlarged Inuit livers. Draper does say this about urea: “…their high-protein diet imposed on Eskimos a need to dispose of an unusually large metabolic load of urea…” But he doesn’t give a shred of evidence on how he determined that. It’s a completely unsupported comment.
In the Kaleta, et al. 2012 paper, I searched on “liver” and “urea” and came up with -nada-. Where are the relevant passages?
Again Duck… Where’s the actual clinical proof that supports what you say about the Inuits’ “…enlarged livers…” and “…their significant excretion of urea…”?
So far you’ve shown -NADA-
You made that assertion. It is reasonable for us to ask you to list the specific text that backs up your assertion. Duck, it is not asking too much of you. –Bryan
Bryan,
I specifically said that Draper never explained the evidence, beyond the very high urea excretion. See this quote from Discover Magazine, who interviewed Draper:
“Bigger livers”. At any rate, the high urea excretion is the byproduct of high protein intake.
I too could not find where Draper actually saw the bigger livers, but that’s what Draper appears to have told Discover when they interviewed him. Or perhaps Discover was getting their sources elsewhere. They are generally considered to be a reputable source, however.
Regardless, CPT1a deficiency is known to cause enlarged livers:
So, according to the NIH, enlarged livers is a common symptom of CPT1a deficiency.
So Duck, we’ve established you totally lack clinical evidence for Inuit having bigger livers. Or having to pee excessively. That your statement saying “Their enlarged livers … And their significant excretion of urea …” may well be complete nonsense. OK.
You cite an NIH paper that says “…People with CPT I deficiency can also have an enlarged liver…” We can chuck this out too. It’s only a general discussion that applies to all peoples with the deficiency, e.g. Hutterites as well as Inuit. It includes no evidence about enlarged Inuit livers. Duck if we buy your argument that “The Inuit are different from us” shouldn’t we then avoid to assume their livers will respond like ours to that deficiency?
Actually this is fascinating discussion. For years I’ve heard these “Inuit enlarged liver, Inuit pee a lot” factoids, you being the latest purveyor of them. I never questioned them till now. Now I find out we have no true evidence for them after all! I can regard this as the latest stool of med-anthro bullsh*t to scoop away till someone does real actual observations on the Inuit and their livers and urinary patterns. Thanks for this. –Bryan
Bryan, I found it!
It seems Draper was just referring to the well known observations of enlarged livers commonly observed in Eskimos:
So there you go. It was just an observation referenced in the literature. And there is plenty of evidence of high urinary nitrogen excretion in the Eskimo literature. They were well known to have a high protein diet.
Ya know… there’s no need to scream “nada” every time you think there’s a gotcha. We can both easily look into this stuff. No need for me to do all the work here!
Duck, I posted my last frustrated note to you before I got this evidence from you. I’ve reviewing it now. I’m sorry if I showed some frustration here, but it’s what happens when someone’s trying to snow us, when trying to back up their statements with really flimsy evidence as has been the case on this topic till now. If you had said “I know there’s real evidence, please give me time to find it” or somesuch, that be great! Will be back soon –Bryan
But what you say Duck, “We can both easily look into this stuff. No need for me to do all the work here!” I respectfully disagree. You make the assertion, you do the work to back it up. Down to the actual text to support what you’re asserting. We all should be doing that and I try to do AMAP. Otherwise we could be tossing out there all kinds of assertions without being sure what we’re talking about and letting “others sort it out.” We are dealing with fascinating but enormously complex material than directly affects our lives. We need to be as rigorous with ourselves as possible. Don’t mean to lecture Duck, but you have to admit, you haven’t been consistently great about that 🙂 –Bryan
Bryan,
This is not some flimsy assertion. I have yet to find a single paper or study—referencing actual measurements on actual Eskimos—that did not conclude that the Eskimos were eating a high protein diet. For example, the following researchers all concluded that the Eskimo diet was a high protein diet and were not in ketosis:
Krogh & Krogh 1914 (Nobel Prize winner)
Lusk 1914
Joslin 1917 (first doctor to ever specialize in diabetes in the US)
Schaffer 1921
Heinbecker 1928, 1931, 1932
Tolstoi 1929
McClellan & DuBois 1930 (Stefansson’s own doctors)
Rabinowitch 1936
Rabinowitch & Corcoran 1936
Rabinowitch & Smith 1936
Kaare Rodahl 1952
Sinclair 1953 (A detailed review of the literature)
Ho 1972
Hui 1975
Bang, Dyerberg & Hjorne 1976
Draper 1977
Bang, Dyerberg & Sinclair 1980
VanItallie & Nufert 2003
Leonard & Snodgrass 2005
Hardy 2005
They all say the Inuit ate high protein, because they did. So, the scientific literature says—without a doubt—that the Inuit were high protein. Therefore, I believe it is you who needs to show otherwise.
Bryan said: “You make the assertion, you do the work to back it up.”
Sorry, but it’s not my assertion. It’s just what the literature says. All of the literature says high protein and no ketosis. If you disagree, it’s you who will have to show otherwise.
Cheers.
Duck, to be clear, I wasn’t questioning you about the Inuit protein intake. I’m not ready yet to do that. Like I said earlier, I can’t yet get near enough data from the Hardy paper. Thanks for all the links. Most of them you’ve already posted and I’ve reviewed them to varying degrees. But you’ve included a few new ones; thank you for those. Looks like I’ll have to learn Danish 😉
What I did question: The enlarged liver/freq peeing thing. Most of the comments addressing that presumed issue point back to that Discover mag article. That site quality is mostly OK–I’ve worked for large consumer tech and general interest pubs for over 20 years and ex-colleagues went on to edit and write at Discover, Popular Science, etc. But that article’s simply a reporting job and doesn’t cite any studies, at least not for our topic here. One of the things I’ve learned in the biz is how the internet can propagate and replicate CW till it gets to the point that even a lie told enough times looks like the truth.
About assertion, Duck indeed you were asserting: “Their enlarged livers … their significant excretion of urea …” Sorry, but that is the case. It’s right there in your post. It’s up to you to supply solid credible evidence to back that up. If I disagree with your assertion, yes, it is up to me to find credible rebuttals. But if you fail to provide strong and relevant evidence to back it up, I’m well within my rights to ask you for it. I am sometimes willing to do your work. But you shouldn’t *expect* me to do your work.
Duck what you say here: “All of the literature says … no ketosis.” Of course that’s false. You yourself quoted literature saying “hypoketotic…” “Hypoketotic” is not “aketotic.” We know the Inuit *do* in fact produce ketones, if not to our level. Only how much? I’ve yet to see serum ketone measurement actually listed in mmol/L (millimolar) or in any other concentration units. Maybe they are there in one of those linked you posted, and I haven’t seen it yet. But Duck, the larger issue has to do with the fact that “ketosis” is a surprisingly nebulous and ill-defined term. Someone can assert that if an Inuk has 0.000001 mmol/L of serum ketones, he is in “ketosis.” Who are we to say he’s wrong? What is the minimum mmol/L of serum ketones to declare someone “ketotic?” You don’t know. No-one else knows either. –Bryan
Sounds good, Bryan. If ketosis is a surprisingly nebulous and ill-defined term, then I don’t even know what to say about it. 🙂 At this point the literature says what the literature says. There’s not much more to say!
About decided the term “ketosis” is nigh near meaningless, it’s funny to arrive at that point isn’t it Duck? After all the keyboard sturm und drang about Nanook and his ketones.
As for what you say “At this point the literature says what the literature says…” that’s right. And much of the literature saying quite different things!
So Duck, what definition of “ketosis” will you stick with? –Bryan
“what definition of “ketosis” will you stick with?”
Probably the classical definition mentioned by Sinclair 1953 and others. It seems like there is a recent movement to redefine what ketosis is—and that’s fine—but I’ll leave that to others to sort out.
OK, once again I posted to you before seeing your answer.
That 1953 Sinclair paper is behind a paywall. If you wouldn’t mind posting his ketosis def here …
Thanks –Bry
“…If ketosis is a surprisingly nebulous and ill-defined term, then I don’t even know what to say about it. 🙂 …”
Duck, why don’t we start with that Wiki def you cited earlier: https://en.wikipedia.org/wiki/Ketosis
“Ketosis /kɨˈtoʊsɨs/ is a metabolic state where most of the body’s energy supply comes from ketone bodies in the blood.”
Using that def, are the Inuit in “ketosis” or not? Do we know? How many calories do they derive from serum ketones? Serum glucose? Serum FFAs? BTW, when the liver breaks down excess protein, not *all* of it become glucose. About a quarter of it becomes fat.
Who’s actually measured these things in our far northern friends? Do you know?
And Duck, most important, if insulin levels remain low, low enough to continue to allow release of fats from adipose tissue, *does it all really matter?*
Is it like arguing how many angels can dance on the head of a pin? –Bry
I hear you Bryan. It’s impossible to define the diet. I get it. Nevertheless, they are known to be a high protein culture. There’s really nothing left to say. I’m getting on a plane in the morning and have to head to bed. It’s been fun. Be well and take care.
OK Duck. Sleep well, and have a good trip. See you back here. –Bry
To be clear, Duck, you *do* furnish a lot of links. It’s only that the quality of the evidence you cite can really vary. But you have a lot of great ideas. Given the state of most “science” out there, I’ll take the ideas! –Bryan
Hi Duck. Sorry. But if you are trying to imply that enlarged Inuit livers were somehow “unhealthy” you’re still batting zero.
What you said: “…It seems Draper was just referring to the well known observations of enlarged livers commonly observed in Eskimos…” Draper offers three refs for these “well known observations” as you call them. They are “Brown, 1955; Hildes, 1958; and Schaefer, 1971.”
Once again these texts prove elusive. However, thanks to our Jonathan Christie here, we have Dr Schaefer’s 1959 glowing report on exceptionally robust Inuit health. In it Schaefer refs Brown and Hildes works for the same years that Draper cites:
“…Many seal-eating Eskimos *though perfectly healthy*, have a relatively large liver. This hepatomegaly was first described by Brown and confirmed by Hildes….” You can see his report here: http://www.ncbi.nlm.nih.gov/pmc/articles/PMC1831365/pdf/canmedaj00812-0101.pdf
Duck, this strongly suggests that Schaefer found nothing in the earlier Brown and Hildes works that suggests these Inuits’ livers were pathologically enlarged. Nothing from Brown and Hildes to suggest their livers were in any way “unhealthy.”
And Duck, about what you said “…And there is plenty of evidence of high urinary nitrogen excretion in the Eskimo literature…” Even now, you persist to fail to show even one shred of real evidence to back up your claim.
Finally Duck what you say here “…[the Inuit] were well known to have a high protein diet…”
So what? Where’s the evidence that the Inuits’ protein intake, whatever percent of the diet that was, harmed their health in any persistent way?
As you requested Duck, I’m rating your work on this topic to date a quieter all-lower-case “nada.”
It still means “nada.” –Bryan
“Hi Duck. Sorry. But if you are trying to imply that enlarged Inuit livers were somehow “unhealthy” you’re still batting zero.”
Thanks for the straw man argument, but no that’s not what I was saying. The scientists I cited believed that their enlarged livers were due to their high protein diet. Of course, I explained that already, but you’re having trouble following that point for some reason.
“Once again these texts prove elusive. However, thanks to our Jonathan Christie here, we have Dr Schaefer’s 1959 glowing report on exceptionally robust Inuit health.”
Wonderful. And guess what? Schaefer beleived their glowing health was due to their, high protein diet.
That’s what I’ve been trying to tell you all this time. They don’t even eat like you do.
“And Duck, about what you said “…And there is plenty of evidence of high urinary nitrogen excretion in the Eskimo literature…” Even now, you persist to fail to show even one shred of real evidence to back up your claim.”
Enough with the lies. I already gave you links to all of the literature. Krogh & Krogh 1914 showed high nitrogen from high protein. As did Rodahl 1952 and others.
“Finally Duck what you say here “…[the Inuit] were well known to have a high protein diet…” So what? Where’s the evidence that the Inuits’ protein intake, whatever percent of the diet that was, harmed their health in any persistent way?”
It’s all documented in the links I’ve provided earlier. ALL of the research says they were high protein—even Schaefer. Even the LCHF Magasinet Swedes understand what you are having trouble seeing.
But once again you’ve missed the point. The point is not whether they were healthy or not. We really don’t know since even Inuit mummies are well known to have had significant arterioclerosis (possibly from inhaling soot from their lamps). That’s not the point.
The point is that the Inuit were eating so much protein that all of the researchers who looked into their enlarged livers believed they were relying heavily on gluconeogensis for much of their energy. And a grand total of ZERO believed that they were relying heavily on ketones.
Is that how you eat, Bryan? Do you eat a high amount of protein and reserve most of your fat for burning lamp fuel for heat? If you are able to eat a high protein diet and can stay in ketosis, then I agree with Peter on this one, who says:
Peter sums it up nicely. Why on Earth would you want to use this extreme culture with unique genes and a high protein diet as the poster boys for a ketogenic diet anyhow? Makes zero sense.
“As you requested Duck, I’m rating your work on this topic to date a quieter all-lower-case “nada.” It still means “nada.”
And once again you’ve resorted to argument from fallacy.
I really have no interest in debating your fallacies any further, Bryan. If you want to know my opinion, then you should read all of the links I provided which actually observed real Eskimos. The literature stands on its own. The literature says they were not in ketosis (the original definition, which you are now trying to change) and that they ate a high protein diet. All of those references I provided refer to the Inuit’s observed high protein diet, which the researchers believed furnished their carbohydrate via gluconeogenesis.
And if you yourself eat a raw, high protein diet, then you can feel proud that you eat like an Inuit and are super healthy. However, if you are into protein restriction, then I have no idea what you are doing looking into a culture that doesn’t even eat like you do. It’s mind boggling.
There’s really nothing else left to say.
Duck, about the Inuit Paradox, to remind you why so many of us care and what we really want to know:
– Can the Inuit Paradox inform our decision–us non-Inuit folks–to try a persistent VLC foodway?
– Does the Inuit Paradox offer real evidence to consider to optimize dietary omega 6/omega 3 balance to lower our systemic inflammation?
The Inuit Paradox keeps offering tremendously exciting and relevant evidence to suggest the above approaches may indeed work to greatly improve our health. Duck, to date, no amount of “evidency-ness” you’ve shoveled onto this forum, when we closely or often even merely cursorily examine your sources, even begins to discredit the Inuit Paradox. Your slew of links have never–and I mean *never*–delivered rigorous evidence to discredit that Paradox. Your vague implied warnings against adopting lessons from the ancestral Inuit foodway: “…they are not like us,” “they burn fatty acids very differently,” “they do not exhibit ketosis as we do” and so forth, are simply that–vague and wholly unsupported warnings. Nothing you said and shown should even remotely dissuade anyone from experimenting with VLC. Ancestrally-living Inuit can and routinely DID thrive on VLC, even a near no-carb diet. By nearly all measures, many ancestrally-living Inuit enjoyed all-around robust health. Here’s a summary of the info that recently surfaced that we bat around here:
– the Inuit have one or a few genetic SNP variants (And so? In re: VLC, why should we care?)
– they “eat a high-protein diet” (So what? Why should we care? What’s “high?” anyway?)
– they “may or may not be in ketosis” (So what? Why should we care?)
– the conflicting accounts/non-accounts of CVD in ancestrally-living Inuit like those found in the 1940 Bertelsen report (I finally have this report. **Bertelsen utterly fails to say what the people who referenced it–including Ottawa Heart’s Dr Fodor–have been saying or implying it says.** Stay tuned for details.)
These points above are either wrong or fail to relate to our goals to find an optimum foodway to preserve and enhance our health.
So Duck, with your impressive ark of non-evidence, can I blame you for trotting out your tired litany of distractions? You recycle your irrelevant points accented with argumenta ad hominem: “…The scientists I cited believed that their enlarged livers were due to their high protein diet…Of course, I explained that already, but you’re having trouble following that point for some reason…That’s what I’ve been trying to tell you all this time. They don’t even eat like you do…” Meanwhile Duck you pose a silly rhetorical question, with a side of unsupportable assumption (the lamp fat thing), for which you already know the answers: “…Is that how you eat, Bryan? Do you eat a high amount of protein and reserve most of your fat for burning lamp fuel for heat?…” Again Duck, of course I don’t eat high protein and you know it. The point is that the diet is VLC–remember? I’ve made clear here I eat 15% protein and mostly fat. There’s plenty of evidence to suggest even the Inuit prefer fat. Maktaaq (Muktuk) is blubber that’s well over 90% fat by calores: http://ndb.nal.usda.gov/ndb/foods/show/8354 In that 2004 Discover Mag link you’ve cited before Duck, http://discovermagazine.com/2004/oct/inuit-paradox , raw muktuk… to many [Inuit], it’s a mainstay.” Canadian Arctic explorer and ethnologist Vilhjalmur Stefansson spent a great deal of time researching the Inuit. His observations and his own experiences and further experiments with a very high meat diet led Stefansson in his book “Fat of the Land.” to propose a diet that is mostly fat. Ho et al in 1972, http://ajcn.nutrition.org/content/25/8/737.full.pdf , says “…Approx 50% of the calories were derived from fat and 30 to 35% from protein.”
Then Duck we see this old saw from you–“I’ve Posted The Links…” You say: “…It’s all documented in the links I’ve provided earlier. ALL of the research says they were high protein—even Schaefer. Even the LCHF Magasinet Swedes understand what you are having trouble seeing…” complete with yet more ad hominem, accusing me of “…having trouble seeing…” something which I’ve never denied to begin with. Sure it’s perfectly plausible, even likely, the Inuit ate a higher percentage of protein than many others following their ancestral foodways. Duck, so what? I’ve seen zero evidence to suggest a higher protein has in any way impacted Inuit health, except possibly episodically and temporarily when sparse food availability forced them to eat ultra high protein.
Duck what you say here, in your one bolded comment in your post: “…the Inuit were eating so much protein that all of the researchers who looked into their enlarged livers believed they were relying heavily on gluconeogenesis for much of their energy…” Duck, I give that a big bolded “So What?” See my protein/fat discussion above. How much are their livers “enlarged?” Marginally bigger,like 5%? Who’s actually measured it? Does it even matter? You’ve yet to show even one researcher to determine this was an unhealthy adaptation. Indeed Schaefer said in 1959 “…Many seal-eating Eskimos *though perfectly healthy*, have a relatively large liver…” http://www.ncbi.nlm.nih.gov/pmc/articles/PMC1831365/pdf/canmedaj00812-0101.pdf
Also your phrase “relying heavily on gluconeogenesis” is meaningless. “Heavily” as compared to what? Just ketosis? What about lipolysis? In that Ho report linked above, we read this: “The fact that the Eskimos had high serum FFA and low glucose levels (approximately 65 mg/100 ml) indicated that free fatty acids played a major role in body energy production…”
Here Duck you quote an irrelevant passage from Hyperlipid’s Peter:
http://high-fat-nutrition.blogspot.com/2014/11/the-p479l-gene-for-cpt-1a-and-fatty.html
and yet completely ignore his main message: You quote from Peter: “I have some level of discomfort with using the Inuit as poster people for a ketogenic diet. That’s fine. They may well have eaten what would be a ketogenic diet for many of us, but they certainly did not develop high levels of ketones when they carried the P479L gene.”
Duck what you conveniently leave out: Peter actually ardently *supports* VLC and ketosis. He writes further down in that same blog post:
“I’m always amazed by the concept that a ketogenic diet might be temporarily therapeutic but must be discontinued because it eventually becomes Bad For You… point-scoring on the internet about what the Inuit did or didn’t eat shouldn’t destroy people’s chances of health…”
Finally Duck, you emerging fave distraction: Your spurious charges of “argument of fallacy.” You say “I really have no interest in debating your fallacies any further…” Duck, sure, that’s easy to say when you conveniently leave out specifics and examples to support your charges, or even show proof I’ve made even one argument to you “from fallacy.” Whatever. We’re used to that from you. Duck, if it makes you feel better to believe all that–whatever all that’s even supposed to be or to mean–then please be my guest. It won’t change the fact that I and very very many other folks derived health-saving and even life-saving lessons from the Inuit Paradox.
Duck, I’ll conclude with Peter’s conclusion out of his same post you cited:
“…point-scoring on the internet about what the Inuit did or didn’t eat shouldn’t destroy people’s chances of health. Destroying a circular argument about Inuit diets may may the destructor feel good. Destroying the feet, eyes and kidneys of a person with type 2 diabetes, who need a ketogenic diet, as a spin off from that victory must be difficult to live with. I don’t know how anyone can do this.”
Amen.
–Bryan
Bryan said: “Can the Inuit Paradox inform our decision–us non-Inuit folks–to try a persistent VLC foodway?”
No it cannot. Because they do not eat anything like Western VLC dieters do. To imply otherwise is dishonest.
Bryan said: “Does the Inuit Paradox offer real evidence to consider to optimize dietary omega 6/omega 3 balance to lower our systemic inflammation?”
Unknown. They possess unique genetic adaptions to apparently metabolize fats differently than we do. Incidentally, Hugh Sinclair once attempted to consume a high n-3 PUFA diet and it caused him to have difficulty with clotting and hemorrhages.
Bryan said: “Nothing you said and shown should even remotely dissuade anyone from experimenting with VLC.”
This is a straw man argument (which seems to be your expertise). I am not trying to dissuade anyone from experimenting with VLC. I am pointing out that the whole of the scientific literature says that the Inuit diet is not a proxy Western VLC diets.
Bryan said: “Ancestrally-living Inuit can and routinely DID thrive on VLC, even a near no-carb diet.”
Wonderful. And they did it by eating excessive levels of protein. The exact opposite of what Western VLC diets promote. They were converting enormous amounts of protein into carbohydrates via gluconeogensis. gluconeogensis = production of glucose. Glucose inhibits ketosis.
Bryan said: “the Inuit have one or a few genetic SNP variants (And so? In re: VLC, why should we care?)”
Because Westerners don’t have those SNPs and we don’t know if they are necessary for thriving on a VLC diet. That should be an obvious variable to consider.
Bryan said: they “eat a high-protein diet” (So what? Why should we care? What’s “high?” anyway?)”
Because protein is restricted in Western VLC diets. Protein knocks people out of ketosis. You should know this of course. And if you have difficulty understanding this, then I will point you to Peter’s article on the subject.
Peter writes:
Read that again. (See my next post for documented Inuit protein consumption).
The Inuit eat an excessive amount of protein, they do not restrict it. Therefore, they cannot be used as a proxy for a Western VLC or ketogenic diet.
Bryan said: “I’ve seen zero evidence to suggest a higher protein has in any way impacted Inuit health”
Another straw man argument. I never said their high protein intake was deleterious. Rather, my point is that their high protein diet is the exact opposite of the protein restriction advocated by Western VLC dieters. Please do your best to understand that point. You should never imply that the Inuit diet is a proxy for Western VLC. Peter’s post on protein and ketosis proves this. And yes, I’m aware that Peter promotes Western VLC diets. That’s why he’s uncomfortable with using them for “poster boys” of ketogenic diets.
Bryan said: “Canadian Arctic explorer and ethnologist Vilhjalmur Stefansson spent a great deal of time researching the Inuit. His observations and his own experiences and further experiments with a very high meat diet led Stefansson in his book “Fat of the Land.” to propose a diet that is mostly fat.”
Yes, his “own experiences” are the key there. Stefansson was advocating a Western version of the Eskimo VLC diet. However, Stefansson was a white man who claimed to have gotten sick when he tried to eat a high protein diet. The only way Stefansson could survive in the Arctic was to restrict protein and eat high fat. You’ve just proven my point. White people cannot eat the high protein diet that the Inuit consume. Stefansson’s experience proved it and his own doctors admitted that he was unable to consume the observed high protein intake in an Eskimo’s traditional diet .
Bryan said: “Ho et al in 1972, says “…Approx 50% of the calories were derived from fat and 30 to 35% from protein.”
Yes. Ho is getting figures from Krogh & Krogh 1914. Krogh & Krogh observed excessive protein intakes. Again, you are proving my point. Western VLC dieters do not consume that much protein, particularly if they want to remain in ketosis.
Bryan said: “How much are their livers “enlarged?” Marginally bigger,like 5%? Who’s actually measured it? Does it even matter? You’ve yet to show even one researcher to determine this was an unhealthy adaptation.”
Straw man. I never said it was an unhealthy adaptation. The point is that they are relying protein to produce a lot of glucose, which inhibits ketosis. This glucose production is why no scientist ever claimed they were in ketosis. A Western VLC dieter restricts protein to stay on a VLC diet. That’s my point.
Bryan said: “your impressive ark of non-evidence”
I don’t see how presenting you with a century of scientific evidence is “non-evidence.” See my next post if you aren’t going to bother reading it.
Bryan said: “It won’t change the fact that I and very very many other folks derived health-saving and even life-saving lessons from the Inuit Paradox.”
I do not deny that a ketogenic diet can be therapeutic for some. However, since the Inuit were not in ketosis, whatever “life-savings lessons” you think are derived from the Inuit Paradox are based on a misunderstanding of what the Inuit actually consumed (in reality a high protein diet).
Bryan said “Duck, I’ll conclude with Peter’s conclusion… “…point-scoring on the internet about what the Inuit did or didn’t eat shouldn’t destroy people’s chances of health. Destroying a circular argument about Inuit diets may may the destructor feel good. Destroying the feet, eyes and kidneys of a person with type 2 diabetes, who need a ketogenic diet, as a spin off from that victory must be difficult to live with. I don’t know how anyone can do this.”
Lol. I agree with Peter. And his statement would be relevant if someone here was trying to use the Inuit’s non-ketosis to dissuade others from trying a trying a VLC diet. But no one here is doing that, so again… it’s a straw man (once again).
It makes no difference if the Inuit were healthy or not because their diet has nothing to do with a Western VLC diet. As you like to say… “Nada”.
We agree that they burn a lot of FFAs, but they also produce a lot of endogenous glucose from their excessive protein intake (see my next post). How is that like a Western VLC diet? It’s not.
Cheers.
Duck, the Inuit Paradox absolutely can and *should* inform non-Inuit who contemplate a persistent VLC foodway, esp them who fear it because “no one’s ever done it before.” I never suggested we should eat all the same things as the Inuit. It’s the nutrient lessons we learn from them. I’m not going to start eating muktuk. But I’m making sure to eat salmon with the skin and bones. Both have high long-chain w3 and plenty of other nutrients. Nothing “dishonest” about that Duck. That’s very valuable to know and act on.
About Hugh Sinclair’s tissues with clotting on high w3, again you fail to read my comment correctly. I said “*optimize* dietary omega 6/omega 3 balance.” I had a similar clotting issue till I dialed back down my w6/w3 ratio from 1:1 to 3–4:1. I was fine afterwards and still kept getting lower CRPs.
Duck if “Nothing you said and shown should even remotely dissuade anyone from experimenting with VLC.” is a straw man argument as you claim, then why do you keep flogging the ill-defined idea that “the Inuit diet is not a proxy [for] Western VLC diets?” Do you do this out of a burning academic interest? People here want to learn how to get and remain healthier. If they need reassurance that they can safely achieve that on LCHF, the Inuit experience can help them hugely. Does that mean we have to eat 50% fat/35% protein like the Inuit do? Of course not. I eat 80% fat/15% protein. Point is Duck, it’s to reassure people they may well do very well on *persistent low-carb* and should not be the least bit afraid to experiment with it.
About what you say here: “Wonderful. And the [Inuit] did it by eating excessive levels of protein. The exact opposite of what Western VLC diets promote. They were converting enormous amounts of protein into carbohydrates via gluconeogensis. gluconeogensis = production of glucose. Glucose inhibits ketosis.” Duck, where to start with this flabby mess you spilled here? Again, your view that it’s “excessive” protein has never been proven. That’s simply your opinion. About it being “opposite to Western VLC” of course that’s wrong. Both are low carb. It’s a matter of setting the fat/protein balance that works best. About gluconeogenesis you have no idea how much of this ancestrally-living Inuit generate. Ditto for “enormous amounts of protein”–“enormous” is simply your personal feeling. Duck, obviously you’re welcome to all your opinions on all this. Just please understand they are not supported by the actual science. None in that “century of scientific evidence” you stuck up here.
Duck you say “Because Westerners don’t have those [Inuit] SNPs and we don’t know if they are necessary for thriving on a VLC diet…” *Sigh* Been there, done that already Duck. If anything, westerners are *better* at producing ketones. In any event, I’ve always suggested that people going on VLC get blood tests if only to assuage any concerns they may have.
About my comment: “Bryan said: they “eat a high-protein diet” (So what? Why should we care? What’s “high?” anyway?)” and your answer: “Because protein is restricted in Western VLC diets…” Duck yes you persist to misunderstand me. Where have I ever said we should eat a high-protein diet? Take a look round. You won’t find me saying that anywhere. And of course you’ve never answered what you think what constitutes “excessive.” Not holding my breath for that.
What you say here “The Inuit eat an excessive amount of protein…” Duck, you think if say this enough times maybe one day it’ll come true? Just wondering.
Oh but wait, then we get this from you! “I never said [the Inuit’s] high protein intake was deleterious.” Oh really? Duck, sure, you didn’t *say* their “high” protein intake doesn’t harm them. But do you believe it does? If not, then Duck why do you just say “The Inuit eat an excessive amount of protein…”? Pray reconcile these two statements for us.
About what you say. “You should never imply that the Inuit diet is a proxy for Western VLC.” Gee Duck. Maybe if you say it enough times, that’ll become true too. Maybe Bryan blog comments exhorting folks to chow unseemly amounts of protein will start spontaneously popping up all round the webosphere 🙂
Duck, you say: “… You’ve just proven my point. White people cannot eat the high protein diet that the Inuit consume. Stefansson’s experience proved it and his own doctors admitted that he was unable to consume the observed high protein intake in an Eskimo’s traditional diet…” Yes Duck. If you want to take Stefansson n=1 as “proof” that “white people” can’t eat the high protein diet the Inuit consume, sure, be my guest. Whatever. I’ve never advocated a high-protein foodway anyway. You know. Just in case I haven’t told you that before. And Duck, a news flash: You’ll find other kinds of non-Inuit folks out there besides “white people.”
Our exchange here: Bryan says: “Ho et al in 1972, says “…Approx 50% of the calories were derived from fat and 30 to 35% from protein.” Duck says: ”Ho is getting figures from Krogh & Krogh 1914. Krogh & Krogh observed excessive protein intakes…” Sure Duck. I’ suppose you’ll actually bother to back up that assertion of “excessive protein intakes” with actual K & K text? I’ve learned not to hold my breath for actual proof from you. If that text evidence actually exists and you actually post it, please remember this is nutrition science from over a hundred years ago around the time we were discovering “vital amines.” Duck, if this becomes yet another assertion you fail to support, I won’t mind.
About this: “I never said [high protein intake] it was an unhealthy adaptation.” Hmm. You’ve gone on about “enlarged livers” and “…their significant excretion of urea…” OK Duck whatever you say.
About this mess: “The point is that they are relying protein to produce a lot of glucose, which inhibits ketosis. This glucose production is why no scientist ever claimed they were in ketosis. A Western VLC dieter restricts protein to stay on a VLC diet. That’s my point.” Oh really Duck? “Glucose inhibits ketones” is your point? Gee, all this time I thought it was the Inuit “hypoketotic hypoglycemic” state you kept going on about. You know, yielding those raging 65mg/dL serum glucose levels ready to put the boots to any ketones with enough temerity to try to leave the liver. And I was thinking all this due to that CPT1a deficiency variant gene you kept going on about–you know, the deficiency that inhibits ketone production. Silly me Duck. Please enlighten us: What mg/dL of serum glucose do you need to start inhibiting ketosis? Enquiring minds want to know.
You say: “I do not deny that a ketogenic diet can be therapeutic for some. However, since the Inuit were not in ketosis, whatever “life-savings lessons” you think are derived from the Inuit Paradox are based on a misunderstanding of what the Inuit actually consumed (in reality a high protein diet).” Yes Duck, been around this block with you too a few times. What’s up with your amnesia? Mon pauvre, try to remember. Hint Q: Compared to Inuit, how well might non-Inuit handle “ketosis?”
And finally this Duck–good job putting words in my mouth: Duck says:“I agree with Peter. And his statement would be relevant if someone here was trying to use the Inuit’s non-ketosis to dissuade others from trying a trying a VLC diet. But no one here is doing that…” Well, Duck, that’s wrong too. You can sure find folks here inveighing against VLC. But Duck, please consider this: You’ve come up with one argument after the next to drive home the idea that the Inuit–the world’s top success story of ancestral VLC–are so “different” from us that their experience can serve little or no use to us. You efforts have the effect to cast doubt on what is perhaps the most inspiring example of low-carb success our planet offers. You upbraid people including me for imagined arguments of fallacy, meanwhile doggedly perpetuating the fallacy of insisting that people who suggest we take lessons from the Inuit are advocating “their high-protein diet” and even that we should eat their foods. Your insistence in this matter borders on an odd obsession. Your stubbornly refuse to see that VLC advocates, in the main, are *not* advocating a high-protein. Why do you do this? Your verbal contortions would be risible except this is very important stuff we’re discussing. Our diet decisions directly impact our health and lives. Duck, I’m not saying you shouldn’t spin your academic arguments regarding the Inuit. That stuff’s great fun and, most of all, we should feel free to voice our views here. But I say again to you, in this important matter, I *will* call bullsh*t when I see it. Most of all, people–especially people with high blood sugar issues–need to know they should feel absolutely free and SAFE to try VLC and even consider it as a lifetime choice, not just a “therapy.” The evidence suggests a low-carb moderate-protein very-high-healthy-fat foodway is perfectly safe. –Bryan
Bryan,
You’ve accused me of not presenting evidence, despite that I provided links to over 100 years of scientific observations on the Eskimos. Since you won’t take the time to read any of it, here’s what the scientists who observed the Eskimos found with their protein consumption (and nitrogen production) from high protein and high gluconeogenesis production.
Krogh & Krogh put a handful of Eskimos individually into a respiration chamber for 4 days at a time and fed them lots of Seal meat. They wrote:
This was the first of many observations of high nitrogen excretion—a sign of significant glucose production from gluconeogenesis and not ketosis.
The Kroghs explained in their highly detailed report that the Eskimos would not enter the chamber unless they were promised various quantities of bread (and sugar for their coffee) during the experiment. The Kroghs agreed and gave them lots of bread/sugar some days and only a little bread/sugar on the VLC days. On VLC days, the Kroghs found that roughly half of their 54g of carbs came from bread/sugar and more than half came from glycogen in the meats. According to Rink 1855, Inuit were known to source bread and sugar since white man appeared in the 1800s, so we don’t know if these modern carbs craved by the Eskimos replaced other traditional carbs in their diet (Angelica, for instance) or if they were new additions to their diets.
In 1931, Heinbecker wrote:
Again, See Peter’s post on the importance of protein restriction in Western VLC diets.
In a review of all the available literature by 1953, Hugh Sinclair wrote:
4 kg of meat daily? Half the fat of what would be needed to reach ketosis? Hmm… And Peter says steaks aren’t ketogenic. So, Western VLCers do not eat this way, of course. Unlike the Eskimos, Western VLC dieters restrict protein. That’s been my point all along. You cannot use the Eskimo diet as a proxy for a Western VLC diet.
Not only did Rodahl observe high protein, but observed even higher protein intake during the Winter:
Bryan, do any Western VLC dieters regularly consume 300gm of protein per day? Is it advocated as part of a VLC lifestlye? No, of course not. Because doing so would result in a metabolism that relied too heavily on gluconeogenesis (i.e. glucose) for energy.
Therefore, you cannot use the Inuit as a proxy for the health of a Western ketogenic diet. They don’t eat anything like Western VLCers do. Nor do any of us have their genes or metabolisms that allow them to eat this way.
My overarching point is that the Inuit cannot be a proxy for Western VLC or ketosis. To imply otherwise is dishonest when we see that all of the scientific literature shows otherwise.
This is not to say that a Western VLC diet is unhealthy—I have no idea if it is or is not. It may very well be that VLC is the best diet in the world! Who knows? All I’m saying is that you cannot use the Inuit as an example of Western VLC. That should be obvious given what was actually observed about the Eskimo diet.
Feel free to dig into the Inuit all you like. And feel free to advocate a ketogenic diet to those who may need it. Just be aware that at 300gm of protein per day, the Eskimos are not eating anything like a Western VLC diet.
Peter is wise to distance himself from the Inuit. You should follow his lead.
Cheers.
Duck, thank you for this very interesting material. Really, I do visit your links or had been. But it does get discouraging when so many you’ve posted go to material that’s stuck behind paywalls or in books or doesn’t address the issue.
Like I made clear in my last mail, you don’t need to sell me on the idea that the Inuit can eat a lot of protein. I never disputed it. I’m not convinced all Inuit around the north ate whopping amounts of protein all the time. There’s plenty of evidence to suggest they eat more fat when given the choice. They land a big bowhead whale, and they’re literally savoring the maqtaak for days. Since most Inuit live near the sea and hunt blubber-rich marine mammals, they often get a chance to eat a lot of fat, and can give the excess protein to their dogs. Nonetheless, I can imagine they need to eat high protein often enough that they’d have to adapt to it.
And how do they adapt? Duck I had to laugh when you asked me: “Bryan, do any Western VLC dieters regularly consume 300gm of protein per day?“ That was *me* from July–October 2007! During those four months I was averaging 300g protein per day. That was 40–50% of my calories. I know this because, during that time, I carefully weighed everything I ate down to the gram and entered all that into my spreadsheet. During that high-protein time, this “white boy” actually felt fine as I recall. At that time I walked 8–10 miles per day, and had plenty of strength to do that. The two main downsides: people told me I had ammonia breath and I had to get up several times per night to pee. Reading this about the Inuit makes me more curious about high protein. Who knows how my bod would have adapted if I carried it beyond those four months? But starting in October, I start systematically dialing up the fat percent till I got to my current level (80%) in spring 2008. I much preferred to eat the fat–the “flavor carrier”–over the protein.
This is also interesting: “Inuit were known to source bread and sugar since white man appeared in the 1800s” Reading through Bertelsen’s report in 1940, I was a little surprised to learn many of his Inuit patients had already adopted a lot of western-style food and habits, especially smoking and drinking alcohol. More on that later.
I want to spend more time looking at what you posted, and especially to crunch a few of their numbers. I’m going to bed now and will come back to this tomorrow. –Bryan
Bryan, you probably didn’t notice, but I had already provided the Krogh & Krogh many days ago (remember, you thought you’d “have to learn Danish,” but all you had to do was scroll past the Danish introduction). Due note the high levels of gluconeogenesis as shown by their high nitrogen excretion, which shows the Inuit rely heavily on glucose production. Those enlarged livers appear to be a (healthy?) symptom of that glucose production—I never said it was deleterious. If we can agree on that, then we’re in good shape here.
None of what I presented here was intended to prove that the Inuit were unhealthy. It was only done to show that they were not in ketosis and therefore cannot be used as an example of a “healthy” ketogenic culture (as has often been done by LCHF advocates).
It’s simply erroneous to use the Inuit as “poster boys” for a ketogenic diet or somehow to prove the safety of a ketogenic diet. You can’t do that given what the scientific literature says about their high protein diet and their unique genetic adaptations for fat burning. I say it’s dishonest to use them as poster boys, but even if you disagree with me, relying on the Inuit to prove the safety of a ketogenic diet so is to commit the fallacy of affirming the consequent—a logical fallacy of inferring the converse from the original statement.
An example of this fallacy would be:
“All cats are animals. Ginger is an animal. Therefore, Ginger is a cat.”
I think anyone can see the problem with that logical fallacy. One can easily commit this exact same fallacy by saying:
“The Inuit VLC diet is healthy. A ketogenic diet is VLC. Therefore, a ketogenic diet is healthy.”
I’m trying to get you to understand that this logical fallacy illustrates why the Inuit cannot be used as “poster boys” for a ketogenic diet.
If you want to argue it’s possible that a culture can exist and thrive on VLC, then that’s fine. But that’s an entirely different statement and you’d need to clarify that they did not eat a Western ketogenic diet.
But arguing that Ginger is a cat is unacceptable and fallacious.
Cheers
I’ve been reading this back-and-forth about the Inuit for awhile, but haven’t commented until now. A few things come to mind: first off, who exactly are *the Inuit*? Aren’t they a series of different tribes in the Arctic region? Couldn’t they conceivably be eating slightly different diets? If we monitored the glucose reaction and ketone production of 4 Americans, could we come to any conclusions about the American diet and the health of all Americans?
I was under the impression that at least some of the Inuit ate pretty high fat diets. If you watch the documentary “My Big Fat Diet”- (you can google it on You Tube), those Inuit traditionally used a liberal amount of oolichan grease (not sure if I spelled that right). They dipped their fish in it, synonymous with dipping lobster in butter. Some Inuit ate mostly seal meat, which is pretty high in fat. Many groups rendered fat which they used to make pemmican. And I had read that berries preserved in seal fat was a delicacy which many of them ate in the winter. So I believe some of the tribes could have been eating a ketogenic diet; at least, I’m not convinced you can rule it out entirely.
About the protein issue: protein turns into glucose *only* if you eat more protein than what is needed for body processes, like tissue and cell regeneration. So it only turns into glucose if you eat an excess of what the body requires. This means that that amount will be different for each person. Some can eat a higher amount of protein and still be in ketosis- (I believe I may be one of those people). It could be that, living in a cold climate, exercising as they do, and eating zero to minimal carbohydrate might mean that they require more protein. Some of the papers you gave links to simply claimed “they couldn’t be in ketosis because they ate too much protein”, but I’m not convinced that’s true. Again, I’m not sure you can rule it out. In western, very low carb diets the protein recommendation may be on the low side in order to ensure that the majority get into ketosis, as that varies from person to person.
If they used urine ketones to measure whether or not they were in ketosis- (I’m pretty sure blood ketone meters are a more recent thing)- that method is notoriously inaccurate, as when people are keto-adapted they often utilize the ketones rather than excrete them.
I’m not saying they definitely were in ketosis all the time; I don’t know this one way or the other. And, as I said, this may have varied between different groups of Inuit; it may have even varied between the seasons. These are just a few thoughts I had.
Morgana, The Inuit are a group of culturally similar indigenous peoples inhabiting the Arctic regions of Greenland, Canada, and Alaska. They used to be called “Eskimos” but that was considered to be offensive since it supposedly translated to “raw meat eaters”. Of course, their tendency of eating raw meat is yet another reason why they do not eat like Westerners do. I don’t see too many Western VLCers eating lots of raw meat.
Morgana said: “I’m not convinced that’s true”
As it has been explained by Peter, and others, the majority of Inuit have CPT1a mutations that while they burn FFAs, they struggle to produce ketones. As Peter wrote,
Even if you could prove that high protein is ketogenic, they cannot be used as an example of a “ketogenic” culture because of their highly prevalent CPT1a mutation. Everyone produces some ketones, including me, but we wouldn’t consider me to be “ketogenic” just because I produce some ketones.
Interestingly, the Inuit deficiency of CPT1a appears to force FA oxidation to brown fat. See the main graphic here, in this paper:
Adipose Fatty Acid Oxidation Is Required for Thermogenesis and Potentiates Oxidative Stress-Induced Inflammation
Since we don’t have CPT1a deficiencies, this suggests that we are burning fat in different cells than they do (mainly brown fat). They need to produce heat, after all. They were known to be warm to the touch, even on the coldest days.
Anyhow, the high protein diet is just another reason on top of their unique deficiency in CPT1a why they were not considered to be ketogenic.
It seems like people now suddenly want to redefine what “ketogenic” is, however the classic therapeutic ketogenic diet contained a specific ratio by weight of fat to combined protein and carbohydrate. (This is the “customary convention” of ketosis that Sinclair 1953 referred to). We should all be able to agree that the Inuit did not satisfy the classic “customary convention” of ketosis. Certainly the children did not as they have been known to die when their bodies attempt to rely on ketones for survival. If there is a brand new definition of what “ketogenic” is, that would be news to me.
Now, if you want to redefine what a “ketogenic” diet is, then you ought to institute a name change since the Inuit obviously do not produce many ketones. Otherwise we are conflating the medically recognized definitions.
Morgana said: “Some can eat a higher amount of protein and still be in ketosis”
If you have evidence showing a lowering of the ketogenic dietary fat requirement for people who are not using one of the three known changes in fat sourcing and protein demand (weight-loss, athletic demand or MCT oils), you’ll have to provide evidence. That would be groundbreaking (you should publish it!) and it would be great to have a citable reference for that. I have yet to find any evidence to change the ketogenic/anti-ketogenic macro-nutrients ratio for situations outside of those three known changes.
Of course, the Inuit were not trying to lose weight and they are known to have difficulty fasting after hours of strenuous work—they require snacks to avoid hypoketotic hypoglycemia.
This is not to say that the adult Inuit could never be in a mild ketosis. I’m sure some did enter ketosis in some situations, like starvation. Nevertheless, as Bryan has pointed out, they don’t do ketosis as well as Westerners do. And they don’t satisfy the customary convention of a ketogenic diet and they burn fats very differently than we do.
So, again, I have no idea why anyone would think they are a proxy for a Western customary ketogenic diet. A VLC diet? Yes, albeit a very unique one (very high n-3 PUFA with extremely rare PUFA-burning genes).
As you can see, there was a reason why Peter distanced himself from the Inuit. And he wasn’t alone. This debate first happened in Sweden and prominent Swedish LCHF advocates Andreas Eenfeldt[1][2] and Annika Dahlquist[3] quickly distanced themselves from the Inuit after they reviewed the evidence.
Those are the words of one of the most prominent LCHF doctors in Sweden. So, I don’t see what the fuss is here.
Obviously this revelation does not detract from the efficacy of a ketogenic diet. It just means that the Inuit are not a proxy for such a diet. The Swedes, and Peter, seem to understand this quite well. I’m surprised others here aren’t able to reach the same conclusion.
Duck Dodgers- I think you misunderstood much of what I was trying to say, and, although you supplied several links, you didn’t really supply many answers. My main point was that there are different groups of people who are called “Inuit”, and it’s unclear to me how many of them have actually been studied, how many of them really eat a high protein diet- (I know at least some Inuit eat a higher fat diet), how many of them really have this genetic mutation- (according to the link you posted some, but not all)- and if we can make a generalization about all Inuit based on- (at least, the link I looked at)- 4 people. It doesn’t matter to me what Andreas Eenfeldt believes about the situation, I like to see evidence and come to my own conclusion. By the way, I’m not saying you’re wrong, it’s just that the links you’ve posted have raised more questions for me than answers.
But first: about raw meat: yes, I do eat raw meat, and I’m sure that at least some low carbers do too. I eat raw herring this time of year, and occasionally raw salmon. I eat salted, hung dried ham in the form of Parma ham or Serrano ham. I also eat a venison salami sometimes; I like carpaccio of all sorts, and many people eat steak tartare, so yes, some of us do eat raw meat. I’m not sure what the point is, it might be neither “here nor there”, but I just thought I’d mention that I do eat it.
Also, I don’t think I was “changing the definition of ketosis”. Ketosis is normally defined by a blood ketone reading of at least .5 Mm to about 3.0- (this is the optimal range). The classic ketogenic diet used to treat epilepsy in the past is neither here not there; it is not necessary to use that diet to go into ketosis, and actually, nowadays they’ve discovered that the less restrictive Atkins diet works just as well for people with epilepsy. The ability to get into ketosis varies from person to person; there is no “one size fits all” in terms of a certain macronutrient profile. According to Dr. Seyfried, women often can get into ketosis easier than men; and according to Dr. Jeff Volek, thin people and athletes also generally have an easier time getting into ketosis. (I won’t supply links, sorry, it’s too late here and I’m getting ready for bed. These were 2 interviews I saw on You Tube. Unfortunately they are long, and I don’t know at exactly what mark they said these things). In any case, what that means is that some people are able to eat more carbohydrate than others and still be in ketosis, i.e., the blood meter range; this goes for protein as well. Of course, obviously eating a huge amount of protein will keep one out of ketosis, it’s just that I’m not totally convinced that *all* Inuit ate a huge amount of protein, though it looks like some did.
Not sure if you’ve bowed out of this discussion or not, but I thought I’d clarify those few points.
Morgana, to chime in about the raw meat (and fermented meat since Inuit do that too), more non-Inuit folks eat it than we may realize. Many eat raw oysters. Sashimi is quite popular in Japan and in many metro areas in North America. Some sauces, like true fish sauce and Worcestershire sauce has fermented anchovies in it. About the herring, I get that in our season for it (this month and next) and pickle them, except I eat the milt and roe sashimi-style (raw) as is common in Japanese cuisine. Same with uni (sea urchin) when I can find it in the store. I gently split the uni open clamshell-style with a cleaver, squeeze some Meyer lemon juice on the orange-y egg sacs and down the hatch yum. Tastes like the sea. Also, like you, I make tartare, from meat and salmon. You find cultures all over the world fermenting fish: https://en.wikipedia.org/wiki/Fermented_fish
Swedes ferment herring (surströmming) and the Icelanders ferment shark (Hákarl). Granted those two ferments are acquired tastes to be sure! But few people think the Swedes and Icelanders are fundamentally “different from us” because they eat raw meats. –Bryan
Why would eating raw meat make anyone think the eaters are “fundamentally different”? Many European nations, as well as Asian ones, have their raw meat dishes: carpaccio, ceviche, etc. In the early 1900s, when forensic medicine was in its infancy, German immigrants in large cities contracted trichinosis by eating raw pork — they did it in the motherland, and had no problem there because they didn’t feed their hogs garbage as we did in the US (As an aside, the fascinating, and, I fear, now out-of-print, book, “Eleven Blue Men” has some fascinating stories of early medical forensics, including how the trichina problem was identified). It seems only in the second half of the 20th Century that Americans got turned off on the idea of raw flesh. Perhaps that was a a good thing, with the mass production of beef.
Annie what you ask: “Why would eating raw meat make anyone think the eaters are ‘fundamentally different’?” This traces back to what Duck wrote to Morgana a couple of days ago (the 13th):
“Of course, their [the Inuit] tendency of eating raw meat is yet another reason why they do not eat like Westerners do…”
This is part of Duck’s persistent efforts to categorically portray “the Inuit” and “the Inuit diet” as profoundly different from “us” and “our diet.” As though “the Inuit” are some monolithic block of people who all share the same special adaptive genes and eat just the same type of diet at all times, however far-flung they may be around the circum-Arctic. Duck categorically asserts things like “…the Inuit diet is not a proxy Western VLC diets”, that “ [the Inuit] …evolved differently than we did,” and “The Inuit are not an example of what happens in Western metabolisms.” He even suggests “the Inuit diet” is somehow unsuitable and even harmful, saying things like: “…they [stayed in gluconeogenesis] by eating excessive levels of protein…” and “…Krogh & Krogh observed excessive protein intakes…” and “…they …produce a lot of endogenous glucose from their excessive protein intake…”
All this to imply that “the Inuit” are so different from us that the rest of the world can derive no lifeway or foodway lessons from them. As Morgana, I, and some others here have been suggesting, the picture is much more complex and nuanced. I maintain that the Yupik-Inuit ancestral foodways are likely much healthier than how Duck portrays them and that they can serve as a tremendous inspiration and guide for the many millions of metabolically sick people who are considering VLC but viscerally fear it due to life-long massive pro-carb anti-fat acculturation. However much I may have misunderstood certain details of it at the time I learned about it in 2007, the Inuit experience critically aided my journey back to health. –Bryan
Hi Morgana. Good question “who exactly are *the Inuit*? The nomenclature’s a WIP. I attended high school in Canada with lots of First Peoples including Inuit from Quebec and Iqaluit in the part of former NWT now called Nunavut. My Inuit classmates were already eating loads of SAD of course, but still hunted (on snowmobiles, in power boats) and did seem partial to maktaaq (muktuk = blubber = 90+% fat). This was back when Canada started moving to call them Inuit. We slid into referring to all the closely related circumpolar peoples “Inuit” even though the Yupik of far eastern Siberia and Alaska don’t call themselves that. Many sources still collectively refer to all of them as “Eskimo” though some promote “Inuit-Yupik.” These two links offer more detail on them and somewhat complement Wikis and US/Canada gov’t sources:
http://www.britannica.com/topic/Eskimo-people
http://www.inuulitsivik.ca/northern-life-and-inuit-culture/who-are-the-inuits
Ancestrally, Inuit-Yupik typically didn’t live so much in “tribes” as in very small single- or several-family units. Most live near the sea and traditionally derive most of their calories from large very blubber-rich marine life, like seals and the bowhead whale. Morgana you said “I was under the impression that at least some of the Inuit ate pretty high fat diets.” and all I’ve learned agrees with that: Fat was the Inuit-Yupik’s main calorie source. At least for the coastal peoples, and most Inuit-Yupik are coastal dwellers. Morgana, you ask “Couldn’t they conceivably be eating slightly different diets?” yes they do, depending on where they live and the season. Veg-wise at one end of the spectrum, some ancestrally-living Siberian Yupik (at least in Chukotka) most consistently included veg, even using root cellars. Alaskan Inuit and Yupik Some regularly ate sea veg, other not so much. At the other end of the spectrum are the far Northern Greenland Inuit, like those around Qaanaaq, who ate virtually no veg because it was rarely available. The inland Inuit, like the reindeer Yupik in Siberia and caribou hunters in Alaska, had a harder time getting iodine, so ate the thyroid glands of these big ungulates, esp during the typical times to conceive children.
For the ancestral foodway stuff I expect you’ll want my sources and I’m busy trying to find them! This is from my research 5–7 years ago, early on in my LCHF journey. Please bear with me while I find them. Meanwhile you can find some of it in Susan Allport’s book “The Queen of Fats.”
Finally Morgana about what you say: “… I believe some of the tribes could have been eating a ketogenic diet…” The more I delve into this matter with Duck and others, the more the Inuit experience raises a fascinating question. What conditions define their energy metabolic state(s)? Indeed what conditions define the energy metabolic states of any of us?
For example, let’s look at one of the most recent direct measures we have on this matter. In their 1972 report, Ho et al say:
“…Each Eskimo’s serum was tested for the presence of ketone bodies … and all serums were negative. This does not preclude an increase in ketone body production during this time… The fact that the Eskimos had high serum FFA and low glucose levels (~65 mg/dL) indicated that free fatty acids played a major role in body energy production…”
Picking this apart, I began to realize that terms like “ketosis” and “glycolysis” sorely lack comprehensive definition. No-one can give us a broadly accepted def for those two terms. We foodway-focused folks typically–perhaps sloppily–default to the term “ketosis” as a default state in which *all* fat-derived energy–ketones and FFAs–predominate over glucose derived energy (glycolysis). Maybe we need a more precise term to encompass all fat-derived energy. How about “keto-lipolysis?” How does that sound to everyone?
Let’s go with keto-lipolysis for the moment. Morgana, we still don’t know how to determine which energy-metabolic state predominates–glycolysis or keto-lypolysis. Do we go by sheer millimolars of glucose and fats+ketones in serum at any given moment–whichever has the greatest concentration wins? Or rather is it by calories delivered to our tissues at any given moment–the one that delivers the most calories at any one time wins? Or rather is it whether or not the metabolic conditions at any given moment trip the insulin switch to start/stop mobilizing fats from adipose tissue? Is it some combo of these three conditions? Again, we have no broadly accepted defs. Indeed I find remarkably few *proposed* defs. However, when you look at what Ho et al found–very low serum glucose (65mg/dL) and highly mobilize FFAs, keto-lipolysis wins hands-down by all three defs.
By the FFA-excluding definition of ketosis that Duck promotes, these Inuit are most likely not in ketosis. But for those of us looking at LCHF, that is a moot point, esp since non-Inuit appear to be much better at ketosis anyway. For us seeking to optimize our health through diet, Duck’s strict def of ketosis is utterly irrelevant. Much more important: are these Inuit in glycolysis? Regardless of how much gluconeogenesis they may or may not be doing? By the above defs, these Inuit are definitely not in glycolysis. For us seeking to optimize our health through diet, that’s what we care about. For us, to dwell solely on how much gluconeogenesis the Inuit or anyone else are doing is an utter waste of time. What we care about is whether or not we are in keto-lipolysis or glycolysis. By as many relevant measures of these states as possible –Bryan
Bryan said: “Duck’s strict def of ketosis is utterly irrelevant”
lol. You’ve got to be kidding me. This is yet another fallacy—moving the goalposts.
As if I invented the actual definition of ketosis. Give me a break. What universe do we live in where you get to redefine ketosis as being something that isn’t ketosis?
Do yourself a favor and look up the word “ketosis” in any medical dictionary and textbook. You’ll find that it says that ketosis is a “raised levels of ketone bodies in the body tissues.” The Inuit do not fit that definition.
But feel free to reinvent the definition if you like. lol
Duck, maybe you’ve been missing the message.
For people looking to improve their health with LCHF, looking at ketosis in isolation DOESN’T WORK.
Just wondering Duck. What part of that don’t you understand?
Also, you utterly fail to produce a broadly accepted comprehensive definition for ketosis. We’ve been around this block before. You didn’t do it in your last post. You’ve never done it in any previous posts. You won’t in the future until when and even if the global establishment agrees it. To simply say “raised levels of ketone bodies in the body tissues” doesn’t even begin to cut it. Raised from what level? To what level? Is fat mobilized from adipose tissue or not? What are the serum glucose levels? All those considerations matter greatly for our overall health.
Duck, you can’t even keep your own various defs of “ketosis” straight. On December 3rd, you posted this: “Ketosis /kɨˈtoʊsɨs/ is a metabolic state where most of the body’s energy supply comes from ketone bodies in the blood.” Guess what Duck? “Raised” levels of ketones do not necessarily mean “most of the body’s energy supply comes from ketone bodies.” And the def you gave on the 3rd says “ketone bodies in the *blood*” But the def you give today says “ketone bodies in the *body tissues*” So which is it Duck? “blood” or “body tissues?”
Duck, if you want, keep flogging your “Inuit are different” “low ketosis,” “high gluconeogenesis” stuff in your craftily crafting way. Just please don’t expect me to stop calling you on the bullsh*t I find in it. –Bryan
Bryan said: “So which is it Duck? “blood” or “body tissues?”
lol. It makes no difference since the Inuit cannot manage to produce many ketones either way!
And with that, I’m afraid our time is done here, Bryan. As I mentioned earlier, the Inuit debate already happened in Sweden last year and it was decided by LCHF advocates that the Inuit have no business being compared to a ketogenic diet. Peter obviously agrees. As do I. So, there’s nothing left to say. That debate ended a year ago. Let it go.
Take care, Bryan. I’m out.
Take care Duck. Bye bye. –Bryan
wbryanh- My question “who are the Inuit” was basically a rhetorical question. The point I was trying to make to Duck Dodgers is that- since “the Inuit” consists of many groups of people- it’s not clear to me at all that every single one of them eats a high protein diet, has enlarged livers, and has trouble producing ketone bodies, though I see by the research that at least some do. According to the link that Duck Dodgers posted, in the groups where this mutation appears, approximately 68% of them have this genetic mutation. Although that is a high number, what can we say about the others who don’t have it? (Apparently, according to that same link, the native peoples of inland Alaska don’t have that mutation at all). It is thought that this mutation used to confer a metabolic advantage in the past, but has become detrimental in the present day. In the link below, it is mentioned that this mutation might have ensured that they didn’t over-produce ketone bodies, due to their unique living situation and diet. (This is all conjecture of course, but the article does mention “high fat diets” and “ketosis”, implying that at least some Inuit are, or were, in ketosis):
http://www.sciencedirect.com/science/article/pii/S0002929714004224
By the way wbryanh, you don’t need to supply any links or “proof” for me that the Inuit ate a high fat diet; I’ve read many times that they did, and it was mentioned in the documentary that I wrote about in my post to Duck Dodgers. The “high fat” aspect was even mentioned in the link that Duck Dodgers posted, as it is in the link above. I hadn’t read in the past that they ate huge amounts of protein- (I didn’t realize it was even possible to eat that much protein, as I thought it made people sick). It’s possible I guess that some did and some didn’t. In any case, I’m not saying that all that was said about the Inuit was all wrong, it’s just that- natural skeptic that I am- some of the evidence seemed a bit conflicting to me, and raised a few questions.
Oh OK Morgana. Thanks. That (probably missense) CPT1a variant does intrigue me. My thought is that it compels more FFAs to go straight to thermogenic tissue, e.g. brown adipose tissue. But who knows? I can’t warm to the idea thought that it’s some “liver-sparing” thing. My sense is that our GIs are too good at vetting trigs in the duodenum to allow a whopping load of long-chain polys to go systemic. –Bryan
I said … “to allow a whopping load of long-chain polys to go systemic.” That is, Morgana, except to let them in to burn right away, e.g for thermal energy. –Bryan
Morgana, rereading your post, I’m absorbing more good points you made. 68% of northern indigenous peoples in far eastern Siberia with the variant means almost *a third* of them have the normal CPT1a gene per that link you gave, making them “less different than us:”
http://www.sciencedirect.com/science/article/pii/S0002929714004224
That gene variant rate could be greater or less for the Yupik-Inuit in Alaska, Canada, and Greenland.
To dilute the message and muddy the waters still further, the researchers tested Chukchi and Koryaks as well as “Eskimo” (I assume here they mean Yupik, the only Eskimo people I know of in Siberia). I couldn’t find anywhere it says how many of each group they tested. Was it an even mix of the three groups? Or weighted toward one or two of those groups? It’s likely the “Eskimos” were a minority in this little cohort.
The Koryak are especially interesting because they live south of the Yupik and Chukchi and appear to eat more plant-sourced food. This Koryak Wiki, https://en.wikipedia.org/wiki/Koryaks, says:
“… Salmon and other freshwater fish as well as berries and roots played a major part in the diet…”
The last point on that CPT1a gene variant: How much weight can we put in a sample rate of only 25 people?
Morgana, about the article quote you cited: “…mutation could be protective against overproduction of ketone bodies…” Yes, interesting that this piece also points to a high fat diet with the Yupik and other indigenes. And like you say the risk of “overproduction of ketones” is conjecture. I’ve heard of plenty of accounts of people on high-fat diets testing negative for ketones, and that was my experience too. When I went 80% fat 15% protein 5% digestible carb in early 2008, I tested my ketones for several months and it always came up negative on the strip. That makes sense. Our bods have at least several ways to regulate our ketone body levels. Our very neuron-rich GI constantly communicates with our brain regarding energy needs, and is able to vet to a great degree the dietary fats in the duodenum, deciding whether the body needs them (for structure and energy) or not, letting the excess wend down to the exit. Even if some excess fat goes systemic we may have ways besides CPT1a variants to gate conversion to ketone bodies, like storing the fat in adipose tissue. Finally, we can easily purge unused ketone bodies that exist at physiological levels. β-hydroxybutyrate and acetoacetate spontaneously break down into acetone, a volatile compound we eliminate through our pores and breath. –Bryan
wbryanh- yes, good point about the ketones. Ketosis isn’t “dangerous”, like some people seem to think, and the body has ways to regulate it. In any case, it’s curious why and how that mutation came about. I wonder how prevalent it was in their ancestral past- (before the introduction of modern foods into their diet?) I think it was mentioned somewhere that most of the people who were tested were already eating at least some non-traditional foods, though I don’t know if that has any relevance at all. In any case, I’d like to study this further….(not tonight though, I just got back from a long day of work). I’ll let you know if I find anything.
Morgana, yes, I’m curious to know too. More and more, I wonder what life factors select for it. Duck posted something recently about how the CPT1a deficiency variant is common among the Hutterites. It’s also common in the Koryaks even though they have more consistent access to veg than the Yupik and Chukchi. Anyway the research is there waiting for you when you get rested up. 🙂 –Bryan
wbryanh- Been looking for information about this mutation. It’s hard to find what I’m looking for- (maybe not much is known about it)- but most of the medical literature looks at it as a “deficiency disease”- (it’s the cause of a high infant mortality rate). Since it’s relatively prevalent in certain Arctic communities, it’s suspected that it served an advantage at one time, though no one seems to be in agreement as to what this advantage might have been. I thought this was an interesting link- it states once again that not all Inuit have this mutation (they give some specific information about the percentages). They also mention that the Inuit ate a high fat diet, not necessarily a high protein diet (although I guess one doesn’t preclude the other): http://pediatrics.aappublications.org/content/130/5/e1162.full
It has been mentioned that this mutation seems to protect against diabetes (though I don’t understand the mechanism). I’ve been trying to discover exactly when in time this mutation became prevalent, and if it was before or after the introduction of “Western” foods- (which I guess many of them have been eating for quite awhile). Could be interesting…..
Like always, there’s a bit of conflicting information. I’ll keep looking though.
Hi Morgana. About CPT1a deficiency, I’m into a house repair right now, but the Pediatrics piece you posted is very interesting and I’ll come back to read it more closely. I’m wondering if it has more to do with lots of long-chain w3 in the diet, regardless of calories burned and extreme cold? The highest verified rate of the deficiency I know of are for those 25 indigenes in Siberia that got their genomes sequenced, and they were a mix of Eskimo (Yupik), Chukchi and Koryak, the latter who lived further south, and that 68% or roughly 2:1 for having the homozygote. (Btw, I don’t know of any such sequencing studies for Alaska, Canada, and Greenland Yupik-Inuit.) But all these people are coastal and eat sea life. Then in that Pediatrics piece you posted, on page e1166, you see 1:4 for the coastal BC indigenes on Vancouver Island, where the weather is very mild, and usually don’t have to spend so much energy hunting for food and warding off cold. The ratio drops down dramatically as you move inland away from big w3 sources. The Hutterites in NA are 1:16, but many lived in coastal Europe (Amsterdam, Leeuwarden, Danzig (i.e. Gdansk) before coming to NA, so maybe lots of herring? Anyway, these are my quick thoughts on it.
About the Inuit eating a high fat diet, it makes sense to me. I don’t doubt they eat very high protein at times when they have to. But from just about all I’ve read and heard, the Inuit favor fat. About what level “excessive” protein may be, I found this Wiki that suggests actual numbers:
https://en.wikipedia.org/wiki/Rabbit_starvation
which has this: ” …It has been observed that the human liver cannot safely metabolise much more than 221–301 g of protein per day (for an 80 kg/176 pound person)…” Ducks posted studies of Inuit eating up to that much, 280–300g. I don’t recall any going beyond that, but quite possibly overlooked them. I even have personal experience with a high protein diet. I spent a month in 2007 dialing up to 300g/day protein, and kept it there from Aug–Nov 2007 (not July–Oct like I said earlier) and felt fine except for ammonia breath and peeing 3–4x/night. Fact is, no-one commits to any figure that constitutes “excessive.” That Wiki continues:
“…given the lack of scientific data on the effects of high-protein diets, and the observed ability of the liver to compensate over a few days for a shift in protein intake, the US Food and Nutrition Board does not set a tolerable upper intake level nor upper acceptable macronutrient distribution range for protein.”
Per this anyway, our livers adjust very quickly to a high-protein diet.
OK Morgana back to carpet-laying. Lots to follow up on! –Bryan
wbryanh- okay, in looking further, it seems that this mutation appeared thousands of years ago; though it’s hard to know how widespread it was, or exactly when it became so prevalent. What about life before this mutation developed: were the Inuit in ketosis? It is a recessive gene, and apparently both parents need to carry the gene in order for it to appear- (I can re-find the links if you need). It’s considered a “deficiency disease”, so researchers have wondered why it’s so prevalent in these Arctic groups. It can cause problems (as we know), like hypoglycemia and high infant mortality, which wouldn’t bode well for the people. It’s been called a “paradox”. Researchers theorize that it probably incurred some kind of benefit in the past, when they were on their traditional diets. One of the common theories is that it “protected them from their high fat diet”; (that is, of course, assuming that high fat diets are “dangerous” and that we need “protection” from them). I haven’t figured out what the mechanism would be that would “protect” them, nor has that been explained. In addition, there are several other theories as to why this mutation might be advantageous (for instance, it keeps them warm, which makes more sense to me).
But looking at it from another angle: what is the “cure” for hypoglycemia? A low carb, or even a ketogenic diet. It was bandied about in the comment section of an article about the Inuit on the blog of Dr. Eades (“Protein Power”) that possibly this mutation appeared in the gene pool, but since they were fat burners (possibly even ketogenic)- the gene just “stuck around”, not doing any damage, whereas in other populations who eat higher carbohydrate diets it would have been selected out. This might explain why it’s far more prevalent in certain populations (the coastal), as you mentioned. Do the inland Inuit eat more carbohydrates? (I believe you said they did). In any case, that’s another possibility, the way I see it; that rather than incurring an evolutionary advantage- (some liken it to sickle cell anemia)- maybe it simply wasn’t causing too many problems on their native diet, but now it is problematic on their modern diets. I’m not saying this is definitely the case; I just believe it could be plausible.
Below is a link explaining how breastfed infants (when they are exclusively breast fed) are in a state of ketosis. I believe the Inuit, like most hunter gatherer cultures, breastfed their babies for a pretty long time. And I guess Duck mentioned that the babies with this gene mutation had to be fed very often- (at least, the ones who had been exposed to modern foods, or formula). It’s kind of hard to ascertain how things were on their native diet, as the Inuit have been exposed to modern foods for quite awhile now. (So, as you mentioned before, maybe they are burning fatty acids, but do “ketosis differently” than we do?)
http://www.ketotic.org/2014/01/babies-thrive-under-ketogenic-metabolism.html
Morgana, what you say here: “…the gene just “stuck around”, not doing any damage…” I definitely want to explore more that option. The longer the fat chain, the less polar it is, thus the less of it travels directly from the duodenum through the hepatic portal because long-chain fats simply don’t travel well in serum. Rather the vast majority of these very long chain w3 fats (20-C and 22-C long) have to take the long roundabout “milk-run” (fat-run?) on chylomicron “buses.” Our GIs load these long-chain fats onto chylomicrons and send them into our lymph system where they travel all the way up to our left subclavian vein where they finally enter serum. (Here’s a Wiki with details on it: https://en.wikipedia.org/wiki/Chylomicron ) I suspect for Yupik-Inuit and related circum-Arctic folks who adapted to such a rugged and intensely cold place, their bods suck up loads of these fats into thermogenic tissue, like brown adipose tissue, long before they ever have a chance to make it down to the liver. So maybe it’s that, despite a diet hugely high in these w3s, remarkably few of these Inuit lipos ever make it to the liver, and so CPT1a fell into disuse. As for evol selective pressures, maybe the need to generate the max thermal energy simply to not freeze to death trumps the problem of need to frequently feed Inuit infants. Of course on all this hard tellin’ not havin’ the actual isotope-tracer tests to show us. But this is one of the ideas I’m noodling around. –Bryan
Expanding on my last comment Morgana, could be the relatively high rates of the CPT1a deficiency homozygote in coastal BC indigenes, like those on Vancouver Island, may be vestigial? At least in part? Left over from when the original First Peoples crossed the Bering Land Bridge 15–20k years ago? We have evidence the homozygote is quite common in current day Siberians from those 25 gene sequences showing the 68% presence for the deficiency in Yupik/Chukchi/Koryak. Could be CPT1a deficiency traveled across the Land Bridge in these original First Peoples, stayed prevalent in the Yupik-Inuit and others in the far north due to enviro pressures, and had time over the relatively few millennia to go only partially heterozygotic. Esp for their relatives such as the coastal indigenes who migrated south and who still eat a high w3 fish diet so less enviro pressure to go heterozygotic. Meanwhile those who migrated inland like the BC interior, away from high w3 and possibly more carbs, experienced more evol pressure to go heterozygotic but even so they still retain vestigially the deficiency. Again all this from reasoning, no proof. –Bryan
Morgana, you bring up other points I’d like to address, but have to stay on the hateful toxic task of laying wall-to-wall. I hope to come back this evening, early morning your time. BTW, It’s Duck who’s been saying the Inuit “…do ketosis differently from the way we do.” I’m not sure what Duck fully and exactly means when he says that. But I’m willing to consider the idea it includes fewer ketones. Which brings up an interesting question: Why do Yupik-Inuit infants need to eat frequently, but the adults can fast? What life-time adaptations allow the adults to do that? I may be overlooking simple answers here, but have my mind on the carpet task. OK Morgana, to be continued. –Bryan
Looking forward to it!
wbryanh- below is a link explaining how glycogen is converted to lactic acid after the animal is killed. One of the points made is that if the animal is stressed, or exercising- (like if it is being hunted?) the glycogen goes into the bloodstream and basically gets used up. Of course, they are talking about muscle meats here, so I don’t know how that applies to liver or to sea animals and their skin:
http://www.fao.org/docrep/t0562e/t0562e02.htm
Generally, there are small amounts of carbohydrate in meat (more in liver), but usually it is considered minimal, and therefore not included in macronutrient ratios. (Well, in the meat that *we* eat anyway). There are also small amounts of carbohydrates in eggs; (the eggs of sea birds were also eaten quite a lot by the Inuit).
Morgana, thanks for the FAO link. I’ve been meaning to look more into glycogen depletion during animal stress like during hunts. The Yupik-Inuit going on often protracted hunts and taking sometimes hours, like in the case of whales, to chase and make the kill. So it’s easy to imagine these creatures convert at least some (most? all?) of their glycogen to lactic acid.
Shellfish–at least bivalves–have a lot of glycogen. I wonder how much the bivalve feels stress and drives its glycogen to lactic acid? –Bryan
wbryanh- below is a link about the carbohydrate content of shellfish after death. (There is a table as well). You will note that although shellfish does contain carbohydrate, it’s still pretty minimal (at least the ones listed). By the way, I don’t agree with everything he writes in this article (mainly his opinion on cheese). But I thought the information about shellfish might interest you:
http://thepaleodiet.com/believe-shellfish-contains-carbohydrate/#.VnMcLVJl9DU
Hi Morgana. Thanks for Cordain’s shellfish carb missive. I hadn’t read anything by him for ages. Shellfish carb loads aren’t negligible and in my early days of taking control of my metabolic health (2007–2009), eating a bowlful of mussels definitely popped my blood glucose levels, though as usual I can’t discount other possible drivers. But even the most carb-filled shellfish (cooked whelks) at 15g/100g are still less carb dense than starchy tubers like boiled potato at 19g/100g of active carbs (http://ndb.nal.usda.gov/ndb/foods/show/3093). and not all that much more than some legumes like lentils at 11.5g/100g of active carbs. (http://ndb.nal.usda.gov/ndb/foods/show/4989) Lentils are on a par with carby shellfish runners-up mussels and abalone. Plus, shellfish comes with a big load of vitamins and minerals which may help offset the BG-popping effect of the carbs.
Interesting, I don’t remember Cordain him being interested in food acid-base issues. I haven’t yet found much research to lead me to put much stock in dietary pH regimens. For healthy people anyway. Our bods offer plenty of ways to balance serum pH. About cheese, some people feel it sits in an ancestral murky zone. But I’ve never had much trouble with it. The path to cheese seems built on completely natural processes. Ruminants like sheep have rennet in their rumen which begins to curdle mother’s milk right in the rumen so the lamb can more easily and completely digest the dairy. –Bryan
Bryan: One note on blood glucose and shellfish. At one point I looked into the whole issue after a long conversation with an insulin-dependent diabetic. He very carefully tracked his sugar intake and blood glucose and dosed with insulin as needed, and had been quite successful at keeping his blood sugar steady.
But what surprised and confused me was that “carbs” were not the main issue. His BG would spike when he ate proteins too, but especially *certain* foods, not protein in general. Gluconeogenesis can be used by the body to produce glucose, but it takes time, and one dish of oysters wouldn’t do it.
What does spike BG quickly is anything that causes the body to release stored glycogen. And this is where one protein meal can have way more effect than another protein meal. Some of the factors have to do with how much assimilatable iron is in the meal, which is also affected by the Vit. C content, and probably polysaccharides and fat, and things like lactoferrin. Shellfish are super-high in minerals, including iron. So is liver, of course. Not so much in fat or “white meat”.
This doesn’t have much to do with the argument about “are Inuit in ketosis” of course, but it does affect the average low-carber who is looking at their BG. There is an excellent full-text article on the subject:
http://diabetes.diabetesjournals.org/content/51/8/2348.full
“Reciprocally, iron influences insulin action. Iron interferes with insulin inhibition of glucose production by the liver. Hepatic extraction and metabolism of insulin is reduced with increasing iron stores, leading to peripheral hyperinsulinemia (48). In fact, the initial and most common abnormality seen in iron overload conditions is liver insulin resistance (49). There is some evidence that iron overload also affects skeletal muscle (50), the main effector of insulin action.”
Anyway, I just think it’s another factor to consider. When I hear from people who are trying to “stay in ketosis” (as measured by ketostix) they often say that “eating too much protein” is an issue, and that they need to just eat mostly fat. But I don’t think “protein” is the only issue with the high-protein foods … the high mineral content has an effect too.
Hi Heather, thanks for the link on iron and T2D. Before I continue on that topic, let me address what you say here:
“Gluconeogenesis can be used by the body to produce glucose, but it takes time, and one dish of oysters wouldn’t do it…”
To be clear Heather, *dietary* glycogen, like what we find in shellfish, doesn’t need to pass through our livers. Our GIs’ α-amylases set upon this “animal starch” like they do on plant-sourced starches we eat like amylose and amylopectin.
https://en.wikipedia.org/wiki/Alpha-amylase
Starch digestion starts with salivary amylases in our mouths and continues in our duodena. So yes, the glycogen in shellfish may well be responsible for popping fragile BGs. I certainly saw that effect in the early days of my efforts to recover what I could of my broken glucose metabolism.
I can’t discount other possible factors like you point out. E.g. shellfish with its abundance of vits and mins, and esp of certain proteins like tropomyosin which can be quite allergenic for many people, causing an immune response, which is an inflammatory event that can pop fragile BGs.
Click to access InTech-Characterization_of_seafood_proteins_causing_allergic_diseases.pdf
That said, though the years I saw my carb tolerance generally improved regardless of my carb sources, e.g. shellfish, fruits, etc. So I do lean toward the idea that glycogen was largely responsible for those early effects.
Back to iron, that’s truly one of the big takeaways for me in our forum here. Of many takeaways; we’ve had so many excellent exchanges. I do think iron it could be a big issue that Duck and other people here have discussed. When I carefully tracked my meal nutrients in the spreadsheet (2008–2010), iron was one of those that routinely exceeded the RDI. Because of that, I started getting Iron/TIBC panels in 2009, and found my iron levels ride at the very high end of the normal ranges. I donate blood to lower them, but that effect doesn’t seem to last long. I need to keep digging into this. –Bryan
Yes, I agree the starches get into one’s system very quickly, esp. the dextrose starches. I had not thought about the carb content of seafood much until it came up here. But I do eat a lot of “Asian” style seafood, and shellfish are big on the menu! What is interesting is that a lot of them are just naturally and obviously sweet. I think some of them might even get sweeter as they dry. There might be some reaction that happens … like what happens with mushrooms, when dried in the sun the Vit D content gets very high.
But another weirdness in the Inuit diet may be that it would be high in taurine. There is a lot of taurine in seafood anyway, but it tends to get destroyed by cooking. Populations that tend to eat raw fish … like the Japanese and Inuit … get higher dosages of it. The more taurine, the better the heart-health markers.
So this could affect the Inuit in a few ways that aren’t related to genetics or carb content:
1. Taurine protects against heart disease, regardless of the other factors in the diet.
http://www.ncbi.nlm.nih.gov/pubmed/19239132
2. Taurine helps with fat digestion. It’s used to make bile.
http://www.livestrong.com/article/458271-taurine-and-bloating/
3. Taurine affects ketone production in the liver (in rats anyway: makes the liver more prone to produce ketones).
http://www.ncbi.nlm.nih.gov/pubmed/10629440
4. Taurine is key to glucose transport.
http://www.sciencedirect.com/science/article/pii/S0041008X11004455
In theory human beings can synthesize taurine, but it appears that getting more from your diet has really good health effects.
http://www.lifeextension.com/magazine/2013/6/The-Forgotten-Longevity-Benefits-of-Taurine/Page-01
————-
My body tends to hoard iron also, and after donating blood my hemoglobin just shoots right back up. I’m guessing that’s an adaptation to constant parasites in past ages. But it could also be an adaptation to thousands of years of eating whole grains. My ancestors lived mainly off oatmeal, and whole oatmeal is a big iron-blocker.
heathertwist- thanks for that information on taurine; I didn’t know that before.
Morgana: You are welcome! I learn so much here.
So far it appears that all the “healthy” diets are in fact high-taurine diets (and most of them are also wheat-free, except the French). The Inuit have raw fish and meat. The Japanese and Okinawans, of course, have their raw fish, plus octopus which is super-high in taurine. The French have raw milk cheese, and maybe stuff like pickled herring (which is not cooked). The Maasai and Swiss have raw dairy. The Maasai also have (or used to have) raw blood.
There is a nice PDF here of the world-wide study:
https://www.google.com/url?sa=t&rct=j&q=&esrc=s&source=web&cd=5&cad=rja&uact=8&ved=0ahUKEwiQ4a3ijvDJAhVY2GMKHTCYBNMQFgg9MAQ&url=http%3A%2F%2Fwww.springer.com%2Fcda%2Fcontent%2Fdocument%2Fcda_downloaddocument%2F9780387756806-c2.pdf%3FSGWID%3D0-0-45-722329-p173764225&usg=AFQjCNHKTYjeVqom7LwE6ofYBk6spOeOEA&sig2=zkS5SWOq0WssgmOAoxUFKw
Has a nice graph of mortality rates vs. taurine excretion. Oddly, Finland and Sweden are low on the Taurine excretion graph.
The outliers to this theory are the healthier vegans: the Rice diet and the Japanese mountain people especially. Vegans though, often have *more* heart diseases than average, which is thought to be either the lack of B12 or the lack of “sulfated amino acids”. Also vegans in the US are low on taurine excretion: http://www.ncbi.nlm.nih.gov/pubmed/3354491
So how do some vegans stay healthy? I’m kind of wondering if the vegans that are super-healthy are also the ones that appear to have a high-sulfur diet (and some other source of B12). The Japanese mountain people live near a volcano and eat mainly roots which happen to be high in sulfur … maybe those roots happen to make it easier for the body to synthesize taurine. High-sulfur vegies might do the same thing: broccoli, cabbage etc., which are the backbone of many low-meat diets. Garlic of course, is high sulfur and noted for being “healthy”. Some water supplies are high in sulfur, and some are not.
It really would be ironic if the common feature of “healthy human diets” ends up being the secret of Pottinger’s cats …
Hi Heather, sorry to not write sooner. I was delving into your taurine links. Esp on its sulphur (S) content. Very interesting–thanks for these!
What surprises me a little, I rarely see discussion about vegans getting enough S. It’s so easy to get enough S on a non-vegan diet that those folks don’t have to think about it. But conceivably could be an issue for vegans who don’t eat enough brassicas like broc and cabbage and alliums (allia?) like garlic and onions. Here’s a WAP piece on it:
http://www.westonaprice.org/health-topics/heart-of-the-matter-sulfur-deficits-in-plant-based-diets/
After the “Organic Four” (C,H,O,N) and phosphorus (P) and calcium (Ca), S is one of the most common elements in our bods. We need it for all kinds of critical processes, including to make amino acids and to shuttle electrons in cells in addition to the reasons you gave Heather:
https://en.wikipedia.org/wiki/CHON
https://en.wikipedia.org/wiki/Composition_of_the_human_body
https://en.wikipedia.org/wiki/Sulfur#Biological_role
About our bods making enough of their own taurine from raw S from raw meat, cooked meat, S-rich veg etc. I eat raw meat/shellfish and love it, but could it be we can do fine on dairy/eggs/cooked meat/S-rich veg? I’m still trying to put a finer point on it. Here’s the links that Life Extension supp comp author gave us for it if you guys want to have pokes at it:
6) http://www.ncbi.nlm.nih.gov/pmc/articles/PMC2994408/ (full)
7) http://www.ncbi.nlm.nih.gov/pubmed/2496406 (abstract)
8) http://www.ncbi.nlm.nih.gov/pmc/articles/PMC3501277/ (full)
9) http://www.altmedrev.com/publications/3/2/128.pdf (full)
10) http://www.ncbi.nlm.nih.gov/pubmed/9437654 (abstract)
11) http://www.ncbi.nlm.nih.gov/pubmed/12514918 (abstract)
12) http://www.ncbi.nlm.nih.gov/pubmed/1811446 (abstract)
13) http://www.ncbi.nlm.nih.gov/pubmed/18305447 (abstract)
–Bryan
Heather btw, on endogenous vs supp taurine, I didn’t yet check the quality of the citation-containing journals. That’s a biggie cuz we’ve seen an explosion of bogus pay-for-print research journals the past decade. Even if you see an impressive ref in PubMed, all rich and science-y full of big words and graphs, you still could be getting a low-worth or even worthless report. You can go here to vet journals:
http://scholarlyoa.com/
Any journal I don’t immediately recognize (Lancet, BMJ, etc) I go to that site to check it. Free full texts more often come from bogus journals that the paywalled stuff. But you can find plenty of paywalled junk too.
Also, some of these links call taurine and “amino acid.” Some argue that’s wrong cuz taurine lacks the carboxyl group (-COOH). Anyway FYI: https://en.wikipedia.org/wiki/Amino_acid and of course Wiki’s not an unimpeachable source. –Bryan
Yeah, there are a lot of bogus studies out there now! On taurine though there is SO MUCH study and it mostly seems in agreement. Taurine was one of the first nutrition issues studied … Pottinger’s cats! What amazes me is that I haven’t heard about it much til now. Probably because I assumed that us meat eaters get plenty of it.
The surprising thing though is that it is not the case that a meat-eating diet automatically has enough taurine. When taurine *excretion* is measured, countries like Finland and England come out LOW in taurine. Clearly something else is going on. Likely how much the food is cooked is one big issue. And some foods compete with it. And some people seem to synthesize it better than others. There is so much to still be studied!
http://www.ncbi.nlm.nih.gov/pubmed/11510759
The French come out higher than Finland … maybe all that nice raw cheese. The variation in taurine excretion is kind of odd, given that it is supposedly easy to produce in the body.
I could see how some vegans get more sulfur than others, just based on the types of vegies they eat. Some of the popular vegan diets do stress eating lots of sulfur-vegies. But the rice diet seemed like an anomaly. And then it hit me: in the descriptions of the Rice diet, it was specified that fresh or dried fruit could be used! Given this is in the days when refrigerators were rarer, I’d guess there was a fair bit of dried fruit. And guess what? Dried fruit is often treated with sulfur!
Good set of links, thanks. I’ll peruse them.
And yeah, a lot of places call taurine an amino acid or a “conditionally essential amino acid”. It’s kind of a weird chemical in any case. It doesn’t actually get “used” all that much.
Heather, interesting! About what you say “…The surprising thing though is that it is not the case that a meat-eating diet automatically has enough taurine…” I’ll retract what I said “It’s so easy to get enough S on a non-vegan diet…” till we know more.
And great catch on the hidden sulphur in Kempner’s Rice Diet!
About Pottenger’s cats, first I heard of them, and have to laugh, makes me think of Schrödinger’s cat 🙂 But seriously the raw protein vs cooked animal-protein sources are interesting. Pottenger’s cats cough up confounderballs of course. First they are cats not people (as much as some beg to differ), we’ve had up to nearly two million years (per Richard Wrangham and others) of cooking our food, so we may have evolved adaptations to get/make/conserve taurine, and the results of Pottenger’s work, we can view them only correlatively. But those caveats said, it’s still exciting! About measuring taurine excretion, how to interpret the results? Can we simply say that greater taurine passing comes from greater taurine consumption and/or endogenous production? Or can it mean the excretor is more ably absorbing the available taurine than those who pass more of it, leaving less to go into urine? Or something else? So many variables.
About what you say here Heather, “…a lot of places call taurine an amino acid or a ‘conditionally essential amino acid’…” I agree there’s a lot of confusion about it out there in the web-o-sphere. I think most folks, when they hear “amino acid” they think “protein building block” which taurine almost certainly isn’t. I couldn’t find a single example of a protein that incorporates taurine into its AA chain. And don’t see how it could; its sulfonyl hydroxide sits right where the carboxyl group needs to be in order to link AAs together. See on page 9:
Click to access ch18-carboxylic%20acids.pdf
All that said, Heather, seems little doubt that our little oddball taurine is important! The relevant section out of this: http://jn.nutrition.org/content/136/6/1636S.long
“…Taurine is the most abundant free amino acid in animal tissues…In addition to its role in the synthesis of the bile salt taurocholate, taurine has been proposed…to act as an antioxidant, an intracellular osmolyte, a membrane stabilizer, and a neurotransmitter. …Taurine is found in mother’s milk, may be conditionally essential for human infants…recent work has begun to reveal taurine’s action in the retina. It appears that taurine, via an effect on a glycine receptor, promotes the generation of rod photoreceptor cells from retinal progenitor cells…”
BTW, another important S-containing compound is the vaunted antioxidant α-lipoic acid, which sports a disulfide bond.
https://en.wikipedia.org/wiki/Lipoic_acid
http://www.ncbi.nlm.nih.gov/pubmed/19998523
I took ALA (cheapo TJ’s racemic mix because I couldn’t afford ALA-R) as part of my gaggle of supps in 2008–2009. –Bryan
Bryan:
“About measuring taurine excretion, how to interpret the results? Can we simply say that greater taurine passing comes from greater taurine consumption and/or endogenous production? Or can it mean the excretor is more ably absorbing the available taurine than those who pass more of it, leaving less to go into urine? Or something else? So many variables.”
My daughter made an analogy I found interesting. She said maybe taurine is like oil in a watch. It just SITS there and doesn’t really “do anything” … but if the oil isn’t there the watch stops.
The people doing the Esselstyn protocol wouldn’t be ingesting any taurine to speak of. Since they are alive and actually healthy you can figure they are making as much taurine as they need. The studies seem to show that vegans do excrete taurine, so they create a little more than what they need? So they would be excreting the extra? And left to ones own devices, one creates more taurine than one actually currently needs? But the vegans do seem to excrete a lot less than non-vegans. And it seems pretty clear that the more taurine you excrete, the healthier you are and the longer you live? So again, where do the Esselstyn and Pritkin vegans fit in here?
So … which would be better: eating very little taurine, plenty of sulfur vegies, and very little fat … or eating lots of taurine with a generally healthy diet? What happens if you heat a high-fat vegan diet anyway?
I don’t know either. Doesn’t seem like it would be a difficult thing to study though.
Yes on the middens! It’s amazing, just how BIG some of those are. Well, if I had the choice of chasing a gazelle or picking through tide pools, I’d vote for the tide pool! Chimps sometimes kill mammals and eat them, but it takes them a lot of time to chew them. Bonobos pick food out of swamps, including shellfish and snails. The bonobos get more Omega 3’s.
Yet another interesting link:
http://www.ketotic.org/2012/08/if-you-eat-excess-protein-does-it-turn.html
Morgana, about excess dietary protein forcing (nor not) gluconeogenesis (GNG), thanks for that ketotic.org link. I’ve wondered about it too, though I admit I generally assumed more GNG till now. With your link I’ll delve more into this. Even before we discuss other possible GNG gating factors, I’d like to point out that a quarter or more–maybe way more–of the protein could be converted to ketones/fats, depending on protein’s amino acid mix. Of the 20 AAs, 13 are obligate glycogenic, 2 are obligate ketogenic (lipogenic?), and the remaining 5 swing either way depending on the bod’s conditions/needs.
https://en.wikipedia.org/wiki/Glucogenic_amino_acid
https://en.wikipedia.org/wiki/Ketogenic_amino_acid
Also Morgana even if we *do* see increased GNG, people with exquisite insulin sensitivity may do such a bang-up job rapaciously sucking glucose into their cells the moment it hits serum that these people keep enjoying very low mg/dL of blood glucose–low enough to still allow fat mobilization. Aren’t low BGs what really matter? Whatever the mix of energy metabolic states we’ve batted around ad naseum–glycolysis, ketosis, lipolysis–what may matter most is whether or not we trip the insulin switch which decides whether we keep fats stuck in adipose or mobilize fat into serum. IOW, it appears the *sustained* concentration* of glucose in serum is what matters, not how glucose is hitting serum at any one time. For ancestrally-living Inuit, all the direct measure evidence fits the bill–low serum glucose, lots of mobilized FFAs.
For the Yupik-Inuit, besides their subsistence foodways, steady hard work and frequent warding off of cold, they appear to have a unique advantage–exceptionally permeable cell membranes. w6 and w3 are our only “essential” fats, meaning we have to get them from diet, and they also appear to populate our cell membranes in proportion to how we get them in our diet. I.e. the less w6 and the more w3, the more w3 in relation to w6 we find in our cell membranes. w3 is slightly more flexible than w6, so a higher w3/w6 cell membrane ratio results in more permeable cells. The ancestrally living Inuit eat the highest w3/w6 ratio foodway of anyone on Earth, so possibly enjoy the most permeable cell membranes. This increased cell membrane porosity may maximize nutrient ingress including glucose and its closely related downstream metabolite, Vitamin C. This may help explain why the Yupik-Inuit seem to do so well on quite low glucose and Vitamin C. We need to look at the effects of high w3/w6 ratio cell membranes on the GLUT1 transporters: https://en.wikipedia.org/wiki/GLUT1 –Bryan
Thanks for that information on amino acids! Wow, I did not know that before. I feel like I’m learning a lot from this thread.
Happy New Year Morgana! Hope your holidays were peaceful and relaxing and healthful. OK, at least two of those three.
I finally returned to your ketotic.com link–via some intriguing stuff on fat-driven gluconeogenesis. Chris Masterjohn looks at the mounting evidence to suggest that our bods can make pyruvate/glucose from…ketone bodies! Specifically, from acetone:
http://blog.cholesterol-and-health.com/2012/01/we-really-can-make-glucose-from-fatty.html
That’s what circled me back to your link which suggests GNG output–even in the presence of excess AAs–remains more or less constant. Until now, I couldn’t picture what else could happen to excess (glucogenic) AAs except to go off to GNG, thus “necessarily forcing BGs higher.” I now consider other GNG processes might be going on at the same time, which the bod dials down as AA-driven GNG ramps up, all to maintain the same net output. Those other GNG sources include glucose from glycerol, the backbone compound for triglycerides. And now, apparently, glucose from acetone. Another candidate example of how we remain the robustly exquisitely homeostatic beings we are (or should be). –Bry
Thanks wbryanh, Happy New Year to you too! Also, thanks for that link, it was interesting. I especially thought that all those ketogenic diet “debunkers”- you know, the people who say the ketogenic diet is “unhealthy” and “unnatural” and is going to kill us- need to have access to this information!
Good timing on your post Morgana. I just made my first post at Chris’ site. I’m afraid I’m a little effusive about the his acetone → pyruvate discussion (thanks to a pair of gin and sodas). But maybe you’ll want to check it out anyway.
http://blog.cholesterol-and-health.com/2012/01/we-really-can-make-glucose-from-fatty.html?showComment=1452118854632#c3355989122137031760
I included that ketotic.com link you posted showing stable net GNG under varying inputs. –Bryan
Just noticed that this my first post on Masterjohn’s site (blog.cholesterol-and-health.com)–yesterday at 2:20pm–it calls me “Unknown.” My followup post calls me WBryanH as expected. –Bryan
The post I looked at (yesterday) called you just “Bryan”. This new link you sent me doesn’t seem to take me to the same article on ketones; there were things about cod liver oil and other stuff. In any case, it was clear yesterday which comment was yours, so no worries.
I’ve been thinking more about this theme. First off, it debunks the idea on “Perfect Health Diet” that there is a such thing as “glucose deficiency”- (I never believed in it in the first place, since I couldn’t find anything to back it up scientifically. I think Jaminet might have just made it up; although, generally, in regards to other matters I do respect much of what he says).
Also, I’m wondering if it might be harder for people who are not yet keto-adapted and used to eating high carb diets to make this conversion? I remember reading on Peter Attia’s blog that when he first started experimenting with the ketogenic diet, it was harder for him to generate enough energy in the beginning, whereas later on his body adapted and it became much easier. I noticed something similar when I first tried a low carb, keto-type diet- (though granted, I was also recovering from chemotherapy and a lot of other horrible treatments, so who knows how much that might have played a part). Eventually though, I noticed I had far more energy, and on a much more “even keel”, than when I was high carb.
In any case, it brings up a lot of questions. Hopefully Chris Masterjohn will do a follow up post.
Morgana, yes, I remember the “low-carb flu” in the first half of August 2007. I noticed it mainly in the first week. I’ve never heard that it lasts more than a few weeks. But evidently even that short time is enough to thwart many people. The only longer-term symptom I experienced was when I smelled baking bread and other baking wheat-based foods. Made it momentarily a little hard to walk past bakeries, doughnut shops and pizza parlors. Took ~ nine months for the fragrance to stop triggering me. Then one day, it magically stopped. I still love the smell of baking grain-based foods. I just don’t think about eating them.
About glucose deficiency–or more like carb deficiency to make clear we’re talking about *exogenous* and not our “home-grown” glucose from glycogen, GNG, etc. I’ve concluded it’s simply impossible for us to quantitatively determine such a problem can ever exist in healthy people. No-one can do this. Not the Jaminets. Nor anyone else.
Even keto champions like Mark Sisson, Emily Deans, etc, keep telling us “some brain cells need glucose.” But, again, no-one seems to have any proof of this.
Our *only* cells I’ve been able to confirm that absolutely positively require glucose at all times are our red blood cells. This because, afaik, our RBCs are our ONLY cells out of our 200+ cell types that *completely lack mitochondria.* Thus, our RBCs–which are essentially hollowed-out hemoglobin “tote sacks”–need to lacto-ferment glucose to generate enough energy for their very modest energy needs. E.g. to keep active nutrient (and maybe ion?) gradients across the cell membrane. Yes, Morgana, I said “lacto-ferment.* Just like we lacto-ferment sauerkraut and kimchi. Our RBCs are little fermenters! Amazing eh? BUT, no-one seems to have any idea how much glucose these cells require. Again, their energy needs are quite modest. They have little else to do besides passively course through our blood to deliver oxygen to cells and cart away the carbon dioxide. But as low as our RBCs’ energy needs are, that constant need may explain why we have to maintain some minimal level of blood glucose at all times. For BG to always be around to serve as little on-the-fly Gluco Happy Meals for the RBCs’ endless trips around our bods.
Here’s the only argument I’ve seen that even begins to make the case for some level of glucose dependency in non-RBC cells:
Biochemical, Physiological, and Molecular Aspects of Human Nutrition
By Martha H. Stipanuk, Marie A. Caudill. Page 211, near top of first column.
“…Other specialized cells are also primarily glycolytic because of a relative lack of mitochondria or limited blood or oxygen supply relative to their rates of metabolism; these include leukocytes, white muscle fibers, cells of the testis, the renal medulla, and some cells of the cornea, lens, and retina of the eye…”
But even here, Morgana, who’s actually *measured* any of this? E.g. who actually measured respiration in our eyes’ lenticular cells? Even for these “remote” cells, how do we know ketones can’t deliver all the energy goods? Those little ketone bodies diffuse through blood and tissue pretty fast and effectively. Esp acetone.
Could it be our RBCs are the *only* reason our bods need to produce glucose at all? At least for energy purposes?
It’s all such a massive load of “WE DON’T KNOW.” –Bryan
There are obligate glucose-requiring cells of the nervous system and/or brain – as a Type I diabetic on a very low-carb diet, I’m not affected by hypoglycemia until my blood sugar has been <60mg% for a long time. Then, I notice purple patches in my visual field, I feel the cold (even if it's not very cold), my thinking slows and I'm prone to errors of judgement. Ketosis protects against the hypoglycemic symptoms we want to avoid – seizures, coma, death – but hypoglycemia still leaves the brain sucking wind https://ketogenicdiabeticathlete.wordpress.com/2015/12/18/hypoglycemia-can-ketones-help-fuel-the-brain/
Jonathan, remember I said “it’s …impossible for us to quantitatively determine such a problem can ever exist *in healthy people.*” E.g. people who can rely on appropriate levels of endogenous insulin and don’t have to inject insulin. Injecting insulin can overwhelm the bod’s “home-grown” glucose, disposing too much of in into cells, driving BGs dangerously low. When we bring med interventions into the picture, all bets are off.
In such a case, your symptoms may come from under-fed RBCs that begin to fail to deliver enough oxygen to your cells. How do you know that’s not the case? We simply have no direct measurement of what’s really going on. We can propose and infer pathways, mechanisms and causes & effects all we want. But it’s very hard hard to prove any of them till we actually measure them. That’s what I’ve been talking about. –Bryan
Emily Deans reckons “Some cells in our brain are actually too small (or have tendrils that are too small) to accommodate mitochondria (the power plants). In those places, we must use glucose itself (via glycolysis) to create ATP” – seems more plausible
http://evolutionarypsychiatry.blogspot.com/2010/08/your-brain-on-ketones.html
Jonathan, I also read Emily Deans’ post where she makes that startling assertion. She doesn’t source it. She doesn’t tell us what we call those cells. She doesn’t even tell us if they are neuronal or glial cells.
Frankly, her claim makes no sense to me.
Our brains have two main classes of cells: neuronal and glial:
https://en.wikipedia.org/wiki/Brain#Cellular_structure
Some of the smallest neurons in the brain are Cerebellar granule cells
https://en.wikipedia.org/wiki/Cerebellum_granule_cell
and they come with mitochondria:
http://www.ncbi.nlm.nih.gov/pubmed/8931459
The smallest glial cells are the microglia:
Click to access NeurohistologyLectI.pdf
and they too contain mitochondria:
http://www.ncbi.nlm.nih.gov/pubmed/23815397
In fact, astrocytes, our brains’ most abundant glial cells, not only sport mitos but even appear to make their own ketone bodies!
https://en.wikipedia.org/wiki/Astrocyte
http://www.ncbi.nlm.nih.gov/pubmed/14769487
Looking at this another way, the smallest mitos are 0.5 um in diam while the smallest cells are ten times bigger, 4–5 um. So plenty of room for mitos to fit inside even the smallest cells. RBCs (~ 5um) ditched their mitos. But that’s likely because they didn’t need them since they are basically hemoglobin cargo vessels. RBCs even lack nuclei.
Jonathan, that brain cells have mitos only makes sense. You expect these cells to be extremely active metabolically, which requires lots of energy. Without mitochondria (and thus without a place to perform the Krebs Cycle) the only way cells can produce energy is through anaerobic fermentation, a very inefficient and low-energy-yield process.
I wanted to ask Emily about her comment. But that appears to be a non-starter. I couldn’t post my question to her blog post because she closed the comments. Her FAQ makes it clear “…my email volume is incredible, and I simply do not have the time to respond…”
Jonathan, I do question if Emily’s statement is correct. And even if these mysterious mito-less brain cells do indeed exist, how abundant can they be? If we have just a small number of them, they’d require a vanishingly small amount of glucose to power them. But again, I’m far from convinced they even exist. In my research, time and again, the only cells I read about that completely lack mitochondria are red blood cells. If you find evidence that these mito-less brain cells do indeed exist, I’d love to see it and will gladly stand corrected. –Bryan
Jonathan, thanks for sending me down a glial tendril. Found some interesting stuff that brings up more questions than answers.
Here’s an Emily Deans piece that describes more her suggestion that tendrils rely on glucose: https://www.psychologytoday.com/blog/evolutionary-psychiatry/201109/brain-energy
In it she gives a smidge more detail: “…Certain long nerve tendrils are too spindly to carry mitochondria. Those spindly bits need to run on pure glucose. Glucose becomes ATP… directly via glycolysis…”
At least we now know Emily’s talking about mito-less tendrils, not the brain cell cores the tendrils emanate from. But she gives no idea how many such “certain long nerve (glucose-dependent) tendrils” we find in a “typical” brain. What portion of the brain’s energy do these sop up?
And do these tendrils run on locally made glucose? Of the brain cells, astrocyte glial cells seem to have an exceptionally high number of very thin tendrils. Astrocytes are also the one brain cell type that produces ketones. Chris Masterjohn gave evidence of multiple pathways from acetone (a ketone body) to glucose. So did astrocytes evolve the ability to produce ketones to generate fuel for their own tendrils? Via a pathway to glucose?
I can’t find what a “spindly tendril” is composed of. Or what its energy needs are. Or where the glycolysis takes place to feed the tendril.
On another note, this link tells us brain cells are not wild for free fatty acid fuel, even though FFAs can easily cross the blood-brain barrier: http://www.ncbi.nlm.nih.gov/pmc/articles/PMC3790936/ So for brain fuel, looks like it’s mainly ketones and glucose.
Just my random findings and thoughts on the matter before I head to bed. Good night –Bryan
Anyway Jonathan, your statement:
“…In those [brain’s] places, we must use glucose itself (via glycolysis) to create ATP” – seems more plausible.”
the “seems more plausible” part may not at all relate to your symptoms and your low BGs. IF you were also cranking out plenty of ketones at the time.
Sure, glial (and/or neuronal?) cell “spindly tendrils” may indeed need glucose for their ATPs. And so? Maybe your spindly tendrils were getting all the glucose they needed from one or more of the (acetone→glucose) pathways Chris Masterjohn spells out here:
http://blog.cholesterol-and-health.com/2012/01/we-really-can-make-glucose-from-fatty.html
Pathways fed by acetones streaming from your liver and/or your astrocytes.
So, to sum up Jonathan, what caused your brain fog and other symptoms? Did they result from:
1) low BGs underfeeding your brain cells, as you suggest? Or,
2) under-glucosed faltering RBCs failing to deliver enough oxygen to your brain and to clear enough carbon dioxide from your brain? Or,
3) both? Or something else?
I couldn’t even venture a guess which scenario “seems most plausible.”
We’ve often heard the human brain is bioscience’s final frontier. Still, I’m amazed how little we know about it. –Bryan
It’s uncontested that by some mechanism hypoglycemia is less severe in the insulin-dependent if they are keto-adapted, by whatever mechanism – yet the dolts at the American Diabetes Association do not acknowledge even this observation – so IMO there’s no point in waiting for the Catholic church to look through the proverbial telescope before taking action …
Jonathan, if I listened to my Kaiser doc/ADA/mainstream, I’d be injecting insulin now. Instead of enjoying the totally med-free life I currently have.
But I’ll never forget one visit in 2007, when I put my doc on the spot about the macros I should eat. I asked him, in essence: “The higher carbs will surely kill me faster. We can eat only so much protein. That leaves dietary fat. What do you recommend?”
He looked very uncomfortable and anxiously looked around his office like the walls had ears.
He then leaned over toward me and–I kid you not–he *whispered* to me:
( “I’d eat a high-fat diet” )
The he looked around anxiously again, and quickly added:
“Make sure you come in often for your lipid panel!!”
HAHHH!!!
Hilarious, isn’t it! But such an awful human tragedy, all that pain, all those lives snuffed out …
Jonathan, to make clearer.
You assert: “There are obligate glucose-requiring cells of the nervous system and/or brain…”
To back up your assertion, you give your symptoms:
“…I’m not affected by hypoglycemia until my blood sugar has been <60mg% for a long time. Then, I notice purple patches in my visual field, I feel the cold (even if it's not very cold), my thinking slows and I'm prone to errors of judgement…"
All I’m saying: Your symptomatic evidence fails to prove your assertion that the brain has obligate glucovore cells. Why? Could be your symptoms *don't* stem from a glucose shortfall. Instead, it could be your under-glucosed RBCs fail to deliver enough O2 to your brain cells. And maybe those same underfed RBCs fail to remove enough CO2 from your brain cells.
Too little O2 and accumulating CO2 can definitely slow your thinking and cause other troubles!
Jonathan, just trying to make clear your evidence in no way proves or disproves any obligate glucovory in the brain. We aerobically respire fatty acids as well and glucose. That is to say, both energy-producing processes–originated either from fatty acids or from glucose–require sufficient oxygen to work. Perhaps a shortfall of oxygen–not glucose–helped cause your symptoms. Perhaps CO2 buildup helped cause your symptoms. We can't say for sure. But we can’t discount those possible causes. Bottom line: WE DON’T KNOW. –Bryan
Well, as some people say- (Tim Noakes, among others)- there is no such thing as “essential carbohydrates”. We need protein and we need fat, but we don’t need to eat carbohydrate, as our bodies can make them from protein, and even from fat.
And I agree, we probably don’t really know to what extent some of our cells need glucose. Some people (like Jaminet again) claim that ketogenic diets cause dry eyes, or dry mucous membranes in other tissues (like the intestine?) I’ve never noticed this at all in my case. Oh sure, I do seem to have less mucous and post nasal drip on a low carb diet (I assumed that was a good thing?) I don’t notice any problem with eyes, and my digestion is much better on low carb, so I’m assuming that’s another myth.
A propos the smell of fresh bread baking: to this day, the smell of wheat bread fills me with longing. As a celiac, I experienced bread (gluten) addiction; in people with leaky gut, the opiates in gluten can go into the bloodstream and cause something like a “high”; a.k.a. addiction. My whole wheat bread addiction was one of the main things that clued me in to the fact that I was a celiac. But even though the smell is tempting, I know that gluten makes me very, very ill, so that’s enough to stop me eating bread! I guess other people are not so “lucky”, and I can understand how it must be difficult not to give into cravings. When I first found out I was a celiac, and had to go on a gluten free diet- (I was still high carb for years, even though gluten free)- I would smell people’s bread, bagels, pizza crust, etc., just to get the vicarious pleasure!
Going low carb was relatively easy for me, in terms of cravings. Those gluten free breads and carbs taste pretty grim, so I never really missed those foods at all. Sugar was a little more tricky; however, once I stopped for a time, I’ve now come to the point that I actually dislike sugar. I’m highly sensitive to cloyingly sweet foods. Many fruits just taste too sweet for me now. Eating out in restaurants can be hard, as the food is sometimes too sweet, to suit “normal people’s” palates. I feel sometimes like I’m an anomaly in a world of sugar loving people!
Morgana, about sugar, “cloying” is a terrific word for it. Definitely you and I are still exceptions. Every once in awhile I’ll taste something that has a lot of added sugar, and it’s too much and unpleasant. To look at this another way, foods that never tasted sweet to me before now taste quite sweet, e.g. broccoli and *esp* cabbage. When I first started my VLC journey in late July 2007, I went a year without cabbage. When I finally returned to it, I couldn’t believe how sweet it tasted. I googled to see if Big Food was sugaring up cabbage like they did corn! When I was a kid (60s/70s) corn was very starchy. You had to cook it to eat it. But by the 90s, you could eat it raw off the cob and it tasted very sweet.
If there’s one thing that’s come home to me during my journey, it’s that we know *so d*mn little.* So much stubbornly remains beyond our ability to measure. Even something so seemingly basic like: How many cells actually compose us? I was like: “How can we NOT know that?!” And yet our cell-count estimates span almost *two magnitudes:*
http://phenomena.nationalgeographic.com/2013/10/23/how-many-cells-are-in-your-body/
Carl Zimmer, posted Wed 10/23/2013
“…estimates sprawled over a huge range, from 5 billion [I’m guessing CZ meant 5 trillion –B] to 200 million trillion cells…If scientists can’t count all the cells in a human body, how can they estimate it? The mean weight of a cell is 1 nanogram. For an adult man weighing 70 kilograms, simple arithmetic would lead us to conclude that that man has 70 trillion cells. On the other hand, it’s also possible to do this calculation based on the volume of cells. The mean volume of a mammal cell is estimated to be 4 billionths of a cubic centimeter…Based on an adult man’s typical volume, you might conclude that the human body contains 15 trillion cells…”
Much as I try to quantify and ferret out robust evidence, at a certain point Morgana, I had to go with my gut (haha ba dum tss) and choose *some* foodway. Of course Tim Noakes et al can’t *prove* that carbs are wholly optional calories. We have few if any direct measures. Nor can we reasonably expect to see such measures over a long term with a sufficiently large sample rate to let us say “Yes, for sure, that’s the way to go alright!” People reasonably ask: Where are the broad long-term studies for VLC-VHF? I don’t know of any.
That said Morgana, my eight + years living VLC-VHF have been exceptionally and uniformly positive. It may well be the single best thing I’ve ever done for myself. Since I embarked on VLC in 2007 at age 46, EVERYTHING improved by all observed measures I’ve done to date. Without exception. Like you noticed with lowered mucus production and still properly moist eyes, my symptoms cleared up and all else that was well stayed well. Even my springtime allergies nearly totally cleared up. I’m far from the only one who’s experienced frankly wondrous improvements. I’ve heard and read endless accounts about people who radically improved when they went grain-free VLC. Whatever their various mitigating factors may be.
Even mainstream biochem grudgingly mumbles and tilts toward inherent superiority of keto. Oxygen is a necessary evil. It’s key to aerobic respiration, which we humans have to do. But oxygen is… oxidizing! It attacks unstable fats like w3 and causes them to quickly rancidify. It helps create oxidized species like free radicals that rampage through our systems, that appear to wreak havoc and accelerate aging. Well guess what? When we respire fatty acids, kcal-to-kcal, we generate way less O–*6+x* less O–than when we respire glucose. That’s way less O that hangs around the cytosol to attack hapless cellular byfloaters. It’s easy to do the math. Glucose yields only 4 kcal/g and sports a whopping six Os per molecule. A long-chain fat (e.g 18C stearic acid) yields 9+ kcal/g and carries only two Os. Way less O means way less damage to our sensitive mitochondrial tissue and other organelles that bobble around in the cytoplasm and can stray in the path of bully oxygen which rapaciously steals electrons from anything within reach.
Morgana, If you accept the current biochem, it suggests that, at the deepest cellular level, keto lets us work BETTER. In the short term and esp in the long term.
But because we have a surprising paucity of direct empirical evidence, I have to rely on the circumstantial evidence I can find in all the relevant disciplines, which include paleoanthropology, paleoethnography, paleofornesics, organic chemistry, biochemistry, genetics, and nutrition science. I continually review anecdotal evidence, meanwhile always look at its depth, breadth and quality. I collect all the the clinical measures I can coax out of my doc. I often simply stop and ask myself: How do I feel? Even with all that evidence, I feel like pioneer forging (foraging?) into the old known/new unknown. I am my own Grand Experiment, though I meet a growing number of fellow-travelers. At this point, I have to say, I feel great and pretty great about it! To this point, even now, it astounds me that VLC it appears to have only numerous upsides and zero downsides in my regular daily life. I know of no other life change I’ve made that rewarded me with such strong and unalloyed positive results. –Bryan
Cloying is the perfect word for too much sweetness, and is the word I’ve used for decades. A couple of times, when I’ve accidentally sipped iced tea that someone “presweetened”, it’s literally made me gag. The thought of sweetened coffee is gruesome, especially if black without the cream to tone down the sugar. Needless to say, I don’t waste money on those cloying synthetic coffee drinks that are so popular. Fruit is fine usually, but some overripe types, even with no sweetener added, are awful. People think it’s weird that I can’t understand why anyone would add sugar to berries (or even grapefruit). Maybe some of us are different from the general public in the lack of a “sweet tooth”. I’ll have to research to see if there is any indication of a genetic factor. But, even as a child, I preferred dark, dark chocolate to milk chocolate, and literally gagged on things like pineapple upside down cake. The very thought of it makes my throat tighten. When my Mom would make it, I’d beg off on dessert.
annielaurie- I guess there could be a genetic component, though in my own case I highly doubt it, as I come from a family of sugar addicted people. In fact, as a child, I myself was a sugar-o-holic! I know many people say we are “hard wired” to like sugar, but I’m not sure that it’s that simple. (I agree that we are probably hard wired to like the very subtle sweetness of natural fruits and vegetables, the rest I’m not sure about…..) Basically, our taste for sweetness is cultivated. Usually babies and very young children are fed sugar and fast carbs, first thing, while weaning. Actually, it might even start in the womb- (my mother definitely ate lots of sweet foods! Especially chocolate). At one time I loved sugar so much I never imagined I could possibly give it up, but low and behold, after a few weeks on a ketogenic diet, not eating sugar, I grew to dislike the taste. (Though I still like the sweetness of vegetables and some fruits, and of course very dark chocolate; nothing below 85%). Because of my experience with sugar, I am a firm believer that the taste for sugar- (in it’s “cloying” form)- is largely cultivated- (though there may be other aspects at play here too, like genetics, possibly certain deficiencies, etc.)
wbryanh- I know what you mean about corn! I loved corn as a child, but somewhere along the line- (even before I went low carb)- I just decided I didn’t really feel like eating it anymore. It used to have a certain “nutty” taste, which it doesn’t have now. Funny enough, my brother (independently) came to the same conclusion; we talked about it years later. And I know what you mean about the sweetness of vegetables. For me, this is a huge benefit of eating low carb; all my food tastes so much better now! I hadn’t realized how much sugar dulls the taste buds. (Actually, not just sugar. Before I even gave up sugar, I stopped eating all grains, and when I did, other food tasted so much better! So I think something about eating high carb- for me, at least- affected my taste buds). I enjoy the flavors of food so much now. This is one of the things that has kept me wanting to eat low carb, and it also keeps me from wanting to cheat.
Of course, I’ve also experienced a whole slew of health benefits. Too many to mention here…..
Morgana on one level it seems self-evident that if we cut out added sugar that we’ll get more sensitized to what we still eat, that smaller amounts will taste sweet, right? But still, in the months after I went LC, my sense of taste returned so dramatically I wondered, how could that be? Finally this idea hit me: My incipient neuropathy had gone away. My nerve endings everywhere were healing–and beginning to sense more and feel more.
In late 2006/early 2007–the months preceding my T2D diag–I had tingling in my fingers and toes at night. After the diag (29 Mar 2007), I started to restrict cals and exercise like mad, meanwhile kept following the gov’t guidelines (50% carb, “wholehealthygrains,” etc). For a while my RC and all-day walks brought my BGs down from the troposphere, but then they started going up again, till they peaked of 245 on 29 Jul 2007. And this was after a 30 mile hike during which I ate nothing but a Clif Bar every 2–3 hours!
That was it. I went LC that day. That’s how I’ve been rolling ever since.
Constant keto really does seem too good to be true. I keep half expecting some bombshell to drop, that we’ve just discovered some horrible consequence of following LCHF long-term. Doesn’t everything have downsides? Yet the more I follow it and read the latest research on it, the better it looks. For me, there just don’t seem to be any trade-offs. –Bryan
I may have experienced a downside to keto – after 15 years, I got GERD from Helicobacter – fixed with two antibiotics, but then chronic diarrhea which lasted for three years, nothing made much difference – SCD, FODMAPs, food sensitivity testing, Elixa probiotics – I had Candida and high levels of a couple of commensal bacteria (“possible pathogens”) and C. diff so was treated with Nystatin, Cipro and Flagyl with little result. I read Richard Nikoley on potato starch, I’d done psyllium husks and Acacia senegal without improvement but I thought what the hell – and mirabile dictu it’s working! It’s plausible (to me at least) that my low carb diet starved out some desirable bacteria like the bifidos that make sfca’s – I tested low in 2ndary bile acids http://www.upi.com/Health_News/2016/01/06/Antibiotics-promote-C-diff-infection-by-killing-gut-bacteria/1281452107192/ which inhibit C. diff – so I’m convinced (in spite of n=1, many possible confounders, perhaps coincidence) it’s prudent to add prebiotics to the keto diet, especially potato starch since neither psyllium husks nor Acacia senegal made much of a difference …
Jonathan, I’m sorry you had to suffer all that! Ugh!
Did you ever find a proposed mechanism for how long-term keto may have led to your GERD? Besides possibly low bifidos? What I’ve read up to now, eg this:
http://chriskresser.com/more-evidence-to-support-the-theory-that-gerd-is-caused-by-bacterial-overgrowth/
links H Pylori more to carbs, in particular malabsorbed carbs in the GI which start to ferment. Which surprises me, at first glance, that potato starch seemed to clear up the problem that may involve SIBO! Btw, I had one excellent experience with PS, and then nothing after that, neither good nor bad. You can search this forum for my discussion on that.
I’d love to see a site where people doing long-term keto record their experiences and symptoms. To follow LCHF long-term is to ultimately go into the unknown, since relatively few people these days do it. For me, to this point (8.5 years) I’ve had absolutely no negative experience with it. But that’s only a little over half the years you’ve spent in keto. And it could be problems may in fact crop up even after such a long time. I ate HC for my first 46 years, but didn’t get hints of a problem till I was maybe 40. Of course, I wasn’t so focused on the matter either! I’m sure then I missed symptoms that now would look as big as barns.
I have to leave for an appt so will look at your bifido link when I get back. –Bryan
wbryanh, Jonathan Christie- First off, thanks for that Chris Kresser link….that was very interesting! I’ve read lots of his stuff, but not that one.
In any case, my own reason for going low carb in the first place was mainly to help my digestive issues- (though I did not have GERD; that was about the only thing I didn’t have, ha ha). I am a celiac, so I was already gluten free, but I seem to also have issues with fructose and high FODMAP foods in general. Going low carb helped my digestive issues immensely- (among other things), but it still wasn’t perfect. Then last Spring I decided to go on a low FODMAP diet, which I did for about 2 months, and then slowly added back the foods one at a time to see what I was sensitive to. This helped me immensely, as I discovered that even some low carb vegetables cause me problems. And, luckily, I’m not sensitive to all high FODMAP foods, so I can still eat some things like asparagus and shiitake mushrooms; I even discovered, through the diet, that I can eat some fruits- (when I originally went low carb I didn’t eat any, thinking fruits didn’t agree with me at all). I stopped eating grains completely because I notice I feel better when I don’t eat them- (apparently this is true of many celiacs). Luckily for me, the low carb diet- as well as knowing which FODMAP foods I can and can’t eat- totally cured all my digestive problems.
However, as some say, there are times in our lives when one thing works, and then it can happen that things in the body change, and we need to make little tweaks in our diets. My theory is that in this day and age, it’s particularly difficult to eat the very varied diet of our ancestors- as well as the fact that so many foods today just aren’t of the same quality as they used to be. It could be that a particular way-of-eating can work for awhile, but eventually some problems may occur, possibly due to nutrient deficiencies, or changes in gut bacteria. This is why we need to always be vigilant and continue to tweak the diet when we find something has changed. It looks like you’ve done that, Jonathan Christie, by adding in potato starch. I am also aware of the fact that if something ceases to work for me, I need to re-evaluate, and find answers. You’re right, wbryanh, that so little is known about long terms effects of ketogenic diets! (Though there seem to be plenty of people online who have done fine long term. One good example is Dr. Phinney, who looks quite healthy at his age).
Also, since we all have such different microbiomes, I’m convinced that there’s no one-size-fits-all…..just like Denise always points out! In the Chris Kresser link, he talks about stomach acid (or lack thereof) as being a major issue with GERD. I used to be mostly vegan, and I think that that diet caused low stomach acid for me. I was also unwittingly eating a lot of foods that I was intolerant to, causing yet more problems. In my own case, low carb seems to have greatly improved my stomach acid (as well as bile, another thing that was insufficient in my case). All of these digestive enzymes and hormones work together, so if one is off, it can affect all the others. I also think that for some of us, after years on a low fat diet, it can be difficult to suddenly digest high fat foods; the body isn’t used to it, so there may be malabsorption. This is my theory (one of them) as to why some people have problems on a ketogenic diet. If you can’t properly digest the food you’re eating- (my case on a vegan diet)- you won’t be able to absorb the nutrients you need and imbalances will occur.
In any case, this way-of-eating works for me now; but I am aware of the fact that if that ever changes, I need to be flexible.
Morgana, @Jonathan Christie, so much in your latests, wow. Where to start?
Please I hope you’ll bear with me as I speak generally in this post, and address your specifics in the next. When I read your posts I think again about how we live in a world of accelerating complexity–remember Toffler’s remarkably prescient book Future Shock? Our world filled with many thousands of novel substances (esp hormone disruptors like the organo-chlorides and -phosphates, eg BPAs, phthalates, PBDEs) and treatments, (eg antibiotic courses, infant formula and C-sections that deprive neonates of critical immune signatures, inside work and sunscreens that deprive us of healthy uV exposures) and behaviors (eg we face constant low-level stress as we do things ever more by the clock, we often sleep during nonstandard times, which violates circadian rhythms). All these Brave New World things that ramped up in the wake of the Second World War.
Of course we don’t pay attention to any of this when we’re young. We “feel fine” meaning we often stay clueless to subtle developing symptoms because we’re so preoccupied with family and kids and careers and our goals. Meanwhile, these chronic exposures and treatments and behaviors steadily damage us in our early decades, which leaves us, increasingly symptomatic in our middle/later years, to face the daunting task to sort out the myriad causes and effects. So much is by guess and by golly because of the enormously complex and interrelated nature in how our many thousands of bod processes work. We humans are the pinnacle of four billion years of evolution of life on Earth. The exquisite inner harmony and robustness how we are made, it embodies an almost unfathomable intelligence that accumulated over those eons. We are still in kindergarten when it comes to sorting it all out, and when I say “we” I mean even our research community that more and more of us deeply question, and rightly so. As well-meaning as they are, and/or as driven by corporate money as they are, researchers often do a terrible job sorting this stuff out, and we can’t depend on them. Consider those researchers who contributed to the nutrition advice the US started to promulgate in 1980 and which profoundly and even hopelessly lacks granularity, eg, for fats distinguishing only “saturated” and “unsaturated” and not examine the vast diffs of the fats within each of those two much-too-overly-broad categories. Increasingly, in that ancient Aristotelian balance of the Expert vs the Crowd Wisdom, I find the counterbalance of the increasingly engaged and IT-enabled Crowd to be more important than ever.
I want to acknowledge what a super tough job we have and how I admire that we try to sort out and unwind the accumulated damages we incurred in our first 35–50 years and to *understand* what makes us healthy and unhealthy. Maybe you feel I’m silly to say this seemingly self-evident thing, but I know so many people who simply give up and just accept whatever consequences come their way, to not try to sort out why their health slowly comes off the rails, which by the way I am not convinced is entirely a given as we age. Sure, even ancestrals tended to develop *some* CVD as they aged. But what tended to kill them were opportunistic infections that snuck past reduced immune systems (our thymus glands seem inexorably to shrink as we age and so lose immune signatures) and the fallout from from osteoarthritis, like after they fell and broke bones and became immobilized. Those two conditions of aging seem common among ancestrals and us modern-world people.
So what is the answer then? For me it’s, “Less is More.” All the interventions we do, from supps to elim diets to potato starch, I hope we keep in mind these are interventions, that they are temporary and we should limit their terms AMAP, that we should be working to restore our bods to their original balanced health that we are deeply designed to enjoy. I took supplements from 2007-2009, and tapered them off by that last year, as my BGs stabilized. My BGs did rise for a bit after I stopped the supps but then started getting lower and stabler again, which showed me we should be patient and take the long view when we trim out an intervention. Of course I know our health states differ, and that my chronic disease may be milder than others and so gave me less dysfunction to unravel. Still, I hope we can, AMAP, work to *reduce* inputs in our lives. Eg to eat AMAP organic/pesticide-free grass-fed locally-produced minimally-selectively-bred ancestral foods (esp no grains), use older kitchenware–glass, cast-iron, and stainless steel, to replace with hardwood floors those toxic chemical smorgasbords we call wall-to-wall carpets, reduce AMAP the body and hair products we use which are chock full of novel chemistry, regularly intermittent fast, transition to minimal-footware (even barefoot) running so we can benefit from that wonderful exercise without chronic impact on and repetitive injury to our knees and spines.
Often our best body “hacks” are the thing we *remove* from them. Perhaps the best of them of all: intermittent fasting.
Morgana, you say, “…there are times in our lives when one thing works, and then it can happen that things in the body change…” I hope that, with each condition we remediate and then immediately taper off, ultimately with each step we take to *eliminate* novel inputs, we will less and less face the prospect of “things that change in the body” because our bods become ever better to stay homeostatic and healthy and more resistant to the frayings and unravelings of aging. I hope for us to remediate as quickly as possible and then get out of the way to let our bods take care of themselves. –Bryan
I’m not so sure! Vitamin C for example – Pauling reckoned you can’t get enough from diet, your collagen will deteriorate and you’ll wrinkle – there’s a striking difference between my wife and I (who take C) and many of our contemporaries, we’re less wrinkly. I think Cs a keeper, as is magnesium which is woefully underavailable. Same with ALA and ALC, selenium and NAC … substances under-supplied in today’s food because of changes in agriculture, and much-needed because of the increase in xenobiotics. As an overarching philosophical principle it has merit, but there is a grave danger of throwing the baby out with the bath water …
Jonathan Christie- One of the reasons people may need “more” vitamin C nowadays could be that our diets have become so much higher in sugar- (by “our diets” I mean culturally speaking, not individually speaking). Sugar competes with the uptake of vitamin C in the body, so people who eat high sugar and refined flour diets are probably lacking in vitamin C. (Although foods high in carbohydrate also turn to sugar in the body, interestingly enough, natural carbohydrates in the form of fruits and vegetables are generally high in vitamin C). There does seem to be evidence that people who eat low carb require less vitamin C.
In my own case, I don’t take supplements because they make me feel awful for some reason. I tried taking magnesium awhile back, since I kept reading that we are “all probably magnesium deficient”; however, I got really bloated and felt absolutely terrible. And I took this very popular American one (the name eludes me now), the one everyone recommends and says it’s so “easy to absorb without causing symptoms”…..hmmmmm…..I think my body just doesn’t like supplements. I try getting what I need from food.
Interesting stuff! As an insulin-dependent diabetic obligate low-carber I don’t think I have a glucose vs. C uptake issue, but I do believe most every diabetic and citizen with a fasting bg>100 is likely scorbutic. I’m a believer in C because both our calcium scores are zero (as Pauling predicted) after decades of hi-C supplementation – quite unusual in a post-menopausal woman, absolutely unheard of in a 35-year 70-year-old diabetic. Magnesium sends me to the bathroom so I do Epsom sat baths. The other stuff I take doesn’t make me feel one way or the other, they’re a leap-of-faith investment in my future health but I’d drop them in a heartbeat if they made me feel bad!
Jonathan, when did you get your first calcium score? When did you go low-carb? –Bryan
diagnosed with diabetes 1 in1983, started vitamin C ~1985, CT scan ~2004 Ca=0, EBCT scan ~2011 Ca=0
Thanks Jonathan. And LC diet? Do you remember when you got going on that in earnest? –Bryan
1998, the year Dr Richard K. Bernstein published The Diabetes Solution – I was an instant convert, having failed the alternatives!
Jonathan, Dr Bernstein’s Diabetes Solution was my (first) pivotal read! I don’t agree with it all (in that edition anyway) but it was a key read for me.
Dr B’s a terrific living example of what he preaches! Still sharp as a tack even up to a month ago when he made this vid:
I laugh when I think back to the summer of 2007 when I sat in a local coffee shop blurting out “AHA!” “AHA!” as I read his book and people looked over at me. :-)))
I hope I meet him before one of us goes 🙂 –Bryan
Jonathan, here’s what I see: You started Vit C in 1985 with no idea your starting coronary calcium level. Then 13 years later, in 1998, you go low-carb. Then, six years after that, in 2004, you get your first coronary calcium test.
My question: how can you confidently attribute your low CC all to your Vitamin C supp? You had already six years of LC before your first coronary calcium scan. Maybe the low-carb diet played a big role? Maybe even the main role? You certainly gave it plenty of time to work its salubrious magic. And what about the improving quality of your food? If you’re like most of us after diag, you not only go low-carb you steadily ditch whatever SAD junk you ate and move more fully to high quality food, eg locally grown organic/pesticide-free produce, grass-fed meats, and high w3 cold-water fish like salmon that’s lower down on the trophic scale. And who knows what other changes you made since your T1D diag in 1983? You could have made near countless changes in the 21 years leading to your first coronary calcium test. How do you know which change played what role in your improving health? That’s all I’m asking. –Bryan
If you research calcium scores in diabetics, there simply aren’t any reports of zero scores in diabetic men over 60. No black swans. Add to that my wife is also 70 years of age, post-menopausal – Ca scores of zero are very rare in her demographic also. Yes we eat mostly organic and avoid sugar and grains, but any number of people do that. The only thing we have done different is we’ve taken 5 g per day of vit C for 3 decades, and it’s had the effect on us that Linus Pauling predicted, many years before he predicted it: your collagen will resist calcium infiltration i.e. atherosclerotic plaque. And it has. What are the chances? We’re genetically protected, er, by some magic never elucidated by science? I doubt that – but possibly it has to do with vit C functioning as Pauling predicted and protecting against atherosclerosis by strengthening the collagen in our arteries. Honestly, I don’t give a rat’s ass, and that said I’m not going to give up taking vit C to see if I develop a calcium score to satisfy the curiosity of the peanut gallery …
Jonathan, who suggested you should quit your Vitamin C? Right. NO-ONE.
Note I never suggested people should categorically drop their supps or any other intervention. I made this clear in my Dec 4th post to you.
Here, all I did was look at your timeline and asked how you “knew” it was your long-term Vit C therapy that was (largely? wholly?) responsible for your zero coronary calcium score. You said why you believe you should attribute this effect to Vitamin C. Fine. Thank you for your opinion.
As for how rare Ca=0 scores are in your cohorts, I couldn’t say. This study:
http://www.ncbi.nlm.nih.gov/pmc/articles/PMC515311/
says “…a 60-year-old non-smoking non-diabetic women with hypertension and high cholesterol would have a 47% chance of having a CAC score of zero…” IOW, almost *half* the women in this senior cohort get Ca=0 results. Does this Ca=0 rate slope off to near zero over the next decade of age, to your wife’s current age? I don’t know.
As for what you say “We’re genetically protected, er, by some magic never elucidated by science?” Yeah, well Jonathan, there *are* plenty of people who appear to be genetically advantaged to cardiovascular protection. I’m surprised you don’t seem to know about any of them. Here’s a recent one:
http://www.ncbi.nlm.nih.gov/pubmedhealth/behindtheheadlines/news/2015-10-22-genetic-variation-reduces-risk-of-heart-disease-in-women/
Jonathan, next time, if you will can the ‘tude, the gratuitous “rat’s-*ss” and “peanut gallery” stuff, that’d be appreciated. I’m very glad you and your wife have zero CC scores. –Bryan
The great majority of diabetics have a calcium score which goes up with age and is associated with a greatly increased heart risk http://www.medscape.com/viewarticle/503651 The ADA points out that *At least* 68% of diabetics 65 years and older die of heart disease so my CAC of zero at 70 years of age is remarkable – but not to you apparently, since 47% of women aged 60 have a CAC of zero (relevance??) and in any case would be easily explainable by genetics. Diabetics are dying left and right of heart disease, so the influence of any genetic protection is miniscule. I’ve fought long and hard to get where I am, don’t expect me to roll over for your trivialization of my rationales for my freedom from heart disease.
Well that’s just it Jonathan. You fought long and hard and made many changes. No-one’s trying to take that away from you. Really, I applaud you! I also ask: Please get over yourself!!
Jonathan, if you don’t want to keep an open mind, if you don’t want to hear challenges to you dearly held beliefs, if you’re here only to flog the wonders of supplemental Vitamin C, then fine. We don’t have to discuss the matter further and I don’t have to pay any more attention to what you have to say on it. Go ahead and believe whatever you want. No-one’s stopping you.
All I’m trying to point out, is that because you worked hard and long and made *many* changes, please don’t expect me to believe you really *know* what therapy primarily affected which of your conditions. Far as I’m concerned, based on what you told us here, you *can’t* know those things.
Case in point: You went low carb six years before your first Ca test. At a time not many people ate low-carb. How can you say *that* didn’t play a major role in your exceptionally good coronary calcium scores? You vastly reduced the inflammatory events in your bod. Reduced BGs meaning less glycation of proteins in your arterial endothelial lining, thus laying fewer seeds to grow arterial plaque. If this meant you reduced the amounts of your injected insulin, that also lowers inflammation with similar and added salubrious effects on your arterial linings.
And what about Vits D and K2? Did you increase those as well? Those fat-soluble vitamins are key to move calcium out of blood and into bone. Less blood Ca means less building material for arterial plaque.
Jonathan, maybe massive amounts of Vit C really is the wonder therapy here. Maybe it isn’t. Who truly knows? Whatever. If it fits your narrative and agenda to keep flogging it, if that’s what gives you the self-validation you seem to need, then please be my guest and we’ll just leave the matter here. I’m not here to listen to folks drone on about their pet beliefs that they can’t sufficiently support with solid evidence. Indeed who try to support them wholly or mainly on mere correlation. –Bryan
Morgana, @Jonathan Christie, I love this convo! JC, about Vitamin C and smooth skin, I think of the clear unblemished skin the ancestral Inuit have and the touted smooth skin of clear of the elderly people who live in the Japanese mountain town of Yuzurihara, and you know other factors are at play. These Inuit got a mere 15mg/day Vit C from food, and these elderly Japanese set the stage for their long healthy lives long before vitamin tabs went mainstream, plus why do they apparently fare so much better than the rest of the Japanese who surely take Vit tabs too? Again, other factors are at play, esp our chronically higher blood sugar levels as you so correctly alluded to Morgana. Glucose outcompetes its downstream metabolite Vitamin C for the GLUT channels that port these nutrients from our blood into our cells. These ancestral Inuit ate very few carbs and ran low BGs, 65 mg/dL, this lower glucose means less Vitamin C can still make it into the cells and do its wonderful collagen upkeep catalysis.
So see what I mean? This may very well illustrate the idea of pursuing *less* — in this case reduce and even remove the carbs. To let our bods make the glucose that it judges it needs. Again, glucose is vital to us. That’s why it makes sense we’ve evolved multiple ways to make it from non-carb nutrients like proteins and fats. And for you Morgana, to stop eating the SAD with all of its novel ingredient and skewed nutrient balances and bioavailabilities. You *removed* and replaced with foods your bod evolved to properly deal with.
And reduce our carbs by how much? This ties back to Masterjohn’s 2012 post showing we make glucose from fat as well as protein, and by multiple pathways. Maybe carbs *are* a truly optional nutrient. For some of us anyway. Maybe most of us?
Jonathan, you say “…there is a grave danger of throwing the baby out with the bath water…” I totally agree! The trick is to identify the “baby.” We do tremendous damage to ourselves with the SAD and our other daily environmental exposures I’ve mentioned before. So we absolutely need to take interventions. Another trick is to know when to get out of our bods’ way as they correct themselves.
Btw, I don’t discount the possibility that we can take interventions to extend our healthy lives beyond what we would normally live in the ancestral environment even spared the acute events of those days (wars, sabertooth tiger attacks, etc). I’m glad people like Ray Kurzweil pioneer this and we may learn valuable things from their experiences:
http://www.vice.com/read/100-pills-a-day-to-live-to-150
It’s just that we really know so little about the enormously involved and complex interactions in our bods that we could do more damage than good, eg to take so much supps Vits C and E that we shut down our bods’ endogenous anti-ox production, the latter which give us the added bennie to increase insulin sensitivity. See here:
http://well.blogs.nytimes.com/2014/11/26/why-antioxidants-dont-belong-in-your-workout/
This is a similar idea to how the testicles can atrophy on ‘roided up athletes (please pardon the rough language in this article):
http://www.esquire.com/lifestyle/health/a4350/steroids-0408/
Again, I wonder if we are very often best off, once we correct imbalances through interventions, to reduce and remove AMAP to let our bods make the nutrients they need. To not force them to deal with nutrients level beyond what they need. –Bryan
The people of Yuzurihara are a super-interesting case to me. I do have a couple of thoughts. One is about cooking methodologies. In Yuzurihara, and in some other “healthy people” places, the common cooking method is to put things in a pot of water and boil them a little. What this does, in practice, is to save all the good stuff that leaches out with other cooking methods. It also makes sure the meat or vegies never get above 190 degrees. So if you eat a lot of tubers, cooked in water … you likely get a fair amount of Vit C. Esp, when greens are added to the water and they are fresh-picked.
The other has to do with fish. It is sort of a rule in Japan that you have a little bowl of soup with each meal. That soup is generally made with dried bonito flakes and kelp. So the “good stuff” from the bonito flakes goes into the water, and so does the “stuff” from the kelp … which gives a nice shot of iodine and taurine with every meal.
I’m not sure how the Yuzuriharans make their broths, but if they follow the traditions of much of Japan, Korea, and China, they use dried fish. In Y. they have a salmonish fish in their rivers, and I could see them saving the guts or bones or whole little fish to use for making broth.
Greens aren’t mentioned much in the writups about Y., but taro and sweet potatoes (two of their main crops) also are very good for greens.
As for the Inuit … they have a diet that is mega-high in taurine, which is also very good for your skin. Taurine also helps regulate magnesium handling … maybe one of the reasons everyone seems to have magnesium issues these days is that we have very low taurine levels.
http://www.healthcentral.com/rheumatoid-arthritis/c/798984/116673/ta/
Hey Heather, Top o’ the Year–
The Yuzuriharans, I also looked into their cooking patterns. Not just how they prep their food but what is their cookware? For example, cast-iron was (still is?) a big part of traditional Japanese cookware, which challenges the ideas here that high iron per se is necessarily bad for us. Esp if, as you suggest, they eat a lot of soups, consume all the broth nutrients which could include iron uptake from the pot. About preserving Vit C, do I read this study right, it appears that you can denature it at 30–60C but preserve it when cook at a *higher* temp band, 70–90C? Today is first time I heard of that, but here check it out:
http://www.ncbi.nlm.nih.gov/pubmed/20546391
Anyway this study seems to align with what you say, to cook at 190F.
I’ll guess the Yuzus get most of their Vit C from the greens. Fresh greens are loaded with it but their starchy tubers don’t have much:
Click to access Edition%20288_p12.pdf
“…The diet consists mainly of starchy tubers – satsumaimo, a type of sweet potato; taro, a sticky white root; konnyaku ( = konjac root = shiritaki noodles), a gelatinous root vegetable; and tamaji, a small sweet potato…”
http://ndb.nal.usda.gov/ndb/foods/show/3207 11507, Sweet potato, raw, unprepared: 2.4 mg/100g
http://ndb.nal.usda.gov/ndb/foods/show/3214 11518, Taro, raw: 4.5/mg/100g
http://nutritiondata.self.com/facts/custom/659612/2?print=true konnyaku noodles, negligible Vitamin C
The first two are for the raw tubers, so may get even less Vit C after you cook them. You’d have to eat at least 2kg (4.4lb) of them raw each day to hit the USDA’s RDI of 90mg of C per day. With the greens, they get possibly 200–250mg/day. Well over the RDI, but way below typical supp amounts. Do these oldsters all supp now? Another Q to answer.
But Heather maybe the Yuzu diet carbs are lower than many of us assume? One of those fave foods of theirs, konnyaku, has almost *no* digestible carbs. I regularly eat konnyaku in the form of shiritaki noodles. For that very near no-carb reason. It’s got a great noodle texture but doesn’t budge my BGs. So depending on the balance of these root veg/tubers.
I’d also like to learn how much fish the Yuzus eat. All that Epoch Times link says is that they eat fish, but doesn’t give how much. Could be just the dried flakes like you sugg. Or maybe it works out to several oz of fish per day. I haven’t been able to find the details on it.
What about eggs? None of the sources mention it, but the Japanese eat lots more eggs (tamago) than North Americans. And often raw or near-raw, preserving CLA and other delicate nutrients:
http://www.japantimes.co.jp/life/2014/09/16/food/raw-appeal-eggs/
Bottom line: the Yuzu diet may be much further from a vegan diet that some assume.
That EP link plus this ABC Connie Chung vid from four (or more) years ago:
discusses if hyaluronic acid (HA) might be the “miracle anti-aging ingredient.”
To listen to Connie Chung, the foods definitely have an acquired taste, to put it gently. So could also be the Yuzu diet is low on food reward, a concept Stephan Guyenet often discusses.
And of course, that ABC clip includes that the longevity could be more than diet (cue to 9:00), including exercise and low stress.
And then there’s the blend of their bucolic rural life with the big city (Tokyo) just two hours east, offering options/conveniences.
And what’s in their water anyway? 🙂 –Bryan
Cast iron can leach a fair bit of iron, but it’s hard to say how much is actually absorbed. Iron is rather odd that way. If a meal has heme iron in it, the non-organic iron is more highly absorbed. Also vegies tend to block iron. Our bodies are actually pretty good at blocking iron usually. There is something about the American diet that makes us absorb too much of it. But I’m pretty sure the Yuzus aren’t getting too much iron because they just don’t have a lot of age spots.
Age spots are lipofuscin, which is iron encapsulated in fat to sequester it from the body. If you shine an ultraviolet on your skin in a dark room, the iron deposits show up as black … they sit there and absorb UV. Probably another reason the Yuzus have nice skin. Not much lipofuscin!
Measuring iron absorption is really difficult, which is why it’s easier to just measure ferritin levels. But even ferritin levels aren’t accurate, because so much iron is sequestered in the liver and spleen, skin and brain. What I have noticed though, is that those “healthy centenarians” you see (and my grandma, who was healthy to 96) don’t tend to have many age spots, and their skin is healthy too. So the skin might be a good quick gauge of iron overload.
Thinking about the konnyaku though … I take it daily, though not the “set” version you get in noodles. If you get the “raw” version it has this nice habit of tamping down yeasts and h. pylori and other baddies, while feeding the good bacteria.
Which does make me wonder. The reason cows can manage eating a diet of mainly cellulose, is that they have these nice bacteria that eat the cellulose. The cows (and gorillas) “eat” the dead bacteria, which can be thought of as animal matter? Bacteria at minimum produce butyrate, which is the main fuel for gut cells. But what else are they producing? Vit K maybe, B vitamins. Maybe other vitamins? Other proteins?
At which points all bets are off. You can’t measure the nutrients a person *gets* from just what they *eat*. For all we know these cloistered populations have some symbiotic bacteria that just works really well for them.
For Vit C, there is the issue of how it is measured. It’s really variable depending on cooking methods etc. And there is the issue of how it is used up, which is also really variable. But I dunno either. What does seem to be the case is: whatever they are doing, works. I’m guessing they do eat a lot of greens: most of the Asian cuisines feature plenty of greens.
Eggs: I noticed that too. It’s very odd that they would NOT eat eggs. Maybe chickens don’t do well there? Eggs are very much a “whole food” and people (and rats) can survive on a “nothing but eggs” diet apparently fine.
Carbs: I don’t think their “carbs” are low at all. By simple deduction: they aren’t eating much protein or fat. All the rest is “carb”. How you define “carb” … that is a question! It’s been a big question I’ve had ever since the “low carb” movement got invented. A lot of carbs are semi-digestible, or it depends on the person. I don’t digest fructose well, so probably some bacteria I have does the honors. And probably produces “something” but I don’t know what. There’s a whole slew of “carbs” that have complicated digestion patterns. Xylitol, sorbitol for starters. Xylitol happens to be found in plums and apricots, and kills h. pylori (and others). Glucomannan … polysaccharide in konyakku and aloe, and also in yeast shells, oddly. Fructans … lots of them in sunchokes, which really do set off a lot of people’s guts (“Fartichokes”!). Cellulose … which is thought to be totally not digestible by humans (but is by some bacteria).
The thing about the Yuzus though: the writups talk about them eating a high hyalauronic-acid diet. Yams just don’t seem to have that much HA.
“Starchy vegetables are said to stimulate the production of hyaluronic acid, and may be consumed in the form of white or sweet potatoes, green peas, and carrots.”
http://www.wisegeek.com/what-are-hyaluronic-acid-sources.htm
Mostly what I read is that the best sources of HLA are things like chicken feet. Or eat high-magnesium sources so your body can produce it.
“Although there are no known herbs containing Hyaluronic acid nor specific foods that contain hyaluronic acid, some starchy root vegetables, including Satsumaimo (a type of sweet potato), Konyaku (a type of gletanious root), Satoima (a type of sticky potato), have a greater impact on stimulating the body’s natural production of HA. Like most whole fruits and vegetables, these starchy root vegetables help the body to retain moisture and assist the body in its own lubrication. ”
http://www.primev.com/hyaluronic-acid-ha/secrets-of-herbs-containing-hyaluronic-acid.aspx
So somewhere along the line, the article about the Yuzus missed that point?
heathertwist- I believe that green and black tea both block iron as well? And I’m assuming the Japanese drink quite a lot of green tea? That’s my method, and I hope it’s working…..though I haven’t checked my ferritin in awhile. (I’ll have to do that next time).
I was also under the impression that Japanese people eat a lot of duck eggs- (though maybe not in that part of Japan that you’re writing about). I don’t think they eat many chicken eggs. I wish I could get duck eggs here in North Germany; they just don’t seem to be popular here. I absolutely love duck eggs; I find them far superior to chicken eggs!
Right, both green and black tea block iron. What is interesting to me is that tea is often made in an iron pot. Now, the iron reacts with the tannins I think … the tea in an iron pot doesn’t taste at all like iron to me, but the iron does mellow the tea maybe. Our well water had dissolved iron in it and it sure tasted horrid, so I can’t imagine that the iron-tea-pot iron would be desirable. Complicated reactions!
Drinks though, esp. acidic ones, cause iron to be more absorbed. So drinking a glass of orange juice with a meal (or taking a Vit C tablet) is a good way to get too much iron in your system. Which is exactly what I WAS doing before I got iron overloaded … 😦 . 20/20 hindsight!
Tomatoes do much the same thing as Vit C. Chili though, is an iron blocker.
I drink lots of tea these days too!
Duck eggs are popular in Japan and China, but they eat plenty of chicken eggs. Ducks don’t lay as many eggs as chickens in any case. Most of the recipes seem to be for chicken eggs though. If you watch Maangchi’s videos or read some Japanese recipes or watch movies, it seems most meals call for an egg. When you send your kid to school with lunch, a common thing to do is have a bowl of rice and a whole egg, raw, for the kid to crack over the rice.
Chickens are a really interesting bird. They pretty much spread over most continents. The Polynesians brought chickens with them in their canoes, and hence to South America. Chickens loose around your house (or often, IN the house!) gets rid of the spiders and ticks etc. and fertilizes your plants, and is the world’s greatest garbage disposal.
I do like duck eggs and kept ducks at one point … I stopped because they are just plain messy. But I think both have excellent nutrition! One of the reasons store-bought chicken eggs aren’t so good is that they feed the chickens a lousy diet and they don’t get enough exercise. Mine have super-rich eggs and deep orange yolks … definitely more like a duck egg than like a store-bought egg.
It may be though that the developed eggs have more nutrition, although eating them is a bit gross to Westerners. The ones with embryos are called Balut, and the people I know who eat them swear by them for added energy. Like, if you know you are going to do an overnighter at work, you stop for Balut first.
What is interesting to me about this is that when we’ve had chickens or a goose nest on eggs, the predators left the nest alone for the whole 25 days or so that the mother was sitting. But just before the eggs were ready to hatch … the predator attacked the nest and ate all the eggs (the mother was ok). It is true that the eggs get a certain smell at that point, and I’m guessing that this signals some kind of added nutritional something.
Heather, @Morgana, I’ll quickly add I drink green tea all day long (Yamashiro uji-cha, loose-leaf) and I still have iron retention issues, though they remain (barely) within the normal range. Just to remind, there can be other issues.
BTW, I brew the tea at relatively low temp (155F/68C) and steep it for a short time (1 min for first steep, 2 min for 2nd etc). This way it supposedly preserves the polyphenols, if you believe in the reputed bennies of those phytochems. But I love it because this prep lets the tea give a wonderful floral flavor. Not at all astringent. Along with this tea’s other great features, like terrific appetite dampening. –Bryan
Hey Heather, thanks for all this. A lot to absorb (haha urm). Now that you mention, I did read that non-heme iron is harder to absorb. I tend to retain iron for whatever reason and I like to fry my Spanish eggs in a cast-iron pan. So I need to pay attention to this stuff and I give blood, too, for however much that helps. (At least it helps others!) About lipofuscin spots, those *may* be what I see in a few places on the top of my forearms and in one or two places on the back of one hands. Is there a way to tell a lipofuscin spot from a brown spot of some other etiology? Anyway, I’ll delve into this.
About konnyaku, I need to check into the diffs between the set and raw versions. I do better with the Hosoda Bros noodles (Temaki Shirataki 2P, whatever Temaki and 2P signify) than on the cheapo JFC stuff. Not entirely surprised by this.
For our gut flora, Duck had some interesting idea on this elsewhere in this forum. Including the idea that we should limit the # the species we introduce, since these species in turn foster other species, so better for us to intro a few of the right “foundation” species and let them dictate the rest of the pop. If there’s an arena we know very little about, it’s our gut flora and how they interact with each other and with our bods to supply the nutrients we need and enable the metabolic processes we need. What are there other ferment products besides SCFAs? (eg the butyrate you mentioned) I google this every now and again, and don’t get much.
On Vit C and eggs, we’re good there…On carbs, yes, I’m not suggesting they are low–they do eat starchy tubers after all. Just maybe not as high as we might assume, because the Yuzus eat konnyaku which essentially has zero active (ie enzymatically digestible) carbs. You’re right it seems they don’t eat much fat or protein, though we need to put a finer point on their fish intake, and to learn if they eat eggs after all. It could be they eat a naturally calorie-restricted diet, due in part to that seem to get remarkably little food reward. I’d love for some researchers to get in there and do actual counts: grams of fats, proteins, carbs, total cals, so we know much better what we’re talking about.
Also we need to remember the healthy oldsters, they in the their 80s, 90s, older–they were born before WWII and so confronted few novel chemicals and coped with much lower food availability. Their environment tended to be cleaner and the less developed (and wartime) Japanese econ forced them to adapt to a CR diet. For such folks who never get anywhere near metabolic syndrome, they may do as well on HCLF as LFHC since in either case it’s RC. Plus with the Yuzus, with all their (lightly cooked?) tubers and fresh raw or lightly cooked greens, they could be getting a non-trivial number of calories from fermenting fiber aka mainly non-or-minimally enzymatically digestible carbs (eg resistant starch) which yields 1–2 net kcals/g mainly as SCFAs. A “fat” diet, hah. 🙂 Anyway, I read everything I can find on our latest gut flora discoveries, esp that by Carl Zimmer whom I find writes super well on it in the NYT and other pubs.
About HLA, very interesting they get it from chicken combs. Wonder if you can find also in chicken feet, a very popular item in our local Asian supermarkets and which are great to toss into soups. About your last comment Heather: “…the article about the Yuzus missed that point?” I’ve no doubt they might have. The press so often does. I can say that as a member of that club 😦 –Bryan
Konjac
Several times you’ve referred to the lack of calories in konjac, that it isn’t digested? I’ve heard other people say that too, and being able to see the unchewed noodles (yech). That isn’t my understanding or experience though. My understanding is that konjac does get digested by the bacteria in the colon, basically feeding the butyrate-producers. Maybe it depends on what kind of bacteria one has? It would seem very odd to me that anyone would spend the time and land space to grow a tuber with zero caloric value. Growing and processing konjac is a lot of work! (I have some in my garden).
“Results of the in vitro digestion confirm that KGM and konnyaku are resistant to degradation by digestive enzymes. Gas production in fermentation vessels containing konnyaku and KGM was lower than for inulin from 8 to 24 hours. Both samples produced SCFA concentrations similar to guar gum, which favored acetate and propionate over butyrate production.”
http://www.ncbi.nlm.nih.gov/pubmed/22149628
When I buy konjac powder, it dissolves in water, making a nice thickener that is heat-stable. When that mix has another chemical added to it … pickling lime or baking powder … then it becomes the “noodle” state where it is a solid and very stable. I expect that changes the digestibility? I dunno, but the powder form seems to work better for me. The “raw” form sticks to the gut, and since I appear to get issues with ulcers, it would probably coat the ulcer and help heal it? Also it’s more sticky and makes fructose digest more slowly?
I don’t know what form the Yuzus eat konjac in though. If they just dig up the root and cook it … it’s the raw form I think, not the noodle form.
High-Fat Gorillas
LOL! And an excellent point. I wonder what would happen if you tested the colon contents of the Yuzus. Or the Inuits. I do believe that some folks that are eating huge amounts of fat aren’t actually digesting all of it … fat is one of the few items one can eat that the body can decide to just not process. Some of the undigested fat probably produces butyrate? Sugars though, if unabsorbed, tend to produce dysbiosis which is an issue.
Iron
I tend to absorb too much too. Plus I was snarfing down molasses beer and beef in most meals AND our well water was full of iron. But my aunt had the same issue, so probably it’s genetic. Donating blood is an excellent solution I think. IP6 works rather well too. Tea should work to prevent absorption during a meal, but I don’t know if it affects blood levels.
Ferritin levels are really important in diabetes. There is pretty good evidence that iron might be a major player in causing diabetes. Sure, the older folks may have gotten less food, but a really important thing is that they were not raised on high-iron foods. Most kids got stuff like oatmeal and eggs and milk for breakfast. Bread and cheese and milk for lunch. Maybe one chicken a week, or a pot roast if you had money. Food was largely starches and vegies, and the starches weren’t fortified. Milk, eggs, and beans were the main protein sources. “meat” was largely in the form of sausage or bacon … no fridges. So overall, people had low iron levels.
If you can get hold of a good UV light, shine it on your face and hands while you are in a dark room. The iron deposits show up in black. “Age spots” will be some of them, but a lot of them have no pigment.
Bacterial species
I guess I don’t worry about it much. I figure the mix varies depending on what you are currently eating. I work in the garden a fair bit, so I get dirt bacteria, plus I’m with the chickens. I do take Sacch. Boulardii when I have to take antibiotics though. That is a yeast, not a bacteria, and it’s amazing for handling candida.
It is interesting though. The Japanese seem to have a bacteria for digesting seaweed. Maybe the Yuzus have a bacteria for digesting konjac!
http://www.wired.com/2010/04/sushi-guts/
“The gene that codes for the enzyme has been found in one other place: the genome of Bacteroides plebeius, a microbe found in human intestines. However, not all B. plebeius strains produce the algae-crunching enzyme. It has only been found in Japanese people.”
Calorie Restriction
Since forever we’ve been hearing about how the main issue is that our predecessors … or the “other country” people … are healthier because they are on CR most of the time. I kind of think that is hogwash. Lately there have been actual studies, pairing Chinese businessmen with their American counterparts, for activity levels. The Chinese ate MORE calories. The book “What I Eat” does an even better job, with pictures! The calorie levels and the exercise levels and the fat levels just sooooo do not fit.
I keep looking for patterns, and I have found a couple.
HLA
Most of the sources are the “gooey” pieces, like yes, chicken combs! And yes, chicken feet! Also skin, collagen. I can’t get a good fix on whether tubers actually CONTAIN HLA or if they just promote the body producing it. If “starches” in general stimulate the body to produce HLA, then your rice-eaters in general would have higher levels of HLA.
However, there are also interesting things about antibodies that destroy connective tissue. Turns out that fish oil blocks them? And why are their antibodies eating our connective tissue anyway?
“When the cartilage breakdown due to age it is called osteoarthritis. At times, the immune system of the body can attack its own tissues. This immune attack an affect the synovium or the fluid which provides lubrication and nourishment to the joints. Inflammation is one of the body’s natural reactions to any kind of injury caused to the tissues”
http://www.naturalarthritistreatments.net/arthritis-in-general/fish-oil-for-arthritis
So your Yuzus may make more connective tissue … or, they just don’t destroy it so much. Same with Taurine. Maybe some people eat more of it. Maybe some people don’t use it up so fast.
heathertwist, wbryanh- what ferittin level is considered too high? I’ve seen conflicting opinions. The last 2 times I tested, I was in the “normal” range (by conventional standards) but some Paleo advocates seem to think the higher end of those ranges are too high. So I’m quite confused about that. Also, is it difficult to donate blood- (do you feel faint, or sick afterwards?)
heathertwist- that was very interesting about the Chinese eating more calories. I’ve read that many groups of people, including people from bygone eras, ate more calories than typical Americans do now. I don’t think our problems are so much the amount of calories eaten, rather the composition of the diet.
Diabetes & Ferritin
IIRC the risk for diabetes goes up after a ferritin level of 116 or something. Which is far lower than the cutoff for “high iron levels”. Oddly enough the association has been known for years, but no one ever seems to talk about it.
http://aje.oxfordjournals.org/content/165/9/1047.full
Full study too. So that is from 2006!
Bloodletting
I started donating blood originally because I was afraid of needles. Seriously, if you want to get over being afraid of needles, this is the way to do it! The Dr office is already scary and you are afraid of having whatever XYZ you have, plus the nurse might not be good at finding a vein. But at a donation center, they are REALLY GOOD at finding veins and treat you nicely! My only gripe is there aren’t many GF snacks. Bring your own snack, I recommend. The OJ and coffee is good though.
Donating CAN make you dizzy, so you need to sit down after and drink some liquids. The only time I had problems though was when I walked around a lot after in 90 degree heat.
Bloodletting is known to help diabetes:
http://diabetes.diabetesjournals.org/content/51/4/1000.full
Again, the docs never seem to bother telling people! Bloodletting is very safe. The donation centers always test your blood first, to make sure you aren’t anemic. They also test the blood you donated for stuff like STDs and hepatitis … which appeals to the geek in me. You lose a fair number of calories too (650?).
As they say: “Donate blood. The life you save may be your own.”
IP6
If you can’t donate blood (there are lots of exclusion criteria) then taking IP6 is said to work too.
Amount of food per day
Interestingly, on the Lewis and Clark expedition, the meat ration per man was 9 lbs of meat per day. So if there is an average of 1000 calories per lb, that is like 9000 calories a day! And that’s just the MEAT part. Granted they were working pretty hard, although a lot of the time they were also just sitting around camp. But your average athlete today works out pretty hard too. OTOH, in the book “What I eat”, one of the lowest calorie counts was a gymnast, who spent hours each day balanced on one hand.
Good MornEve Heather and @Morgana:
Heather, you’re right, konjac does yield some calories. I’ve been using a strict def of “digestion”–mainly following that convention of my research materials–to include only those calories we digest with our enzymes and which go system-wide in our bods. I.e. all that “-ase” stuff we do in our duodena and others place in our small intestines. This, as opposed to the calories we get when our colons’ gut flora ferment fiber carbs. Those SCFAs we get from that, I understood to now they feed our colons’ endothelial cells but who knows–maybe we discover they too go systemic. If the Silverbacks get up to half their kcals from hindgut fermentation, you’d think at least some of that goes systemic.
But yes to your point, konjac does yield energy. Maybe we need a term to collectively refer to both processes? Eg “digestiferment?” The yield from ferments appears to be 1–2kcal/g of fermentable fiber. Of course that’d vary by which fiber you eat. Again, another area we have so little info.
Heather. what you say here: “ …fat is one of the few items one can eat that the body can decide to just not process..” YES. That is a huge point! 4–5 years ago I found sources that discuss this very thing and have been trying to find them since to post here for us.
I recall that to import fat is an expensive process. Lipases first have to split the TAGs into FFAs, then the GI has to decide which FFAs get remade into TAGs to bundle onto large chylomicrons then import into our systems for the long and winding trip through our lymph before they even get to blood. Thus our GIs–which btw have millions of neurons for rich info exchange–evolved ways to vet dietary fats in the duodenum, to communicate with the system (via vagus nerve, maybe others) for the bod’s fat needs. Furthermore, high carb levels can invoke enzymes that can hobble this fat-vet process. Evidently in the presence of high carb, we import more dietary fat than we would without the carbs. It’s fascinating stuff and I am trying to find it for us. All this helps explain the idea that “carbs make us fat, but dietary fat makes us thin.”
On iron, here’s what Kaiser sets for ranges:
Total Iron Binding Capacity (TIBC), Total: 236-404 ug/dL
Iron: 41-196 ug/dL
TIBC, Unsaturated (UIBC): 100-315 ug/dL
Transferrin % Saturation: 15–60%
I need to look deeper into this as you and Duck and others made many good points how we may well be overexposed to iron on its heme forms and in novel formulations. One thing we know, iron can feed bacteria. People who survive plagues in the bad old days, they often had anemia and so too little iron to feed the bacteria. Thanks for the uV light idea, I’ll definitely try it.
On calorie restriction, I definitely don’t think it’s “hogwash!” But let’s be clear on terms. I include subsistence diets as “CR” diets, because even in the pre-SAD days, people often seemed to want to eat somewhat more than just what they needed for subsistence. CR is apparently enshrined in some philosophical practices, eg.
https://en.wikipedia.org/wiki/Hara_hachi_bun_me
to eat until you are “80% full.” But in earlier days one often didn’t even need to follow a teaching–life forced it on them. If we go back even a few generations, more people did more physical work and food cost more. Even my American grandparents who worked on farms and did a lot of physical labor, they got enough to eat to match the calories burned, but they didn’t overeat. Even when I first started paying attention to my Dad’s parents’ eating habits when they in their early-mid 60s, it struck me how small the meals they ate. I’m not surprised the Chinese businessmen eat a lot, and I don’t think it’s necessarily healthy. China’s entered a period of unparalleled prosperity and we see the excesses and indulgences that go along with that and obesity there is increasing fast. You can already find “fat farms” in China for their little obese “emperors” and “empresses.”
http://www.reuters.com/article/us-china-obesity-idUSTRE77P4N420110826
Fat camp shows China battling the bulge
About HLA, connective tissue, and immune attacks on it (my step-Mom has terrible rheumatoid arthritis.) all very interesting. So many rabbit holes to dive into! We are still so very near the beginning of our knowledge of these things.
Morgana, maybe there are more fun things to do that the process of giving blood, but the people who collect it, they are always so nice and grateful and do everything they can to make you comfortable.The needle is a little bigger that what you see at the blood draw lab, but I feel a small pinch and that’s it. The actual donation typically takes ~15 mins. You can read, listen to whatever’s on your pocket device, yak with your fellow donators. If you feel faint–and it’s usu psychological, not from actual blood drawdown which is surprisingly little–just tell them and they will monitor you and stop the donation if needed. At the end I always feel fine and great for doing the good deed! –Bryan
wbryanh, heathertwist- thanks for the information about blood donating! Last time I checked, my ferritin level was somewhere in the 70’s. (Can’t remember the exact number). According to some people this is okay, but others claim it’s too high. I was given iron tablets when in the hospital about 6 years ago; I hated taking them, but they basically forced me to. Since then, I’ve read that synthetic iron in the form of supplements is the worst kind, and can hang around in the tissues- (sort of like what Duck Dodgers was talking about). So sometimes I think it may be a good idea to donate. In addition to that, when I was very ill, at one point I needed a blood transfusion myself, so sometimes I think it may be good for me to “give back” to the Universe. I do worry a bit though, since I am underweight (don’t know if that makes a difference?) and have low blood pressure- (which makes me worry about being prone to faintness. Though since I’ve gone low carb, I have far fewer episodes of faintness and dizziness, so maybe it’s nothing to worry about). When they test your blood before you donate, can you get a copy of the results? It might be good for me to see how everything is doing. Since my illness, I’ve been kind of avoiding doctors as much as I can, so I haven’t checked my blood markers in awhile. Is high cholesterol an issue? (I.e., can you still donate blood if you have high cholesterol, and do they even check it?)
Another thing: not only does “bloodletting” help diabetes, but I’ve also read that high iron levels can be an issue with heart disease, and possibly even cancer.
In the study I linked to, it mentioned “High ferritin diabetes”. You really don’t seem to fit that category. Donating blood is, I think, a very good thing … but you might want to wait until you aren’t underweight? Having had undiagnosed celiac for some time (as I think you mentioned earlier?) it’s unlikely you have way too much iron. Celiac involves internal bleeding much of the time, and the inability to absorb food. Getting your OWN nutrient status up is the important thing in that case.
Celiac can also damage the pancreas, according to one endocrinologist that was at a conference I went to. In which case again, the only cure is to get generally healthier?
heathertwist- I had undiagnosed celiac disease for much of my life, yes; however, I have been gluten free for about 11 years now, which is a long time. (I was anemic off and on when I was a child, and I had to take iron tablets). Then when I was in the hospital about 6 years ago, I was given iron tablets for about 6 weeks; which I hated, they gave me digestive problems. At some point after my recovery, I switched to a low carb, Paleo style diet, which means I was suddenly eating red meat- (I had been pretty much vegan before. When I discovered it wasn’t the perfectly healthy diet it was cracked up to be, I started eating meat again). At one point, a few years after I got out of the hospital, when I had my ferritin tested it was all the way up to 100! My doctor felt this was normal, but I had read that that was a little high. After that I started drinking more green tea, and eating red meat and liver in the morning (with tea), and fish or poultry or cheese with dinner (with wine. I’ve read that wine actually aids absorption of iron). Next time I tested it was around 85- (I was wrong in my last post, it wasn’t in the 70’s, but in the 80’s). I hope that’s okay.
As for my weight, I don’t think I can bring it up; I keep trying, but I just stay skinny for some reason. It couldn’t have anything to do with celiac disease anymore, I don’t think. My job requires constant exercise, however. So I might just be like one of those skinny railway workers you write about! Oh, interestingly enough, what kept my weight up and made me “look healthier” was sugar. I stopped eating sugar years ago, and though I feel healthier- I’m sure it is better, in the long run- I look very skinny. It’s a shame; I think I looked better before.
I also have no idea what my blood nutrient status is, as I haven’t tested in awhile. I feel pretty healthy though. Maybe I’ll just wait until my next doctor’s appointment (around late Spring), then check my ferritin level again and decide if I should give blood.
Well, if you give blood and feel ok, then it’s probably ok. You are right: some people are just naturally skinny. Blood cells get replaced regularly anyway, and the blood center will test you for anemia before donating.
The issue with “weight” is an interesting one. I mean, your “weight” consists of your bones and organs, muscles, fat, and water. If you “gain weight” from sugar it’s likely mostly fat and water … which may look nice on a woman (and women need a bit more body fat anyway, to be fertile at least). But as for muscle … unless you have muscle wasting, there isn’t really a guarantee that “more muscle” makes you stronger or anything else. Those railway workers, some of them, were rather skinny by modern standards. Bruce Lee too … he was ripped, but he didn’t have those huge muscles the action heros have these days.
Calories from the colon
Yes. What ruminants do is amazing … but it probably evolved from a lesser version of the same thing? And yeah, bacteria are the Swiss Army Knife of gut adaptation! We do know that the Japanese have their own species of bacteria for digesting seaweed. There is also a bacteria for digesting oxalates, which prevents kidney stones in people who eat lots of high-oxalate foods. We’ve “trained” bacteria to produce all kinds of stuff these days in the lab.
The article mentioned 6%-10%, but also mentioned the amount might be higher in people who ate more fiber. And I’m guessing it depends on the type of fiber. Most people these days don’t get a lot of the “gooey” semi-solid fibers, but there are scads of those in the Yuzu diet! I don’t know if you’ve tried eating those yams, but wow, they are GOOEY. If they didn’t get digested, then your poop would be one big mass of goop, I think. When I eat psyllium, it increases my stool size by quite a bit … I don’t think it gets digested much. But the konjac (gooey style) doesn’t do that at all.
Anyway, we know humans can turn carbs into fat. So if the super-low-fat people are eating carbs, they aren’t spending taurine on digesting fat, and are producing their own fat and proteins from the digesting food. Given that humans have some ability to produce taurine (which is probably genetically determined, plus how much sulfur is available in the diet) then the person should be nicely healthy on a diet of yams (esp. yams grown in volcanic soil).
Goo and yeasts
Another important thing about the “goo” might be that it doesn’t feed yeasts. In fact it tamps them down, esp. konjac. That is another thing that has been mentioned in this conversation … glucose-based starches that have been gelatinized, digest slowly (the “resistant starch” idea). This is really important for farm ruminants, because the yeast and acidophilus overgrowth will kill the animal if they eat too much grain. Turning the grain into something like spaghetti will allow say, a racehorse, to eat more oats without getting ill.
You can test this by putting various types of starch in a jar, then adding some water and yeast. If you do that with sugar, you get instant overgrowth. If you do it with flour, same thing. Do it with rice … yeast will grow, but slowly.
Body Fat and Calorie Restriction
Well, in your family perhaps you ran around a lot, but that sure wasn’t the case in ours. Anyway, it HAS been studied a fair bit and the link between exercise and fat is tenuous. You have some nice fat athletes — Babe Ruth comes to mind. And the farmers around here, a lot of them are quite obese. But hardly couch potatoes. Farming is hard! Look at the Sumo wrestlers in What I Eat. They work out for hours a day! Yes, they eat a lot and gain weight on purpose, but they regard the choice of foods to be a big part of their ability to gain weight. Sumos on the traditional Japanese diet don’t get so fat. They would be more like the railroad workers … eating lots of calories and using lots of calories and staying skinny.
Also, yes, the folks in our grandparents and great-grandparents age were even skinnier. More like the Japanese: short and thin. But why would we assume they were starving? The guys building the railroad certainly weren’t, and not all of them were heavy laborers. The menus of the time were written out, including the allotment for slaves and servants. In an upper-class household, at any rate, everyone had plenty to eat. Even the pampered ladies who didn’t go outside without their parasols and considered breaking a sweat to be very low class. Some of them got a little chunky … most didn’t get obese. With a few exceptions that are worth noting, like Henry 8 and Queen Victoria.
So you have examples of people eating high-calorie high-exercise diets … railway workers, Lewis and Clark soldiers (9 lbs of meat a day!) and staying skinny. We also have examples of high-exercise people that get fat (Henry 8, some farmers, Babe Ruth, sumos, other wrestlers and weight lifters). My take is that there is a trigger for “storing fat” … probably triggering a gene for hibernation. Or a bacteria!
Hi Morgana and @heathertwist. I’m fighting a very rare cold here so been a little out the pic. But still checking in and reading your posts.
Morgana, about the blood donation info, you’re welcome! About getting your blood tested, this likely varies from one country, even one district, to the next. You should check locally where you live. You can also tell them about your weight and BP levels and see if they have concerns. In my experience, the people who assist in your blood donation really want you to have the best experience possible and take very good care of you. Just express your concerns and they will monitor you. If you feel faint, they’ll let you stay on the recliner until you feel better and help you to slowly get up in case you feel any hypotension.
For ferritin levels here’s from the Mayo Clinic:
http://www.mayoclinic.org/tests-procedures/ferritin-test/basics/results/prc-20014449
As far as iron–well you know my wariness on supps! Women lose a bit of iron through their menstrual periods, though I’ve never seen this quantified. I’m sure that loss varies, but it’s hard to imagine in most cases they can’t make it up through dietary iron. As has been discussed here a lot, the problem’s usu too much iron, esp in “fortified” foods. –Bryan
@Morgana, @WBryanH: On the supps: What I’ve read is that people need about 1mg of iron a day. I.e. not much! Unless they are losing blood. Women lose a little normally. People with parasites or internal bleeding can lose a lot!
Ray Peat has a very good article on the subject:
http://raypeat.com/articles/articles/iron-dangers.shtml
“Q: Don’t you need iron supplements if you are anemic?
In general, no.
Many doctors think of anemia as necessarily indicating an iron deficiency, but that isn’t correct. 100 years ago, it was customary to prescribe arsenic for anemia, and it worked to stimulate the formation of more red blood cells. The fact that arsenic, or iron, or other toxic material stimulates the formation of red blood cells doesn’t indicate a “deficiency” of the toxin, but simply indicates that the body responds to a variety of harmful factors by speeding its production of blood cells. Even radiation can have this kind of stimulating effect, because growth is a natural reaction to injury. Between 1920 and 1950, it was common to think of “nutritional growth factors” as being the same as vitamins, but since then it has become common to use known toxins to stimulate the growth of farm animals, and as a result, it has been more difficult to define the essential nutrients. The optimal nutritional intake is now more often considered in terms of resistance to disease, longevity or rate of aging, and even mental ability.”
Calories from the colon
Yes, we are just beginning to understand all this! It does seem that when people are starving, they have a lot less excess calories in their poop. We normally waste a lot of calories. Since a lot of that bulk is just dead bacteria … one would think that over the years of starvation there would be a mechanism to extract more calories from the bacterial mix?
Anyway, it looks like there is some research on it:
“SCFAs absorbed in the colon contribute 6%–10% of the entire energy requirements in humans, and their contribution likely increases in humans who ingest more dietary fiber.”
http://www.ncbi.nlm.nih.gov/pmc/articles/PMC3601187/
The Japanese have species of bacteria that digest seaweed … likely they are good at digesting konjac too. But bacteria also produce vitamins, and probably some amino acids too? Your gut CAN absorb all kinds of stuff, which is kind of the point of suppositories.
Interestingly one of the SCFAs that is produced is acetate … aka the stuff in vinegar. Acetate has interesting effects in people, including help regulate blood sugar and causing fat loss.
Fat and starvation
The reason I don’t buy the “everyone was starving” logic that is common these days, is partly because of the 60’s. Back in the day, we weren’t starving. In fact Mom kept bowls of candy out all the time, for snacking. She made huge meals, and we’d raid the fridge as needed. Also we had cases of soda pop in the closet. But she … and everyone else I knew … was thin. There was exactly one “fat kid” in school, who was of course teased a lot. It is true portions were smaller sometimes, but no one I knew restricted themselves on purpose. We ate til we were full. We lazed around reading comic books mostly.
Then suddenly in the ’70s, everyone got fat. And fatter and fatter. Even while we work harder and harder at getting healthy. This is not because we suddenly changed or got richer. “Something” changed, yes. I don’t think anyone knows what it is though. Lots of guesses, but none seem to hold up in court.
Also, body builders. A lot of them eat a high-calorie diet. They work out some, yes. But their point is that if you eat only specific foods, the fact you are eating a lot of calories doesn’t count. We did this at work once. We lost an average of 35 lbs each. We DID track calories, but it wasn’t a low amount of calories. We quit because it got boring I guess. But it worked like a charm.
For a given person though, eating the same usual foods, eating less of the food can cause weight loss, sure. Most people doing CR eat more or less the same foods they ate before, just less of them.
The Chinese and Japanese though, are jumping from their traditional foods to Western foods, and they quickly get ill. I’ve seen the differences in the Asian stores … the Western influence is all over the place, even in the traditional foods. More weird oils, more dry packaged foods (chips!), more beef (beef was scarce for most of history).
Part of the deal on Western foods though, is that they *make* you eat more. I mean, that is the point, isn’t it? The more you eat, the more money I make selling you the food. Traditional food was made to be filling, because well, you want to be thrifty. So I design my chips such that you can eat a whole bag easily and crave more. While the traditional noodle soup … you’d eat one bowl and be full. Try eating 5 hard-boiled eggs, vs. one slice of pizza (more or less same amount of calories).
Iron and bacteria
Yes, iron feeds lots of bacteria. Usually not the ones we want. The cells in the gut absorb some iron and sequester it. Then release it into the blood if needed. Unless that process gets sidestepped, which seems to be what is going on recently.
Babies aren’t supposed to get much iron, and their guts are designed to let mama milk almost directly into the blood. But when you add iron to the formula, the babies get adult bacteria growing there instead of baby bacteria, which is probably not a good thing.
Like I’ve said before, I think part of the deal with the Rice Diet was that it was very low iron. Also low salt. So that likely had a huge effect on sugar handling and kidney function.
“SCFAs absorbed in the colon contribute 6%–10% of the entire energy requirements in humans…”
Heather, I didn’t realize it was normally as high as that. I’d done the calcs on it during my high-fiber days, chowing up to 100–120g fiber per day. If we assume *all* of that ferments and yields 1–2kcal/g, then the range is 100–240 kcals. That top end does come to 10% of the diet, but most people eat less fiber. If you take the 2002 US RDI for it:
http://www8.nationalacademies.org/onpinews/newsitem.aspx?RecordID=10490
38g for men, then the max ferment range comes to 38–76 kcals, a few percent of the daily energy. And again we can’t ferment all fiber. Anyway I need to look closer at the math in that NCBI link you posted.
I wonder if a person can slowly ramp up her fiber to give her hindgut time to adjust, how high could she get it? What percent of total kcals? 20%? 30%?
About what our microbiota can do, wow, we just scratch the surface. Our environments constantly change, so our little bugs must too. Remember how shocked geneticists were to discover human DNA contained only 30,000 genes? They’d assumed up to 10x that much. But makes sense when you think on it. We let the microbiota take care of so much. Our repro cycles (and so our mutation/natural selection cycles) are so long (~25y), our bods proper can’t keep up with the constantly shifting demands without storing a whopping load of DNA, and then you get management probs. Instead why not let our little bugs manage AMAP? Some of them have almost as many genes as we do! And we can “hire” and “fire” them at will, depending on the changing demands our environments pose. Heather what you say: “But bacteria also produce vitamins, and probably some amino acids too?” Here’s a link that talks about the AA production side:
http://www.ncbi.nlm.nih.gov/pmc/articles/PMC3144392/
“…emerging evidence indicates that gut microbes can impact nitrogen balance by de novo synthesis of amino acids and intestinal urea recycling. These contributions are most pronounced in ruminant animals that, amazingly, can live on a protein-free diet because their microbiota is capable of synthesizing most or all amino acids required for survival.”
That last sentence intrigues me because even plants have AAs, so never though ruminants lived on a “protein-free” diet esp since they graze all day and eat lots. So need to look into this more.
About poop, when I fast, I go from daily to as long as almost a week between movements. Yet it’s always fine, no constipation, usu not much volume. To me, that lends weight to the idea we continue to extract nutrients from our colon contents when our bods need it. Again our GI has a whopping load of neurons, often called the “second brain:”
http://www.scientificamerican.com/article/gut-feelings-the-second-brain-in-our-gastrointestinal-systems-excerpt/
And Richard Wrangham in “Catching Fire” spells out his zero-sum gain theory of neurons in our bods, that we grew bigger brains due to the GI shifting neurons to them because we made the GI’s job easier by starting to cook food! Not sure that’s true, but who knows? Also not sure the colon is as neuron-rich as the small intestine. But still. We have evidence that our GIs are enormously and nimbly responsive to emerging conditions.
On acetic acid, that’s the smallest fatty acid, only two Cs on the backbone. Funny that’s what’s in our bottles of Bragg’s! I’ve heard lots of things about vinegar’s healthful effects and I use it every day. I’ve vaguely wondered if any AA goes extra-efficiently into Krebs Cycle since it’s almost already an acetyl from the get-go.
Body Fat and Calorie Restriction
I grew up in the same years as you Heather, and it’s true few of us kids were overweight then, and we already had plenty to eat. We tended to be out and running around, often not wanting to interrupt what we were doing to come to table. I do think we stayed thin in large part because our food was not nearly as engineered then, it didn’t as much press our buttons to “crave” it. Even so, I remember seeing lots of middle-aged folks with growing middles. When I look at my grandparents photos, I don’t see many overweight folks of *any* age. All of them were young during the Depression which indelibly impacted them. I saw them count pennies for everything including food, even though they didn’t have to. They didn’t starve, but for much of their early lives they really did have to pay attention to food costs. When I stayed with them, they always admonished me, they told me “not to bolt my food.” Later I wondered if slowly chewing their food was a way for them to extract more energy from what we might think was a limited amount of food.
And yes like you say, as we rolled into the 70s and 80s, more and younger people got fat. This may be due to a confluence of many factors. Under Nixon, Earl Butz blew away lots of New Deal Ag progs in the name of agri super efficiency, and food costs did drop a lot because of it. Michael Pollan talks about this a lot in Real Food. We started to include HFCS in food in 1975. McGovern et al out out the govt’s disastrous nutrition recommendations in 1987–1980. The chem companies steadily cranked out thousands more new hormone-disrupting chems in that time. PBDE-based flame retardant started to show up in furniture. The list goes on.The main point: accelerating tech since WWII led to a blizzard of changes, many of them we now learn are bad for our metabolisms. And absolutely, the new food is not by accident. It’s like you say, the food industry designs it to press all our evolutionary hot-buttons and buy more of it. Again Pollan writes very well about this, either in Real Food or Omnivore’s Dilemma. –Bryan
Heather, thinking more on the idea that a high-fiber diet is a high-fat diet (due to SCFA ferment products). Several years ago, I broke down the diet of Mountain Gorillas, who eat 40–50 pounds of roughage every day. These gorillas have big hindguts (they look like beer bellies) so they can handle all that fermentation. Anyway, I calc’ed (plus got supporting evidence from somewhere?) that these gorillas got up to their cals from these SCFAs. Thus they “eat” a 50% fat diet–like some or many of the Yupik-Inuit! Hah! –Bryan
“This ties back to Masterjohn’s 2012 post showing we make glucose from fat …” If this pathway produced copious amounts of glucose, I would never have had an insulin reaction – it’s clearly bottlenecked, perhaps to the point of irrelevance. Gluconeogenesis is also too slow to prevent insulin reactions. In healthy starving humans, muscle is lost as well as fat, so it may not be of much help there either.
Dr. Alex Zhavoronkov’s experiment isn’t very likely to bear fruit (or kill him) in time to give us much guidance.
“Dr. Goran would advise “against the use of high-dosages of concentrated antioxidant supplements” however my experience on 5 g of C and 400 mg of Unique E was that I put on muscle easily at the gym, if anything easier than my first go-around at the gym when I got injured quite frequently – so my n=1 experience is that the vitamins protected me from injury and did not prevent me from gaining muscle.
IMO, there’s a scary lot of bollocks out there amongst the good advice, many of them tiny no doubt. I think we all throw the dice with whatever dietary strategy we choose as soon as we realize we’re digging our graves with our teeth, but so long as we achieve a low insulin level we’ll probably have a long healthspan:
“The fact that an age-related clinical event developed in approximately 1 out of 3 healthy individuals in the upper tertile of insulin resistance at baseline, followed for an average of 6 yr, whereas no clinical events were observed in the most insulin-sensitive tertile, should serve as a strong stimulus to further efforts to define the role of insulin resistance in the genesis of age-related diseases” http://www.ncbi.nlm.nih.gov/pubmed/11502781
First Jonathan, I have to agree about insulin resistance and add to that chronically high blood insulin levels. These high levels may bring as much, maybe more, pathology as high BGs. For example, the enzyme (insulin-degrading enzyme or IDE) that dismantles insulin after it spends an average of 71 minutes in our blood, that enzyme also appears to play a role to break down beta-amyloid deposits in the brain. Those which otherwise accumulate and set the stage for Alzheimer’s Disease:
http://www.ncbi.nlm.nih.gov/pmc/articles/PMC1559921/
If we suffer chronically high insulin levels, we may fail to keep up with breaking down the beta-amyloid because IDEs are always preoccupied breaking down insulin.
We really should be testing blood insulin levels and IRs so can often catch metabolic syndrome at an early point where we can meaningfully reverse it. Too bad the euglycemic clamp takes so much time, costs so much, and takes so much labor. For blood insulin the C-Peptide proxy marker is better than nothing. But not sure how much we can rely on it.
About what you say here: “…If this pathway produced copious amounts of glucose, I would never have had an insulin reaction – it’s clearly bottlenecked, perhaps to the point of irrelevance…”
Actually Jonathan it appears not to work that way. Our bods (except the pancreas) see insulin, not BGs, as the metabolic switch. The pancreas senses BG levels and tells the beta cells to respond accordingly. The liver and the rest of the bod, all they see are blood insulin levels. If they see high insulin levels they assume BGs levels are *already high.* Thus they shut off all endo-pyruvate/glucose production, which includes glycogenolysis and GNG from AAs. Jonathan, remember, your bod doesn’t know the diff between endo and exo insulin. It sees only “insulin.” It thinks high insulin means high BGs.
About what you say here: “…in healthy starving humans, muscle is lost as well as fat…” this depends on the fast length, activity during the fast, and how keto-adapted you are to start with. My experience in 300+ IFs which last as long as 3-⅔ days (88 hours), I lose little to no muscle mass. During these fasts I do bursty resistance training lasting only a few minutes each session. This keeps me out of glyco, but keeps me up-regulated so that my bod conserves more AAs. I weigh myself regularly during my fasts, and lose up to two points in body fat by the end.
About Kurzweil, Zhavoronkov, etc, I’m happy to let them be the pigeons. My main point is that, while we have interrelated processes of almost uncalculable complexity, I can’t categorically say we can’t hack our way to a longer life- and health-span. I’d never do what they do. But I’m happy to sit back and watch them. Who knows? We may learn something. –Bryan
wbryanh, Jonathan Christie- First off, wbryanh, thanks for the dense, and very interesting post! I thought I’d mention that my experience has been quite different to what you’ve written though. In my own case, I’ve felt bad for as long as I can remember…..stemming from when I was a child. Such is the nature of undiagnosed celiac disease. I complained constantly of feeling sick- (but since I wasn’t visibly sick and throwing up, people attributed my problems to “stress”). I sometimes had such intense intestinal pain that I would be doubled over, and couldn’t do anything. I also had pretty bad gynecological issues as a teenager- (whether that has to do with the proximity to the intestine or some other factor- sugar?- who knows). This is not a “sob story”, I’m just making clear that the SAD was obviously very, very bad for me right from day 1. But at some point, I assumed that everyone probably felt as bad as I did; I thought maybe I was weak or something. Since we are raised on this diet, and as a child you don’t know any better, it’s hard to do something different, or even imagine a different reality of any kind. So I tried to remain strong and just deal with my problems.
I totally agree, wbryanh, that the USDA recommended diet is horrible for many people! It obviously made me very ill. Now that I eat a diet that would make the conventional advisers cringe (more meat, more fat, no grains, low carbohydrate) as well as- horrors!- animal fat- I feel way healthier in my 50’s than I ever have in my entire life. Not only am I pain free, but I don’t have those horrible issues dragging me down, making my body feel like a dead weight. I’m sure very few people can say that they feel better in middle age, but there you go…..I just needed to find the right diet for me. I am strongly against “one-size-fits-all” advice. I wouldn’t even think of telling people they have to eat like me, since I’m pretty sure it doesn’t work for everyone.
And what I meant by “things change in the body”: I was talking about how our needs may change at different times in our lives. As a for instance, a growing child may need a different diet from a middle aged man- (another reason why I detest one-size-fits-all advice; just look at the situation with cholesterol!) Here is another example: when I was recovering from all my devastating cancer treatments and operations (at a time when I was very ill), I didn’t have much appetite, but I had very strong desires for fresh squeezed orange juice made with blood oranges. Even though I could barely walk, I hobbled to the fresh produce market every day to buy fresh blood oranges. What would get me out of bed in the morning was the thought of this fresh orange juice, and when I finished my daily glass, I would actually feel depressed, since the moment of joy was gone. Dr. Lustig would have a cow if he heard about that, ha ha, but I’m convinced that that helped to heal me and that I really needed it at the time! (Jonathan Christie would possibly say that it was due to the high vitamin C content, which is a great healer). Now that I’m well again, the thought of fresh squeezed blood orange juice doesn’t really appeal to me. Although I like half a blood orange in a salad every now and then, the thought of a whole juice makes me a little queasy, as all that sugar doesn’t feel good in my stomach normally. But at the time, it felt great and very easy to digest. I’m convinced that it was something I needed at the time, but no longer need. I think there are many examples of these kinds of situations, and we have to be aware of the effect that food has on our body, what seems to “hit the spot”, etc. I think these things are telling us what we need, and those needs may change from time to time.
Morgana, I keep rereading CM’s post:
http://blog.cholesterol-and-health.com/2012/01/we-really-can-make-glucose-from-fatty.html
And wonder all the more why–four years later–so few people/orgs have reacted to it!
We know we have multiple pathways to convert fatty acids/triglycerides to glucose. Not just glycerol to pyruvate which we’ve known for yonks. But even the acetone → pyruvate/glucose pathways, we’ve known those for several decades.
Yet even mainstream scholastic biochem texts kept routinely misleading us–at best. And they still do!
Why is Masterjohn the ONLY guy of any authority to point this out? Why is he still the lone voice out there?? I really don’t get why the near non-response to this intriguing info.
Per this Wiki discussion, Metzler and Metzler appear even to contradict themselves on the matter:
https://en.wikipedia.org/wiki/Talk%3AGluconeogenesis#Um.3F
Scroll down to read about it in “Michaplot”’s long-ish comment.
Lehninger’s Principles of Biochemistry was my main course book way back when in my pre-med days. Amazon lists it as a top seller. The 6th ed (2013) appears to be the latest. I just ordered it. We’ll soon see what’s in there. –Bryan
“I’ve been reading this back-and-forth about the Inuit for awhile, but haven’t commented until now. A few things come to mind: first off, who exactly are *the Inuit*? Aren’t they a series of different tribes in the Arctic region? Couldn’t they conceivably be eating slightly different diets? If we monitored the glucose reaction and ketone production of 4 Americans, could we come to any conclusions about the American diet and the health of all Americans?”
I thought this was very interesting, maybe it’s been quoted here before:
Click to access 461.full.pdf
They did rather good observations and tested glucose tolerance on Inuit back in 1928. Also he talks some about the differences in diet in different parts of the North. He tested for ketones using a check for acetone in breath.
1. The Inuit had good glucose tolerance
2. They exhibited mild ketoses after 2 days of fasting.
3. They were not normally in ketosis even though eating very few carbs.
He made an interesting note that some obese white subjects didn’t exhibit ketosis after fasting — his take was that maybe some people have the ability to burn fat without using carbs (or ketones?) to do it. He commented that the ability to do this varies in all humans … children normally require more carbs to burn fat than adults do.
“In relation to the problem of accounting for the slightness of the
ketosis found in the Eskimo subjects, it is therefore apparent that
they, like the obese subjects referred to above, require less carbohydrate
to burn their fat than normal white subjects. Children
on the other hand, as shown by Wilson et al. (S) require a larger
proportion of carbohydrate to permit the complete combustion of
fat. All these data are consistent with the hypothesis that there
are two mechanisms possessed by the animal organism for the
combustion of fat, one of which involves the coincident combustion
of carbohydrate. The varying ketogenic-antiketogenic ratio
might then be a function of the relative effectiveness of these two
biological mechanisms, with the further possibility that adaptation
can be brought about to a low carbohydrate diet by an increase
in the effectiveness of the direct mechanism for the burning of fat. “
Heathertwist, what you quote ” … two mechanisms possessed by the animal organism for the
combustion of fat, one of which involves the coincident combustion of carbohydrate…” Is he suggesting we need a *minimum* level of serum glucose to burn serum fat? If so, I’ve never read this idea in recent research. Indeed, we seem have to drive our blood glucose *below* a certain level to allow fat to mobilize from adipose tissue and into the blood so we can burn it.
Bear in mind Peter Heinbecker observed low ketones in Inuit in 1928, decades before we learned about the CPT1a variant gene that seems to suppress ketone production in many (most?) Inuit. IOW, it’s likely serum glucose levels do not cause the primary effect on low serum ketone levels. –Bryan
heathertwist- Yes, I did see that link earlier. The thing is, they tested 4 subjects, so I’m not sure we can make a generalization about all the Inuit based on this! Though it is fascinating nevertheless.
Well there is that. Although it jibes with everything else I’ve read about testing on the Inuit.
I kind of wonder though, if it really has to do with “high protein diets” and maybe more about certain elements in the diet, esp. the sulfur-containing ones. It seems that the best diets for cardiovascular health are the ones with high levels of taurine … which does not survive cooking, and is found primarily in seafood and organ meats. A number of aboriginal diets did feature either raw or fermented fish or meat.
http://www.ncbi.nlm.nih.gov/pubmed/20804626
Duck you say: “Peter is wise to distance himself from the Inuit. You should follow his lead.”
About following Peter’s lead, good advice. Thanks!
Here’s how Peter conclude that post you refer to:
“Confirming that the Inuit are not poster boys for ketosis is a “so what?” moment for me…It’s a massive dis-service to any one of the many, many people out there who are eating their way in to metabolic syndrome to suggest that a ketogenic diet is a Bad Thing…I’m always amazed by the concept that a ketogenic diet might be temporarily therapeutic but must be discontinued because it eventually becomes Bad For You. It reminds me so much of the converse concept that low fat diets, which might worsen every marker of health which people may care to look at, will deliver major benefits at some mythical future date.
Ultimately, point scoring on the internet about what the Inuit did or didn’t eat shouldn’t destroy people’s chances of health. Destroying a circular argument about Inuit diets may may the destructor feel good. Destroying the feet, eyes and kidneys of a person with type 2 diabetes, who need a ketogenic diet, as a spin off from that victory must be difficult to live with. I don’t know how anyone can do this.”
Absolutely agree! –Bryan
“Ultimately, point scoring on the internet about what the Inuit did or didn’t eat shouldn’t destroy people’s chances of health”
We agree. It shouldn’t. But, it’s yet another straw man argument. Explaining to people that the Inuit are not in ketosis does not “destroy people’s chances of health.” Get real.
A ketogenic diet should not require “poster boys” to prove its efficacy. LCHF advocates like Andreas Eenfeldt knows this well and isn’t afraid to explain it to the people he’s trying to help. It shows that he’s above and beyond such storytelling.
I honestly don’t know why anyone would think that exposing a myth is going to “destroy people’s chances of health.” I’m fairly certain that ketogenic diets do not require such myths to help people. If you think such storytelling is necessary, then I don’t know what to say.
Sure Duck. Why not add Hyperlipid’s Peter to your growing list of folks you accuse of slinging “straw-man arguments?”
Let’s look at your comment on Peter’s quote: “…it’s yet another straw man argument. Explaining to people that the Inuit are not in ketosis does not ‘destroy people’s chances of health.’ Get real…”
Well Duck you and I and bunch of other people here know that, at a biochem level, Inuit ketosis may not relate to non-Inuit LCHF states. But there are many others, people new to this, who won’t sort that out right away. Maybe even never. Those people who suffer from diabetes or other metabolic disorders who hear about LCHF but are afraid to try it. They’ve heard all their lives that “they need carbs” and “dietary fat with clog their arteries.” Like most people these nutrition newbies assume “ketosis” means burning ALL fat-derived nutrients. And who can blame them when so many “authorities” present “ketosis” as the default “other” energy metabolic state to glycolysis?
Then these newbies hear about the ancestral Inuit who lived healthy full lives eating almost no carbs. The Yupik-Inuit are the top success story in our world for living ancestrally on low carbs. These newbies get excited thinking “maybe there IS something to LCHF after all. Look how well these far northern people lived on it!”
Then folks like you come along, hell-bent on exploding Inuit myths, asserting “Inuit are not in ketosis,” “Inuit are ‘different’ from us, that “they eat ‘excessive’ amounts of protein (whatever ‘excessive’ is) and finally “we can’t use Inuit as an example.” You ignore the fact that LCHFers can choose any protein/fat balance within LCHF, that what’s most important is to both *lower the amount of carbs* and lower the *effective glycemic index* of endogenously produced glucose–e.g. from gluconeogenesis so as to keep serum glucose low enough to allow full fat mobilization from adipose tissue. From all I’ve see from direct tests of ancestral Inuit, that’s exactly what happens–the ancestral Inuit have lots of mobilized fat and low serum glucose. I have not see one direct measure of ancestral Inuit that doesn’t show full fat mobilization into serum. None of the text sources you’ve copied in here for us has ever shown that.
Duck, so what if you are correct in some of your specific narrow charges? Whether you mean to or not, you risk discouraging those suffering newbies who seek solutions to their metabolic ills, who don’t understand that your attempts to debunk certain Inuit myths has no bearing on their experience with LCHF.
Call Peter’s statement a straw-man argument if you like. I truly don’t care. You strew you “arguments of fallacy” charges around like confetti anyway. What I care about is that the nearly all the Inuit stuff you intone here can grievously mislead those newbies. Duck, you can bet that, as someone who suffered in a state of diabetes, for whom LCHF has put T2D into complete remission and truly gave a new lease on life, I’m going to keep calling this stuff like this out every time I see it. –Bryan
Anna, Duck, here’s a site that goes into a great deal of detail about ketosis. The most extensive treatment on this metabolic state I’ve seen. I’m trying to find how the author, Dr Peter Attia actually defines “ketosis.” I hope he includes it in there somewhere since he goes into such electron-bumping depth.
Also Anna, I scanned that comments and find a lot of reasonably intelligent convo on ketosis.
Anyway guys check it out if you’re so moved:
http://eatingacademy.com/nutrition/ketosis-advantaged-or-misunderstood-state-part-i
–Bryan
Bryan, I’m sure gut micro biome is important, I was just saying what you eat is much more important. How often you exercise too. A high carb meal or a work out is going to affect your insulin response and blood sugar level so much more then your microbes. So people eating RS while on HC diet and not exercising is a bit confusing to me.
Besides, you can change what you eat every meal, you can work out, but you can’t really change your microbes in a meaningful and aware way, it’s not like you can pop a “good bug” pill.
And as for the correlation, how do we know that it’s not the other way around? may be your insulin response affects your microbes?
And what about fasting? my microbes are still there, yet my BG can be 50. It can only be so low during a fast because of ketones, not my bugs.
Our micro biome is very complex, as we all agree, we know and understand is so very little indeed.
Interesting experiment with RS, many people claim good results, I’ve never tried it. It doesn’t really seem natural to eat large concentrated quantities of it in one sitting. As Morgana said, potatoes are relatively new and wasn’t available to many tribes.
I think our bacteria adapts to the type of fiber we eat, every plant we eat has some food for our biome, even meat does! and RS is not a must for our or our biome survival. Plenty of people dr Price observed weren’t eating RS and were healthy.
Also, as Morgana said, if we eat HF diet, we may not need our biome to produce SCFA, or at least not as much.
Oh yes Anna I agree with you in the main. For most people, the more they get right the other elements in life, e.g. doing at least consistent even if modest aerobic exercise with bursts of resistance, organic/pesticide-free whole foods, proper sleep, and proper stress management (that’s a tough one), the more that gut flora corrects on its own. Like you suggest, our systems are very dynamic, no question our system affect gut bug life and vice versa. There are actual “good bug” probiotic pills, but we have very many questions and doubts about those, including how well do they survive the trip through the very hostile stomach environment. However, we have very clear documented evidence that fecal transplant have greatly helped people and even saved their lives. Many health providers, including my HMO Kaiser, now perform fecal transplants.
http://my.clevelandclinic.org/services/digestive_diseases/departments-centers/gastroenterology-hepatology/fecal-transplant
In some cases, the gut flora is so deranged, the “host” needs to do an intervention. In the worst case, like those with stubborn C. difficile, this can mean that fecal transplant mentioned above. Other people less afflicted *may* be able to benefit from a course in resistant starch. But I emphasize *may.* My first dose of potato starch made me feel *wonderfully calm.* No question I derived a benefit. But that was it! I got -nada- from PS and other RS starches after that, least what I could perceive, how I felt and checking BGs.
Bryan,
yes, some people are definitely so sick and their gut flora is so compromised that they need a transplant to help fix it. But that’s a very clear intervention that has clear results, not like eating some probiotic pills, as you were saying that may not even make it through a stomach.
Btw, I wonder if a simple few days fast would have fixed the gut flora issue by simply starving the bad guys?
Brian, how do you know you are in ketosis most of the time? Do you check your ketones level? at 50-80 grams of carbs, depending on your protein intake, I’d expect you to be out of ketosis often after a meal.
Can I ask you why you have stopped all the vitamins? Please share at least some of the reasons that are in your “book” 🙂
Thanks
Hi Anna, sure I can explain it. From 2007–2011, I carefully tracked all the macro- and micronutrients in every meal I ate, using the spreadsheet + USDA Nutrient Database and other measures which I mention elsewhere in this forum. I finally honed my foodway down to a set of foods (still a quite broad list) that works for me and I know the macro counts by heart. I no longer check my ketone levels, but with reasonable cell sensitivity and keto-adaptation, it often tests low/negative anyway. I stopped that but I still check my BG levels, which is a more informative check for me because my native serum insulin is so low (avg 0.6-0.8 ng/L) that even a modest pop out into glycolysis immediately reflects in high BGs. I keep my protein intake modest and very high quality (lots of eggs from pasture-raised chix), so have little or no excess for my bod to turn into glucose/fat. My macro balance is 80% fat, 15% protein, 5% carb.
About vitamins, the main concern is that oversight for this vast $26B market is woefully lacking. It’s truly a Wild West, or Wild East as you’ll soon see. The FDA treats supps as food, and so are in theory subject to the same oversight. In reality the FDA, already terribly understaffed and budget-starved, devotes almost all its monitoring resources to “real” food. This is very troubling when you consider most of the supps ingredients come from China where just about anything goes. Tens of thousands of little Mom & Pop shops produce many of the supp ingredients like glucosamine and condroitin and even in the larger factories which produce vitamins like Vit C, QC can be sorely lacking. E.g. the water they use to process the mins and water soluble vits (like the Bs, and C) could come out a polluted river and be filled with heavy metals like cadmium and mercury. Some years back I spend an hour on the phone with a Solgar manager, who told me the Vitamin C in *all* supps comes from China, because China drove the cost of manuf so far down it put everyone else out of biz. Then there’s actually making the doses to the stated amounts, novel formulations with still unknown bioavailability, possible estrogenic compounds like BPA and phthalates in the gel caps and enteric coatings, and the general concerns of taking pharmacological doses of anything.
Hi Bryan,
thanks for your reply about vitamins and your ketosis/BG tests. I see your concern with contamination, but I guess that for me the benefits of Vitamin C, for example, outweigh the potential dangers of contaminants, which I think our livers are build to handle. Plus vit C helps to detox them anyway. But I think the more “healthy” one is, whatever that means, the less important vitamins are.
Hi Anna–
I totally agree our livers evolved to be able handle a certain level of contaminants. It’s not like pre-ag “paleo” world was a pristine place. Our ancient forebears constantly ran into natural toxins, arsenic, lead, aflatoxins, etc.
My concern is that our modern world bombards us non-stop with novel chemicals, many of which have still undetermined long-term biological effects on us. Their cumulative presence may now be persistently overwhelming our toxin filters. So many of the thousands of humble quotidien products we use are mute monuments to extraordinarily complex engineering, containing up to thousands of compounds, again many of them novel, existing only since 1945. We encounter them everywhere, in our homes, like in carpet and drywall, in our cars, in our kitchenware (plastic, teflon, aluminum), in our workplaces, and yes, in the formulations and coatings of our supps. Once I appreciated this fact, I went into full mitigation mode, to reduce as many potential toxins in my life as possible. I agree with you that Vitamin C benefits us, and that we actually need it to prevent scurvy. That’s one of the reasons I created the “spreadsheet + USDA Nutrient Database”–to assure myself I was getting the RDA on Vitamin C. I am not convinced that pharmacological amount of C or any other micronutrient help us and in fact may even *work against* us, e.g. loads of supp C and E can shut down our own bod’s endogenous anti-ox production and result in greater insulin resistance:
http://well.blogs.nytimes.com/2014/11/26/why-antioxidants-dont-belong-in-your-workout/?_r=0
and above certain levels, supp vits C and E may even become *oxidants*
http://www.theguardian.com/science/blog/2009/nov/03/vitamin-c-pro-oxidant-blood-pressure
And I agree with you than more robust health can reduce our micronutrient needs. Our bods and their microbiomes evolved a tremendous ability to produce, store, and conserve vitamins, to conserve minerals, and to produce their own anti-oxidants. All the more reason to seek our micronutrients through our food. –Bryan
Not at all sure you’re right about that, Bryan. The RDA of C prevents scurvy, but Linus Pauling pointed out that taking more than the RDA engendered more uses for it through induced enzyme formation. His theory of heart disease involves not enough C weakening the collagen of the arterial wall which exposes lysine residues to which lipoprotein(a) attaches as an emergency repair, which becomes plaque.
I had chronic fatigue syndrome in the early ’80s, learned of Dr Cathcart’s bowel tolerance C therapy, took 140 grams per day without so much as a murmur from my guts (!) for three weeks, then rapidly tapered to a normal bowel tolerance of 10 grams per day as my chronic fatigue resolved. I never took less than a gram or two of C from that day to this for fear of a relapse.
The point is that I applied Pauling’s heart disease remedy long before he ever published it, and my coronary artery calcium score is now zero, meaning no atherosclerotic plaque whatsoever – this is a quite remarkable result for a thirty-five year insulin-dependent diabetic, possibly unique.
Just saying.
Hi Jonathan. I don’t question at all your personal experience. The amount of Vitamin C we might benefit from can vary wildly from person to person. You’ve been T1D for many years, so it’s easy to imagine that the common co-morbidities you often find with T1D set up a greater anti-oxidant need. While I generally feel we should regard supps very warily, I’m certainly not saying people with pathologies for which supps might give therapy should avoid them. By all means they should go for it. Indeed, I took supps in 2007–2009 when still early in my T2D remediation. But for people with no frank pathologies, I hope they will consider to seek micros through food where for them the doses are likely to be right-sized, and in the proper formulation and matrix for optimum bioavailability and absorption, plus they avoid the toxins that too often come with supps. About what you say “…not enough C weakening the collagen of the arterial wall which exposes lysine residues to which lipoprotein(a) attaches as an emergency repair, which becomes plaque…” if you can cite specific research that supports it, that’d be great. About your coronary artery calcium score, when did you first start getting that measured and by with method? –Bryan
Abundant refs in Linus Pauling’s How to Live Longer and Feel Better. He and Mathias Rath did the lipoprotein(a) research, find it on PubMed. I had a virtual colonoscopy 10 years ago, then an EBCT scan two years ago, then a CT scan in hospital for my guts. Zero calcium. Pauling pointed out that primates don’t make vitamin C out of glucose like most every other living thing on the planet except guineau pigs and a couple of other creatures. If you scale the amount of C a dog makes to human weight, you get several grams – guineau pig chow contains the human equivalent of 8 grams of C
“Abundant refs in Linus Pauling’s How to Live Longer and Feel Better.” Um. OK.
“an EBCT scan two years ago, then a CT scan in hospital for my guts. Zero calcium…” Jonathon, you started your Vitamin C therapy in the 1980s, right? That’s 30 years before your EBCT scan. While your Vitamin C may well have played a role in abating your coronary artery calcium, that’s quite a long time from the start of the therapy and your scan. We often make countless changes in diets and lives in 30 years. How can you be sure that Vitamin C alone is responsible for these salubrious effects? –Bryan
Quite so. Nevertheless, I’ve been taking grams of C for those 30 years, and the outcome is what Pauling predicted – zero plaque. My doctor said “We think that’s genetic!” so maybe I’m just a fortunate mutant. It’s entirely anecdotal – but anecdotes can be quite convincing when you’re the subject of the anecdote. I generally bow out of debates with folk who have heart disease with: Have you got a better idea?
Just curious, but has anyone else heard that there is risk with Vitamin C supplementation when iron stores are high?
See: Most Free-Radical Injury Is Iron-Related: It Is Promoted by Iron,
Hemin, Holoferritin and Vitamin C, and Inhibited by Desferoxamine
and Apoferritin (1994)
I donate blood, keep to the bottom end of normal. Scary stuff, iron!
Duck, high iron by itself is not really optimal anyway, without vit C, so it’s best to keep it low regardless. So I donate blood.
And if iron was using up all vit C stores, we would get scurvy if iron was high, clearly, not all vit C is used up by iron, so perhaps there is another size to the story, but interesting nonetheless. May be vitamin c actually neutralizes iron by donating electrons?
I know that vit C increases iron absorption.
Duck,
did some more digging about iron and vit C and found some more stuff that seems to debunk the iron/vit C issue that is observed only in vitro, but not really in vivo.
“There is a considerable amount of in vivo research into this vitamin C/Fenton question. Without fail, in vivo research has NEVER been able to demonstrate that vitamin C is dangerous because of Fenton like reactions. Without fail, in vivo research ALWAYS demonstrates a positive effect of vitamin C on oxidative markers and damage in tissues.”
Click to access BW_iron.pdf
And Bryan,
here is a nice summary of vit C studies that show that vit C is not a pro-oxidant, but instead causes “a reduction in markers of oxidative DNA, lipid, and protein damage”
http://www.fasebj.org/content/13/9/1007.full
Anna, about that FASEB published study on Vit C, does it make clear what kind of C it is? Supplemental or in food? Maybe the report says it somewhere; it just didn’t jump out at me. Also, the authors are affiliated with the Linus Pauling Institute, founded by the man who is likely the single greatest proponent in history for us to take pharmacological amounts of Vitamin C for its purported health bennies. We must consider the bias that may be inherent in this report. Unfortunately the world we live in now compels these concerns. Special interests so often drive “science” these days. We live in a world where revenue-starved gov’ts have had to slash funds for research that once had any hope to be independent. I’m not saying this report concludes wrong info. Just saying we should always questions the sources. –Bryan
Bryan,
I agree, we should question the source, but we should read both sides and see which one makes more sense. To me so far, the Linus Pauling Institute side makes more sense and it’s backed up by my personal experience as well. Besides, they are not making money on vit C as it can’t be patented and is very cheap, so their conflict of interested is much less, although obviously can’t be ruled out. So I’m always looking for the new information about vit C that will make me change my mind.
As for FASEB study, they were looking at multiple studies that used supplemental vit C. Vit c in food is too low to even have 500 mg. Plus, if it were food, it wouldn’t be clear which compound of this food affected the results either.
As for NYT article, I’m not sure about the details, but my suspicion is that they are speculating as it’s hard to measure real anti-oxident production inside a human mitochondria, so I’m not sure how they are claiming that.
And I agree, adding more stuff is not always good. As I’ve said before, I’ve greatly reduces the amount of vitamins I take, but to me vitamin C is a good gamble (as we can’t ever be 100% sure) and I take my chances with it. I’m not striving for just optimal, obviously many people have lived very long lives without supplements, so it’s clearly possible. I’m pushing the envelope in hopes to exact a little more longevity. And if you believe in ROS theory of aging, dealing with ROS is very important and I think vit C helps with that.
And yes, most people should first reduce omega-6 oils, carbs, orange juice, rancid omega-3s pills, antibiotics, Lipitor, coca-cola, etc, before considering sups.
Best, Anna.
“…anecdotes can be quite convincing when you’re the subject of the anecdote…” LOL, Jonathon, so true! –Bryan
Jonathan, very impressive. Out of curiosity, how did you take 140 g of C a day? That’s a lot of pills to swallow. Also, how much C do you take daily now?
thanks
Allergy Research Group Mixed Mineral Ascorbates in water every hour – tastes like chalk! Cured CFS in an aunt and my sister, but not in the daughter of a friend so 75% success in n=4 expt
I was taking 5 grams per day, but then I caught a tummy bug and went down to 2 grams per day since 5 seemed to piss off my guts
Jonathan, cool thanks.
Bryan, most of the studies that test for vit C, use only 500 mg a day, like the study referenced in one of your articles. It’s far too little to make a clinical difference for most people.
Another point, we need vit C not just to prevent scurvy, it’s important for collagen formation, that’s why it’s all the range now in face creams. It’s also heavily used by the immune system, especially when it’s under attack by a virus, for example, bowel tolerance increases dramatically.
It’s also critical for detox (acting as a reducing agent), given that we live in a much more polluted world. Unfortunately, I don’t have any references now to back it up, as I’ve looked into it many years ago. I only have my n=1.
The fact that vitamin C has pro-oxidant as well as anti-oxidant properties is well known and not news. In 1986 Linus Pauling wrote in his book HOW TO LIVE LONGER AND FEEL BETTER in the chapter Vitamins in the Body:
“The ways in which ascorbic acid (Vitamin C) functions in the human body relate first to the fact that it engages on both sides of the universal oxidation-reduction reaction that subtracts or adds hydrogen atoms to a molecule. (Vitamin C) is readily oxidized to dehydroascorbic acid by the surrender, to oxidizing agents, of the two hydrogen atoms… [shown in the figure]
This action is readily reversible, for dehydroascorbic acid acts as a strong oxidizing agent, and by picking up two hydrogen atoms is reduced to ascorbic acid. It is likely that the reducing power of ascorbic acid and the oxidizing power of dehydroascorbic acid are responsible for some of the physiological properties of the substance.” [PAULING, 1986]
from here:
http://www.vitamincfoundation.org/lunec.htm
Hi Anna, you said: “…most of the studies that test for vit C, use only 500 mg a day, like the study referenced in one of your articles. It’s far too little to make a clinical difference for most people…”
What do you think is the minimum daily dose to make a clinical diff for most people? –Bry
Bryan,
To make a difference for really sick people, they need to test vit C close to bowel tolerance levels taking it in divided doses through out the day. And for normal “healthy” people, I’d at least test in grams, not milligrams, again, in divided doses through out the day with 2-3 grams being a minimum tested.
That NYT piece discusses how even 1g (1000mg) per day Vit C can contribute to shut down our bods’ endogenous anti-ox production. Endogenous anti-oxes which appear to give the additional bennie to increase insulin sensitivity. The 2–3 g per day supp Vit C you cite goes well beyond that dose the NYT discusses.
I suspect we’ve learned enough about nutrition to be dangerous to ourselves. Or at least to act against ourselves. However unwittingly.
We are in a unique period in our human existence in which we can, and do, accelerate the “adding” of novel substances to our lives, like supps. Since the end of WWII, we’ve seen and experienced massive novel inputs into our lives, thousands of new organic compounds, antibiotics, etc. Our response to the emerging chronic pathologies from the ’70s onward has been to throw *more* synthetic stuff at them, like supps, in the hopes to mitigate them. Anna, IOW, we keep *adding* stuff with the hope to mitigate the massive amounts of novel inputs we’ve experienced. Where does that endless feedback loop finally stop?
Maybe we should consider to *subtract* stuff from our lives? At least see what happens? –Bryan
Anna, btw, the “Made in USA” label means zip. The manuf can import all the supp ingredients from China, stuff them into caps, and slap a “Made in USA” on the bottle. Perfectly legal 😦
Duck, let’s please not distract from the main point: We can’t say–at all–how healthy or harmful early grains were for people. You often imply that early grains are healthy, or at least not health-harming. E.g. you said: “…the cultures that thrived on…wheat.” The *culture* may have thrived. But we have plenty of evidence to suggest the *individual* did not thrive. The very strong, likely predominant focus in this forum is how we can optimize our *personal* health, no?
You say: “Please. I’ve already given the sources here.” Duck, I wish you’d more carefully read my posts before you answered. You simply confirm what I said. Your most modern source is from 1938. To repeat from my previous post, is long before we have blood marker testing, epidemiology, and biochem understanding to even begin to speak with any authority how healthy or not any wheat is, early or modern. None of your links offer adequate science. The links mainly support beliefs, however widespread these beliefs may be. We all know too well that even a very strong chorus for or against something can, in the end, be proven very wrong. E.g. for 1500+ years the mainstream believed in Ptolemy’s geocentricity–that all celestial bodies revolved around our Earth–until the 17th century. The mainstream believed classical physics until quantum mechanics came along last century.
Indeed Duck you do concede “…Nobody can ever really prove anything one way or the other [regarding how healthy it is to eat early grains]…” But then we move right on to this your graf which starts: “Do note the references showing that bread, and specifically wheat, was considered to be the healthiest of all foods…” You then go on to underscore the reputed wonders of grains, replete with plenty of your italicized words to hammer home your points to us. Duck, can you see how the reader might get the idea you feel early grains were very healthy for us? At the very least, your message is very tendentious toward them.
Finally Duck what you say here is a near total fail: “Let’s not conflate life expectancy at birth with life span. Hippocrates lived to between 83 and 90 years of age. Aristotle lived to 62. Von Linné lived to 70. Medieval scholars had an average lifespan of 59–84.3 years in the Middle East and 69–75 in Islamic Spain. New England colonists had lifespans of 62-65 years.” Really Duck?! Your first three examples are three n=1s? How rookie a logic fail is that? About the scholars, it’s stupid to choose a small and privileged segment of society and imply their average lifespan somehow represents that of the rest of society. Even in a modern Islamic society discussed here: http://bahai-library.com/lapidus_history_islamic_societies the scholars (“ulama”) represented only 20% of society. Your New England colonists stat is most interesting. The link you gave me is broken, but I found this: (http://www.columbia.edu/itc/hs/pubhealth/rosner/g8965/client_edit/readings/week_3/demos_1.pdf). The lifespans table on page 77 aligns with what you say for people 21 and older.
And guess what? The Pilgrim’s main grain food was *corn*–not the glutenous grains like wheat and barley: https://www.plimoth.org/sites/default/files/media/pdf/edmaterials_diet.pdf. Very interesting!
Of course I agree we can’t prove the positive or negative health effects of early grains, glutenous and otherwise. People can keep posting links ad infinitum to support their beliefs, hunches, notions, and predilections. Many of these links are very interesting to read and discuss, but they also can be very misleading. Which is why I’ve been saying here people should ultimately *test themselves* with as many of the health measures they can do at home and coax out of their docs, track them and their lifestyle inputs over as long as term as they can, and learn to interpret their results **in their context and totality**, generally avoid to put a lot of weight on any single measure. We can no more say that ancient grains are health-promoting than we can say they are health-inhibiting.
WBryanH said: “let’s please not distract from the main point”
Well, you and I have different points. While you seem to have an agenda to demonize grains, my main points are that the evidence demonizing grains is circumstantial, at best, and that, right or wrong, Western civilizations believed that wheat was the most nourishing of foods right up until the Industrial Revolution. Perhaps all of our ancestors got it wrong, but it is a simple fact that wheat was once seen as the perfect food.
In fact, the 1857 edition of The New American Encyclopaedia literally states:
This was not a controversial statement at the time. It’s just what people believed (again, right or wrong). The demonizing of grains is based on ignoring other influential factors. I can’t prove that grains are amazing and I won’t say that everybody needs to eat them. I’m simply providing an oposing perspective against all the grain bashing here.
WBryanH said: “Your most modern source is from 1938…The links mainly support beliefs, however widespread these beliefs may be.”
Yep. That’s my point. You do understand. 🙂
WBryanH said: “We all know too well that even a very strong chorus for or against something can, in the end, be proven very wrong.”
Sure. But my first point was that the anti-grain evidence that’s being presented here in these comments is misleading. If you’re going to prove that grains are bad, looking at skeletons and populations that experienced other diseases isn’t going to prove anything.
WBryanH said: “You then go on to underscore the reputed wonders of grains”
Perhaps you misunderstood. I simply pointed out that, right or wrong, our ancestors widely believed that there was no better food than wheat. You can choose to ignore that history if you wish. But, I think it’s worth pointing out.
WBryanH said: “Finally Duck what you say here is a near total fail”
lol. It’s rather funny that you think a fact is a “fail”. Like it or not, those were the average life spans of the time.
So, yeah, you’re one of those individuals who perpetuate shortened life span myths.
WBryanH said: “And guess what? The Pilgrim’s main grain food was *corn*–not the glutenous grains like wheat and barley”
Again, this is misleading as your own source states that they had been “familiar” with English wheat, rye, barley and oats before coming to the New World. I suppose you also think they all had diabetes and were obese in their 70s. lol 😉
WBryanH said: “Many of these links are very interesting to read and discuss, but they also can be very misleading. Which is why I’ve been saying here people should ultimately *test themselves* with as many of the health measures they can do at home and coax out of their docs, track them and their lifestyle inputs over as long as term as they can, and learn to interpret their results **in their context and totality**, generally avoid to put a lot of weight on any single measure. We can no more say that ancient grains are health-promoting than we can say they are health-inhibiting.”
Amen. See, we do agree!
So, let’s end the grain bashing then. None of us know one way or the other.
Duck, it really does seem we’re in alignment on many nutrition issues. Only I need to reject your premise I “demonize” and “bash” grains. I challenge you to find anyway where I categorically assert that people should avoid grains. You won’t find anything remotely like that from me. As far as the fulsome evidence you supply to support your statement that “Western civilizations *believed* that wheat was the most nourishing of foods right up until the Industrial Revolution” sure that is fine. Only Duck, why do you seem to feel the need to supply all this history, since most of us knew it already, or at least have a strong cultural sense of it? Praising grains already was the default till very recently, and it still is in many places. Even the Bible holds grains high. Duck, you really shouldn’t confuse the very appropriate questioning of grains with “demonizing” and “bashing” them.
As far as life spans, you totally miss what I was saying. You say: “…this is misleading as your own source states that they had been “familiar” with English wheat, rye, barley and oats before coming to the New World. I suppose you also think they all had diabetes and were obese in their 70s. lol ;)…” Sure Duck the colonists were “familiar” with these glutenous grains. But in the New World they were eating mainly *corn.* Duck, what part of that don’t you understand?
Duck, I wish you would actually *read* the things you comment on. That’d make things more interesting at least.
Anna said: “Do you think that white flour is a problem and whole wheat is ok, or it doesn’t matter, any wheat flour is ok? Perhaps the milling process is what makes the difference?”
White flour has no nutrition, and therefore it cannot sustain life. White flour is well known to promote degenerative diseases. This was well documented by Dr. Weston Price and Sir Robert McCarrison. In 1931, Sir Robert McCarrison gave a series of lectures, at the Royal College of Surgeons, summarizing his findings, saying:
Dr. Price also observed very healthy Swiss eating mainly whole rye, dairy and very little meat. So, those observations and McCarrison’s studies clearly support the superiority of whole flours over white flours.
However, I think that one can probably get away with eating white rice or white flour if they can find a way to make up for the nutritional losses in other ways. For instance eating white rice or a few slices of baguette with other mineral-rich foods (hemp, cacao, seaweed) may end up being a wash.
European countries seem to do OK on white flours because they do not fortify their flours with enrichments. It’s been known for almost a century that tastebuds can crave B vitamin enrichments that are added to white flours. In most of Europe, there are no enrichments in their white flours so one’s tastebuds automatically craves B vitamins from other sources (i.e. actual food).
So, my feeling is that white flour in the US is particularly problematic due to the enrichments. In Europe, you would naturally gravitate towards getting your nutrition elsewhere. You’d have no choice actually, because if you didn’t get your nutrition elsewhere, you’d become deficient and lose your appetite (a well known symptom of B vitamin deficiency). Therefore, we might say the enrichments added to white flour are something that enables people to eat refined foods as a staple, which they would otherwise be unable to do if the enrichments were not there in the first place. Keep in mind that some countries, like Denmark, actually ban enrichments.
Aside from that, there are likely other issues with modern flours. In France, they have the Pain Décret, which is a law that limits the ingredients of traditional bread to wheat flour, water, yeast, and common salt. In the US, you can add whatever garbage ingredients and enrichments you want to baked goods. Plus, industrial mills fumigate (sometimes bromate) and process the hell out of flours.
Also, industrial whole wheat flours are not ground up wheat berries. What they do is they create white flour using all the processing and then they claim to reconstitute the bran and germ.
This all makes it very difficult to pin down what’s actually wrong with modern flours. My guess is that the processing, adulterations and enrichments are more problematic than wheat itself. However, if someone’s gut is damaged, they will have trouble with wheat no matter how good the wheat is.
Incidentally, the The New York Times recently published an article (see “<a href="“>Bread is Broken“) that claims that industrial mills discard the wheat germ and don’t add it to whole wheat flours—even though they are supposed to by law. It’s a shame because Vitamin E is protective of some of the damaging effects that may be attributed to gluten.
Basically, we don’t eat real wheat anymore. You can grind your own wheat berries or find a baker that grinds its own whole grain flours. Anecdotally, people seem to think that they tolerate real wheat better, and I wouldn’t be surprised.
Anna said: “I’m curious, do you have any theory on why americans are getting fatter and fatter and more and more people world wide are having Diabetes? If it’s not wheat, then what? Do you blame sugar or simply too much calories? and if it’s increased caloric intake, why did it happen?”
Zhou et al. have a relatively new theory that it’s the flour enrichments. They note that developed countries that fortify their flour have significantly more obesity and the timing of mandated enrichment increases mirrors the rise of obesity in those countries. They hypothesize that the enrichments are promoting obesity and possibly stimulating appetites. I think they are on to something.
You can try it yourself. Anecdotally, you may notice that making a recipe (say pizza, for instance) out of enriched flour may stimulate your appetite more than organic unenriched flour. The reseach suggests that the appetite stimulating effect of B vitamins may depend on your B vitamin status however.
Cheers
“White flour has no nutrition, and therefore it cannot sustain life. White flour is well known to promote degenerative diseases. This was well documented by Dr. Weston Price and Sir Robert McCarrison. In 1931, Sir Robert McCarrison gave a series of lectures, at the Royal College of Surgeons, summarizing his findings, saying:”
What I wonder, reading this, is: did you read the blog post we are discussing? White rice is just as nutritionless as white flour, which is exactly the point Denise is making. Actually white rice is WORSE, because it has very little protein. And yet in Kempner’s protocol, people did well on the diet. I do believe iron is a cofounder there. So, IMO, is the fact that rice works differently than wheat. And/or, as Denise theorizes, maybe it has to do with the amount of fat (we are waiting with bated breath for the next post!!!).
As to “we can’t know what happens” … have you even READ Denise’s take on the China Study? I mean that is a long blog post or two and some big number crunching, but you can’t say it doesn’t have many people and it involved home-grown “natural” wheat too. The whole reason I started following rawfoodsos was because of Denise’s brilliant work there. But you are basically trashing the entire basis of her work … she is carefully and mathematically looking at the evidence.
Now if you don’t like the evidence for some technical reason, then sure, talk about the geeky details about why the numbers are wrong. But “It’s too hard to figure out” doesn’t really hack it with geeks; that sounds like the Homer Simpson Defense. And yeah, if you are defending wheat, you should use some of the post-1940 science, which gets down to the chemistry of all this.
Anyway, I get the impression you don’t really understand the science of what you are talking about, and are talking more at an emotional level. As a matter of courtesy though, you should read Denise’s basic article, and also the China Study articles, which are pretty amazing.
Duck, thanks for your reply.
I read dr. Price and he indeed showed that whole grains are better then while flour. I didn’t remember him observing any tribes eating whole wheat though, so thanks for the reference of Hunza indians. Although, it’s hard to draw any conclusion from just one example, especially because they practiced caloric restriction and protein restriction that skews the results:
http://undergroundhealthreporter.com/hunza-diet-health-weight-loss/#axzz3tBUxQwpL
So it’s still not clear to me if whole wheat and whole grains are directly beneficial and life extending or just not as harmful as white flours.
As for the vitamin B flour fortification theory, I didn’t see any evidence of that in Russia, where I’m from. Flour is not enriched in Russia, yet diabetes is on the rise there as well and obesity is becoming more common. Also, my remote relatives in India are vegetarians and have extremely low vit B levels, yet it didn’t affect their hunger, they eat high carb diet, are overweight and pre-diabetic. I don’t know if flour is fortified in india, I doubt that, but they eat a lot of it and have one of the highest per-capita rates of diabetes. So, I don’t think that enrichments of white flour are that consequential.
Why do people overeat if it’s not fortification? because they can! As the world is getting wealthier, the world is getting fatter. So my theory is that overconsumption of food based on availability, access and increased wealth is basically responsible for our obesity epidemic. And diabetes and obesity were always predominately the disease of the rich, who didn’t work much and had access to unlimited food supply.
Pre-industrial revolution agrarian society involved lots of manual labor, walking, etc. to burn/use the carbs they ate. Also, food supply was more limited with practically no snacking on potato chips, chocolate milk, candy, nuts, soda, health bars, etc. People were going hungry much more often. Now the world is getting wealthier and food is getting cheaper because of mass production, subsidies, advancement in agriculture, etc. Combine that cheap food with constant convenient access to it 24/7 and a much less active life style and you will get continuos excess caloric intake that leads to most of the diseases. And this gets worse with every generation because constant insulin spikes or whatever other genome changes in pregnant women, lead to the next generation to be less insulin sensitive and more prone to being overweight.
Even France, with its culture of small portions and no snacking, getting fatter. The French tradition of not opening the refrigerator between meals for a child isn’t as prevalent it once was. Obesity in children is growing at a rate of 17% while obesity in adults is growing at a rate of 6%. The french paradox, ironically could be partly attributed to smoking, as nicotine is an appetite suppressant and lots of french people still smoke. Also, a shot of espresso in the morning, which is very common in France, is appetite suppressing.
I think that carbs need to be tailored to one’s activity level, not precisely, obviously, but if one eats high carb diet that is not calorically restricted, one needs to be active to cycle the glycogen in the muscles to stay insulin sensitive or to practice IF. And while some people can eat high carb and not overeat, for most people constant eating of HC without corresponding physical activity causes increased appetite.
Anna- you’ve been wondering about the obesity/diabetes epidemic. I, too, wonder exactly what the cause is- (though there are many very plausible theories out there). I’m an American living in Germany, and in the 8 or so years I’ve been here, I’ve seen obesity really take off. It does seem to me that in recent years there are far more American-style fast food places here, and more people seem to be eating junk food. I think obesity is pretty well correlated with junk food, and I think, with globalization, this could be the problem worldwide. Some argue that we had fast food back in the 50’s and 60’s, but I think one thing people fail to take into consideration is that many of the ingredients are now different. Along with sugars and high fructose corn syrup- (both of which we’re eating in record proportions, apparently), I wonder if soy and soy oil might not also play a part. (Soy is an endocrine disruptor). In addition to that, there seems to be evidence that some of the additives used in junk food are either addictive, or cause overeating- (similar to what Duck was saying about fortification). For awhile I believed the “high carb” theory, but now I’m not so sure…… well, to be honest, I do notice that generally most people seem to be eating huge amounts of carbohydrate, so it could be that, but that doesn’t really explain how many traditional cultures stayed thin eating relatively high carb diets. Maybe it has something to do with eating processed versus natural carbs, or maybe there were other nutrient dense foods in those populations that were protective? In any case, exactly “what’s causing the obesity epidemic” is a question being asked by many great minds at the moment.
Morgana, thanks for your comments on the obesity epidemic, but may be it’s not some additives or HFCS or junk food, but simply because food is available 24/7 and it’s cheap. It’s easy to eat junk food because it doesn’t require any effort to cook. You can get it any time you want, you don’t need to go home and boil some rice and then wait for it to cook…
Food may be cheap in America; here in Europe it’s not that cheap. In much of the world people don’t have access to good, affordable food. And the thing is, obesity is correlated with poverty, so that doesn’t really explain everything, the way I see it. Although you do have a point, that’s part of it…..but I don’t think it’s the only answer.
Morgana, poverty is relative. Poor in US is not the same as poor in Africa. Junk food is cheap even in Russia. Junk food is cheap relative to income of people in EU. You can’t be obese if you are truly starving. There were no obese people in concentration camps, clearly.
But I’m sure other factors are at play.
For the record, I do think that HFCS and refined linoleic acid oils are also to blame. Interestingly, enriched flour contains a lot of iron which is generally poorly absorbed and is known to promote inflammation in the gut. However, HFCS and linoleic acid are believed to significantly increase iron absorption.
So, it may be eating enriched foods with HFCS and linoleic acid might be particularly bad.
“Only I need to reject your premise I “demonize” and “bash” grains.”
Heh. You literally just wrote a comment warning about the dangers of wheat bran, lectins, and phytic acid while saying “some will argue” that phytic acid is a beneficial. That’s grain bashing. And you’re actively downplaying the research on why antinutrients may be beneficial in those with replete diets.
“As far as life spans, you totally miss what I was saying.”
Life spans have been nearly constant for the past 2,000 years. Furthermore, Americans transitioned to wheat as their principle crop in the 18th century. There’s not much else to say.
Duck, once again, you cite no valid evidence. -Nada-. That’s a recurring problem with you. You do not read thoroughly or carefully.
In essence you’re saying that to question grains is to *bash* and *demonize* them. You’re suggesting that, because I report that my health improved when I left grains, that I’m bashing grains. I’m simply relating my experience.
Duck how does the above NOT underscore your ultimately uncritical grain bias?
Let’s look at what you said:
” …You literally just wrote a comment warning about the dangers of wheat bran, lectins, and phytic acid while saying “some will argue” that phytic acid is a beneficial. *That’s grain bashing*…”
Duck, this refers to comments I wrote to Anna, here:
“my take is that we should regard warily *all* wheat flour. White flour, for the very fast carbs/gluten/lectins and loss of nutrients replaced by fortification plus chemicals introduced in its processing, the potential downsides of which Duck amply covers through the forum (search on “fortification”) Whole wheat includes the bran and comes with its own concerns, e.g. phytic acid that, in your GI, can steal essential minerals from your food. Though some will argue that, in the case of iron which we too often get too much of, phytic acid could be a *good* thing…”
I follow with this:
“I quit grains early on (2007) simply because grains are high in carbs–long before I faced the additional health questions of gluten, hemoagglutenating lectins, and phytic acid.”
I end with this:
“…this is just my n=1. Please get as many health checks as you can, as often as you can…”
What do I actually say here Duck? Do I call grains into question? Absolutely! We all should. Do I “warn about the dangers of wheat bran, lectins, and phytic acid” as you accuse me of doing? No I do not assert they necessarily come with “dangers.” I say only that they pose “health questions.” Do I say everyone should avoid grains? No I don’t. What I AM saying is that people should monitor themselves and see how they do with grains and without grains.
Duck, you really should confront and examine your inherent grain bias.
Wbryanh,
We can agree to disagree. It’s really no big deal. Neither of us are telling people what they have to eat. Question grains all you like. I just think it’s hardly helpful to only question grains without fairly looking at all sides of the story. That’s all. My responses were merely to provide the other side of the story—not to actually prove grains are amazing or whatever.
For the record, I thought heathertwist was the one doing most of the grain “bashing,” referring to Otzi and various skeletons to somehow show that grains were harmful, without considering the other factors affecting the status of those skeletons. It’s a bit more complex than just looking at what was in someone’s stomach at the time of their death.
heathertwist said: “White rice is just as nutritionless as white flour, which is exactly the point Denise is making. Actually white rice is WORSE, because it has very little protein. And yet in Kempner’s protocol, people did well on the diet.”
As I understand it, Kempner’s protocol was not designed for healthy individuals. Rather, it was designed for people to lose weight and regain their health. What isn’t mentioned in the article is that you can achieve the same results with a potato diet (see Chris Voigt) and the success of such a diet is attributed to A) the hypocaloric nature of the diet (you can only cram so many waterlogged carbohydrates into your gut) and B) the significantly increased intake of resistant starch from such a diet (a portion of glycemic starch often passes to the colon as beneficial resistant starch, a kind of fiber). Resistant Starch has been shown in studies to promote much of the health benefits mentioned in this article.
A potato-only diet can be quite therapeutic for weeks or even months. But, a potato-only diet is not really an ideal way to eat long term.
heathertwist said: “have you even READ Denise’s take on the China Study? I mean that is a long blog post or two and some big number crunching, but you can’t say it doesn’t have many people and it involved home-grown “natural” wheat too.”
Yes, I read it awhile back when I myself was anti-grain and low carb. And I don’t recall it ever distinguishing the difference between whole wheat and white flour consumption. Perhaps I missed it. There’s a huge difference between the two, and most anti-grain sentiments miss it.
heathertwist said: “And yeah, if you are defending wheat, you should use some of the post-1940 science, which gets down to the chemistry of all this.”
Ok then.
Wbryanh recommended that one can create a USDA-based spreadsheet and he found he could easily get all his micronutrients (vits + mins) without eating a single grain. However, this approach is rather antiquated and shortsighted (not his fault, it’s just what his anti-grain books told him to do) as it assumes that the health benefits of whole grains are merely due to their basic nutrition profile. Unfortunately, that’s not the case. The health benefits of whole grains are actually believed to come from the phytonutrients that aren’t listed in the USDA database.
For instance, it’s well known that oats are particularly healthy and have anti-diabetic properties. A good deal of the health-promoting effects of oats are believed to largely be from their unique phytochemicals, like avenanthramide and high levels of tocopherols.
Nutritional and functional properties of oats: An update (2014)
Whole grains are not just calories and USDA nutrients. They contain of all sorts of phenolic acids and flavanoids (avenanthramide, ferulic acid, vanillic acid, caffeic acid), carotenoids (leutin, xeazanthin, β-crythoxanthin, β-carotene, and α-carotene), γ-Oryzanol, sterols, stanols, fiber (β-glucan, resistant starch, inulin, oligosaccharides), lignans, and other phytonutrients like amylase and protease inhibitors. [See Table III] A good deal of these health-promoting phytonutrients are removed during the refining process.
So, as much as all these investigations into the known problems with refined grains are very interesting, as far as I can tell (and perhaps I missed it), the anti-grain investigations often ignore the difference between whole grains and refined grains. For instance, I believe the China Study data showed problems with “wheat flour” (not “whole wheat flour”).
Nevertheless, China also has severe iron contamination from antiquated milling equipment made of iron (see Investigation of the wear failure mechanism of a flour milling roller). China also has very high iron in their wheat (see Mineral element concentrations in grains of Chinese wheat cultivars). This may be due to high iron dust from the Gobi Desert, which is known to create enormous iron phytoplankton blooms in the Pacific Ocean. The whole country and its various regions are an ecological and environmental mess. I’m not entirely sure how anyone can easily draw many meaningful conclusions from it without considering those factors.
Finally, the rollermill technology to completely purify white flour has been around since the mid-1800s. Over 90% of the flour consumed in the US is white flour, so it’s hard to say that people are gaining health benefits from giving up whole grains. For all we know, they are just gaining health benefits by giving up (fortified/processed) white flour.
Cheers,
Duck,
Even if properly milled fresh non-fortified whole grains are healthy, don’t you think it’s a moot point because they are simply not available to americans? As you were saying, even whole wheat flour/bread is not really whole wheat, so what’s the point? Nobody is going to mill grains at home… Isn’t it better to avoid it all together then?
Also, your studies claim whole grains as being healthy, but compared to what diets? To white flour/sugar diet or to very low protein starvation diet? Sure, whole grains will be better. I apologize if I missed some links, but have you seen any human studies that compared a whole grain Wheat diet with a diet absent of wheat and refined sugars and not nutrient deficient? How would they compare? How would whole wheat diet compare to a Low carb diet?
I wonder, is there anything in whole grains that a grain-free diet would be missing? or are these “healthy” nutrients in whole grains are only needed to “protect” the body agains the high carb content on these grains?
Thanks.
One of the benefits of eating grains is to not be an orthorexic party pooper. Grains are so incredibly tasty. And yes you can get quality fresh milled grains in america. Also they are mineral dense with a lot of manganese and selenium. Plus they add quality carb calories that displace a lot of inflammatory protein and fat calories in most diets.
Zach, yes I agree with you on one point, the only benefit of eating grains for me is enjoyment, especially freshly baked goods.
Where can I buy bread or other baked goods made form freshly milled grains? I’ve never seen that.
As for selenium and manganese, lots of it is in fish and seafood.
And as for fats/proteins being inflammatory, I’d say carbs, even whole grains, could be just as inflammatory if eaten in access, if not more.
Seafood is so dang contaminated, I’d be hesitant to eat it more than once a week or so.
Can you give me an actual mechanism on how carbs are inflammatory. People love to say that sugar/starch is inflammatory but iv yet to see any proof. Protein and fat on the other hand have many known mechanisms for causing inflammation.
May be seafood once a week is enough for our selenium needs.
You propose whole wheat as an alternative, but you still didn’t answer where an average american can find freshly milled grain products for everyday consumption?
Carbs are inflammatory via insulin resistance and hyperglycemia. Just look at diabetics. Untreated high blood sugar leads to all sorts of complications, it’s common medical knowledge.
And before you say that it’s fat that causes diabetes, not carbs, it doesn’t really matter what causes it, but after you have it, if one keeps eating lots of carbs and calories, diabetes gets worse. So yes, carbs and proteins and fats can be inflammatory if one consumes excess caloric intake. Carbs just make it easier for most people to overeat and LC makes it easier to eat less. Perhaps just like very low fat, I don’t know, I didn’t try it.
A good brand of whole grains is Bobs Red Mill, if you don´t have a store that sells them they can be ordered probably from amazon or go to bobsredmill.com. You can make a heavy bread by soaking 2 cups of whole or cracked grains like buckwheat, rye, wheat – soak overnight then the next day add enough water to blend into a thick paste roughly one cup of water, add a bit of salt, and let it ferment until it rises a little and bubbles a little, one to two days usually. Then bake – not to hot of an oven it makes a heavy loaf and if you don´t bake it enough it will be wettish in the middle. Google how to line a loaf pan with parchment paper and you will get your loaf out of your pan super easy. If you want a thicker loaf use more grain. I suppose you could add yeast or baking powder if you want it to rise a little more.
Rebecca, thanks for the suggestion, but I assume that Bob’s flour is not going to be fresh, probably months old, so oils will be rancid and components oxidized, not exactly freshly milled as people used to eat it…
I was talking about buying whole grains not flours.
Rebecca, sorry, I’ve misunderstood your post. I didn’t realize that you can make bread using only cracked wheat. How does it come out? Does it taste similar to normal whole wheat bread?
thanks!
I have only made this once, I used a mix of whole buckwheat and cracked buckwheat, but the principle applies to wheat and rye either whole or cracked. The taste was good, it will taste like whatever grain you use. But you will not get a big slice like store bought bread, and it will have a heavier, more pound cake like texture.
Cool, thanks.
I work in an organic bakery and we mill organic whole grains. Pretty simple, Google around.
And lol, you’ve never tried a low fat diet and yet you think you have relevant opinions? Fat absolutely causes insulin resistance and diabetes, it’s proven by the fact that billions of cultures eat a high carb diet without suffering from that disease. In that context it is still not carbs that cause inflammation but fat causing inflammation and resistance to insulin.
Go high carb, low fat for a few months and change your life. Seriously.
Zach, you must live somewhere in California or NY if you have access to freshly milled flour goods, good for you. It’s not as common as you think, lol. I googled it, but didn’t find any places. You need to get out from your bubble more often.
I’ve actually tried low fat vegetarian (with fish) diet for a year, so I’m sorry if my opinions offend you. If fat caused diabetes, I’d be dead by now because fat is almost all I eat, lol. Yet, as I type this, it is a clear proof that I’m not dead and my inflammation is almost zero. So may be it’s not fat that causes diabetes, but caloric access or mixing fat with carbs? But once you have it, carbs will make it worse.
Zack, There are countless examples of people reversing diabetes on HF diet, why is it so hard for you to believe?
I believe that some people reversed their diabetes on Low fat diet. The underlying similarity between LF and LC is low caloric intake that leads to weight loss.
Keep an open mind, perhaps your way is not the only way.
I beg to differ that carbs will make your diabetes worse once you have it. I have it, I made my diabetes better doing low carb high fat and have now switched to low fat high carb and my diabetes has improved a bit more. I think the combo of carbs and fat is the culprit it also depends on how damaged your metabolism is. When I started low carb high fat I could not have done low fat high carb, but with the improvements I made I now can do high carb. There are so many things it depends upon. There is no once size fits all.
Rebecca, I agree, one size doesn’t fit all. I meant to say that keeping eating high carb diet while eating fat, basically not changing anything, will keep blood sugar high and your diabetes worse, requiring more and more insulin.
As I’ve said, some people can improve their diabetes on LCHF, some on LFHC, but both seems to reduce their caloric intake and lose weight or reverse insulin resistance.
I live in minnesota…
I feel really sorry for you that you have to eat almost exclusively fat to avoid diabetes. That must suck hard. And no, not a single soul cures themselves of diabetes by not eating at carbs, that is just a band aid for a much bigger issue. For instance, I eat 500g++ a day of carbs but if I eat an extra 200g of fat a day I don’t die of blood sugar poisoning. If you ate your diet and added in 500g of carbs, you might. That’s a big difference. Insulin sensitivity is of utmost importance to health. Eating vlc just means you are very insulin resistant, that is not reversing anything.
Zach, why do you keep jumping to conclusions??? I don’t have diabetes, neve had it either and I love my high fat diet. I love stake, eggs, cheese, butter and bacon, so don’t feel sorry for me now, feel sorry for me when I ate beans, broccoli, sprouted bread and was avoiding rib-eye stake for a year of being a vegetarian.
Btw, What’s that bigger issue that LC diabetes cure causes? Lots of diabetics improved their health on LCHF, it’s well documented, again, why so hard to believe?
I eat mostly LC, but occasionally pig out and eat lots of carbs, not 500, I can’t eat so much and why would I want to? but 100-200 and I’m fine. I’ve had a pizza on occasion and didn’t go into a carb coma. As a matter of fact, just last weekend I probably had 150 gr of carbs for dinner and still alive.
It’s fasting insulin that matters… Mine is 1.8. What’s yours?
No idea on fasting insulin and no need to find out. I’m a glucose storing and burning beast!
But I *have* tried a low fat, high carb diet, and it was the absolute worst thing for me. As Anna said, a low fat, high carb diet can make people- (at least some of us) constantly hungry. This is a sign of possible insulin resistance. In my own case, I had to eat very few calories (which eventually led to anorexia) to keep from gaining weight. So, Zach, I would not recommend your diet willy-nilly to everyone! I personally turned my health around by going low carb high fat. I eat far more calories than I did before, in other words I’m sated, and I’m thin. In addition to that, fat absolutely does not cause insulin resistance (at least not for me). As I said, I’m healthier than I ever was before. and I’m much older now, so that should count for something….. Your way may work for you, but it does not work for everyone.
There are a couple of ways that “carbs” can be inflammatory that I know of:
– Fructans. A whole lot of Northern Europeans don’t digest fructose very well (although we are generally better than most of the world at lactose). So SOME carbs are high in fructans, which is where wheat, onions, sunchokes, fruits, sugar, and a few other items come in. The undigested fructans end up feeding yeast mostly, and that makes for bloating and Candida overgrowth. Rice and many other grains, oddly, do not contain fructose (they are based on glucose). In traditional Japanese recipes, the “sweetener” is usually rice syrup, which is glucose, not sucrose.
— Iron. A lot of carbs in the US have added iron. The iron is quite inflammatory.
— Some whole grains have substances in the husk that don’t get along with everyone. Fermenting does help with that. But some things … like the arsenic in brown rice or the WGA in wheat … don’t ferment out.
— Rancidity and mold. Whole grains esp. can go rancid easily. Unless you store grains carefully, they tend to be pretty rancid and often have a fair bit of mold. The mold has caused some interesting historical times (like witch hunts). Grain mold is a big issue with farm animals and a big cause of birth defects. Most of what you eat is pretty well handled, but there seems to be some amount of mold residue in all grains.
There are similar issues in tubers. Potatoes have solanine. Taro can be toxic if not handled correctly. Tapioca too.
I kind of think some of the logic behind the “rice diet” was just that it avoided the toxic features of some of the other foods. If you were trying to cure kidney issues, you’d want to avoid proteins in general, but also all those toxic things that the kidney filters out.
One thing about eating a “fresh vegetable” diet is that when vegies are moldy or wilty, you’ll notice it! Same with meat … if the meat is old, your nose knows. Fish … wow, old fish is so obvious. But ground flour or meal? How can you tell?
heathertwist said: “Some whole grains have substances in the husk that don’t get along with everyone. Fermenting does help with that. But some things … like the arsenic in brown rice or the WGA in wheat … don’t ferment out.”
I doubt it’s helpful for healthy individuals to worry about cooked WGA. There’s no known evidence of cooked WGA being harmful.
Also, take a look at this:
Sounds like WGA might be rather good for you, don’t you think?
I don’t understand why many here are orthorexic about cooked WGA. It’s like people are trying to find things to worry about without.
To all involved in the “wheat debate”- I thought this post was interesting, as it explains some of the cultural biases of various time periods:
http://www.montignac.com/en/the-history-of-man-s-eating-habits/
If Duck seemed like a grain apologist before, his comment below (at post bottom) removes all doubt.
We very poorly understand the biological behavior of phytochemicals–much less than vitamins and minerals: http://lpi.oregonstate.edu/mic/dietary-factors/phytochemicals
Furthermore Duck cites a link straight out of Big Agra–rife with conflict of interest–to back up his claim. Two of the four leads for that paper he cites, “Whole Grains: Definition, Dietary Recommendations, and Health benefits” work at the General Mills Bell Institute. Gee. How could you expect them to craft their grains message? These people won’t bite the hand that feeds them.
Bottom line, neither Duck nor anyone else can furnish any true science on the effect of phytochems in the human GI tract and serum. No true mechanistic-level studies exist that demonstrate how these very many–estimates range from 1000+ to 5000–and mostly large compounds are supposed to affect our health. The CW on phytos has been that many are anti-oxidants and serve to neutralize oxidants in our bodies. We have no in vivo evidence to show how these compounds actually survive the trip through our GIs, through a powerfully acidic and hostile stomach chamber, and into the small intestine. No-one know what happens to those phytos that survive the trip–many of them quite large, 40 and more carbons long–once they finally arrive to the duodenum, Nutrient Digestion Central. Many phytos are simply too large and too weakly polar to simply enter and travel effectively through our serum. What happens to these phytos in the duodenum? Do we load them onto chylomicrons and send them into our system via the lymph? Do we enzymatically break them down into other components? How much of their vaunted anti-ox properties survive to that point? No-one’s determined this. A more recent hypothesis on phytos suggests they can have a *hormetic* effect–meaning to provide stress stimulus to our bods so our own bods generate their own anti-oxes. Mark Sisson discusses the hormesis idea here: http://www.marksdailyapple.com/hormesis-how-certain-kinds-of-stress-can-actually-be-good-for-you/
The hormesis idea makes sense when you consider the idea that phytochems evolved to help plants repair and defend themselves. Plants can’t get up and hide in a cave to avoid the sun and the creatures that want to eat them. These anti-oxes may well help the plant recover from day-long uV exposure and limit the amount–e.g. by presenting unpleasant-tasting bitter glycosides–that animals graze on it.
All questions above, we’ve eaten plants for millions of years, so I’m quite willing to accept the idea that some phytos help our health. For the moment let’s assume they *do* benefit us. Are grains truly a good source of them? The evidence so far suggests NO. Grains may even be a particularly *poor and narrow source of phytos.* Let’s go back to that Oregon State link: http://lpi.oregonstate.edu/mic/dietary-factors/phytochemicals
There, you find the researchers break out the phytos into a dozen broad categories: carotenoids, chlorophyll/-phyllin, curcumin, fiber, flavonoids, garlic, indole-3-carbinol, isothiocyanates, lignans, phytosterols, resveratrol, and soy isoflavones. For each of the dozen phyto classes, you’ll find a Food Source link. (>Sources>Food).
Of those dozen groups, grains figure prominently and broadly in only ONE of them: fiber. Certain grain products are also high in lignan (in rye) and phytosterols (wheat germ and bran). In those three categories, however, you find plenty of non-grain foods that fare as well or even better than grains.
Phytochems are not new to us. We’ve heard about their purported health bennies since at least the 1980s. When I began my foodway journey in 2007, I naturally looked at them at that time, and have tracking them since. For Duck to suggest I limited my nutrition approach to “USDA Nutrient Database + spreadsheet” is patently ridiculous. It’s yet another case of him assuming something I didn’t say. I created the spreadsheet in 2007 precisely because our authorities relentlessly propagate the pro-grain dogma, telling us we need to eat loads of “wholehealthygrains” for us to stay healthy. I needed to prove to myself that we could in fact, get all our vitamins and minerals from non-grain foods. But of course I didn’t stop there. I’ve always eaten a wide variety of non-grain plant foods. Especially brassicates (e.g. broccoli, brussels sprouts, cabbage, kale), which offer an uncommonly rich and varied assortment of phytos as you can see in that Oregon State site. As far as Duck’s claim that the spreadsheet + USDA Nutrient Database approach is “… what his anti-grain books told him to do…” he extracted that notion out of his derriere. I challenge Duck to find anyone anywhere who recommended that approach. He simply can’t find that. Certainly not in any “anti-grain” book.
Duck writes very well, presents a facade of credibility, and offers interesting ideas to follow up on, esp the questions around fortification. But I’m afraid he’s given so much logic fail and flimsy and even risible evidence to support his claims, I must take what he writes as ideas–occasionally excellent ideas–and nothing more. That’s something at least. But at this point I have to ask: who pays Duck to propagate his pro-grain message?
Here’s that Duck comment: “Wbryanh recommended that one can create a USDA-based spreadsheet and he found he could easily get all his micronutrients (vits + mins) without eating a single grain. However, this approach is rather antiquated and shortsighted (not his fault, it’s just what his anti-grain books told him to do) as it assumes that the health benefits of whole grains are merely due to their basic nutrition profile. Unfortunately, that’s not the case. The health benefits of whole grains are actually believed to come from the phytonutrients that aren’t listed in the USDA database.”
“I’m afraid he’s given so much logic fail and flimsy and even risible evidence to support his claims, I must take what he writes as ideas–occasionally excellent ideas–and nothing more”
wbryanh, I’ll politely ask you to refrain from this kind of argument from fallacy. It seems like in every comment you make an effort to insult my intelligence, simply because you disagree with what I’m saying. Please stop it. We can agree to disagree, but such insults are unnecessary.
Duck, I honestly feel you are an intelligent person. Which is why it surprises me you often offer really quite poor evidence to support your claims. I labored with that disconnect for a while, and finally had to start wondering if you are a paid shill. No other answer jumps to mind at this time.
wbryanh: “Duck, I honestly feel you are an intelligent person. Which is why it surprises me you often offer really quite poor evidence to support your claims.”
Jesus. You just can’t stop with the insulting fallacies. This time it’s Argument from personal incredulity and Argumentum ad lapidem.
How many times do I have to ask you to stop?
wbryanh: “I labored with that disconnect for a while, and finally had to start wondering if you are a paid shill. No other answer jumps to mind at this time.”
Unbelieveable. Now you’re using a genetic fallacy.
I asked you politely to stop and you just hurl fallacies back in my direction. I don’t know what else to say.
For the record I have no conflict of interests. A shill for the grain industry would not be against fortification, which is widely supported by the 13 major grain lobbyists.
I used to be low carb and bought into the anti-grain propaganda after (processed) carbs made me quite sick. At first I felt great, but after almost a year I got even sicker from low carb dieting. It was horrible. Through my own experimentation I regained my health through the Perfect Health Diet and then made even greater health improvements by slowly incorporating real whole grains and legumes back into my diet. It wasn’t the carbs that made me sick, it was the processed and refined carbs that made me sick. You could say I’m post-low carb now.
So, please stop, wbryanh. We can agree to disagree. You don’t have to insult someone just because you have an personal incredulity. That does not give you the right to insult me. I think you don’t even realize you’re doing it.
Duck, do you mind sharing what you mean by “after almost a year I got even sicker from low carb dieting. It was horrible.” What symptoms/issues did you have? I’m honestly interested as I’m always watching out for side effects, as we are all doing our own personal dietary experiments. Thanks.
Anna, I’d be happy to. On my processed SAD diet I was very thin, but had lifelong brain fog, psoriasis, rosacea, dandruff (probably due to candida or some kind of dysbiosis). After going low carb I felt quite good, but I quickly lost 10 pounds that I didn’t need to lose and began to look like a crack addict. Everyone was worried about me. Within a few months panic attacks started and then I lost the ability to fall asleep. My sympathetic nervous system was shot and stress hormones were taking over. I was a mess. My short term memory worsened considerably—I could turn the stove on and forget about it 2 minutes later. It took a lot for me to finally admit that the low carb was the wrong choice for me. My guess is that low carb worsened my candida (I later learned that some candida can thrive on ketones).
And so I began to research the potential benefits of carbohydrates. I learned about resistant starch and began experimenting with increasing fermentable fiber intake. Improved sleep and amazing dreams happened quickly. I began to feel relaxed again (our gut flora create our calming GABA and other neurotransmitters). My memory improved slowly but surely. I solved my candida issue with PHD and other therapies—and for the first time in my life the brain fog lifted and then disappeared over many months. It was incredible.
Over time I learned to incorporate real whole grains and legumes into my diet. Today, I can eat plenty of real whole wheat and my skin stays supple and smooth. If I eat enriched flour, I get a bit of dandruff and rosacea. I didn’t get dandruff or rosacea while eating a good amount of white flour in France—which is how I realized that fortification and flour adulterations might be what was problematic for me. France forbids those impurities in their traditional breads. I began digging into the research and found that indeed fortification may be responsible for some health problems.
Duck, thanks for sharing. Interesting about fortification affecting your health.
Also interesting about your sleep as well. Perhaps it was also a magnesium deficiency and not just a lack of fiber/carbs effect? Greens, beans and grains are very high in magnesium. And magnesium is very important for nervous system as well. It also improves memory and helps panic attacks.
Duck Dodgers- that was interesting about your health journey; now I understand a bit where you are “coming from”- (not that there’s anything wrong with that; I have some relatives who tried eating low carb, had a few similar problems, then tried the Perfect Health Diet, which they say helped them a lot). I, myself, seem to do well on low carb. I would like to respectfully mention that I think the “resistant starch” issue has been over-hyped. I’m not sure that it’s important for everyone. Obviously, your own n=1 tells you it’s good for you. The point is, the study of the microbiome is so new, it’s in it’s “infancy” really; we just don’t enough about it yet. The main reason resistant starch has been touted as being healthy is that we happen to know quite a bit about it. However, there may be other compounds in other foods that we don’t know about yet. Only some gut bacteria have been identified, but there’s a whole world out there that we still know nothing about! Not only that, but the microbiome is a whole ecosystem, so what’s most important is not certain bacteria (at the expense of others), but the right balance of bacteria. This will vary from person to person as well. As some have pointed out, there aren’t that many sources of resistant starch in nature, so some of our hunter gatherer ancestors would have had trouble getting it. (And potatoes are quite new in our diets). I, myself, don’t do well with grains; they actually mess up my digestion horribly, so it’s obviously not helping my microbiome any! I think eating other types of fiber can be just as beneficial. Each person has to find what works best for them, and I think basing it on how you feel can be a pretty good marker.
I agree, Morgana. I don’t think it’s particularly helpful to catalog your microbiome when we barely understand what the various species do (which may indeed be a fad). But there’s of course evidence that the microbiome can effect health in ways we don’t fully understand. There seems to be value in feeding the microbiome something. I don’t think it’s a “fad” to eat fibers. Most indigenous cultures are known to eat considerable quantities of fiber (Hadza for instance). I doubt they do it out of boredom—otherwise it would be a waste of time and resources. Probably makes them feel good.
Duck- I totally agree, the microbiome can affect health in various ways, some of which we are just barely beginning to learn about. And I agree that eating some plant foods and fibers are not a “fad”, but probably good for us. Just for the record, I do eat plant foods- probably more than many- but I stick to the ones I can digest well. Resistant starch is a problem for me, generally, so I probably don’t eat that much of it, and I eat low carb mainly because it’s very good for my digestion. I don’t eat much in the way of potatoes- (occasionally a small amount, that’s all I can tolerate). And as I said, potatoes are a relatively new food. I do eat nuts though, and I think some of them might have resistant starch? (Like cashews: do they have resistant starch? Or almonds? If so, then I do eat some of it).
Duck, Morgana, just wondering. Where does it say we should eat amylose-based resistant starch–like that from potato starch and bananas/plantains–to properly nourish our SCFA-producing gut flora? Where does it say there are no other types of fiber–like those found in leafy greens, colored veggies, fruits, lower-carb root veggies like carrots, and anything else that’s naturally without gluten–that can adequately nourish these SFCA-producing flora? Do grains offer any type of fiber unique to grains that nourish these SFCA-producing flora?
I haven’t been able to find any clear info on any of this. Thanks for your thoughts, ideas and links. –Bryan
wbryanh- I don’t think it *does* say anywhere that we *need* to eat resistant starch! However, a lot of bloggers- (many in the Paleo world, for instance)- started experimenting with resistant starch, then started blogging about it; this is why I called it a “fad” in one of my earlier posts to Duck Dodgers. These are basically “laypeople” who recommend it- (though I respect many of them, for other reasons). Most of the experts who study the microbiome tend to be more cautious, i.e., saying that we need to learn more before we tell people to radically change their diets. But, yes: you basically vocalized my own thought, that other types of fibers may be equally beneficial, and resistant starch may not be necessary. That doesn’t mean that it’s not beneficial for some! My own theory is that how we feel about what we eat probably determines what’s best for us as individuals.
Nowhere does it say we “need” to eat RS. However the research does say that if you wanted to maximize your SCFA production (a big if), you’d almost certainly have to eat RS in order to do it. Many of the non-starchy fibers, like cellulose, just don’t ferment into very much and few very people have the flora to ferment cellulose in the first place. On the other hand, Inulin can be found in dandelion greens, and it is a very powerful fiber. But of course, inulin doesn’t ferment into all SCFAs, so you need a few different fibers to get the full spectrum.
Whether we necessarily need to maximize our SCFA production is another question altogether (I don’t have the answers for that), but suffice to say, many cultures seemed to have had high SCFA production.
A general summary of that research on RS can be found here. I used to supplement with RS and it definitely saved me from the problems I was having. But, I don’t supplement anymore, I just eat real foods now.
Keep in mind a fiber is only fermentable if you have the right flora in place, (why cellulose isn’t considered a MAC), so your mileage may vary depending on which fibers work best for you. For all you know, you may do excellent on dandelion greens and jerusalem artichokes rather than starches. Everyone’s gut is different, and it is possible to modulate your gut over time.
Thanks Duck. Dandie greens seems to work well for me. I’ll forage them from forest duff near my house and make salad with a tin of sardines, fresh garlic, sprouted sunnies, red pepper flakes, a little apple cider vinegar, and juice of a half a Meyer lemon. Oh and some grated pecorino. Delicious and my GI feels good and and BGs usu do really well. So there’s my little n=1.
I’ve been looking for a list of all the diff fibers, what foods you find them in and in what quantities (per 100g), which gut flora they feed, and the fermented products these flora produce. I’ve found putative fiber/food efforts, like this: http://www.webmd.com/diet/compare-dietary-fibers and here:
https://en.wikipedia.org/wiki/Dietary_fiber#Types_and_sources_of_dietary_fiber But nothing that matches the fiber to the flora to the fermented products. If anyone has links for that, that’d be great. –Bryan
Bryan, I’ve seen the different fibers-to-SCFAs before but can’t remember where, offhand. I’ll see what I can find. But, if I remember correctly from the n=1s, the people who did VLC often had poor results from RS. My guess is that due to the lack of starch in their diet, they just didn’t have the biome to process it and they pooped most of it out. Makes sense.
Interestingly, your body will intentionally persorb a finite portion of all fibers into the bloodstream where they may (or may not) have the ability to bind up various free metals or whatever else. Nobody really knows what goes on there, but it’s the same mechanism that brings phenols and antioxidants into the bloodstream as well. All fibers, phenols, antioxidants are just xebobiotic glycans (could be hormetic as you say…nobody knows).
I wouldn’t worry to much about getting the full spectrum of fibers. There are some studies which have found that using just a single fiber can create far more floral diversity than a variety of fibers can.
It’s paradoxical, but makes sense if you think about it. When you have a single fiber, just a few species might grow. But soon species that feed off of the metabolites of the first species (i.e. cross-feeders) begin to flourish from the steady supply of metabolites. And then, perhaps, more species that feed off the metabolites of the second generation of species begin to flourish (cross-cross feeders?) and so on.
It’s sort of like growing a crystal or a snowflake—it gets more complex so long as the foundation is stable.
So, you see, someone who relies on one or two staples (maybe just potatoes like the Irish, or say baobab and a few tubers like the Hadza) likely may have more flora diversity and SCFA production than someone who tries to eat a wide variety of fibers. This might explain why the Kemper protocol worked just fine for those who needed it.
This just goes to the earlier point that there’s so much we don’t know. So, I probably wouldn’t stress about getting all fibers if you’re already doing well with certain fibers. You might be better off sticking to one or two fibers. Nobody really knows.
Thanks for all this Duck, and no rush on those links. I have no GI issues or anything else to resolve at this point, but it remains a big academic interest. About the Microbiome Project, we are at the very beginning of what will likely be an incredibly rich study, like the genome project. Btw that single-fiber idea, with the blooming of gut flora diversity on the potato diet, that’s very interesting. Another example to suggest less can be more and for us to get out of our own bodies’ ways. –Bryan
My pleasure, Bryan.
I found this paper showing SCFA levels from non-starch fibers:
A comparative in vitro evaluation of the fermentation properties of prebiotic oligosaccharides (2001)
Obviously, the results of the comparison only apply to flora that are already in place to ferment these polysaccharides. So, everyone gets different results, which are modulated over time. In other words, if one was a germ-free mouse, they’d obviously get zero SCFAs from taking these fibers.
That paper doesn’t compare with RS, but RS is known to produce a LOT of butyrate. However, again, one typically needs to have a diet high in starch to possess the RS gut bugs for fermentation—otherwise it would just be like eating sand, the RS passing right through you mostly unfermented due to lack of RS-degrading flora. You could change this over time, but it might be best to stick to one or two fibers, preferably from real, whole foods.
Fecal butyrate levels vary widely among individuals but are usually increased by a diet high in resistant starch (2011)
You get the idea. I have seen studies generally comparing the fermentation levels of RS and other non-starch polysaccharides, but I think you can get the idea from this.
Thank you Duck–very much what I’m looking for.
I wonder if some species of flora will ferment multiple types of fiber? Are there species that ferment RS plus fiber from various low-carb foods too? Reason I ask, you say this:
“…one typically needs to have a diet high in starch to possess the RS gut bugs for fermentation…”
Yet when I started the potato starch in ~ 2012, it was already five years being VLC. The very first time I consumed it, my GI, my whole bod felt really really good and calm. And I never experienced GI upset except maybe a little at 4TB/day.
At that time (and now), I eat fiber from various sources, avocado, coconut, various leafy and cruciferous greens, artichokes (including all the leaves), citrus (including the skin)… –Bryan
Bryan, as for which species inulin tend to modulate, this paper may be of help:
Inulin-type fructans modulate intestinal Bifidobacterium species populations and decrease fecal short-chain fatty acids in obese women. (2014)
I really don’t pay much attention to the species though. So, my apologies if this isn’t helpful.
Duck, interesting, thanks again! Btw, I’m not immediately seeing how higher fecal SCFA concentrations somehow suggest higher metabolic risk. Aren’t colonic SCFAs a good thing?
I wonder if there a comprehensive list of the ferments our flora generate? Will keep googling that. –Bryan
Duck, this from you : “…inulin doesn’t ferment into all SCFAs, so you need a few different fibers to get the full spectrum…”
Do you know which flora inulin feeds, and which SCFAs those flora produce?
That’s the kind of info I’ve been looking for for years. Thanks –Bryan
Oh.. and, of course, some modern gut issues, like SIBO, may have issues with some fibers (FODMAPs, RS, etc). So, obviously this is not a blanket recommendation for everyone. Although some people have claimed to have cured their gut issues with fibers—supposedly the fibers may pick up and sweep away bacteria back into colon where they belong. But that’s one of those n=1s that might not work for everyone. Again, YMMV.
For me, I seem to thrive on RS, so it’s now eggs and toast for me in the morning (toasting bread is said to significantly increases RS3 in bread).
Guys FYI: http://lpi.oregonstate.edu/mic/other-nutrients/fiber#introduction
One of the better breakdowns I’ve seen of dietary fiber types and the plants you find them in. Alas, that’s not saying much.
And still no links to the flora these feed and what ferments those flora generate. –Bryan
DIETARY FIBER
Lignin: Lignin is not a carbohydrate; rather, it is a polyphenolic compound with a complex three-dimensional structure that is found in the cell walls of woody plants and seeds (7).
Cellulose: Cellulose is a glucose polymer with β-1,4 glycosidic bonds found in all plant cell walls (see Figure 1 above) (6).
β-Glucans: β-Glucans are glucose polymers with a mixture of β-1,4 glycosidic bonds and β-1,3 glycosidic bonds (see Figure 1 above). Oats and barley are particularly rich in β-glucans (7).
Hemicelluloses: Hemicelluloses are a diverse group of polysaccharides (sugar polymers) containing six-carbon sugars (hexoses) and five-carbon sugars (pentoses) (6). Like cellulose, hemicelluloses are found in plant cell walls.
Pectins: Pectins are viscous polysaccharides that are particularly abundant in fruit and berries (4).
Gums: Gums are viscous polysaccharides often found in seeds (4).
Inulin and oligofructose: Inulin is a mixture of fructose chains that vary in length and often terminate with a glucose molecule (8). Oligofructose is a mixture of shorter fructose chains that may terminate in glucose or fructose. Inulin and oligofructose occur naturally in plants, such as onions and Jerusalem artichokes.
Resistant starch: Naturally occurring resistant starch is sequestered in plant cell walls and is therefore inaccessible to human digestive enzymes (4). Bananas and legumes are sources of naturally occurring resistant starch. Resistant starch may also be formed by food processing or by cooling and reheating.
Guys, my n=1 on resistant starch, I got terrific results in the very beginning, and then quickly sloped off to zero after a few times eating it. I started with Bob’s Red Mill unmodified potato starch (easy, cheap, near-zero carbs), initially 1TB/day and then worked up to 4TB/day. The very first time I tried it, it suffused me and my GI with a wonderful sublime calm. I’ll never forget that. But then that was it. I experienced no dramatic effects after that, either in how I felt and in my BGs.
Morgana, along the lines what you said”…there aren’t that many sources of resistant starch in nature…” after the potato starch stage, I started to experiment with very green banana and raw potato (some feel bananas originated in India). In both cases I could eat ~50g per meal without unduly popping my BGs. I continued to feel no different. It’s almost like a needed a prebiotic “top-off” and then that was it.
And I agree with you Morgana about the complexity of our microflora and how little we understand what they do and especially how they interact. Here Michael Pollan delves into the intrigue, promise, complexity and unknown:
http://www.nytimes.com/2013/05/19/magazine/say-hello-to-the-100-trillion-bacteria-that-make-up-your-microbiome.html?_r=0 –Bryan
wbryanh- Interesting! I never caught on to the “potato starch” bandwagon; I was always skeptical of it, since for me, potato starch just doesn’t seem like a real food, but more like a supplement. (And I assume it’s relatively processed; at least, it resembles a flour, not something I’d want to eat necessarily). But yeah, basically, some of our ancestors might have had access to resistant starch, but certainly not all! (How many cultures had access to bananas? Some, but only a few). Some people had access to plantains, some to manioc…..potatoes are a more recent food…..so, yeah…..I’m just not sure that resistant starch is necessary for all. I suspect that the foods that are “beneficial” probably vary, depending on the rest of the diet the individual is eating. There are some groups that ate very few plant foods- (not just the Inuit; but also the Sioux Indians, I believe also the Mongolians)- and they seemed to thrive. In any case, for me most foods with resistant starch don’t seem to be the foods that I can digest well. (Unless nuts have resistant starch, I think some might). Based on what I’ve read, it sounds like fiber is very important for people who need to live off of a lot of plant foods, as the gut microbes convert the fibers into by-products that in turn “feed” us. But, if you’re eating a more carnivorous diet, this might be less necessary, as the nutrients are readily bio-available in those foods, we don’t need to make the conversion. (I think Dr. Eades writes about this on his blog….or maybe it was Dr. Eric Westman, I might have that confused…..maybe both?).
Hi Morgana. My RS experiment stage, it was a while back when Sisson, Kresser, Nikolay, etc were all glomming onto the wonder “butyrate-spawning-monster” potato starch. So I trying to recall the details of my program, what I did. Honestly, I decided to try RS it because of Sisson. But certainly I had your same processed-product concerns. I decided I’d take PS it just for a very short time, just to see what happens. I did quickly move to the more natural RS sources, but like you say, potatoes at least weren’t paleo/ancestral. My general approach, given our overwhelmingly complex modern world filled with novel products, is that *less is more.* The less done to the food from when it’s conceived to when I get it, the better. The more “heirloom” (meaning less selective breeding) the better. However I started my nutrition and lifestyle journey in 2007 with a quite deranged metabolism, and so accept the idea that selective limited temporary application of non-natural products might help correct me. E.g. I took supplements from 2007 to 2009 before I scaled them down and then stopped all of them. Morgana thank goodness I’ve arrived to a state of health that, for several years now, I haven’t felt I needed any more interventions! –Bryan
Duck, let’s stick to the issue at hand. I’m pointing out where your evidence is poor, and *provide evidence* to support that. In this forum I have done so already many times now. When I question what you say, I *provide evidence* to support what I say. Anyone who cares to search our names in this forum will see I do that. I have always been willing to engage with anyone who questions what I say and the evidence I cite. This is called healthy debate. It’s exactly the kind of thing we should see and engage in here. I am sorry if you feel that when I question you–or when I defend myself again your comments which some people may well interpret as being condescending and insulting to me–that you take that as an insult and a personal affront. Yet I am not entirely surprised. When I questioned grains, you considered that “grain bashing.”
Duck, I am certainly not invalidating your personal experience. I’ve heard a number of success stories with the Jaminets’ Perfect Health Diet. And to remind you, I do feel we align in a number of nutrition areas. I hope I’ve made it clear I feel you offer valuable things here. But I *will* continue to call bullsh*t when I see it.
As will I, wbryanh.
As will I.
Thanks for the interesting and detailed information.
As for dropping grains … well, I do eat them, mainly white rice because I like it. But I will say, if I had to grow all my own food (like the Japanese mountain people) I’d go for tubers! It amazes me that most of the world actually started growing grains at all. I do a fair bit of food-growing, and I did put in some amaranth, sorghum, even wheat at one point. Also I do lots of potatoes and sweet potatoes and taro.
Grains are DIFFICULT.
1. They are quite sensitive to water levels. One drought wipes out the crop. Tubers store their own water.
2. You have to get rid of all the weeds to get the plant to grow. Tubers will usually grow in the middle of a mess of weeds, and kind of take over.
3. You have to harvest them at just the right time or they rot. Tubers you can usually leave in the ground til you are ready to eat them.
4. After you harvest the grain, you have to beat it, de-husk it, grind it, ferment it.
5. Then you have to keep it in a super-dry environment or you get toxic mold.
I can totally understand why hunter-gatherers would gather some grain heads and eat them. But why they started *farming* them is beyond me. I expect some of it is financial. You can store grains in silos for years. Like gold. So you can hoard grains and dole them out during famines. Another answer might be “ethanol”, although you can make decent beer from tubers too, and certainly from fruit.
Our ancestors weren’t really looking at tables about nutrients. It was more like “this tastes good” or “this makes me feel good”. Somehow the grains won out, in much of the world. Like I said, this floors me. I just don’t understand it. The tuber-eaters seem to have done just fine historically, but they swap and do grains if they can.
Heathertwist, you say “But why they started *farming* grains is beyond me. I expect some of it is financial. You can store grains in silos for years.”
Heather I feel what you suggest–selling/bartering of excess, storing for lean times–is a lot of the reason. Grains literally did civilize us by allowing us to engage in widespread food production for the first time, and to do it remaining in one place. We finally could start to develop towns and cities and amass belongings including documents when we developed the first writing systems 5000+ years ago. Jared Diamond discussed the many ramifications in one or more of his books maybe “Guns, Germs, and Steel?”
You say “Somehow the grains won out, in much of the world. Like I said, this floors me. I just don’t understand it. The tuber-eaters seem to have done just fine historically, but they swap and do grains if they can.” Interesting isn’t it? My thoughts: we started growing grains in or near the Fertile Crescent, which stretches roughly from Cairo region in Egypt to modern-day Iraq. Jared Diamond talks about the relatively low natural barriers on the Eurasian continent that allowed wheat and barley to spread far and whole. The runaway most popular tuber, the potato, comes from South America, and explorers brought back to the Old World less than 500 years ago.
About what you say “Our ancestors weren’t really looking at tables about nutrients. It was more like “this tastes good” or “this makes me feel good” we may well find actual chemical properties peculiar to wheat to make us prefer it over other starchy plants. http://www.ncbi.nlm.nih.gov/pubmed/6099562
Dr Davis dwells on the presumed opioid properties of some gluten metabolites in his book “Wheat Belly.” But please don’t rely just on him for info on the topic! –Bryan
Yes, I think there is something to the opioid issue. A lot of foods act like drugs … coffee and chocolate come to mind. They are beginning to find more hard evidence that non-celiacs still have brain changes when they eat gluten.
“95 adults in the U.K. were picked to go gluten-free for three weeks, then go back to normal for another three weeks.When they were gluten free, they got fewer cramps and stomach discomfort, but they also picked up a sharper mental focus because they were less fatigued. The researchers think this is an important breakthrough in the study of how gluten affects us, and our brainpower.
They said: ‘The fact that they were able to start tasks quicker, concentrate better and think clearer during this time, and felt the need to rest less, all point towards the idea that sensitivity to gluten does exist for some individuals who don’t have celiac disease.””
http://www.aol.com/article/2015/12/02/going-gluten-free-could-boost-your-brainpower/21276724/
I’m not sure exactly what factor in wheat causes this though … there is still the FODMAPS thing and the WGA and all the other stuff.
Anyway, for rice I’d think yes, it might be about storage and civilization. Pretty much all the anthropologists agree that “civilization” began with grains of one sort or another. The South Seas Islanders, for instance, didn’t bother with grain, but they also never did large-scale cities or armies etc. But the exceptions are kind of interesting. The Japanese mountain people in Yuzurihara grow only tubers, because the land is too steep for rice. And they are said to be the healthiest of the Japanese.
And interestingly, after living off tubers for a week or three, I still couldn’t give up my rice! The yams and potatoes tasted great, but they don’t have “the thing” … maybe the sheer concentration of calories is what the body is after too.
Anna said: “Even if properly milled fresh non-fortified whole grains are healthy, don’t you think it’s a moot point because they are simply not available to americans? As you were saying, even whole wheat flour/bread is not really whole wheat, so what’s the point? Nobody is going to mill grains at home… Isn’t it better to avoid it all together then?”
Yes, you have a point. I’m not a fan of industrial flours. The French do OK (i.e. good for a Western nation) with their unfortified white flours and strict purity laws (decret pain) and better milling standards.
However, you can find whole wheat berries in any high quality American supermarket—including spelt and farro—for porridges, salads or grinding. In New England it is possible to find gristmill flour—I believe there are still a dozen or so gristmills operating. I believe even Whole Foods sells some gristmill flours in those states. They are excellent. Home grain mills are becoming more popular and are quite good (see them on Amazon). Some people even using coffee grinders to grind their wheat. Anecdotally, I’ve seen some people suggest that the wheat they grind at home is more tolerable than industrial wheat, which does not surprise me. Also, there are plenty of non-wheat whole grains that are available to Americans: Quinoa, Chia, Amaranth, Farro, Kamut, Teff, Sorghum, etc.
Anna said: “have you seen any human studies that compared a whole grain Wheat diet with a diet absent of wheat and refined sugars and not nutrient deficient? How would they compare? How would whole wheat diet compare to a Low carb diet?”
I have not seen such studies. However, one of the known potential problems with low carb diets is that they can be low in MACs (Microbiota accessible carbohydrates) like Resistant Starch, which is well established as being beneficial to health.
https://en.wikipedia.org/wiki/Low-carbohydrate_diet#Resistant_starch
This is one of the major criticisms of a low carb diet. See Tim Steele’s blog for endless details on this. He’s an amazing resource.
Anna said: “I wonder, is there anything in whole grains that a grain-free diet would be missing?”
Well, it would depend on the diet, but a grain free diet might be deficient in resistant starch and other phytochemicals I mentioned in my previous comment. It would depend on what kind of grain free diet one chose. I think the interesting thing about whole grains is they make it really easy to obtain those phytonutrients. (Also, low carb diets can sometimes be deficient in manganese, which is essential for managing iron, but that’s another story and not relevant to your question about a “not nutrient deficient” diet).
Anna said: “or are these “healthy” nutrients in whole grains are only needed to “protect” the body agains the high carb content on these grains?”
I don’t think anyone has the answer to that. My sense, however, is that those phytonutrients help us maintain homeostasis in managing problematic micronutrients like iron. Phytates likely also promote this homeostasis by potentially chelating excess free unbound iron. So, I imagine they are needed, but I suspect no one can say for sure just yet. More research is needed.
Duck,
good point about whole grains for porridges and side dishes. Unfortunately they are not as tasty or convenient as buying bread 🙂 but certainly doable. And making bread at home using home-milled flour is really a time luxury I can’t afford, it’s just not worth it for me as I don’t eat enough carbs to justify the time.
I’ve seen Tim Steele’s blog and had a discussion with him, so I”m not convinced at all on the benefits of RS. I think it’s a FAD. I eat lots of vegetables, so I’m sure my microbes will survive 🙂 or adapt to my diet. I don’t adapt my eating to it, lol.
As for phytochemicals, again, I’m not convinced of their benefits, nonetheless, I eat lots of veggies, coffee, tea and chocolate, just in case 😉
Seafood for manganese and bloodletting for managing iron 🙂
But just in case I’m not missing something, I eat rice, bead or a croissant at least twice a week, I wish I could find it baked from freshly milled flour…
Anna said: “As for the vitamin B flour fortification theory, I didn’t see any evidence of that in Russia, where I’m from.”
Well, I’m still looking into it, but as far as I know, the appetite-stimulating effect of B vitamins doesn’t have to come from fortification. It could feasibly come from anything that has a taste of natural B vitamins (marmite, beer, brewer’s yeast, or yeast extracts, for instance). I assume there is something yeasty in the Russian diet. 🙂 Incidentally, bakers at the turn of the century knew that people preferred the taste of white flour made with brewer’s yeast. Same idea.
Anna said: “Flour is not enriched in Russia, yet diabetes is on the rise there as well and obesity is becoming more common.”
It’s simply a correlation that populations with fortification tend to have more obesity and diabetes. Again, it’s not my finding (it’s Zhou et al‘s)
Anna said: “Also, my remote relatives in India are vegetarians and have extremely low vit B levels, yet it didn’t affect their hunger, they eat high carb diet, are overweight and pre-diabetic.”
I think you are misunderstanding. Low vitamin B status is known to make someone more susceptible to the appetite-stimulating effect of B vitamins. So, anything rich in B vitamins should stimulate their appetite if they have low B vitamin status. If they were truly deficient and not tasting any B vitamins whatsoever, they would likely get beriberi and they would lose their appetites (as what happens with pellagra or the 19th century dyspepsia epidemic). The appetite-stimulating effect of B vitamins has been shown to happen by Osbourne & Mendel, and others, from just a small flavoring of B vitamins—it’s an innate sense we evolved with to choose nutrient-dense foods over nutritionless foods.
Anna said: “I don’t know if flour is fortified in india, I doubt that, but they eat a lot of it and have one of the highest per-capita rates of diabetes. So, I don’t think that enrichments of white flour are that consequential.”
No, fortifications are certainly not the only factor. Again, you’d have to look at the correlations examined by Zhou et al. The correlations are there, but that doesn’t mean they are exclusive. Also, diabetes may be caused by iron overload, or at least by a mismanagement of iron stores—perhaps due to other micronutrient deficiencies. So there are obviously many different ways this can happen. One does not need fortification to become obese or diabetic. Fortification just seems to promote it somehow (perhaps by simply enabling and stimulating people to eat more refined foods as staples).
Keep in mind that in India, diabetes is associated with a large shift from consumption of coarse grains to polished rice and refined wheat as well as sugars. This means that micronutrients like Manganese and copper are literally being refined out of their diets. Both minerals are required for SOD production (like MnSOD), which are our most powerful endogenous antioxidants. Without those minerals and those antioxidants, we lose the ability to manage our iron stores, and this deficiency may be what actually promotes diabetes.
We can’t easily blame carbohydrates alone for diabetes when all of these cultures are becoming more chronically diseased as they refine their carbohydrates. Some researchers believe that the increased fiber and the bitter tannins in whole grains initiate satiation signals that makes it difficult to overeat them. When you refine those satiating compounds away, you will likely eat more than you should. So, it’s obviously multi-factoral (as I’ve previously mentioned).
Duck, I realize that there is correlation between fortification and obesity, but it could be just that, a correlation and not a causation, or at least a very tiny factor. I doubt that if we stop the fortification now, obesity will go away or at least will be reduced significantly.
Also, we agree that a switch from whole grains to refined flours and sugars is party at fault, with increased iron absorption as a by product of reduced anti-nutrietns. So sometimes you clearly want these “anti-nutrients”.
We also agree that we can’t just blame the carbs for obesity epidemic. I blame wealth (and increased food intake that correlates with it) and sedentary life style.
Thanks.
“I work in an organic bakery and we mill organic whole grains. Pretty simple, Google around. ”
Zach is correct. It is pretty simple. There is an organic bakery near me and every morning they throw whole organic grains into the hopper of their mill. They press a button and a short while later later they have freshly milled flour. The mill fits into a large closet.
There are organic bakers all over the country that mill their own flours. You can even find a few in your organic freezer section. Berlin Bakery and Alvarado Street Bakery are two brands that mill their own grains and are sold nationally. (Berlin Bakery only bakes with fresh-ground spelt and they claim it is well tolerated by many who usually have problems with grains). From experience, I can say the Berlin bread definitely doesn’t have an appetite-stimulating effect.. it’s kind of dull tasting, but my kid likes it. 🙂
At any rate, if there are local organic bakers and millers in your area, then I would favor those local options over national brands.
Well, Duck, Idk, I live in South Carolina and before that in FL and there weren’t and aren’t any organic bakeries around. I guess it’s my bad luck. On the other hand, I’m tempted much less : )
Frozen bread just doesn’t have the same apeal as freshly baked, but I’ll try it out .
WBryanH said: “Furthermore Duck cites a link straight out of Big Agra–rife with conflict of interest–to back up his claim.”
Laugh. The references show what the health benefits of grains are believed to be. It’s perfectly legitimate to reference actual cereal scientists for such an opinion on what the health benefits of grains are believed to be. I suppose you’d rather I cite an anti-grain authority. lol 🙂
The point being that grains can be a good source of some phytonutrients (not all), and these phytonutrients are believed to offer grains their health benefits. For instance, γ-oryzanol found in brown rice. Or the significant amount of phenolic compounds found in barley.
Duck, you write: “…It’s perfectly legitimate to reference actual cereal scientists for such an opinion on what the health benefits of grains are believed to be…”
Hmm. You cite opinions from cereal researchers, paid by the cereal industry to write about cereal. And then proceed to imply these are unbiased views.
Um, OK Duck. You’re certainly welcome to feel that way.
Anna said: “I eat lots of vegetables, so I’m sure my microbes will survive 🙂 or adapt to my diet.”
Sure, they’ll “survive,” but low carb vegetables tend to be mainly cellulose (unless you’re eating a good amount of inulin-rich dandelion greens every day). The problem with cellulose is that much of it is not fermented, since most humans lack cellulose-degrading bacteria. You just poop most of it out (good for bulking stool though).
What’s important to understand about fiber is not just consuming it, but also having flora that can ferment it. This is known as Microbiota Accessible Carbohydrates (MAC). Cellulose is not considered to be a MAC because of the lack of cellulose-degrading microbies in humans.
And even if you did have cellulose-degrading flora, cellulose doesn’t really ferment into beneficial SCFAs very well. But hey, as long as you’re aware of the research, do whatever makes you feel good!
Duck, I eat some inulin-rich and other digestible fiber veggies like onions, avocados, apples, cucumbers, carrots, mandarines, sauerkraut, tomatoes, etc. I eat them because I like them. I don’t eat a lot of it, but I eat lots of butter and olive oil, so I’m sure some of it makes to SCFA.
Anyway, my microbiome hasn’t complained so far 🙂
There is no consensus on how to feed or not feed our microbes by the way. We don’t know much at all about it. Many people have lots of problems with veggies. My theory is that a healthy micro-biome adjusts to what we eat. I seriously doubt that our human ancestors were eating lots of vegetable in winter and worried about it. And IF seems to be beneficial as well, while our microbes are totally starving.
Anyway, I don’t claim to know it all, but I feel fine with a small about of veggies.
Mandatory reading for anyone interested in understanding nutritional science and dieting. Looking forward to the next episode.
Very nice work! =)
Denise – This makes perfect intuitive sense. I’m a longtime low-carber myself but I’ve always thought is got to be the modern-day combination of both fat and sugar that is the real problem. Where, in nature is this found? I don’t know. Seems like only man-made food-like substances to me. In real life scenarios, it’s a lot easier to stay in the low carb realm rather than the low fat. Just my opinion,
“I’ve always thought is got to be the modern-day combination of both fat and sugar that is the real problem. Where, in nature is this found?”
JACKPOT!! 🙂
Corn. Follow the trail of corn, from PUFA to tortilla to fatty livestock to HFCS, and you’re on the trail that leads to obesity
Quite so – and let’s not forget the partial hydrogenates in corn oil …
Except not all corn causes obesity. The Pima indians ate nothing but corn and beans, and had no weight issues. Unless they live on the other side of the border and eat American corn. There is some argument about WHY one type of corn causes diabetes and the other does not, but it likely does have to do with how fast the starch breaks down and how the corn is processed.
I bought some “heritage corn” from a Mexican store and worked with it. It was sold in whole grains, which I ground. Even ground though, it works completely different from what you buy as “cornmeal” or “masa” in an American store.
Heathertwist- yes, modern corn has been bred to be far higher in sugar than traditional, native corn. Native Mexican and Indian corn was probably pretty healthy.
Where’s Part 2?
In other words, as far as diet is concerned, extreme is good. I hope that ends the business of pushing for a mushy middle between paleo and vegetarian.
I’m not sure that you can go there from the evidence. Another possibility is that if you wreck your metabolism, you can reset it with an extreme diet.
As a Diplomate of NLA in Lipidology and presently studying for the Obesity boards I swim through the morass of data, personal experience and what works.
All weight reducing diets are restrictive.
To find out if you have a healthy diet you need 3 tests: LDLp, CIMT, CAC
If you have no plaque and your LDLp is <1,000, I think your diet is good for you.
Most obese have Insulin resistance. I think they need LCHF.
Otherwise, eat what you like. God bless.
God I would love to see those test in an experiment of longterm LCHF and HCLF adherants.
Fantastic article, eye opening stuff. Although i think very low fat diets (under 15%) aren’t optimal from a nutrient point of view. I had a look on chronometer to see the lowest amount of fat i could eat and still get enough of everything using only real food. I ended up with 16% as an absolute minimum, although i managed to work it down to 9% using a few “food” supplements and replacements. For example, skim milk and cod liver oil. Can’t wait for the next article.
Also, i cant help but wonder if there is one more golden spot in the swamplands. Matching carb intake with physical activity. Which is pretty much the range 30-40% carbs. Which interestingly tends to be close to the amount modern hunter gatherers tend to eat. http://www.nrjournal.com/article/S0271-5317%2811%2900091-1/abstract “Hunter-gatherer diets were characterized by an identical carbohydrate intake (30%-35% of the total energy)”. They may eat up to 40% due to the glycogen present in fresh meat. Aside from the observation that many hunter gatherers were healthy not much can be drawn from this. I’m unaware of any studies that match carbohydrate intake with exercise. Although the perfect health diet uses similar guidelines and seems to have good results if the testimonials are anything to go by. I would love to see a study comparing low carb, very low fat and intensity matched carb diets.
I also found this, but i cant read past the extract. http://www.ncbi.nlm.nih.gov/pubmed/21679058 . Balanced caloric macronutrient composition downregulates immunological gene expression in human blood cells-adipose tissue diverges. However, i did find an article discussing the paper, here are some interesting quotes. https://www.ntnu.edu/news/feed-your-genes
“what if you could find out how our genes respond to the foods we eat, and what this does to the cellular processes that make us healthy – or not? That’s precisely what biologists at the Norwegian University of Science and Technology (NTNU) have done.
The answer researchers have come up with may surprise you: the best diet, from a gene’s standpoint, is one-third protein, one-third fat and one-third carbohydrates. That’s what the research shows is the best recipe to limit your risk of most lifestyle-related diseases.”
“We have found that a diet with 65 per cent carbohydrates, which often is what the average Norwegian eats in some meals, causes a number of classes of genes to work overtime,” says Berit Johansen, a professor of biology at NTNU. She supervises the project’s doctoral students and has conducted research on gene expression since the 1990s.
“This affects not only the genes that cause inflammation in the body, which was what we originally wanted to study, but also genes associated with development of cardiovascular disease, some cancers, dementia, and type 2 diabetes — all the major lifestyle-related diseases,” she says.
“Both low-carb and high-carb diets are wrong,” says Johansen. “But a low-carb diet is closer to the right diet. A healthy diet shouldn’t be made up of more than one-third carbohydrates (up to 40 per cent of calories) in each meal, otherwise we stimulate our genes to initiate the activity that creates inflammation in the body.”
“Genes that are involved in type 2 diabetes, cardiovascular disease, Alzheimer’s disease and some forms of cancer respond to diet, and are up-regulated, or activated, by a carbohydrate-rich diet,” says Johansen.
Johansen is not a cancer researcher, and is not claiming that it is possible to eliminate your risk of a cancer diagnosis by eating. But she thinks it is worth noting that the genes that we associate with disease risk can be influenced by diet.
“We’re not saying that you can prevent or delay the onset of Alzheimer’s if you eat right, but it seems sensible to reduce the carbohydrates in our diets,” she suggests.
“It was interesting to see the reduction in genetic activity, but we were really happy to see which genes were involved. One set of genes is linked to cardiovascular disease. They were down-regulated in response to a balanced diet, as opposed to a carbohydrate-rich diet,” she says. Another gene that was significantly differently expressed by the diets that were tested was one that is commonly called “the youth gene” in the international research literature.
Perhaps the negative gene changes above 40% carbs become neutral or positive again once fat is lowered enough. Also i am unsure exactly how many diets were tested, i think only two. More diet variations would be interesting.
Great comments! I think the biggest value of the macronutrient extremes (very low fat or very low carb) is for a therapeutic effect once a disease has already initiated; I wonder if some sweet spots in the Swampland can work towards disease prevention via other mechanisms like gene regulation (assuming food quality and lifestyle factors are dialed in). Very interesting…
As for the difficulty in obtaining enough nutrition on very low-fat, I’ll be covering that in the next post — but in the meantime, you might be interested in Angelo Coppola’s “Plant Paleo” diet, which is quite nutritionally sound and very similar to what I’d propose as a low-fat + ancestral combo (vegetables, tubers, legumes, root veggies, fruit, gelatin/cartilage, oysters/other shellfish, weekly organ meats (liver is only 25% fat and fills in many nutritional gaps, especially fat-soluble vitamins), other lean meats and seafood):
http://www.humansarenotbroken.com/about/plant-paleo/
BTW, I think 10 – 15% fat still works fine for that therapeutic effect except for extreme cases of heart disease, diabetes, etc., in which case the stricter level may be needed initially. As someone metabolically healthy, my own diet averages 15 – 20% fat, and I find that to work quite well for me.
neisy,
In the case of Esselstyn’s patients, they continued the VLF diet (no oils, 10% or less fat) even after their heart disease was reversed or improved. It became a lifestyle change. Kempner’s Rice Diet was another story. Much too restrictive for a permanent change but from what I read from your research and from other sources, Kempner’s patient’s problems didn’t appear to resurface.
Where would you say obesity falls on that spectrum? Does it require the same drastic measures such as the rice diet?
I wish there were more focused follow-ups for the studies. If LCHF and HCLF both produce results for the duration of the studies, how would you maintain the results? I’ve come to the conclusion that restriction through diet in my teens has only impaired my health and metabolism. I don’t know how to reconcile this new conclusion with what I feel needs to be done in order to regain my health and weight.
Maybe the real secret is choosing between the two camps, the one that you can live on forever?…
Yes how many times have I wondered what am I supposed to eat. When you have weight issues or health issues I think choosing either extreme as a fine way to go, but that is not necessarily forever, you can always switch to the other extreme as your body and health changes. If you cannot tolerate one extreme for whatever reason try the other one, neither will hurt you in the short term. I personnaly have just done this and my body tells me Yes this is good. And when we are where we need to be – we can relax our dietary guidelines somewhat if we choose too. Listen to your body and how it responds to the changes you make that is the best way to know.
Thanks for the words of encouragement. Did you mean you just did LF and felt better? I’ve done HF for so long that this is terrifying and counter-intuitive, but I’m hopeful. At least I’m letting go of the dogma that one way is healthier.
Do you think a maintenance diet would be somewhere in the middle between the two?
Out of curiosity, what did/ does your diet looks like?
Once upon a time I weighed 205 pounds, I got down to 186 pounds doing low carb high fat and for 13 years no diet worked anymore and I sort of gave up. Then a friend lost a lot of weight doing low carb high fat and I tried again, I had made some other improvements in my health in the meantime and then my body once again responded to LCHF. It was tough going but I got down to 135 pounds over about 5 years time. But I really don´t like all the animal foods all that much except for cheese. I also have type II diabetes and I did not believe I could eat a low fat high carb diet. But I no longer tolerate all that fat in my diet, no gall bladder and getting older ya know. So one day I just started eating tons of fruit, I love fruit, and wonder of wonders with the same medications I took to manage my blood sugar on LCHF my blood sugar stayed the same with the high carb low fat. It is all in the composition of the foods we are putting together in our meals. This is a very recent change for me, and I did not make the change due to anything I had read, I just paid attention to how my body responded and I lost a few more pounds. So what do I eat know, I am not obsessive compulsive about it. I usually eat 3-4 pieces of fruit, whatever I feel like for 2 meals a day, and sometimes all 3 meals. But I do eat vegetables, Ezekial bread and eggs, beef etc… usually once a day, but only if I feel like it. Sometimes I think my body tells me I need some animal protein because I will get a craving to eat some eggs or meat. So then I do. Go figure I never thought in a million years I would get a craving for eggs. What I absolutely believe is that high fat and high carbs is a recipe for disaster for most people, except for the few who are genetically blessed and eat whatever they feel like without any health or weight problems. Most of us fall on one side or the other we do better closer to one extreme or the other. If you thing about all the things we have all been reading, not just this article, somewhere in the middle could be okay if you are a normal weight and have no health problems. If you are worried about being on a high fat diet for so long, try a very low fat diet and see how you respond. But the science clearly shows, at least to my mind, that high carb and high fat are the culprits for many health problems.
HF + HC is the bane of our existence! Probably because it’s so darn tasty. This combination is not found in nature so there’s no danger on overdosing on these when sticking to an ancestral inspired diet like Mark’s or Denise’s.
Wow, your experience sounds just like mine… Only I was always normal weight and grew up either starving (being poor and neglected as a child) or consciously dieting. So, even though I’m supposedly “genetically blessed” I no longer respond to diet and have incurred A LOT of chronic symptoms and obesity at my fairly young age (27). So I’m kind of stuck eating really low-calorie with absolutely no results and a lot of frustration. I idealise Paleo because it worked for me a few years ago and it made me really healthy and happy for a brief time. Of course I wanted bigger, better, faster so I introduced IFing and LC and removed all fruit, got kidney stones and my perfect-health bubble shattered and sent me to a tailspin of binging and depression.
Oops, I’m telling you my life story on a public forum… Sorry about that! Thanks for sharing your experience, it’s at least encouraging. Right now I eat the way you described but it produces no weight-loss for me so I might have to extreme-ise my already extreme diet (by my young peers’ standards. Darn it!)
“this combination is not found in Nature”. I suppose it’s how you define HF/HC, but if a food has both, somewhere in the 50-50 range for each ought to be considered high in both categories, no? Try good old human breast milk. While it can vary over the production cycle as the infant’s age increases, it’s about 52% fat, 42% carbs. For comparison, a cake doughnut is 51% fat, 44% carbs. Coincidence? You decide. Maybe we are genetically programmed to go for this combo.
Check out this video there might be an answer –
This is a great video – explains very simply why some of us our fat – very intersting.
How to Lose Weight Without Losing Your Mind
In nature, the people living on breast milk are supposed to be gaining weight.
And your point is? One commenter stated that the combo does not occur in Nature, not that one could lose or gain weight from it. It does exist in nature, and there is no evidence that our Paleo ancestors (who were probably doing their best to avoid starvation) didn’t eat this combination of nutrients. It seems everyone in the US judges any diet or food by whether it will help them lose weight. Maybe if they didn’t eat junk and sit watching TV 6 hours a day, they could assess foods for their other qualities. And probably enjoy life more.
It’s worth looking at the Asian diets. The traditional Japanese diet, for instance, is quite low fat but a whole lot of Japanese ate that way and were quite healthy. The Japanese mountain people still do, and they do fine on it (lots of active old folks!). Personally it suits me quite well … very good for losing weight and maintaining weight loss, and it doesn’t end up looking too different from neisy’s version of low fat. I think when you concentrate on a “cuisine” you forget about the fat content. The Asian cuisines tend to have more flavor, with a little bit of flavored oil (like sesame oil). I feel about 20 years younger when I eat that way.
However you also get into other issue relating to the source of the macronutrients. I’m beginning to think that to make really tall and muscular humans, you need milk and maybe beef. There is something in dairy that triggers the “grow BIG” gene, and the kids who don’t get dairy when they are growing end up being shorter (albeit as or even more healthy?).
@heathertwist I’ll repaste Ancel Keys’ acerb quote from later on in this thread:
“The team player’s diet is apt to be built on the same philosophy as the old Chinese idea – if you want to be big and strong you eat the muscles of big and strong animals – plus the notions of nutritionists who believe that whatever grows baby rat meat faster is better. So they are stuffed on the biggest (and most expensive, therefore fattest) steaks to be found, they guzzle gallons of milk, and nowadays may be plied with vitamin pills as well.”
He made this comment about feeding the Minnesota Golden Gophers football team early in the 1940’s…and he continues on to how this heavy eating leads to CVD and obesity when they got older and quit working out.
But, yes, it makes those young rats (and humans) grow fast….and it was the basis for the famous paratrooper rations….
Japanese mountain people! This reminds me of children’s stories we used to read to our kids about wise old people, talking badgers and pine forests. There is a nostalgia for that in Japan, transporting people out of their real world of urban stress and soy sauce into their imagined past. All that exercise and fresh air combined with a spartan diet! Autophagy at work producing happy centenarians! Hai!
Yeah, there is a certain amount of mythology about old folks. This town is pretty well studied though.
http://www.livestrong.com/article/312974-yuzurihara-diet/
One of the interesting things is that their skin remains supple and young looking, as do their joints. This is believed to have to do with hyaluronic acid, which is in their favorite yams. So there is more to the topic than just fats!
I’d also comment that these diets have little or no wheat or milk, which are both confounders of a sort because they have a different set of health issues.
Here is another Japanese centenarian. He died recently at 116. His diet was:
According to local media, Kimura ate a three-meal-a-day diet of rice, pumpkins and sweet potatoes.
http://worldnews.nbcnews.com/_news/2013/06/12/18914235-oldest-man-in-recorded-history-dies-at-116-in-japan?lite
So today I started an experiment with eating a yam-based diet. Today I ate 3 purple sweet potatoes, and two bowls of gelatin broth, some konjac root, and a bit of catfish. That diet is close to zero fat.
The thing I noticed today is that I had zero hunger. I stopped at one small (5 oz) sweet potato because I simply couldn’t hold any more. The gelatin may have had something to do with that too, I dunno. But I was running errands and felt no need to stop for a latte or energy bar or anything else. So the question is: if you eat pumpkins and sweet potatoes, does your body synthesize the fats you need? Or would the fats come from “extras” in the Japanese diet, like miso, sesame oil, fish fat? Kimura seems to be in rather good shape for 116.
All plant foods have small amounts of fat. It’s impossible to eat a whole food diet and not get enough of “essential” fat. Everything else can be synthesized.
So my question is: why do SOME people on super-LF diets get dry skin (me, in the past) while some do not? My diet at the time was also whole foods, but a different set of foods, and after a year on that diet I had lost weight but my skin looked 30 years older.
Dehydration comes to mind.
Really there is not much in the way of evidence to suggest omegas have anything to do with skin moisture.
This article concerns our microbiome to our skin, and the problems of dry skin.
http://www.ncbi.nlm.nih.gov/pmc/articles/PMC3279608/
I expect you are right, and that’s more or less what the articles say too. The HA keeps the skin moist and the joints in good shape … without any mention of oils. The yams don’t actually have much HA though, and the mountain people don’t eat meats, which are the usual source of HA.
Also people that for whatever reason don’t get the right fats get eczema, and so do rats. So maybe there is something about the yams, or the miso they eat, that causes people to produce more HA and also to have the right fatty acids.
I looked up satoimo and it’s just taro. The foods these people ate were cheap subsistence. Yams and pumpkins are the exotics, and weren’t common in Japan until 100 years ago. Cheap, easy to grow, nutritious and not overly calorie dense as grown.
We forget that fat and protein were very expensive 100 years ago. When people had no choice but to eat a 90% carb diet, they probably were in a semi-autophagic condition all the time, and on the edge of beriberi. I’m not surprised that your yam diet depressed your appetite. That’s what it should do.
Japanese that live near the ocean traditionally ate a lot of fish, and the fish they eat … like mackerel … is rather oily. Also sea mammals do wash up regularly and they are extremely high in fat. Water birds are also pretty high in fat. So it doesn’t surprise me that they were healthy.
The mountain people don’t live near the ocean, and they grow their own food mostly. Which would make fat very hard to get. Also a diet based on yams doesn’t strike me as balanced? Somehow it seems to work though. There are a couple of other yams that are more “native” to Asia, d. alata and d. opposita. Nice rundown of yams here:
http://www.marksdailyapple.com/difference-yams-sweet-potatoes/#axzz3r7WzOYOH
The “sweet fish” the mountain people eat is maybe Ayu, which is related to salmon, so probably has a fair bit of fat?
http://www.kanoyama.com/fish-facts/
Also if it swims up from the ocean it would provide enough iodine, which is an issue for inland communities.
I used to travel to Japan for business, and ate a lot of salaryman food. Korean barbecue, big bowls of udon, okonomiyaki (a cook it yourself seafood omelet), lots of yakitori sticks, and lots of Kirin beer (sometimes the only liquid on the table). Never a lack of food, but nothing really greasy or fatty. Occasionally our hosts would take us to somewhere expensive, and that’s where the fatty beef appeared, for shabu shabu. Another time it was Chinese, and the centerpiece was a big carp.
I linked this in an earlier section. I’ve always liked it because it contrasts the Japanese and American diet in a unique way.
http://www.theatlantic.com/past/issues/86nov/fallows.htm
I read the Atlantic article and I enjoyed it. He is spot-on … the “exercise” issue I think is mostly a red herring. Or maybe it matters only in the swamp. I live near a lot of farmers, and you really can’t be a farmer without exercising, even if you use a tractor mostly (just CLIMBING on the tractor is work!). But many of the farmers are just huge and very obese, or have major issues with arthritis or whatever. Others are really healthy: they are thin and limber, even in old age. For fun I started asking them about what they eat.
The thin and limber farmers tend to be the chicken farmers, who mainly eat a whole lot of eggs, or the ones who eat a lot of vegetables (many are basically vegetarians or vegans). The less-healthy ones tend to be the beef farmers. But in any case, the “exercise” issue isn’t the main one.
As for being hungry on the “Japanese diet” … the portions really are smaller. But I also wonder if the Americans avoid some of the more nutritious choices. For instance, mackerel is rather high in fat and often served for breakfast. Lunch often includes raw egg yolks. If you have mackerel or a raw egg yolk, it is quite filling! But most Americans would probably avoid both.
Plus of course if you “grew up American” you are just plain BIGGER and so require more calories.
However, my own experience has been that since I’ve switched to a more “Asian” (my version of it) diet, I just eat a whole lot less food. It’s more filling somehow. I do eat all the weirder stuff … the egg yolks and baby whole fish, kimchi, miso, mackerel for breakfast, and now, lots of yams! Since reading this article I’ve doubled down on the low-fat part and am actively avoiding our normal OTHER food (like Indian curry or fried tacos …). Also I am older. My daughter is still growing, and my meals just don’t fill her up at all.
A couple other food anecdotes from Japan. Breakfast often had pieces of dry smoked salmon with white rice. A few times the rice came with a raw egg. The rice is supposed to be hot enough to cook the egg, but usually it ended up raw egg rice glop, which wasn’t too bad. Natto would also show up for breakfast. Snacks on the train – mandarin oranges and smoked chestnuts. The Japanese version of teppanyaki (like Benihana and other US Japanese steakhouse – eating on the grill) was a lot more subtle (no flaming onion ring towers) and used a lot of things you don’t see in the US, like thin sliced grilled winter squash. Finally, snacks at a baseball game: marinated squid or octopus rings. Tasty, but like chewing rubber bands.
Nom! I do love dried squid snacks too. Might be when you get introduced to them. I got them as a kid, and gave them to my kids. They love them. Also some of the other weirder foods. But they can’t stomach McDonalds or most of the other fast food … it tastes “weird” to them.
My only problem with the 15 year Esselstyn study was that ALL of the participants were on statins. In fact Esselstyn said that stains + diet works better than diet alone
There’s a protocol that tries to use carbs based on the amount of resistance excercise: Carb Bacloading by John Kiefer.
Equal macronutrient intake is like the early version of Jonathan Bailor’s diet (Smart Science of Slim), usually used to getting thin. But it doesn’t convert to the same macronutrient at the cellular level where the genes are expressed:
1) If you are getting thin it means you are burning your fat stores – the diet a the cellular level is higher in fat.
2) Fiber and other fermentables can give like 6% of calories for the cells in the form of short chain fatty acids.
Same with very low fat diets – they may be the only human state with a high level of creating fats from carbs by your own cells (that is other than bacterial fermentation). In a “balanced” diets most stored fats comes from the dietary fat.
Some low skin quality is visible in some high-carb vegans. No as bad as drunkard faces, but below normal people of similar age. McDougall himself has bad skin for his age, Durianrider also. But it doesn’t seem to affect Esselstyn, at least as per what’s expected for his age. Perhaps the reason is the first two promote fast-burning starches / fructose respectively, while the latter eats a lot of anti-inflammatory greens and vegetables?
Durian Rider – hmmm
http://anthonycolpo.com/durianrider-66-kilograms-of-obnoxious-unabashed-ignorance/
Interesting link. Interesting also to see there are folks that share my view that some of the more virulent vegan jihadism may have a biochemical basis. Whenever I have broached that subject, the vegan jihadists go into fatwah mode. It would be interesting if someone did a study to examine that possibility. I’ve never encountered any other dietary regime whose followers, at least many of them, display such arrogance and anger. Some that claim they wouldn’t swat a fly also claim that they would gleefully watch an omnivore’s painful death agonies.
Very strange!
Yes, they are. But dietary deficiencies would go far to explain their strangeness, and their rudeness. I’d hate to think that it’s just that only mean-tempered folk become vegan.
Hunger causes high cortisol levels … my family is mostly pretty mellow but when they get hungry, watch out! I’ve gotten in the habit of just making sure they get some food when they get grouchy. The term “fat and happy” has some basis in fact. It might not be so socially acceptable, but fat absorbs toxins in the body too.
But many of the vegans and raw foodists I’ve seen are overly thin IMO, with very little muscle mass. A couple told me they had to change their eating, because they simply couldn’t eat enough calories on their food choices. So I expect that even if they are used to the hunger level, it might in fact be making them grouchy.
Note though that the Japanese mountain people are noted for also being *happy*. They don’t look overly thin either. They aren’t vegans though … they eat a kind of oily fish, though not very much.
Anthony Colpo thinks that refined grain is healthier than whole grain and that dietary cholesterol has no effect body cholesterol. Hmmm. He’d also get smoked by Durian Rider on a bike and Colpo is an avid rider.
Somehow I doubt that
Yagh you guys are nuts. I just finished wood smoking a bunch of ribs and sausage for the winter. Both those guys would smoke me on their bikes but then a 50 lb Schwinn tops out at about 12 mph. No matter what you do.
The best use for bananas is bananas foster.
Here’s a list of alleged good uses for bananas (you can ignore the banana-sicle one)
– Make a face mask
– Tenderize a roast
– Polish silverware and leather shoes
– Brighten up houseplants
– Deter aphids
– Use as fertilizer or mulch
– Add to compost pile
– Attract butterflies and birds
http://www.rd.com/home/banana-uses/
Somehow I doubt you know much.
“Body” cholesterol? I assume you mean serum cholesterol. And, no, unless you have a metabolic disorder, dietary cholesterol doesn’t have an effect on serum cholesterol. Mainstream medicine finally acknowledged this, and it was big news a few months back. It’s even acknowledged by the USDA food mavens, who took it into account in working on their updates to the food “pyramid”, “plate”, “rhombohedron”, or whatever they are going to call it this time.
Zach, never heard of “body cholesterol.” But if you mean “serum cholesterol” there’s no connection between diet and serum cholesterol. The liver both makes cholesterol and breaks it down too depending on the body’s perceived needs for c’stol at that time. Diet has little to nothing to do with it. E.g. I had a vegan godparent who STILL had high c’stol, even though there’s zero c’stol in plant-sourced foods. The FDA is moving toward dropping the dietary c’stol limit, finally getting rid of that idiocy thank God.
Even Ancel Keys knew that dietary cholesterol had no affect on serum cholesterol, because he did the experiments to prove it. It was for this reason that he developed the theory that dietary fat raises cholesterol. (Some of the mainstream government officials who make dietary recommendations got that part wrong, because, you know, they’re not doctors or nutritionists). In any case, it’s been known for a very long time.
Carbohydrates raise triglycerides, so that might have been what Anthony Colpo was talking about when he made that statement about cholesterol.
Guys, “durian rider” is a nobody and a fool. How he ever came to be talked about is beyond me. I advocate 100% fruit diet and imo that guy and everyone associated with him is a joke and are toxic to the perception of the fruit diet. He’s not a serious person, he’s a clown.
Ancel Keys spent a lot of time figuring out how to be healthy in the middle of Swampland (30% fat). His Scientific Diet prescription for weight loss is calorie counting, of both food AND activity (big tables of that), to create large daily calorie deficits. I’ve used that methodology for 8 years to lose 50 lbs and sustain the loss, though I didn’t attribute the method to Keys. I do this living squarely in the middle of Swampland. For lack of a better term, it’s a high carb, high fat diet, with adequate protein.
When I tell people how it works, they are shocked at how much exercise it takes to sustain the weight loss. I walk and bike enough each day to eat 2300-2500 calories and maintain weight. It takes at least 3 hours every day, but it’s broken up through the day. If I ate 1500 I could do this sedentary. But my stomach is a sized for 2500 calories…and my thighs are sized for 1000 calories…my paleolithic ancestors left me with a body optimized for both…
Denise, once again you’ve done truly amazing work and I couldn’t be prouder of you. I wanted to bring up an interesting topic of gut microbiome and what kind of microbes are found in the guts of people on high fat vs high carb diets. It wasn’t until I cut out processed foods, sugars and added more fat and protein into my diet before I saw the result of not getting colds every week (and these weren’t allergies). Remember what I went through for years? Now, being on relatively higher fat with carbs consisting only of fruits and vegetables (no grains), I only get colds maybe twice/3x/year. Your research brings up many good questions and some mighty interesting theories. Great job!!!!
You should have NO CONCERN about your blog being too long. People truly interested in this topic will eagerly devour it … no matter the length. Those less curious can easily skim, scan, skip … and still leave with an incredible amount of useful information.
Thank you very much for your too long to print but too fascinating not to read blogs.
After reading many interesting replies and questions about what does this mean going forward, I see two possible directions. One is we are only safe in the dietary extremes, or quality matters in the middle. The fringes work because they help regulate energy and calorie intake by lowering palatability and creating a primary energy path way, either fatty acids or glucose. Epigenetics shift that optimize usage and feedback as best as possible on that diet regime. The middle ground is mushy because the dual energy pathways can get out of sync. Eating crappy food is gasoline and very dangerous in the middle. The extreme diets ironically allow the toleration of more crappy food. Does that make them better? Maybe not, but just simpler. If the quality is high in the middle, with perhaps some intermittent fasting, you can have both carbs and fat…Ala the French Paradox.
Interesting take, Joe! I tend to agree — my interpretation is that the extremes are best for reversing existing disease (AKA they’re “therapeutic”), but they aren’t necessary for maintaining health in someone who’s already in good shape and has their food quality and lifestyle dialed in.
Mwah and many hugs to you for a yoeman’s job of extracting these compelling findings from forgotten but significant studies and doing it with welcome humor. We love you for doing it!
Sent from Yahoo Mail on Android
From:”Raw Food SOS” Date:Tue, Oct 6, 2015 at 10:21 AM Subject:[New post] In Defense of Low Fat: A Call for Some Evolution of Thought (Part 1)
neisy posted: “Not a typo. Not April Fool’s Day. Not a spontaneous and mystical possession by the spirit of George McGovern. Not even a social experiment to see how many people I can get to unsubscribe from this blog in the span of a day (PLEASE STAY, I LOVE YO”
Fantastic article Denise. The voice of sanity as usual.
I love your honesty!
Great post! I remember watching your AHS talk some time ago in which you speculated on the presence of a metabolic capability to live on a very high carbohydrate low fat as a survival mechanism similar to ketosis, and am glad to see the followup on that. It makes sense for such a mechanism to exist, as starchy tubers are basically the only plant foods readily available in amounts that are capable of supplying one’s daily energy needs.
I look forward to reading your personal views on ‘carbosis’ in part 2 – it seems to me to be like ketosis in that it likely confers specific therapeutic benefits but are probably not a favorable permanent metabolic state.
Personally, I’d think that unless you lived off of chicken breast and egg whites it would be really quite difficult to intake sufficient protein on such an extremely low fat diet.
There are many examples of people experiencing metabolic damage from both too high fat and too high carb. So it’s not all magic at both ends of the spectrum.
The raw foods/fruitarian 801010 diet for example has some horror stories, and the high fat paleo diet seems to see longer term issues also.
The diet being discussed here however is the Kempner/Pritikin/Onish/McDougall/Esselstyn/Barnard diet. This diet would appear sound and supported in terms of its therapeutic benefits.
What do you think are the longer term issues with high fat paleo? I haven’t encountered any in 7 years of the diet, but perhaps that isn’t long enough?
CVD issues, with Atkins himself as the prime example. He was lean and healthy on HFLC in the 1970’s, but by the 1990’s looked jowly and overweight. In the 2000’s he started to exhibit serious CVD problems.
I think that Cordain’s original take on Paleo as a lean meat low carb diet is probably better as a longevity diet. But I don’t know of any examples.
Actually, there is considerable reason to doubt that Atkins had CVD. Atkins got a viral infection, leading to chronic cardiomyopathy, which he freely discussed during his lifetime, including on national television. At the time of his admittance to hospital, he weighed 195lb, not excessive for a muscular man of his height – over 6″. He played tennis weekly. The 258lb commonly cited for his weight was what he weighed when oedema set in as his organs failed. http://usatoday30.usatoday.com/news/health/2004-02-10-atkins-statements_x.htm
As to the jowls, he was 72 years old! This very unflattering photo of him doesn’t indicate that he was overweight, merely that he was showing his age. http://www.cbsnews.com/news/diet-guru-atkins-dead-at-72/.
Hey Andrew,
“it seems to me to be like ketosis in that it likely confers specific therapeutic benefits but are probably not a favorable permanent metabolic state.”
Yes! That’s my interpretation as well.
RE: obtaining protein, it’s actually not too hard if you include gelatin, shellfish, and very lean meats/seafood, and perhaps also legumes. All whole plant foods have some protein, so even nothing but starches, veggies, and fruit will typically wind up yielding 10 – 15% protein (more if you’re heavy on lentils).
Wow, just wow. Thank you for your amazing research and analysis! You are awesome!
Well-timed, Denise. Transitioning from a diet of Primal-inspired magic, I’ve been having a horrible horrible (and I don’t encourage literary redundancy, mind you) time with a Peatish, HCLF eating. It’s been nearly 6 months and except for exacerbating my insomnia, acne and weight nothing has improved.
I even got myself onto the 23andme bandwagon to try and understand my (presumably) shoddy genetic lot in life. The results: supposedly I’m one of the lucky few who respond to any diet and any exercise (my once thin but now obese body was unimpressed, to say the least). Apparently I also have no food sensitivities despite my lifelong suspicions that I do and the inherent tendency to restrict food groups and macro-nutrients (oops…).
To Denise:
Do you think there’s an ancestral/ genetic/ (what-have-you) inclination to do better on one approach over the other?
I also wonder if the perfect median between the two would be a weekly cycle
(a few days of 10-15% F and others of 65% F) or would that just make your body hopelessly confused? (Without MS or Diabetes, obviously.) I find the body does better on consistent (bland) foods.
Hey Lee,
Thanks for sharing your experience! Out of curiosity, does your Peat-inspired diet include a lot of dairy? That seems to be a big issue for some people, especially with acne and weight gain. Along with your 23andme data, you might be interested in getting your gut microbiome analyzed at some point — that seems to be a missing link explaining food sensitivities and variation in response to different diets.
“Do you think there’s an ancestral/ genetic/ (what-have-you) inclination to do better on one approach over the other?”
Quite possibly, but I no longer believe it’s ‘fixed’ in terms of “I have x genetics and therefore my optimal diet is high/low fat”, so much as environmental and lifestyle factors triggering different gene expressions and altering a person’s response to diet in ways that change throughout life.
I actually do believe a cycling between the extremes could work well. I’m writing about that in Part 2! 🙂
Thanks for getting back to me! 😍
I think a Peat diet without dairy is like a Paleo diet without bacon. It could work in theory, it just wouldn’t have the same appeal. 😄 So yeah, dairy is a mainstay of my current diet and I have several SNPs that indicate lactose tolerance into adulthood (though I can’t get high quality dairy and might be better off without it).
I have a nagging fear that my cortisol levels are exacerbated by my sugar intake (from fruit and juice) and thus cause my chronic insomnia, but you and Peat have made me reconsider this phobia. I could just be squared right in the macronutrient swampland and need to revisit my diet.
Circumstances facilitate the reception of new information, and whereas before I would’ve turned my nose and kept to my Paleo-dogma, now I value anything that makes me revisit it. (You can say my self-imposed suffering is an anti-dogma crusade!) So thank you for what you do! 💕
I can’t wait for part 2 and (selfishly) encourage more posts (or an awaited second book!) on making sense of one’s genetics and addressing them with lifestyle. Yeah I’ve read around on this thorny subject, I just don’t think anyone but you can do it justice. 🐰✌
Is there some reason that you switched something “magic” for something “horrible horrible”?
For people who may not be familiar with Peat, here are some of his quotes advocating low fat and/or skim milk: https://goo.gl/zinfaa
I think many people consume too much milk fat, and confuse Peat with the whole milk Weston Price stuff.
I also think many peoples definition of HCLF isn’t really LF.
Finally, something that might explain Freelee’s ability to eat insane amounts of fruit and juice and carbs while staying so enviabily thin! (And my not so enviable results on high fat low carb diets.)
Finally something that might explain the banana’s girls impressive results and ability to maintain such a lean phyisique. I’d searched everywhere for something that could explain this, this post is “everything”, as the kids say these days.
Oddly enough, the original Rice Diet only permitted one banana per day. Was it the potassium? It obviously wasn’t because of the sugar if 100-500g of table sugar was allowed!
Yes because the diet focused on reversing kidney issues and potassium can be problematic.
people, just wanted to say: please, don’t take dietary advice from this writer. i’m not questioning her intentions or her knowledge, but she has no legitimate training or experience in research or clinical work. as you can well see, this post is representative of her transition in terms of knowledge; in her self-education of food and nutrition, she’s making progress and has evolved, in her own terms. she may well continue to evolve until she’s on the same page as those who do have the training, research and clinical experience.
again, not knocking her intentions or her intelligence (although she–like any writer–is in dire, dire, *dire* need of an editor), but she’s no more qualified than any commenter here. whatever side of the so-called “debate” of HC vs. HF you find yourself on, please focus on the peer-reviewed books by trained professionals that has gone through some kind of editorial process.
Yes, let’s all get on statins and PPIs immediately.
I saw no dietary advice here. I saw a very thorough examination of data that says maybe, just maybe, low-carb is not the be-all end-all to dieting.
And why, pray tell me, should one listen to Jonathon Smith. Is he qualified to make such statements?
I wonder, Johnathan, have you read Denise’s blog before or just stumbled across this post? It’s just that she is the least likely blogger to imprart any nutritional advice. I’ve always found her posts enlightening and refreshing becuase even though she’s been taken under the wing of Paleo gurus like Mark Sisson, she was never apologetic about her near-Vegan, low-fat diet. I think the real purpose of her blog is to be a breath of fresh air in a blogosphere of nutritional dogma, and if you notice, those who comment on here come from a variety of dietary walks of life. Don’t worry about us being duped one way or another, we have functioning brains. We just like to read and look at pretty graphs! 😄
She has in no way given advice on what to eat in this article. She is just reviewing some old literature and doing a good job too. As a person with a science background she does a good job dealing with the issues in scientific research. Who cares if she doesn´t have a PhD, or MD behind her name. I have recently made a fairly radical dietary change from LCHF to almost frutarian and have been puzzled over how well my body likes this and that I have even lost a little more weight. She has given me some answers to that, or one of the links that came up in the comments. This is all fascinating stuff, read enjoy, it is a brain puzzle.
I think you need to read all of this again, Denise isn’t offering any dietary advice in there. What she is doing is taking reams of research and presenting it in an accessible format and delving into both sides of the issue. I’m actually not sure what your objection to her is, because it’s not as though she’s trying to present a poorly constructed study that she did herself. On the contrary, she’s taking that ‘peer-reviewed’ research that you’re lauding and explaining it, and referencing the research so that all of us can go and read it ourselves. Most people here have probably learned far more from her than they ever would from the actual studies themselves, due to the way they’re constructed and the original audience they’re intended for.
Jonathon, you miss the point, Denise Minger doesn’t give dietary advice. She does a fantastic job leading us to examine our raging dietary dogmas. I’ve followed a low-carb diet since 2007, it normalized my blood sugars and other blood panel numbers, and have no intention to return to HCLF. Still I find what she writes immensely valuable and informative. Btw Jonathon, if I’d followed the advice of those with “legitimate training and experience in research or clinical work”–including my dear old doc– I’d now be popping oral meds and injecting insulin now instead of controlling it through lifestyle.
-1
Jonathan, you fail to realize two things:
1. Scientific research on nutrition is extremely lacking and not fully understood. Like Sam Harris said:
“I have this feeling that we don’t understand human health and nutrition enough, the fact that there’s any controversy at all about what human beings should eat so as to be healthy, I find to be an incredible scientific embarrassment, the fact that you have debates about carbs and protein and fat consummated by good faith by experts and there is still some uncertainty, is an amazing state of our current situation in science.” – SH
Sam sounds like Ray Peat there:
“Nutrition is one of the most important sciences, and should certainly be as prestigious and well financed as astrophysics and nuclear physics, but while people say “it doesn’t take a brain surgeon to figure that out,” no one says “it doesn’t take a nutritionist to understand that.” Partly, that’s because medicine treated scientific nutrition as an illegitimate step-child, and refused throughout the 20th century to recognize that it is a central part of scientific health care.” – RP
A couple other good Peat quotes, notice the word “hardly:”
“Nutritional research has hardly begun to investigate the optimal ratios of minerals, fats, amino acids, and other things in foods, and how they interact with the natural toxicants, anti-nutrients, and hormone disrupters in many organisms used for food.” – RP
“For fifty years, the mass media have been making the public think about the fats in their diet, filling the culture with clichés about bad saturated animal fats that raise cholesterol, or lately the trans-fats in margarine, and images of arteries clogged by bad fats. The public instruction about the fats we should eat resembles the owner’s manual for a car, that tells you what kind of motor oil and fuel and coolant to use; they are telling us that they know how our body works, and that they know what it needs. But now, even after the human genome has supposedly been partly “decoded,” the biological functions of the fats have hardly begun to be investigated.” – RP
“The amino acids in proteins have been defined as “essential” on the basis of their contribution to growth, ignoring their role in producing long life, good brain development, and good health. The amino acid and protein requirements during aging have hardly been studied, except in rats, whose short life-span makes such studies fairly easy. The few studies that have been done indicate that the requirements for tryptophan and cysteine become very low in adulthood.” – RP
And 2. I don’t need Denise to be a clinical researcher to understand and interpret the studies that she posted that show high starch/carb cultures living very healthfully.
Jonathan said:
“please focus on the peer-reviewed books by trained professionals that has gone through some kind of editorial process.”
Books?
Denise has posted many studies here. I’m not sure why you’re ignoring that. I think it’s clear that you’re angry with something that is not only pro “carb” but pro-the devil sucrose. While you do this you also ignore a key point that Denise wrote above:
“I do want to make one thing abundantly clear before we continue, though. The title “In Defense of Low Fat” doesn’t imply its inverse, “In Attack of High Fat.” Quite the opposite! My goal here is to create a space where two very different dietary approaches can sit down for tea, respectfully coexist, and interact without any subsequent homicide investigations. In fact, I’ll be arguing for a more panoramic view of nutrition where the success of both high-fat and low-fat diets are compatible, and maybe even make sense. It just requires zooming out farther than we’re used to looking, and acknowledging that our ever-rivaling communities could actually learn a lot from each other.” – DM
All you’re doing Jonathan is subtle ad hominem on Denise and you’re not actually refuting anything in her post.
Thanks, Jonathan. Instead I’ll take advice from you. Apparently you never learned to capitalize words properly and write rambling, run-on sentences. Yet you critique Denise’s writing? I’m impressed.
Jonathan Smith: I think Denise is quite welcoming of peer review. A work doesn’t have to be published in a book or journal anymore in order to take part in scientific discourse. You’re free to refute anything that doesn’t sit right to you, but discrediting her entirely due to her lack of “legitimate” (whatever that means) training or research, isn’t helpful or interesting.
jonathan smith, you deserve a seizure for that post.
Thankyou for this. Rather than making people run away, this sort of article will attract the really interested, and I have now subscribed. I have tried vegan, then low-carb paleo, and have recently joined the Peat-clan. I always ran into a roadblock trying to understand why juice-fasting worked (Did this years ago), when it is a very high fructose diet which should instantly kill you according to Paleo-peeps.
If you write, I will read. Thanks. As omnivores, we will make choices. Informed ones are preferable.
Excellent post.
I’d just throw my twopence worth into the mix here.
Many years ago I tried a Pritikin style diet and ended up with problems. Looking back that might have been because I just wasn’t getting enough calories, especially as i was an athlete at the time.
That’s why next time I looked for a diet, I rejected low-fat and went low-carb/paleo. Eventually I ended up with all the symptoms referred to by people like Matt Stone – insomnia, frequent urination, cold extremities. So eventually I had to ditch that as well.
Now, I sort of riff off Peat. Broth, liver, some shellfish, dairy. Lot’s of dairy. I find I do pretty well on it. Some people say they break out with dairy, not me. I break out on PUFAs. I also eat sourdough bread and beef. This diet seems to work for me.
Re. Rice diet for psoriasis
I went gluten free and my psoriasis dissappeared, later went paleo with varrying amounts of carbs and the psooriasis only came (briefly) back when I failed in my diet and ate wheat. In my view it is possible that the prosiasis and arthritis improvements seen on the rice diet are not due to low fat but rather due to avoidance of gluten/wheat
Denise, thank you for a great post! It definitely questions many of the paradigms we thought were settled.
Has anybody seen fasting insulin levels on LFHC diet referenced in any of the mentioned studies? It would be very interesting to look at. Please post if you have.
thanks, Anna.
Neisy, thanks so much for this detailed and highly objective review of the low fat scientific literature dating back to WW I and the earlier years of the 20th century. It is fascinating that so many serious researchers were collecting data on nutrition, disease and weight gain even if their scientific method was lacking sophistication by today’s standards. You have given us an awesome contribution by your analysis of this remarkably complex body of nutrition information. I am eagerly awaiting part 2 and please do not apologize for the length of your blogs as the depth of information is well worth the reading time. Many warm hugs!
Denise, I’m not trying to defend high fat diets. But I wanted to draw your attention to the following fact. There’s enough anecdotical evidence that the original Okinawa diet is anything but low fat. See here for example. http://stan-heretic.blogspot.nl/2009/10/beware-of-okinawa-diet-scam.html I’m not saying that this evidence is 100% true but it intimates that the topic is actually quite complicated.
Also, what about dental health? Aren’t sugar and starch detrimental for our dental health. And on the contrary a high fat diet helps remineralizing teeth? I wonder what would you say.
I’m not trying to defend high fats diets BUT ….
Then you go on to defend high fat diets. lol
You’re joking right. You count that blog post as evidence?
Denise, I’m not trying to defend high fat diets. But I wanted to draw your attention to the following fact. There’s enough anecdotical evidence that the original Okinawa diet is anything but low fat. See here for example. http://stan-heretic.blogspot.nl/2009/10/beware-of-okinawa-diet-scam.html I’m not saying that this evidence is 100% true but it intimates that the topic is actually quite complicated.
Also, what about dental health? Aren’t sugar and starch detrimental for our dental health. And on the contrary a high fat diet helps remineralizing teeth (thanks to fat soluble vitamins)? I wonder what would you say.
Weston Price already covered this that starch and carbs are not detrimental to teeth health, it’s overall nutrition that is.
As for fat soluble vitamins, fat contains very very little vitamins. Most come from organ meats, pro-vitamin consumption and the sun.
I agree that sugar is not detrimental to gum health. Most health issues stem from some sort of vitamin deficiency (for teeth I think K is the main one). You can have great teeth eating both HF or a LF diet.
I think it’s unfair to suggest fat is vitamin deficient because fat rarely occurs in nature without being prepackaged along with protein and a chockfull of vitamins (a slab of tallow, anyone?). Animal protein and dairy are some of the most versatile and complete foods in terms of vitamins. Many plants lack the same spectrum (though tubers come close!). I’m sure there’s a median between the two and I really like the Jaminets for pointing out that nutrient deficiency is a recipe for disaster. This is why I’m so concerned about either HF or LF because in the long run they seem like they would cause some sort of deficiency.
(And I’ve officially hijacked most comments now…! ;D)
In my experience I saw only negative effects from consuming high amounts of fat. Low fat foods such as liver are why higher in most fat solubles than any fatty meat including dairy. Vit d should be synthesized, vit a and k can be produced via pro vitamin forms and vit e is only needed in small amounts when high amounts of pufa aren’t consumed so I see no reason at all to eat high amounts of fat or fatty animal products (egg yolks, cream, tallow) to get your fat solubles
> In my experience I saw only negative effects from consuming high amounts of fat.
You mean, negative effects on your dental health or more generally? Can you elaborate on that?
Well all around but yes on dental health too. Sensitive teeth and a general ache in my molars. I believe it was from being slightly hypo (tsh of 6.0) which I recovered from on a HC diet.
I believe there are far more important things in regards to health than just hitting arbitrary amounts of certain vitamins and minerals. A very healthy and resilient body can achieve greatness on less than ideal diets and a sick body will not always be able to recover even with a copious amount of nutrition. So many variables.
P.S. I was taking a lot of supplements while on low carb as well which may of made things worse. I take zero supplements now and feel no need for them.
Zach… The aching molars, sensitive teeth…to me this indicates sub-clinical hypervitaminosis. The beginnings of what used to be called “Pseudotumor Cerebri” or now known as IIH (idiopathic intracranial hypertension).
It’s been an issue with me for years and any exogenous preformed vitamin A can start the aches again. Along with pressure in the eyes/skull, ascites, bone pain. I think the only safe vitamin A is the one our body makes for us out of beta carotene.
Paleo, and before that, Atkins, I think are exposing people to too much. Fortification with synthetics are doubly bad. Citizens living in first world countries shouldn’t be consuming products fortified with It.
Sorry to have hijacked this thread. When I read about the success of low-fat, mostly vegetarian diets, I can’t help but think it’s somehow due to less iron and a whole lot less preformed vitamin A.
Really interesting stuff, thanks! That could definitely be what was happening. I agree that letting our body produce certain vitamins and other things like cholesterol.
Errr…..I read Weston Price’s book. He absolutely DID say that refined sugar and white flour were bad for teeth, and general health as well.
Refined sugar and white flour is detrimental to teeth because they displace whole food nutrients with empty calories. I said starch and carbs, not empty calories.
It was a little misleading I guess, because refined sugar was used in the rice diet. And someone else in the comment section interpreted the remark about Weston Price as meaning that sugar was not problematic for teeth and gums. I was only trying to clarify the issue. But it is true that Weston Price had nothing against whole, natural starches and sugars, yes. But he was highly critical of refined carbohydrates, white flour and sugar in particular.
Zach you’re wrong. White flour and sugar are detrimental to the teeth because of the direct effect they have in the mouth both on the teeth and in changing the chemistry and pH of the mouth.
No, you’re wrong. There is no possible way to prove direct causation of tooth decay from refined flour and sugar because of the many other factors involved. Anacdotally, millions of people eat plenty of refined flour and sugar with no dental issues.
Zach: who are these people who eat lots of sugar and refined flour, with no tooth decay? I guess you haven’t seen “That Sugar Film”, huh.
In any case, sugar does block the cleansing system of the mouth (the parotid gland). Granted, this is just one theory of dental caries- (though it has been confirmed in rats). Nobody really knows what causes cavities- (hard to believe, ain’t it?!) But, “anecdotally”, sugar and white flour do seem to be problematic, at least for cultures who have just recently turned from their native foods to these foods- (as well as the teenagers in “That Sugar Film”). Also, sugar blocks the body from the uptake of vitamin C, which is important for gum health as well as for the immune system, so I think it can’t exactly be good. In addition, we do have evidence that when early humans changed from hunting and foraging to framing, their teeth and bones suffered greatly.
Oops, I meant to say “farming”, not “framing”.
I think you’re both wrong, the mechanism for tooth decay is that sugar reverses the lymph pump in the pulp of the tooth, preventing the flow of lymph out of the pores of the tooth which allows bacteria to enter the tooth and cause caries http://www.healingteethnaturally.com/dentinal-fluid-transport-steinman-leonora.html Dr Ralph Steinman came up with this – he raised his kids on a sugar-free lacto-ovo diet, they were carie-free – he and his wife both had plentiful caries so this was not a genetic effect
No actually, i was trying to say exactly what you wrote- I just used different words; but, yes, the dentinal fluid transport system, I had forgotten that that was (technically) what it was called. If you look lower down on the link you sent, it is explained that the way this works is via the parotid gland (which controls the hormones involved). Basically, you and I were saying the same thing- (though I probably didn’t explain it well).
Cool!
But how is it that only you and I and 6 other people 1 of whom is dead know this stuff??
Because its fiction. ; )
You’re coming off more and more like a troll Zach
Hi incognito,
Sorry for the late response to this! The Okinawans are an interesting (and probably inconclusive) case because their dietary patterns changed dramatically after WWII. More recent (1970s and beyond) surveys reflect the newer diet; the link in my post tried to gauge the diet circa 1950 (of course, it’s subject to recall flaws and is probably far from perfect!). I would think the pre-WWII diet would be more relevant to any longevity benefit, since it’s what the centenarians from the past few decades grew up eating — but that’s just a hunch at this point.
As for dental health: sugar and starch mostly seem to be a problem in the absence of adequate fat-soluble vitamins. Anecdotally, I developed severe tooth decay (16 cavities!) on a high-fruit vegan diet, but the addition of fat-soluble vitamins from fermented goat dairy (K2, A, some D) and vitamin D supplementation worked wonders even without significantly reducing my fruit sugar intake. Weston Price’s work (not just from his travels, but studies he performed on patients) suggests that vitamins A, D, and K2 are really what dictate the resiliency of teeth against decay.
The prewar Okinawan diet was very heavy in fish, so it was not a very high carb diet. As with all longevity pockets, though, I suspect the key factor was calorie restriction.
Heavy in fish? I wouldn’t expect that over 10% of pre-war Okinawan calories came from meats, and that fatty pork probably was at least equal to fish calorie-wise.
Here is a study that I have quoted to MS clients to debunk the Swank diet and to justify why perhaps it is the eating less processed foods rather than the eating less saturated fat that is the reason why the Swank diet may help… now you are rocking my boat!!!
http://www.ncbi.nlm.nih.gov/pubmed/11117615
Am J Epidemiol. 2000 Dec 1;152(11):1056-64.
Dietary fat in relation to risk of multiple sclerosis among two large cohorts of women.
Zhang SM, Willett WC, Hernán MA, Olek MJ, Ascherio A.
Source
Department of Nutrition, Harvard School of Public Health, Boston, MA 02115, USA. Shumin.Zhang@channing.harvard.edu
Abstract
Ecologic correlations suggest that higher intake of saturated fat and lower intake of polyunsaturated fat might increase the risk of multiple sclerosis (MS), but the results of case-control studies have been inconsistent.
Because no prospective data are available, the authors examined these associations in two large cohorts, the Nurses’ Health Study, which consisted of 92,422 women with 14 years of follow-up (1980-1994) and the Nurses’ Health Study II, which consisted of 95,389 women with 4 years of follow-up (1991-1995). They documented 195 new cases of MS.
The pooled multivariate relative risks comparing women in the highest quintile with those in the lowest were
1.1 (95% confidence interval: 0.7, 1.7) for total fat,
0.7 (95% confidence interval: 0.5, 1.2) for animal fat,
1.2 (95% confidence interval: 0.7, 2.1) for vegetable fat,
0.8 (95% confidence interval: 0.5, 1.3) for saturated fat,
1.1 (95% confidence interval: 0.7, 1.7) for monounsaturated fat,
1.7 (95% confidence interval 1.0, 2.8) for n-6 polyunsaturated fat,
1.3 (95% confidence interval: 0.8, 2.0) for trans unsaturated fat, and
0.7 (95% confidence interval: 0.4, 1.1) for cholesterol.
Omega-3 fatty acids from fish were also unrelated to risk. However, the authors observed a nonsignificantly lower risk of MS for a higher intake of linolenic acid.
Can you shed some light on this??
Thanks
I thought that possibly the high pufa intake could’ve been ameliorating/covering up deficiencies associated with MS by suppressing metabolism?
Hi Patricia,
My first thought with the quoted study is that the range of fat intake probably didn’t encompass low enough levels to detect a correlation between fat intake (especially saturated) and MS. In Swank’s study, anything above 20g/day of saturated fat — whether 21 grams or 60 — had pretty much the same effect on his patients (in terms of exacerbation rates and mortality); the apparent benefits of saturated fat reduction didn’t appear until people were eating in the 10 – 15g/day range.
In the Nurse’s Health Study data, we can see from this table (http://aje.oxfordjournals.org/content/152/11/1056/T1.expansion.html) that women in the lowest quintile for fat intake were still eating 28.7% of their calories as fat, and 11% of their calories as saturated fat. It’s hard to draw a direct comparison between percentages of energy and absolute intake, but 28.7% fat and 11% saturated fat are almost certainly much higher than Swank allowed for his patients. And those were the women in the *bottom* quintile! 80% of the study population ate more fat and saturated fat than they did.
So, it looks like even the “lowest fat” participants in the study were eating well above the levels Swank mandated for his patients. I’d guess that observational studies encompassing a lower saturated fat intake might detect something more significant! 🙂
I do absolutely fantastic on a starch and fruit diet. Got down to my ideal bodyweight of 160 effortlessly from a high on 210 and reversed my beginnings of anklyosing spondylitis, hypothyroidism and IBS issues. Low carb diet completely destroyed my health over the previous 6~ years and took a good 4 to reverse the damage done. Now I am seeing some amazing things happening. I encourage anyone with any health issues to try a low fat, low animal product diet.
Thanks Denise for putting together this massive article. I have read most of the literature from most of these people but finding it in all one place and with all the more obscure stuff is amazing. I don’t know what else you have planned but maybe take it further and cover some of the newer names that you previously mentioned and also the cultures that naturally eat a high carb,low fat diet.
I agree. IMO Low carb masks and exacerbates any underlying metabolic issues. The ‘Different Magic’ at the >65% fat pole is a black magic.
Zach, what about sugar crashes? Do you experience them? After discovering LCHF I realized that my afternoon sluggishness is anything but ‘normal’. It was gone the next day I eliminated sugar and starch. I don’t have weight issues (I switched to LCHF in order to get rid of my sweet tooth), so I’m trying to bring back carbs into my diet. But every time I go beyond a certain point, my afternoon drowsiness return. And I really hate it.
I crashed a lot at first when returning carbs into my diet and it slowly got better the more I pushed the carb limit. Dramatically reducing fat intake and becoming very insulin sensitive helped the most. Now I have zero crash and steady energy. My last meal was literally a 1lb loaf of fresh baked rye bread (organic rye, blackstrap molasses, salt, yeast, water) and quite o bit of blueberry jam and 16oz of apple cider with zero blood sugar issues. I can also fast without issue which some people claim they cannot do on a starch heavy diet.
Thanks for sharing your experience! Yes, so far I was only able to fast easily when I eat mostly meat, liver etc and non-starchy veggies (interestingly enough in my case diary, like cheese, caused food cravings so I had to ditch it). Still I have to experiment and find my sweet spot.
I’m not sure how long you have been eating low carb but I do believe it’s easier to fast and also less energy crashes because a low carb diet usually promotes a sympathetic dominant nervous system, relying on stress hormones to function. By design a low carb diet needs to rely on cortisol and adrenalin to produce glucose. Plus high amounts of meat can be stressful because of the high amount of inflammatory aminos. Also omega 6 will almost always be higher.
Anyway, this can feel great for awhile but in my experience and from lots of interaction on Internet forums, this takes a huge toll on the body. Mainly in the form of low thyroid, auto immune diseases, food intolerances, inflammation, trouble sleeping, insulin resistance and low energy.
I’m sorry, are you talking about LCHF or just LC? You mentioned high amount of meat. I rarely eat more than 80g of protein per day. The excess of protein makes me sluggish, just like carbs.
Also (olive and coconut oil aside) vegetable oils have the highest amount of omega 6, not animal fat: http://authoritynutrition.com/optimize-omega-6-omega-3-ratio/ So I can’t see the reason why I need to dump my butter and lard. Interestingly enough, although I also use coconut oil, I have to be careful, for my body doesn’t tolerate large amounts of coconut oil, while butter and lard is not a problem.
Anyway, I would appreciate if you give me the links on others peoples experience as well as scientific papers describing how LCHF affects cortisol and adrenalin. Because so far I’ve seen only positive feedback: LCHF, keto-, and even zerocarb folks all report a drastic improvement of dental health. Such unanimity makes me suspicious:) Thanks!
One look at Jimmy Moore’s latest labs speaks a lot about a decade on LCHF. Disregulated cortisol, low progesterone, low dhea, prediabetic hba1c, high fasting insulin, etc …. His wife now has hashi’s, “adrenal fatigue” and high fasting insulin. Everyone likes to ignore this living example or attribute the ill health to anything other than the diet.
http://livinlavidalowcarb.com/blog/potpourri-of-health-tests-on-jimmy-moore-in-may-2015/24818
I was wondering about him. He lost so much and looked so good for awhile. The last time I watched him give a talk he was really fat again. I think that happens to everybody if they go back to their old habits, I assumed he was no longer doing low carb. If a person doing low carb started gaining weight again why on earth would anybody keep doing it? I am a successful low carber, have kept the weight off for years and no longer do low carb, but neither did I go back to my original dietary habits either.
If you look back, JM looked the best in 2005 while eating Atkins maintenance (approx 150 gr carbs per day) + doing some exercise. He claims that stopped working for him and he continued to buckle down and low carb harder. Embarking on his nutritional ketosis experiment. His labs are all anyone needs to see how his health is not ideal. Not everyone attributes it to his diet. I’m not sure how you could not attribute it to his diet. A moderately low carb diet isn’t a bad thing especially in the short term but a decade of this hasn’t made him a healthy man. Can’t be a coincidence his wife is right behind him even developing an autoimmune disease which Dr. Schwarbzein discusses in the video talk I posted.
Thanks for the info. I do not understand why people don´t change something that is going wrong. When I stopped eating low and moderate carb and added a lot of fruit to my diet, I could feel my body sucking up the nutrients in fruit and demanding more. That told me it was time to give up the low carb high fat.
Rebecca, out of curiosity, how did you feel that? thanks.
I felt better and better over the years I did low carb high fat, but after awhile I really saw no more improvements. When I switched to a high carb low fat form of eating I feel just as good if not better, I feel lighter. I have plenty of energy, perhaps a bit more than I did with high fat. I still have a few issues I hope to improve. The main one sleeping. I am going to a starch based diet with fruit and veg. It is too soon to tell if it will bring me more benefits, but I believe in experimentation, and am giving it a go.
Oops I didn´t really answer your question. I guess it was just I felt like I could not get enough fruit, I felt like my body was demanding it. But not in the way people get cravings for junk food. I was easily eating at least 8 pieces of fruit a day, and sometimes more. It is really difficult to explain that, it comes from practicing listening to your body and feeling how it responds to everything you put in. It takes time and patience to do this but I think a lot of people do not really listen to their bodies. I learned it from my husband who has an amazing ability to feel how his body is working and how things affect it. He told me you just have to start paying attention and work at it.
Rebecca, thank you for the explanation.
If you`ve got 2 hours. This is a good talk. Dr. Schwarzbein walks through biochemistry and endocrinology to explain why low carb is a stressor. Jimmy`s labs reflect what she`s describing.
https://www.youtube.com/watch?v=6qUSvzUj6jo (part 1)
https://www.youtube.com/watch?v=rm0MG_zYIdQ (part 2)
Thanks! I skimmed her presentation and it looks very intriguing and informative. Totally agree with her that “losing weight” shouldn’t be the starting point of the ideal diet (if such diet exists at all).
I didn’t have weight issues though. But as a long distance runner I developed unhealthy addiction to carbs and sugar foods. But it’s funny. Because she mentions that a LCHF diet can cause insomnia in the long run. For me it’s quite the opposite. The moment I reintroduce substantial amounts of carbs, I immediately get insomnia (not to mention sugar cravings and, paradoxically, the desire to drink more coffee). I wonder why is that.
Trina, I watched the presentation and also checked her book The Schwarzbein Principle. There she says how much carbs you need to eat depending on your activity. Still, she recommends more than 75g of carbs only for very active people. Now, I’m confused: what does she mean by low-carb diet? In other words, how low is low?
Also, in her book and in the presentation she mentions coffee a lot. May be it is the main culprit of high cortisol levels and not low-carb per se. I know a lot of lchf and paleo folks encourage you to drink coffee and even drink the so called bulletproof coffee, and it doesn’t make any sense for me. So Schwarzbein gave me another reason to quit my coffee habit.
She wrote a second book (http://www.amazon.com/The-Schwarzbein-Principle-Transition-Regeneration/dp/1558749640). She wrote that people read the first book and took carb restriction too far. Insulin serves a purpose. The people who seem to suffer ill health are the ones who appear to take low carb to the extreme. If glucose is extremely scarce, you need extreme insulin resistance to conserve it. I’m not condoning her diet, just found that 2 hour talk very interesting from a science stand point.
Just watched this – pretty amazing driving down blood sugars, drives down insulin and drives down nitric oxide. They have known this since 2007. This explains why low carb high fat only works for awhile. Fascinating how she makes the biochemistry understandable. Finally a real reason why carbohydrates are necessary.
I wouldn’t be so fast to state something “finally”. We’ve heard so many final statements already (“meat is murder”, or “fat is your savior”, “you need to run” “actually, jogging is bad for you, go sprining!”), and I’m sure this is not the last one.
Here’s, for example, a totally different opinion: http://www.diagnosisdiet.com/food/carbohydrates/ I wouldn’t go as far as eliminating carbs completely but Dr. Ede is good at questioning our presupposition about healthy diet (like “veggies are good for you” http://www.diagnosisdiet.com/food/vegetables/).
When I said finally, I was using it as an expression meaning – at last I have heard an explaination that makes sense to me. I did not mean it is the final word on the topic – I don´t know why you interpreted it that way.
Dr Ede is a psychiatrist. Not sure what her full understanding of the endocrine system is. She’s also written some posts about wanting to sing to her keto diet so … lol.
I was replying to a link I followed in one of the comments it was to a talk by Dr. Diana Schwarzbein who is an endocrinologist. This is the link to a 2 part talk https://www.youtube.com/watch?v=rm0MG_zYIdQ – this is part 2 it is all about the biochemistry of metabolism. She talks in one part about research that was published back in 2007 where they learned more about insulin metabolism. There is a pathway in the body called P13K that is important in insulin metabolism – basically what happens if you do low carb, or ketotic diets they drive down blood sugar, they drive down insulin, and that drives down NO nitric oxide and you do not want to have this. NO is vital for health. This to me is a very convincing point that doing low carb when your metabolism is already damaged will definately sooner or later make it all worse, and a healthy person could cause theirself metabolic damage eventually eating low carb becasue of how the P13K pathway works. This is published scientific fact about our biochemistry – I think that makes it something we should pay attention too. It could also explain why Dr Atkins died being 60 pounds overweight with severe heart disease, and why Jimmy Moore is now fat again and unhealthy. It still does not tell us what is the best diet to get healthy and stay healthy and vital into old age, but I do believe it is an important piece of the puzzle.
Notice also the effecsk of very high methylglyoxal from long-term low-carbing.
http://freetheanimal.com/2014/11/hormesis-missing-glutathione.html
There are other markers on his labs that should be of big concern (his falling total protein, albumin and globulin levels).
Storage of fat in the wrong places is the underlying cause of atherosclerosis, type 2 diabetes, NASH and so on.
You can’t store fat without dietary fat.
You can’t store fat without dietary carbohydrate.
Which diet is easiest to achieve, most digestible, most appetising, and supplies most of the nutrition you yourself require?
Also, which diet best supports cognition and emotional well-being?
Probably the diet with B12, long-chain PUFAs, and the potential for ketogenesis.
I commenced a very low fat raw food diet four years after puberty, in the context of undiagnosed IBD. It seemed enlivening akin to magic vs the SAD, initially, and remitted the disease. In subsequent years, the main therapeutic value, after depressing insulin(probably), was the ‘control’ of autoimmunity by anergy. This came with deficits: B12, anemia, D, cachexic musulature (despite daily exercise to quell high anxiety), and a general sallow malaise aeons from wellbeing.
In this period I’d noticed a calm reserviour of energy after walking ten kilometers, past the barrier of exhaustion… and this I sought. A diet that facilitates ketogenesis generates this state as default, also resolving the perpetual ‘malabsorbtion’ issues with B12 et. all. It has generated a state less compromised, that has facilitated the reversal of a considerably affecting uveitits, which I did not even know I had such was its constancy.
Yes, ultra low fat whole food diets disarm autoimmunity, especially if tending to underfed, but I’d like to know if there are mechanisms at large beyond the anergic?
Another good source of information is from John McDougal MD. He says the healthiest diet is a starch based diet. As a standard medical Dr. with at least 40 years of experience his website and a book called the Starch Solution are fascinating. Just google him and check it out. I have done vegetarian and vegan in the past looking for that magical solution they promise and nothing happened but made my blood sugars worse. Then I did very low carb and high fat and it worked like magic for awhile. I am now trying the McDougal approach and I like it and my blood sugar tolerates it. We all need different things in our lives at different times and the only way to find what works for you is to experiment with different diets. And what works at one point maynot be good forever, you have to change as things change. And all the chatter about oh it has to be scientificly validated is just crap. Science has told us so many things that are now proved wrong. Give me case studies where I can see the results in real people, if it works for others there is a chance it might work for me. And any diet no matter what kind still needs to be tweaked to meet an individuals needs and tastes. Dr. McDougal has the evidence his approach definately works for his patients. I am fascinated by his concepts of a starch based approach to good health and normal body weight.
Denise,
you have said in your analysis of Swank MS experiment that the diet allowed for “60 to 90 grams of protein daily, mostly from fat-free animal foods”. It’s possible that MS patients used to eat more protein then the above amount and protein reduction was at least somewhat responsible for their improvement?
Hi Anna,
It’s possible that protein reduction played a role for the MS patients, but there’s no way to tell from Swank’s data, as far as I can tell! I’d consider it unlikely that protein intake went down much, because the animal food content of the patients’ diets shifted from items that were higher fat/relatively lower protein to items that were almost pure protein (skim milk, lean meats and fish, etc.). If anything, protein intake may have gone up some. Just speculation, though. I’ll check some of his papers to see if he recorded his patients’ initial protein intake anywhere.
Denise,
I have found an interesting point about the Morrison study from the book below. He was giving his patients additional vitamin C supplements, about 150 mg a day. The author claims that vitamin C was responsible for their improvement, not reduction in fat. I’m not sure if I buy the vitamin C theory, but what if there was some other unknown variable introduced that he didn’t include into the study for some political or other reasons?
https://books.google.com/books?id=4trIQScMS_UC&pg=PA106&lpg=PA106&dq=lester+morrison+diet+low+fat&source=bl&ots=Nlr0Y8PBBH&sig=GhLn8jopjTdppnqw5x1aPVvX6-s&hl=en&sa=X&ved=0CDgQ6AEwBGoVChMIhYT60qq0yAIVypQNCh2ftwG3#v=onepage&q=lester%20morrison%20diet%20low%20fat&f=false
And I found on another blog that he was indeed using a lot of supplements and involved CR:
“Along with a number of vitamins and minerals, Morrison prescribed supplemental wheat germ and brewer’s yeast because of their high B-vitamin content, the latter also containing the important antioxidant mineral selenium. It is now well-recognized that certain B-vitamins lower blood levels of a potentially atherogenic substance known as homocysteine, while a small pilot trial found a marked reduction in mortality among CHD patients taking selenium-rich yeast on a daily basis”
http://microbialinfluence.com/Vegan2/study.html
And high-protein diets can cause appetite suppression.
Even you said that “the low-fat group saw some initial weight loss—an average of 21 pounds for men and 17 for women during the first three years, but with no additional changes during the rest of the study—whereas the control group remained weight-stable the whole time.”
So perhaps the weight loss or CR or supplementation should be credited instead of LF?
Hi Anna,
Interesting finds! Morrison definitely did a lot of work with supplements (most notably chondroitin sulfate), and it’s definitely possible that other factors beyond fat intake influenced his patients’ results. If his low-fat study was the only one of its kind yielding the results it did, I’d be more hesitant to ascribe the therapeutic effect to fat reduction — but the consistency of very-low-fat programs (with or without supplements, whole foods or not) improving cardiovascular disease, combined with the mechanistic studies I’ll be exploring in Part 2, makes me think that fat played a significant role.
I do think weight loss and a reduced calorie intake (even if it happened spontaneously in his patients rather than deliberately) were confounders for his study. Thanks for your comments! 🙂
I’d recommend reading up on Linus Pauling’s theory on heart disease, which ties together effects from both vitamin C and saturated fats. The theory is that in the absence of adequate vitamin C – and “adequate” was several grams a day – to provide the necessary reducing agents to build connective tissue for arteries, saturated fat deposits provided a backup mechanism for reinforcing blood vessel walls. Having neither might eventually result in hemorrhagic stroke.
Psychohist, in the study they were only given 150 mg of vit C, nowhere near a few grams that L Pauling recommends and longer term saturated fat reduction didn’t seem to cause a spike in stokes…
perhaps CR produces/reuses some other antioxidants that can replace vit C/sat fat combo?
Denise, next up Nathan Pritikin diet.
A few points:
1. Again, protein reduction could have had some effect. In fact, cancer and mTor pathway are related.
2. Caloric restriction and/or weight loss could not be ruled out. Just because they were eating “ad libitum”, doesn’t meant that this restricted LF diet doesn’t cause spontaneous CR or activate the same pathways as CR, especially coupled with low protein intake.
Another interesting point is that LF diet leads to a reduction of fasting insulin, similar to LC diet. And a reduction of insulin correlates with various health improvements (according to your posted studies as well as others). So fasting insulin seems to be a good across the board marker of health.
Thanks.
And the same applies to Esselstyn’s study. His diet was most likely naturally very CR diet. “Whole grains, legumes, lentils, other vegetables, and fruit comprised the major portion of the diet.” “Initially the inter- vention avoided all added oils and processed foods that contain oils, fish, meat, fowl, dairy products, avocado, nuts, and excess salt. Pa- tients were also asked to avoid sugary foods (sucrose, fructose, and drinks containing them, refined carbohydrates, fruit juices, syr- ups, and molasses). Subsequently, we also excluded caffeine and fructose.”
Click to access JFP_06307_Article1.pdf
So, the bottom line for me is that Caloric Restriction is a major possible confounder for most of the studies you’ve mentioned. On top of this, outright protein restriction for many. Falling fasting insulin levels are robust markers of CR, confirming my point.
For me, CR (including protein restriction) comes out as winner. It seems to matter much less LC or LF, whole foods or processed foods, IF + any diet. Instead, CR vs excess calories is where the vast majority of benefits lies.
Thanks again for a great blog post dispelling many misconceptions about carbs.
The first big point made in this blog is that the magic happens on either end of the scale – i.e. the scale of LCHF – LFHC. We have two different metabolisms, one for carbs, and the original one for fat/ketones. Problem comes when trying to run them together – esp eating fats when insulin present (needs proper explanation, bear with!).
If one eat carbs in isolation, the insulin – fat conflict isn’t there, and metabolism is relatively happy – for a bit – at last its not too toxic. I didn’t say it was very nutritious, but the body will survive this situation better than the toxic case of insulin and fat together. So HC diet shows better than a mix….
Paleos didn’t have fridges and corner stores. hey didn’t eat a “balance diet” on each plate. They ate a kill, then went a few days on nuts and berries etc. Food combining stuff.
So in fact we (most of us) can eat both carbs and fats – separately. When I say carbs, I mean real carbs, like veggies. The question how far apart in time – is it lamb for lunch and salad at night? I think the minimum period is enough to get the insulin down after the carbs. Admittedly some carb meals won’t raise insulin substantially.
For my money, LCHF (<25g carbs per day) still best option for most, especially insulin resistant people. I accept you could stay alive and somewhat protected from CHD on HCLF (real food options) but would not be properly fed, perhaps unless suffient DHA ingested.
So for me the Taubes/Teicholz models still completely valid, with the new emphasis of not mixing carbs and fats!!
There are likely other issues to do with gut flora and mixing carbs with fats, it just was't meant to be done this way….
This is a difficult topic for me. I am Asian, I used to be a vegetarian, and I had been basically eating the rice diet (rice, sugar, fruit) most of my life when I got diabetes. The switch to a LCHF diet reversed my symptoms (high blood sugars). Naturally I would like to revert to my previous diet, but my blood sugars will skyrocket.
I am a type II diabetic and did not think I could eat high carb. I did very low carb and high fat for about 5 years, and that helped a lot to control my blood sugars. Then I did a few days of liquid fasting a week for a couple of months and my blood sugars got even better. But then I just was tired of it I don´t even really like meats or poultry or fish. So I started eating lots of fruit, then I found this blog and that led me to an interesting article about a potato diet that goes back to 1849. And another blog led me to the works of John McDougall MD. He advocates an almost no fat starch based diet. He is a standard doctor and he treats patients with diabetes with it. Google him he has a website. And a recent book called the Starch Solution. I am starting to eat like he says and my blood sugar tolerates it with about the same medications I had to use eating lowcarb highfat. I just did not believe in a million years I could eat this way. But when you cut out all the fat and animal proteins your insulin functions differently. And starchy foods, fruits and vegetables all have amino acids and very small amounts of fat. Potatoes have all the essential amino acids. People can live and be healthy on potatoes alone, which has happened in the past. Check out McDougall´s stuff and maybe you will find the answer to let you go back to eating the way you want.
I could try this but I don’t want to go on meds.
I wonder if the rice diet was having a similar effect to an elemental diet, which are basically amino acids and dextrose. fat is added, but they recommend you start very low fat and increase according to tolerance. Elemental diets have been shown to correct sibo better than antibiotics. Correcting a gut microbiosis could possibly have the health benefits you describe. Rice and fruit wouldn’t be a complete protein, but it might be a reasonable whole food version of an elemental diet, with the addition of enough resistant starch to keep big intestinal flora alive during the purge. So, would a diet of similar macrobiotics but different starches be as successful, like, say, bananas with processed fructose? I thought it was interesting that bananas were limited. In other words, is the low fat aspect the crucial one? I remember something lately about a high fat diet not doing good things for leaky gut… but don’t remember the details… And what about fat soluble micronutrients over the long term?
When I had SIBO, IBS and leaky gut, I healed over the course of 2 1/2 years on the GAPS diet. It involved high fat, meats, well cooked vegetables, yet restricted many forms of carbohydrate like all grains, starches, most legumes, unfermented dairy, sugar. Eliminating the starches and sugars and consuming the fat and proteins of GAPS was immensely soothing to my body, mood, and mind. I don’t believe high fat is not good for a leaky gut, unless of course the fat is in the form of PUFAs. I healed on a high fat diet, much to my gratitude and relief.
Generally speaking, Minger is a charlatan.
Evidence to support your insult would be appreciated.
Apparently, generally speaking, Cynthia is a troll
And you are a troll, generally speaking
Name calling is totally inappropriate. This was an opinion piece. And we all have opinions, and a right to form our own opinions.
When calling someone a charlatan, it seems appropriate to furnish grounds unless you’re a troll
My obese, lifetime non-smoker grandfather had a heart attack at age 55. He went on the Kempner rice diet, did great for the next twenty years, and died of a head injury from a bicycle accident at age 75. He ate rice and fruit for breakfast and lunch and meat and vegetables for dinner. My grandmother was distressed that his last meal was “plain rice”. Anecdotal data, but….
Maybe we are over analysizing this. Perhaps our bodies don’t care how we get our calories, just that we get the right amount. Just not too much or not too little. If we get our appropriate nutrients and avoid any serious toxins, our bodies are able to get along just fine. The Rice Diet usually causes initial weight loss then it plateaus. Atkins often the same. Gastric bypass surgery as well. Satiety meets up with healthy calorie intake. Poor diets have low satiety and lead to over eating and eventually energy overload. Insulin resistance beings and the path to chronic degenerative diseases is set. Restore energy balance and IR goes away and disease conditions and risks drop. The middle ground diets can work if we don’t mess up our satiety signals. The French Diet, the Paleo Diet and the Mediterrian Diets do work because they has healthy satiety. Junk food in the Western Diet defeat our energy balance mechanisms. The processed food is designed to defeat normal satiety signals. War ration diets work because scarcity solves the overconsumption problem, willpower is not required.
I read a book years ago where people had benefits from eating nothing but brown rice. People magazine 8/13/79 has an article on the Pritkikin diet
I have gone back and forth with fruitarianism and paleo over the last few years. I have felt amazing on fruit and pretty good on paleo. Then I found out that Arthur DeVany, the grandfather of paleo, just had hip and knee replacements in his early seventies. And Janette and Alan Murray, both low fat raw vegans, ran 366 marathons in 366 days at about the same age. It was a no brainer from then on.
I think what is really important is that healthy diet is either low in fat or low in carbs,
Is there any studies on a 50/50 high fat high carb diet?
Thanks for all the work you put into this. And for your impressive willingness to admit you were wrong. That’s rare. I look forward to the next installment. People’s trollish comments amaze me, especially about your writing. You are a fine writer and I love your sense of humor.
Hi Denise,
I appreciate your research. Do you think some of the differences could be due to genetic differences. I have tried low fat and vegan diets and failed miserably. I switched to a high fat/low carb diet and feel great and look a ton better. I don’t think one size fits all.
Low-carb-high-fat works fine to detox from years of low-fat-high-carb diet.
It is a transition period and gives excellent results in terms of health and weight loss, both are commonly mistaken as the proof that the perfect diet has been found. But once the sugar detox is achieved, a “reasonabe-carb-diet” must be followed.
What low-carbers don’t know is that prolonged periods on a ketogetic diet can effectively cause insulin resistance (yes, the same as high-carb).
Some of us know that perfectly well. However, the insulin resistance is not accompanied by high blood sugar, which is the part of metabolic syndrome that is damaging. Excessive insulin sensitivity can cause hypoglycemia on a low carb diet, so the body adjusts its insulin sensitivity accordingly.
So you’re saying that the Japanese need to detox? You can’t be referring to Americans, who both on a calorie basis and a macro percentage basis, eat one of the highest fat diets on the planet. If lots of fat is what detoxes a person the SAD is doing a bang-up job.
First time reader, and wow that was a long first read! I’ve been doing research on veganism/whole food plant based diets and one of the vegan forums linked to this. One thing I can definitely respect when trying to find the best information is someone who isn’t afraid to correct themself or say they were initially wrong on a certain subject. Anyways, thanks for the words, I’ll be sure to read more.
In a Japanese experiment involving 100 million people, a diet of mostly rice, fish and vegetables yielded the longest life expectancy on the planet.
The japanese love fish rice nad vegetables, but to say its mostly? thats a bit of an exageration. They have wonderful pork, chicken, beef dishes. Deep fried pork in Japan is absolutely fantastic, let alone their tempura style seafood. Rice is typically a side vs a main.
But, most of their food is extremely high quality, fresh, well cared for. Not mass produced garbage – although they have lots of this as well – fantastic selection of candy.
This is my favorite article on thie subject, which I read back in the day. James Fallows describes what happened diet-wise when he and his family moved to Japan for an extended writing assignment.
http://www.theatlantic.com/past/issues/86nov/fallows.htm
Basically they were hungry all the time and had to go to fast food joints to get fat fixes.
What people in the HFLC community don’t get is that the SAD IS a high fat diet. The Japanese eat (or ate) a low fat diet. Not Americans. Ever.
Oh my Denise, you surpass your previous works in sensationalism but you are lacking in examining your own logic I think, on at least this one point. You say that you are:
“Uncomfortable, because it demolishes my long-held rationale for why low fat, veganish diets can be successful: that they work because they involve switching to whole foods (Kempner’s sure didn’t!); that they work because they reduce refined sugar and starch intake (the very lifeblood of the rice diet!); that they work because they increase disease-fighting plant compounds (nary a vegetable to be seen under Kempner’s strictest watch). Let me go on record here: I TOTALLY stand corrected!”
Ha! For the sake of keeping consistency and power in this one article, for the sake of making it more thoroughly convincing you just gave up a perfectly rational and quite healthy stance and declared that you “stand corrected”? Where is your normally solid logic? You are so obviously selling out in order to sound convincing in an article here that really matters minimally toward health.
To wit: ONE SUCCESSFUL DIET DOES NOT DEMOLISH ANOTHER SUCCESSFUL DIET. One successful diet rationale (Kempner’s — successful short term — nothing proven long term, mind you) likewise does not demolish the rationale you had maintained to support a whole food, sugar poor, vitamin/enzyme/polyphenol rich diet. Here I am talking about essentially a typical Blue Zones diet, which unlike Kempner’s diet, has been proven to provide health over a great number of years.
If you wish to stand corrected on something regarding this issue, please consider standing on this correction: success of one plan does not necessitate the failure of another.
I hope when you produce your promised next article on this line, you manage to step aside from the silly notions of percents required for macronutrients. I think your original line of thinking was much more proper, that nutrition depends more on micronutrients than macronutrients, if you want a plan that lasts decades. Obviously you have proven that percentages of macronutrients matter little, just as the other side has proven this to their own satisfaction when they work to minimize carbohydrates.
I hope you can dismiss yourself from going on at length on macronutrients and return to giving advice on how the aspect of veganism that manages to provide bodies with plenty of low calorie carbohydrates is a key to health, whether one is vegan, omnivore, paleo or whatever. I realize the sugar lobby can pour a lot of money into swaying important spokespersons to make statements where the word “sugar” is bandied about as part of a winning strategy. So it becomes even more important, if you wish to retain your respectability, to choose your words and phrases carefully.
You redeem yourself by following with the discussion of Morrison and Pritikin, both of which emphasized a fiber rich diet. Where I think your 10% fat threshold has value is that it allows a maximum of vitamins, minerals, enzymes, and phytonutrients. So I only wish to make the point that so many articles on macronutrients are formulated such that the reader focuses on the percentages of macronutrients, and not on the particular nutrients involved. Vegetable starches are less nutrient dense than greens. They are not something to consider interchangeable within the “carbohydrate” component of a diet. But this important point often, (usually even), is lost in Paleo diet discussions, just as it was lost in Atkins Diet discussions. And of course it is lost in the beginning of this current discussions.
On Roy Swank’s findings, and your go at “alternative explanations”, I’ll add one. Since all participants were allowed oils, which most probably included refined, damaged PUFA, there is the chance that the human body burns saturated fat (and MUFA) in preference to PUFA, and that therefore, the PUFA is more likely to be stored (since so little is actually used by the human body for membranes, etc.) and the stored PUFA is actually what causes the MS, not the saturated fat that forces the storage. I’m thinking Ray Peat might vote for this possibility. I know you pointed out that PUFA consumption was inversely related to the saturated fat, but regardless, if there is an excess of PUFA, over some arbitrary limit, and that limit was reached by all participants, even those with the lowest PUFA intake, then the inverse relationship you spoke of is not of consequence, That is, your “swampland principle” may also apply here, making the percentages of types of fat a moot question if the PUFA just happens to always exceed the limit that causes the MS.
Best of health, and take, in some form or another, some vitamins, and not just with a grain of salt! You need to spend a little more time examining the integrity and substance of your articles, and less time on making them carry a clear, beautiful, though hollow tone.
patronizing
I must have skimmed over this part.
“Uncomfortable, because it demolishes my long-held rationale for why low fat, veganish diets can be successful: that they work because they involve switching to whole foods (Kempner’s sure didn’t!); that they work because they reduce refined sugar and starch intake (the very lifeblood of the rice diet!); that they work because they increase disease-fighting plant compounds (nary a vegetable to be seen under Kempner’s strictest watch). Let me go on record here: I TOTALLY stand corrected!”
This is the crux of the matter. That is, the low fat diet works not because it’s a more wholesome diet overall, but because it removes the fat.
Thanks to Glenn for calling this out!
Hi Glenn,
Thanks for the candid comments! I appreciate the opportunity to clarify some points.
Ah, I may not have communicated my point very well here. I’ll rephrase: I used to assume that low-fat, plant-based diets worked *only* because of the removal of refined sugar and starch, the emphasis on whole foods, the increase in phytochemicals, etc., and that the reduction in fat content was irrelevant — something prescribed unnecessarily by the “plant-based diet doctors.” I still believe all those factors play a major role in making these diets health-promoting (especially long term), but the studies I explored in this post suggest very strongly that fat reduction to about 10% also has powerful, independent effects for specific disease states. The diets described here (especially Kempner, Morrison, and Swank) were still successful even when they included sugar, refined starch, and/or a low micronutrient content. Likewise, Swank and Pritikin found that the primary factor in whether their patients were successful long-term was whether or not their fat intake increased.
I agree! In fact, if you missed it, this is what I wrote elsewhere in the post (emphasis added): “For the past few years (five? six? seven ate nine?), I’ve asserted that the success of plant-based diets is due to their whole-foodsness (eliminating processed junk, refined sugar, and refined flour), their low PUFA intake regardless of total fat (with the implication that higher non-PUFA fat consumption would be hunky dory), and the increase in other health-promoting behaviors that come with making a big change in the foods you eat (more exercise, less drinking and smoking, less couch-potatoism, etc.). I still think those things are relevant. But I now believe I dismissed the role of low total fat intake before I gave the data a fair and thorough analysis.”
Nope! This whole series is about why macronutrients *do* make a difference, but why the effects of macronutrient manipulation only become obvious at the extreme ends of the spectrum. The crux of the discussion isn’t what’s best long-term for the majority of the population; these are therapeutic diets, used to address diseases that are developing or already in place. The next post will offer mechanist explanations for why metabolism changes at very low fat intakes — you may find these more convincing than the studies discussed in Part 1. (I do!)
Interesting theory, but not supported by the data. Please read the Swank section again. His patients achieved dramatic results for several years before high-PUFA oils were allowed back in the diet.
I hope that helps clarify some points! Thanks again for your comments. I do hope you stick around for Part 2, because it may change your mind on the irrelevance of macronutrient changes. 🙂
Thanks for clarifying some things Denise. Yes, I had missed your mentioning that these are only therapeutic diets.
On the issue of whether macronutrients deserve continual emphasis in articles, I’ll step aside for now and wait to read what your next installment brings. I still have strong feelings that without EXTENSIVE disclosures before, during and after any article on macronutrients, the audience, being human, may often go away with distorted perceptions of the importance of having viewed foods by macronutrient category.
Regarding the Swank discussion, I find that I also did not explain my point of view carefully enough for you to understand what I meant, and so, and especially in light of several recent comments on the Swank portion of your essay, I’ll state my point again, but differently:
I had said that “there is the chance that the human body burns saturated fat (and MUFA) in preference to PUFA”. Actually, it is well known that this happens. MUFA and saturated fats (SF) are the preferred forms for creation of energy. Probably because in nature, there never is a great abundance of PUFA in the food supply, outside the consumption of nuts (and yes, in recent history, grains). However, SF is needed continually for building new cell membrane (just as is PUFA). It is also the fat preferred not just to feed heart muscle, but to be stored upon the heart for use in times of stress, as when fats are in short supply as free fatty acids via the blood stream. There are other ways that saturated fats are preferred over the other fats as can be found in this WAPF article which can provide references:
http://webcache.googleusercontent.com/search?q=cache:http://www.health-report.co.uk/saturated_fats_health_benefits.htm
Moving on now, to PUFA.
You had countered my original theory with:
“Interesting theory, but not supported by the data. Please read the Swank section again. His patients achieved dramatic results for several years before high-PUFA oils were allowed back in the diet.”
I didn’t read the article that way. I don’t know what Swank’s actual description of the diet was, but what you said was:
“Very low saturated fat (10 – 15 grams per day, maximum)”
“Small amounts of polyunsaturated vegetable oils and fish oil (10 – 40 grams per day)”
So I am only referring to the PUFA and fish oil that was allowed in the original therapeutic diet. As you can see, there is an allowance for more PUFA via vegetable oils than there is even for SF.
So to make my point more carefully:
Considering what we now know about excess adulterated or oxidized PUFA, especially as manifested in commercial “vegetable oils” and what we know about the rapidity of oxidation of fish oils (studies have shown that up to 80% of fish oil supplements show rancidity in newly opened sample bottles), and what we know about the detrimental effects of these ruined oils on the human body, especially to cellular respiration and circulatory endothelial tissue (Brian Peskin has hundreds of references if you need some), it becomes crucial to not consume any ruined PUFA, and to realize that we also shouldn’t be consuming any significant excess of even pristine PUFA (as from super fresh, relatively unheated veggies, meats or eggs) over what is needed to keep our cellular metabolism healthy. Yet Swank allowed liberal consumption of these oils by his study participants. So how did he improve their conditions? They may have eaten as much PUFA as they had before being inducted into the study. What changed was the consumption of SF. And SF is considered dispensable by most (please see below for my perspective). But when you reduce SF via reduction of *animal products*, you also considerably reduce MUFA consumption. Be patient, I’m almost ready to make a point….
Thus his successful cohort, in spite of being allowed reasonable amounts of PUFA, even unhealthy PUFA as described, made remarkable progress in relieving MS symptoms. Ah, I think I’m ready now to make this point:
All I am pointing out is that since saturated fat has a definite demand in the human body with respect to non-metabolic function, just as does PUFA, when you reduce SF to a certain low level, you are squeezing it’s supply so low (and probably also the MUFA supply) that it no longer can be the preferred source of metabolic calories, but must be almost totally pressed into it’s more essential roles of providing cell/mitochondrial wall structure, etc. But at the same time, an excess of PUFA over what is required for it’s essential functions, must now fill the void to provide fats for cellular metabolism, not just to the heart, but to all cells any time there is a need for energy that glycogen and glucose can’t supply. This situation that Swank has brought about insures that not only will the dangerous, oxidized PUFA that he still allows his subjects to use in almost “normal” quantities not be utilized in cellular and mitochondrial membranes, but that possibly any PUFA they have stored in fat cells that is also already oxidized will be released to be consumed as fuel. We may just have a *PUFA purge* going on here! Thus, in effect, his diet, though emphasized as “low in SF”, is actually a cleanse of the more probable cause of MS. He is possibly getting rid of damaging PUFA by just burning it up.
Don’t take this to be a claim that PUFA directly causes MS. I only want to point out that ridding the body of toxins can help a condition in many ways. In fact, I think the point to be made about the Kempner diet is similar: What is most important is NOT that the diet lacks fat, but that it is essentially a FAST plus enough non-toxic, non-allergenic, non-inflammatory foods to keep a person alive. It is a cleanse. So your point that these diets are therapeutic I *only wish to emphasize*. They are not diets for health maintenance. Their magic is, not so much that they eliminated substantial fat, as that they are so restrictive on many levels that they function as a cleanse.
I hope this helps to clarify why I think the reduction in saturated fats showing success in the Swank protocol is possibly not due to reducing something that is damaging to humans (the saturated fat itself), but due to nutrient/toxin balances thanks to extreme reductions in total fats and a change in the percentages that were allowed within that reduced ration.
An aside: Dr. Terry Wahls pushes nutrient dense, fresh vegetables from the garden as well as the sea. She has refined a method that combats and reverses MS. What she doesn’t emphasize, but promotes regardless, is the consumption of what happens to be reasonable quantities of unspoiled PUFA that are contained in her preferred diet. She has effectively eliminated the ruined PUFA that Swank even still allowed in his diet. So I would say that where Swank HAD TO drop saturated fat very low to protect his cohort from the damage done by the ruined PUFA, Dr. Wahls may be able to accomplish the same effect without limiting intake of such oils as coconut oil. She is providing lots of micronutrients via her fresh, organic diet, and these include only fresh, safe PUFAs. So her diet doesn’t need the reduction in saturated fats. The fact that it is successful somewhat proves that the reduction in fats, especially the saturated fats, is not the key ingredient in whipping MS.
Thanks Glenn, that was very interesting. Enjoyed reading your comments about MS; also, you explained what I tried to- (but you did a much better job than I did)- about why the rice diet may have worked.
But I think you had it right in your comment on the rice diet effectively making the body “think it was fasting”, Morgana. The wartime diet, low in fats, and especially the rice diet, low in so many ultimately necessary nutrients, is so restrictive as to effect some of the same results as a fast. There’s going to be more recycling, and more use of “stores” of nutrients. But there’s probably going to be more disposal of toxins. Needed nutrients are not going to be provided daily and found in circulation. But they must come from somewhere. So especially if weight loss is present, as it is in every fast, recycling is raised to such a degree that while valued minerals and amino acids are preserved, the net effect is to leave unneeded substances (toxins, excess minerals, and even excess hormones – estrogen for example) without a home, and thus they are discarded. So your fasting theory seems sound.
I loved your well thought out comments. I would be curious to hear what people think about . T Colin Campbell, PhD and what he says about research and fats and protein in the following article where he villifies animal protein and not fats.
http://nutritionstudies.org/fallacious-faulty-foolish-discussion-about-saturated-fat/
Glenn, thank you for your well thought out theory and a detailed explanation of the relationship between SF, MS and Swank diet. I do think caloric restriction (of fast, as you call it) could play a much bigger role in alleviating many of the diseases then macronutrients percentages.
But, I have a question to you about the ratio of macronutrients. If I understand you correctly, you don’t think it matters much and doesn’t deserve much discussion. But what about high protein diets activating mTor? Wouldn’t this one macronutrient alone need to be at least somewhat monitored/discussed?
thanks.
Anna, I agree that percentages of macronutrients has a reason to be discussed. I just cringe though, the way it is often discussed, and especially shudder when percentages are laid down as mainstays of entire diet plans.
I don’t want to hijack the thread here, but you pushed me lightly, so I’ll respond a bit now, and I’ll wait for the next article to comment further if prodded, on what I called “the dangers of discussing macro nutrients without EXTENSIVE disclosures before, during and after any article on macronutrients”. Probably Denise will be mentioning a lot of what I have in mind anyway as she is very whole-food, micro-nutrient oriented.
But just for an example, as you brought up proteins. Specifying a blanket limit, or even range for protein without dozens of qualifications is of little use, and with the proper qualifications is a burden to consider, let alone track. As this current article shows, there are times when one can go without levels of fat that are considered healthy, all for therapeutic purposes. The same goes for protein or fasts would not work to one’s benefit. But then there should be disclosures regarding time limits for variations off the recommended range.
There were studies that proved that lowering protein intake below prior limits provided greater longevity. Then followup studies showed that just lowering the amounts of certain amino acids (methionine and tryptophan I believe) gave as much or more boost in longevity as blanket protein reduction.
http://www.ncbi.nlm.nih.gov/pubmed/8001743
Protein requirements vary depending on who’s talking to whom. A body-building blog will have higher levels, while someone talking type-2 diabetes may push for a much lower minimum for protein and even suggest abandoning muscle-building plans because protein utilization often requires more insulin than equal calories of certain carbohydrates. So, two considerations on proteins, but there’s no limit on what might be proper before one sets guidelines.
Better I think is to talk about nutrient density of foods, nutrient characteristics of types of foods (such as carbs). That style of discussion avoids having one reader translate “carb” to mean “Coke”, another “potatoes”, another “spinach”. As you can see, what these foods have in common as “carbs” is far less than their differences. One is essentially a simple sugar, one is a starch but with some significant vitamins and protein, and one is primarily a bunch of micronutrients but with almost decent amounts of protein and fat (if you give credit to it containing some PUFA weighted toward the omega-3), and with SLIM amounts of humanly digestible carbohydrate (relative to the bulk eaten), though there is considerable fiber that will easily take care of a population of colonic bacteria which will likely net out some saturated fat to the host as the fiber is consumed, not to mention more vitamins. These are all “carbs”? Do it still make sense to talk percent of diet to allocate to carbs? Be aware, this is just an opening salvo.
I was under the impression that it was difficult to “overeat” protein, and that people generally- when left to their natural inclinations- will eat a set amount of daily protein, rather consistently. There were some tests done on animals as well as humans, which were mentioned in the Perfect Health Diet book. (Of course, this may not be the case in people who are, for whatever reason, forcing themselves to go against what their body needs/desires). I agree that there are times when people may need more, or less protein; (I’ve noticed my own protein needs changing at times). But this is why carbohydrates or fats tend to be the “changeable” macro-nutrients in diets; lower carb generally means higher fat, or vice versa.
Glen, thanks for your detailed reply. Looking forward to more comments after Part 2.
@Anna – “But what about high protein diets activating mTor?”
Many studies show that amino acids don’t elicit a large and long-lasting mTOR response when on a low-carb diet. So, it depends on what kind of high protein diet.
Hi Glenn,
Thanks for clarifying your comments! I appreciate you taking the time to explain your theory further — it’s certainly very interesting, though I would need to do some research before commenting on its general plausibility.
Unfortunately, I think I also wasn’t clear enough in my reply (and perhaps in my blog post!). The 10 – 40 grams of PUFA weren’t allowed on Swank’s diet for the first two years of the program. Basically, people started enrolling in his program in 1948 – 1949. Until 1951, the diet excluded all vegetable oils and fish oil, along with that sharp reduction in saturated fat. It was only in mid-1951 that Swank allowed his patients to add back those PUFAs. Here’s a direct quote from his “Fat-Oil Relationship” paper:
“From 1949 to mid-1951, (saturated) fat intake, which before entering the study had averaged ~125 g/day … was reduced to 20 – 30 g/day. … In 1951, butter fats and hydrogenated oils were eliminated, and animal fats were limited to 15 g/day. Five grams of cod liver oil, and vegetable oils that remained fluid at room temperature were added and allowed to vary from ~10 to 40 g/day as desired by the patients.”
As you can see in the ‘exacerbation rate’ graph in this post, patients already saw dramatic improvements in the first year of the diet before PUFA-rich oils were added back. The addition of the oils didn’t seem to either help or harm the patients, apart from subjective improvements in their energy and hair and skin.
I hope that clears it up! I’d be happy to send you Swank’s papers if you’d like to read them yourself — just shoot me an email through my contact form. 🙂
Great. Thanks, Denise! The study is clear to me now. Yes, you had implied in your response that PUFA wasn’t allowed, but since you originally published that it was allowed (the 10-40 grams statement), I thought it was allowed from the beginning.
Now though, it seems to me that I am left with the same perspective. Not supported by studies (as you say rightfully would be necessary for better proof), but a perspective that is actually a little clearer and easier to state as a theory:
Cutting out most fats from a diet to cure MS may not be as critical as cutting out all refined PUFA. If that’s what Swank did, that by itself is possibly sufficient to bring remission. If we’re assuming that low saturated fat did the trick, it’s just as easy to assume (and more logical, based on percentages reduced – zero vs 10%) that removing ALL refined PUFA did it. Cutting out all recognizable PUFA from “vegetable oils” is significant in my estimation. PUFA has an essential role as the only source of prostaglandins, and a critical role in cellular metabolism, yet, as Brian Peskin continually writes and refers to studies to back his writings, if one’s cell membranes are substantially occupied by oxidized omega-6 instead of healthy omega-6, the whole function of the linoleic acid is thwarted. Cell walls no longer transport oxygen or other nutrients in and out at optimum rates, and prostaglandins can no longer be supplied in ideal amounts.
Click to access CAMB-Fish-Oil-Fallacies-Report.pdf
So assuming the participants in Swank’s study had been consuming adulterated PUFA via “vegetable oils” or foods fried in such oils, and they had had these oxidized PUFAs taking the place of healthy, unoxidized PUFA in their cellular membranes, the elimination of all ruined PUFA from the diet allowed the disposal of the ruined PUFA over time, when cells were replaced. The grains, dairy and even vegetables that still existed on the diet would have provided ample, unoxidized PUFA to be used in new cell generation from the beginning of the study onward, and over time almost all cells would again be functioning normally regarding the dependence on PUFA. This would seem to be a gain for someone in any condition, not just MS. Why? Peskin claims that adulterated, or oxidized PUFA that has been installed into cell membranes actually has NO metabolic function. It is there, but not functional. It is taking the place of a figuratively “living, breathing molecule of PUFA” but is doing nothing. It is a hindrance rather than an aid to cellular respiration. So a person having a lot of ruined PUFA in their cells is actually suffering very severely from a lack of life-supporting mineral interchange, and if each cell that is in this condition can be replaced by a cell that has it’s PUFA dependent abilities restored, there will be a net gain for that individual. This would be the case for Swank’s MS sufferers over time as aged cells were replaced with better functioning cells, including neurons which have a slow replacement cycle.
If this is the effect that occurred in the Swank study, then without even considering saturated fat or it’s reduction, I’m theorizing that the purging of ruined PUFA over time will explain the remission of MS symptoms. Saturated fat may not be involved. Since oxidized omega-6 is already implicated in causing cancer and vascular damage and supported by studies to that effect, it’s not difficult to see it could be causative with respect to MS.
I don’t have studies, but people are starting to suspect:
http://ms.newlifeoutlook.com/swank-diet/2/
http://omegavia.com/omega-6-omega-3-and-oxidized-ldl/
As Peskin pointed out in my first link, as omega-6 intake goes up, presence of omega-6 in cell membranes also goes up. When intake is heavily oxidized oil, that is what you get in your membranes:
http://omegavia.com/oxidized-ldl-cholesterol-lard-less-lipitor/
Glen,
this is a good example of how focusing on macronutrients without paying attention to micronutrients can be confusing.
As you are pointing out, Is the issue total fat restriction, saturated fat or Pufa reduction?
thanks.
When will Part 2 be published?
Thank you.
What would you define a high fat diet to be? I see you say you eat lowish fat, but to your average dieter 45+grams of fat in a day is not low fat. So what exactly is high fat? I’m asking out of genuine curiosity, not criticism. I’ve read so many articles and they refer to either low or high but rarely define what that means. Truly not meaning to sound like an ass! 🙂
Hi roonitune,
This is a great question! And an incredibly difficult one to answer — largely because fat as a percent of total calories and fat in absolute grams will give much different pictures depending on total energy intake. For instance, a 45-gram fat intake will be a larger percent of total energy if someone’s only eating 1000 calories a day versus 2000 calories.
Personally, I define low fat as 10 – 20% of calories on a weight-maintaining energy intake; moderate fat, 20 – 40%, and high fat anything above that. Very low fat, I’d place at 10% of calories and lower on a weight-maintaining energy intake. So the absolute gram amount would have to be calculated based on what each person’s calorie needs are.
I have no scientific rationale for those brackets other than “it seems to fit.” 🙂
It’s like we are waiting for Desperately Seeking Denise Part II
I’ve been really confused for the last few days since reading this post. I ate a bunch of safe-starch and sugar yesterday and today, not because I thought it was a good idea, but because it wasn’t inherently evil anymore. What’s the difference between eating this and a low-moderate carb Paleo meal? I couldn’t find an answer, so I ate them.
Maybe I should just eat what I want, since obviously no one has any idea what the best way to eat is. Carbs are bad, but only with fat… Or… Carbs are best with fat (a la Perfect Health Diet)… Carbs make you fat… Carbs don’t make you fat… Fat makes you fat… Only calories make you fat… Lord help me!
My 78 year old Japanese mother reprimands me harshly for being so anal about food. It’s all in your head!, she says, No matter how many times I scold her for cooking with soybean oil instead of coconut and getting a quick burger and fries at the local Carl’s Junior, she just laughs at me and pirouettes away to her dance classes, her 12 hour days of working in the garden, etc… God, I wish I had her energy, leanness, joie de vivre. The last time I was that lean and felt that good I was partying every night and getting most of my calories from alcohol and street tacos.
Now I read labels obsessively, make every meal at home with the most expensive and esoteric Paleo-approved ingredients. I avoid social settings where food is served, so I don’t have to eat “toxins.” I’m totally isolated and neurotic, but at least I’m eating the healthiest way possible, right? Aargh! Maybe my mom is right.
Denise, if these studies are true, Kempner’s diet sounds way more effective (not to mention cheaper and simpler) than the Paleo diet. We should all be on it!
But… If we’re not doing an ULTRA low fat OR low carb diet, is this article even relevant to us? Do macros matter at all outside of these slim and hard to maintain magic zones?
I think the answers to your questions might be in the following links. I used to do the low carb high fat diets and I did get a lot of health improvements but it stopped working. You can argue either extreme end of the diet spectrum, all backed up with science. I have been doing a starch based diet for less than a week and I am already reducing my blood sugar medication, a clear sign my insulin resistance is improving. I like Dr. McDougal because he is just a regular doctor, not any of the other types that some people call quacks, and he provides all the information necessary for free, yes he does have books and money making things but all the information is free on his web site.
John McDougall MD – No added fats, starch based diet – His web site –
https://www.drmcdougall.com/health/education/newsletter/
Under the programs button there is one that says free McDougal program. Under the connect button there is a discussion board – where people talk about what happens with them, there is an area of success stories… etc.
This is a great video – explains very simply why some of us our fat – very intersting.
How to Lose Weight Without Losing Your Mind
Hi Robin,
I’m sorry to say it, but in many ways, your mom IS right! First of all, I’m sorry for any confusion or destabilized beliefs this post caused. I don’t want to usher otherwise healthy (non-diabetic/non-heart-disease-suffering) people onto unnecessarily extreme diets; this is more an attempt to explore the mechanisms behind macronutrient interaction, with the ultimate goal of applying the relevant findings to less rigid diets (in the form of macronutrient cycling, designing meals to improve insulin sensitivity, etc.). That’s what Part 2 is going to be about.
I will say that stressing out over food is often more harmful than the food itself. Especially if the anxiety about toxins is preventing you from enjoying life and harming relationships (I definitely went there as a raw vegan). The answer probably isn’t alcohol and street tacos, but on the net, health will generally improve if we trade small sacrifices of ‘food perfection’ for a wider range of fulfilling experiences and less self-imposed stress. 🙂
what if it’s really about the microbiome in the gut, and what’s operational in all the different diets is the change of diet which causes a change in the ecosystem of the gut. What matters is to make the change and reduced calories, not the particular macronutrients and their ratios?
Robin, I feel your pain. Your wonderful Mother sounds wise.
oh yey! does that mean I can drink Coca Cola again ?
Nope! check out this video –
This is a great video – explains very simply why some of us our fat – very intersting.
How to Lose Weight Without Losing Your Mind
Rebecca, please stop posting the same video over and over again. For some of us who are following the comments it’s a bit annoying to keep getting the same thing. We all got it and saw it many times over. Here is one just a few lines above your last post.
Thanks.
Sorry, I did not know if it was just going to the person I replied to or if everybody saw it. Thank you for letting me know.
Very interesting post! I read every word- (i.e., it’s just the right length)- and am looking forward to Part 2. Although I seem to do best with LCHF, and had terrible health problems when I tried high carb with very low fat, I totally agree with you that we can’t dismiss the evidence when it seems to contradict what we think we know. So I find this quite fascinating…..and it proves, once again, that different approaches work for different people.
Most interesting for me was the rice/fruit/refined sugar diet- (I just can’t wrap my head around that one!) I’m wondering about fasting, or caloric restriction (as another poster mentioned earlier on). For instance, maybe the reason wartime rationing seemed better for health was due to caloric restriction…..maybe it had nothing to do with a single “element” (fat, sugar)? And maybe, if the body is used to eating lots of fat as well as carbs, reducing one (in this case, fat)- makes the body “think” it’s fasting? (In a similar way to being in ketosis?). In fact, maybe any kind of sudden, extreme dietary change puts a stress on the body, which causes hormesis. (?) Could be a possibility, anyway.
Another thing I wondered about was leptin resistance. Possibly some of the overweight/diabetic people they tested overate because they didn’t feel satiety cues, and when they were put on a diet that heavily reduced fat and salt- 2 of the things that often make people overeat- maybe that helped to regulate their satiety signals? (Probably most people would be less likely to overeat sugar when it comes without fat). It sounds like it was a pretty unpalatable diet, so that may have had something to do with it’s success.
These are only just thoughts, I don’t really know…..therefore, I’m looking forward to hear what you have to say in Part 2.
This video is all about satiety signals and why people are affected differently.
How to Lose Weight Without Losing Your Mind
Attachments area
Preview YouTube video How to Lose Weight Without Losing Your Mind
Thank you for including this.
smokes…
When you said “When it came to blasting obesity, Kempner employed what he called a “rice-reduction diet”—the same protocol he’d designed for renal failure and hypertension, but with lower calories”
and posted the cool pictures, did it look great. Look how much weight they lost. 0.3kg per day… holysmokes.
Finally gotten around to looking at the paper
Lower calories indeed
The initial diet prescribed for most patients (“unmodified rice/reduction diet”) is a low-calorie (400 to 800 kilocalories [kcal]/day, average, estimated)
And then – Always, the prescribed diet is low in calories (less than 1,000 kcal/day)
Under 1000kcal for big fatties… no wonder they lost so much weight.
Craig, it doesn’t matter whether I wallowed in the Swampland or ate <10% fat. If you look closely at the results of these ultra-lowfat diets, average post-study BGs were on average WAY higher that the BGs I now enjoy, and eating infinitely more satisfying foods. Normal fasting BGs are 75–95. I was T2D in 2007, and since *normalized* my BGs with LCHF, averaging 90 mg/dL. Kempner's Rice diet did NOT, in the main, resolve diabetes. The average fasting blood sugar (FBG) for folks after 22 weeks of the Rice Diet was 155 mg/dL! That’s still diabetic! About the Pritikin diet, looking at the study Denise gives, (http://ajcn.nutrition.org/content/29/8/895.full.pdf , Table 2, pg 895), the average post-study FBG was 136–still diabetic! Same thing for a Pritikin 1983 study: post-study FBG average is 133 mg/dL. (http://care.diabetesjournals.org/content/6/3/268.short). If the other ultra lowfat diet studies Denise cited here discussed BGs, she didn't include that discussion in this blog post.
Your experience is interesting to me. To be back at 90 after being type 2 through a high fat diet is. Ot something I’ve come across.
How do you manage to eat such high fat yet low protein? I can’t think of mix of foods that would result in such. And presumably your not concerned re fats and CV disease?
Craig did you get my response to you I posted within the last 12 hours? That details what I eat? I don’t see it here.
Nothing posted
Craig, coulda sworn I posted the answer earlier. Anyway here it’s again, New & Improved etc: The fats I mainly eat are: coconuts, avos, fruit oils (c’nut, olive, red palm, avo). Some nuts/seeds, too, esp low-omega-6 pufa stuff like macadamia nuts, sprouted almonds, and sprouted sunnies. Finally, high omega-3 fish mostly cans of red/pink salmon (w skin and bones) and sardines, less often herring and smelt (whole). For protein (besides the fish), mainly eggs (usu 2x/day), and non-cow cheese. Occas fermented soy, almost always natto.
About dietary fats and CVD, I don’t worry about it in the least. Excess carbs are a MUCH greater risk. Dietary fats are large nearly non-polar molecules–very low-soluble in blood–which our neuron-rich GIs can vet very well in the duodenum. There, our bods bring the needed trigs systemic via chylomicrons and let the excess fats wend down that long and winding intestinal road to the exit. We have less choice with carbs. Carbs quickly break down into the simple sugars (glucose, fructose, galactose), very small highly-polar molecules that easily diffuse across membranes and into our bloodstreams, even in our mouths. To see what I mean, chew on bread for 3–5 min and note the emerging sweetness. Sugars are VERY soluble in blood. Thus they force us to deal with them systemically, and we do so by turning these excess sugars into long chain saturated fat (specifically 16C palmitic acid) which we store in our adipose tissue–and in those intramyocellular layers you discussed earlier. For the past nine years my blood panels have borne out this biochem. My trigs are 45–65 mg/dL and my total c’stol is 200 mg/dL–the low point for all-cause mortality per the NHANES studies.
I’ve got a new doctor who doesn’t believe in blood panels wbryanh….augh….the hypochondriac and former T2 diabetic in me wants those tests for historical record anyway…
My last panel in 2014 was 90 blood glucose, 38 tg, total cholesterol under 200 and HDL of 67. I achieve this with exercise and maintaining my weight slightly over. As far as diet goes, I lean towards Paleo in emphasizing meats and not excluding saturated fats, but I also eat any kind of carbs and end up somewhere around 50-60% carbs, 25-30% fats and 10-20% protein. It’s not much of a shift from what I ate T2 diet-wise, and it’s considerably more calories. The difference is 2-3 hours a day of walking and biking, which appears to metabolize calories of any type (about 1000 calories per day – the typical ancestral Paleo activity level according to Cordain) not very long after they enter the blood stream. There are no bad calories if you’re turning them ALL into CO2. Doesn’t matter whether they come from duck, oysters or poppyseed cake, they all burn up and are gone by the next morning.
Because of the way I do this, I’m probably carrying full glycogen stores all the time. If I were to go low carb for a few days I could probably drop those 5 pounds. But there’s no point, since I am constantly depleting and replenishing those stores by exercising. For the low intensity exercise I do, sugars and starches are the advantaged foods. If I was exercising at higher intensity, fat would have the advantage, but the sugars and starches would still get metabolized.
thhq, no question, we have many problems with the current state of blood panels. First, how relevant are the tests? E.g. measuring lipids measures only the levels of lipids, free, in LDL, in HDL, etc. they don’t measure the actual # of lipoproteins the lipids are carried in. E.g. do you have many smaller more oxidized lipos which are thought to be atherogenic? Or fewer larger “fluffy” newer, less oxidized lipos, considered to be relatively non-atherogenic? No way to tell based on the current default measures. Second, docs and hospitals say or imply that for total c’stol, “lower is better” though if you went to zero you’d be very dead. NHANES suggests that c’stol levels much below 150 mg/dL starts to greatly increase mortality, though from causes other than CVD, eg hemorrhagic stroke and cancer. Various biomarkers coming and going a lot these days, e.g. in the aughts Apolipoprotein (a) was a “for sure” marker of CVD, now dropped at least at my HMO (Kaiser)
All that said thhq, blood panels are better than nearly all the research papers out there, with poor methodologies and highly questionable stats massaging e.g. “p-hacking.” See here:
http://io9.com/i-fooled-millions-into-thinking-chocolate-helps-weight-1707251800
That plus the many agendas of the big money interests that back so much of today’s research, I put almost zero stock in them. One of, if not still THE most downloaded research paper from PLOS of all time is ironically titled: “Why Most Published Research Findings Are False.” You can read it here:
http://journals.plos.org/plosmedicine/article?id=10.1371/journal.pmed.0020124
When it comes down to it thhq, it’s nearly impossible to do a study that meaningfully relates chronic health and nutrition. The lag between introduction of causitive factor–nowadays while we’re still in the womb, and onset of symptoms, often decades later, plus that we live in a vastly complex world with hundreds of thousands of novel factors, together makes it impossible to meaningfully associate causes and effects.
About macronutrient balance, thhq, I agree it shouldn’t matter. Kitavans on HCLF, Inuit on near zero carb, etc. After all glucose is essential for a handful of cells, e.g. some brain and adrenal cells are obligate glucovores. We should have at least 40–45mg/dL BG to function properly. Thus we need insulin and insulin sensitivity to dispose of BGs into cells/mitochondria. Carbs were a relative rarity in pre-ag days, so our bods evolved five ways to increase BGs–including our livers make glucose as (perceived) needed–but only one way (insulin) to lower them. We crave carbs because it’s the fastest way to lay in fat–super important back in the bad old days when we routinely went days between meals. More body fat meant more days we could survive without eating.
Thus we need to look beyond the endless HCLF vs LCHC debates and try to learn what’s making so much of our planet carb intolerant? It goes beyond the old “eat less/exercise more” trope. I suspect the huge raft of novel organic compounds–over 100k now–that Big Chem’s been churning out since 1945 and are which on so many of the product we eat and use. Many of these, e.g. BPA and phthalates, are estrogenic, leading to IR –> metab symdrome–> diabetes and other chronic diseases. Also since WWII: routine use of antibiotics that wipe out our gut microbiomes, perhaps permanently disrupting our delicate sugar metabolic dance.
No question exercise a big factor for you thhq. Per what you say, exercise normalized your BGs FOR NOW even though you are back to being basically HC. But do you still suffer high serum insulin levels? If so, your BGs may once again creep back up regardless of your workouts. Get the euglycemic clamp if you can aford it, get the C Peptide test in any event. Basal serum insulin should be low, poss below 1 ng/dL. H-Gs measure out as low as 0.2 ng/dL.
I’ve never had serum insulin tests. My T2 was diagnosed from fasting blood glucose repeats of 190-200, and A1C of 8.2 eight years ago. I just had my annual checkup. My doctor refused doing even routine lipids. He claimed there is too much testing these days, and had the attitude that the tests were only interesting to him and not to me. Fat chance he’d have scheduled insulin. I was ticked because I was fasted and ready for sampling. I might change doc’s next year, but I’ve used up my covered checkup for the year.
I’ve often thought an index of ancestral compliance. Because of my personal experience with exercise, I give active vs sedentary living more weight than diet. Motorized transportation and electronic entertainment carry far greater weight than eating a diet of grass-fed liver, bone marrow and beets IMO. I know that modern factors such as BPA’s etc are important, but secondary to the dietary shift to eating vegetable oils, sugars, and starches far in excess of a person’s metabolic needs. Eating the bag of Cheetos does more damage than the BPA’s in them. They’re the chemical gravy on top of all the fat, salt, cornstarch and fake cheese.
Docs typically don’t do C Peptide unless asked. Took me ~ 3 years to get my doc to sign off on the blood panels I want. It’s a cost vs patient insistence issue, and my pestering started to prevail finally. Now he praises my “awesome BG control–best of all his patients.” Plenty of ppl should be getting A1c along with FBG , but don’t. HMOs etc always trying the rein in costs. For me, exercise is ~ 15% of the matter, diet/non-diet exposures the rest. Heartily disagree that undeclared toxins like BPA and phthalates are necessarily secondary. For some perhaps many, these ubiquitous estrogenics are HUGE. When I first diagnosed I was walking up to and resistance training and BGs still started spiraling out of control. The final day, 29 July 2007, I walked 30 miles eating Clif Bars along the way, 300 cals each one every 2 hours. BGs went from 80 to 245. That day, went LC and gradually started replacing engineered food with whole food. Even now, when I eat foods with BPA–the latest was Thai Kitchen coconut cream in BPA-lined cans–BGs popped from 90 to 130 and stayed elevated for 3 weeks. (BPA is fat-soluble). So back to more expensive but BPA-free Native Forest c’nut cream.
Another example: oxybenzone in Banana Boat sunscreen. One day in 2010, I did a 34-mile hike. Ate only 900 cals that day, mainly avocados. No problem, was fully keto-adapted, felt fine. But BGs rode in the high 90s that day, instead of high 70s/low 80s as had become normal even without the long hike. Next day, eating normal cal load, postprand BGs popped to 120s–130s and pretty much stayed 100+. Like with the BPA in the Thai Kitchen can, took 3 weeks for my BGs to correct. Went to EWG and look up all the ingreds in that sunscreen and oxybenzone sent up big red flags as a big-time endocrine disruptor. That was the first and last time since I started this journey in 2007 that I used sunscreen.
Regarding the craving for foods. I ‘ve always liked Guyenet’s reward explanation better than Taubes’ carb insulin opinions. We crave foods that gratify our taste. I crave a mixture of carbs AND fats. The highly craved chocolate chip cookie gets over half its calories in fat. The same is true of salty snacks like chips. There’s no satiation point eating foods like this because they taste so darn good. Fat and sugar are equal co-factors. Just eating a pure sugar lemon drop, or a pure fat butter stick doesn’t create the same effect.
If you haven’t read Hall’s recent study on the carb insulin theory, here it is. It takes expensive ward studies to test unsubstantiated journalistic theories.
http://wholehealthsource.blogspot.com/2015/08/a-new-human-trial-seriously-undermines.html
I’ve read this post, and take many issues with that study, as I do with virtually ALL of these studies. In this case, small sample rate, 6 days not long enough to get keto-adapted, looks only at normoglycemics not T2Ds, pre-T2Ds, it’s in a metabolic ward cutting out many exposure we get in daily life, etc. In general I find Guyenet has an axe to grind. He’s changed greatly since his Taubes contretemps and that makes me sad. Read his stuff before that Taubes event and Guyenet was refreshingly free of agenda. Now for him it’s all about agenda. All that said, it’s clear carb-only or fat-only brings on less craving than the combo, esp so if they are whole foods.
Guyenet compares the Hall study fat loss rates here:
“Metabolic measures indicated that the low-carbohydrate diet caused a 245 gram (0.5 lbs) loss of body fat over the 6-day diet period, while the low-fat diet led to a 463 gram (1 lb) loss of body fat over the same period.”
Other than reducing insulin secretion, where’s the advantage for rebalancing macronutrients to high fat? That’s about the amount of fat loss I would expect for typical 6 day weight loss dieting using calorie deficits on ANY macronutrient mix. I did that for six months and lost 50 pounds, without being at either low fat or low carb.
Hall goes farther and claims that carbs have a long term metabolic advantage over fats for weight loss, which obviously needs a much longer study.
thhq, again, big emphasis on “needs a much longer study.” And more. The Hall is so rife with issues and possible confounders that it demonstrates not much at all.
thhq- I “hear” what you’re saying about food reward with carbs and fat (my downfall is cashews roasted in coconut oil and salt). However, there are also times when, for “dessert”, I enjoy a nice soft goat cheese drenched in high quality olive oil: fat + fat! In any case, although I do believe we *experience* food reward- otherwise we might not be motivated to get the nutrients we need- I never really thought it was a very good explanation for the obesity epidemic. For one thing, I notice that since I’ve gone low carb, my desire for sugar has dropped way down, so I’m not convinced that our “desire for sugar” is as innate as some people claim. (I still crave moderately sweet foods, like coconut or pumpkin or some fruits; this makes sense, because of the nutrients involved; table sugar is just too cloying for me now). I think that our society’s sugar addiction is probably cultivated. When you think about it, we are weaned onto sugary foods from the time we were babies.
As for the study you posted: I’m not really sure it proved anything. For one thing, both Stephen Guyenet and the study authors mentioned that they reduced the fat in the low fat group more than they reduced the carbs in the low carb group. Also, such a short study doesn’t really prove much. If people have been “sugar burners” all their lives, it takes time- (more time than the study lasted)- to make the metabolic shift for the body to start burning fat efficiently, rather than sugar.
Lastly, I’m not sure the carbohydrate-insulin hypothesis states, specifically, that “all people who eat high carbohydrate diets” will get fat. The implication is that some kind of metabolic damage happens in the body- due possibly to excessive sucrose (or some implicate mainly the fructose part), or maybe something else in our environment, as wbryanh has suggested- which causes insulin resistance. Excess insulin is well documented to put on weight in most of us- (for instance, diabetics who need to take lots of insulin often put on weight). In any case, the people in the study you linked to were all overweight, BUT they were all metabolically healthy. Which could have made another difference in the outcome.
Guyenet SUPPORTS low carb, but he doesn’t like disingenuous techniques. Taubes is sold by the word, and he knows that hubris gets him linage in NYT. Health and scientific accuracy are secondary concerns to selling his books and getting support from the Atkins Foundation.
Carb insulin is very simple: follow the money. Atkins sold millions in books and products, and that’s Taubes is after. As fellow New Yorker Boss Tweed said “I seen my opportunities and I took ’em.”
thhq, you say “Guyenet SUPPORTS low carb.” Just curious, since the Taubes-Guyenet contretemps at the AHS symposium in August 2011, when has Guyenet ever come out “in support of low-carb?” I’d love to see that, as I’m sure others here also would. Thanks in advance for sending us that/those link(s).
I don’t think Taubes’ “Good Calories, Bad Calories” is exactly a book that’s been written for the masses. Usually if your purpose is to make lots of money, you write books in a short amount of time, with simplistic language to appeal to a wide audience. And maybe Atkins made lots of money because there were many people who were desperate for help, as the conventional advice was not working for them?
As I read him, Guyenet supports low carb, but not necessarily high fat. Here’s a passage from 2014:
“I view the low-carbohydrate diet as a tool in the fat loss toolbox, but one that’s most effective as part of a broader overall fat loss strategy. In the Ideal Weight Program, both of our fat loss diets are lower in carbohydrate and high in protein. Our approach is to incorporate multiple diet and lifestyle factors that have been shown to impact food intake and body weight, rather than limiting ourselves to a single-factor intervention.”
http://wholehealthsource.blogspot.com/2014/09/low-carbohydrate-vs-low-fat-diets-for.html
This study he’s reviewing showed an advantage for low carb over low fat for both weight loss and maintenance over a year.
thhq, please think about what you just said. Bear in mind we have only three caloric nutrients: fats, proteins, carbs. Are you seriously suggesting Guyenet is supporting “low carb but not necessarily high fat?” If so, that means you have to go way up on the protein. And you can’t go much more than 30–35% protein due to the risk of nitrogen overload. That’s borne out in anthropological studies. No diet goes above that protein level, including that for the northern Greenland Inuit. They preferred the fat, giving the excess protein to their sled dogs.
Augh. Guyenet is involved in selling a diet plan…so he’s coy with details unless you buy in…
Here’s what I could get for free from Kresser’s 2013 interview:
Stephan Guyenet:
“Sure. Essentially we brought together several researchers including Dan, myself, and a behavioral scientist named Larry Carter, and we put together a program that brought together all of our various expertise to bear on this issue of weight loss. What we designed is an Internet-based, multimedia diet and lifestyle program for natural fat loss and maintenance. It’s a diet and lifestyle modification program that we have based on what we see as the most cutting-edge research to date, and it consists of two basic tracks. Based on a person’s individual goals, they get to select which track they want to go down. There’s track one, which is our most intensive weight loss program, most intensive, most rapid, most effective. This is based around a diet that we designed. It’s called the FLASH Diet. FLASH stands for Fat Loss and Sustainable Health, and this is essentially a high-protein, low-carbohydrate, low-fat diet that’s relatively low in energy density, and this type of diet has been studied extensively in the biomedical literature. It is hands-down the most effective rapid fat-loss procedure that is known, and so that’s what we based track one on. That’s the diet. There’s also a physical activity and a sleep component.”
http://chriskresser.com/what-research-says-about-losing-weight-and-keeping-it-off/
Like the man says, high protein, low carb, low fat – now pay me. The FLASH diet book has a picture of what looks like beef stew and veggies that look like celery on the cover. I can get a recipe for that anywhere. Why does everyone try to resell this as some special plan? I’ll admit that Atkins and Taubes are better at this sort of thing. Or South Park, with their manbearpig. Or Calorie Count, where you can get this all for free.
thhq, when you say “Guyenet supports low carb, but not necessarily high fat,” if it is indeed “low fat” then it can only refer to a temporary diet. This is NOT a foodway someone will follow for the rest of their days.You simply can’t maintain a low-carb high-protein low-fat isocaloric (typ 2000-2500cal/day) diet. That’s too much protein, period.
Guyenet’s diet plan in its broad macronutrient conception is like the Ideal Protein Diet, another popular low-carb-high-protein low-fat diet that’s been making the rounds recently: http://www.idealprotein.com/. Again, their promoters do not intend for you to make this a permanent foodway that you will eat for the rest of your days. Rather they mean you to follow this only as long as it takes to shed the pounds till you arrive at your target weight. My Dad followed the Ideal Protein diet and found it the least onerous of the many weight-loss diet programs he’s tried. Even though it’s near 60% protein, the actual amount of protein is reasonable because total calories is so low, 700-800/day. Go to this Ideal Protein FAQ and scroll down to #22 for the details:
Click to access IP%20Frequently_Asked_Questions.pdf
Of course I didn’t read Good Calories Bad Calories!
I lost 50 pounds counting calories before I had ever heard of it.
Taubes says that what I do doesn’t work, from eating 50% dietary carbs to exercising.
But counting calories did work and continues to work. What would I gain by giving my money to someone who calls me out as a moron?
Have you read Eat Well and Stay Well by Ancel Keys? Or Nutrition for Life by Thompson and Manore?
Thanks morgana. I recently found this interesting piece on the body’s mechanisms to protect its weight.
It wants its fat back and will resort to dirty tricks to get it….
Another peeve here is that PUBLIC money has been spent to address the carb insulin assertion. The author of the unproven idea calls for those who question the idea to prove it wrong on their dime. So eventually they do. The rebuttal is that they are wrong, their methodology was wrong, ketosis did not take place, etc etc etc.
And who’s going to pay for the next million dollar ward study? How many times do they have to rebut it?
It’s starting to look like professional wrestling matches. Best two out of three falls wins.
What’s been done so far convinces me. High fat diet lowered insulin secretion 22% vs low fat diet. This should have promoted rapid fat loss, and a big immediate advantage over high carb, if the challenged assertion was correct. It didn’t. In fact, it was worse than that, because the fat loss was higher with the high carbs. This is enough to reject the carb insulin assertion IMO. And at the very least, the journalist’s follow-on assertion that high carb diets are ineffective for weight loss should be discarded by EVERYONE.
thhq, your passage: “High fat diet lowered insulin secretion 22% vs low fat diet. This should have promoted rapid fat loss, and a big immediate advantage over high carb, if the challenged assertion was correct. It didn’t. **In fact, it was worse than that, because the fat loss was higher with the high carbs**.”
thhq, my question to you: Where is your evidence to show that “fat loss was higher with the high carbs?” Where’s the study that compares HFLC and HCLF diets and determines the comparative fat loss on both diets?
thhq, your comment: ” [Taubes’] unsubstantiated journalistic theories.” What unsubstantiated theories?!” Do you refer to the GCBC chapter “The Carbohydrate Hypothesis, II: Insulin” starting on page 376? If so, Taubes he makes numerous references to researchers’ comments, e.g Haist and Best in 1966, Wilhelm Falta in 1925, Rosenzweig in 1994, Dole and Gordon in 1956, Yalow and Berson in 1965… Do you need any more?!
I don’t call it a theory. I call it an assertion. The problem with it is not GT’s lack of references. It needs verification, not researcher’s comments. Maybe the GT/Attia $40MM study group will provide the funding to Hall to complete his study. But I’m not holding my breath.
I actually did read the text of GCBC regarding exercise. GT has carefully crafted a series of N=1’s describing people who gained weight exercising. I’m in the process of doing that now, and it’s a good thing. When you’re 62, rebuilding lost muscle mass is key to body integrity (I have broken shoulder tendons to show for loss of musculature in that area). But to hear GT’s assertions, it was as if exercise was the devil and should be avoided, especially by anyone trying to lose weight.
After reading the restrictive high protein diet your father used I remembered Dukan. High protein diets work by starvation, forcing the body to consume its fat reserves rapidly while (hopefully) sparing muscles using the ingested protein. If you keep your total calories down to 500, the total protein calories are not excessive for the body to process. Very likely you will get into ketosis just from the extremely low calories. You will also preferentially metabolize fat (Thompson and Manore’s text is useful to understand why). High protein diets come with strong warnings on reducing exercise.
When GT talks about exercise being useless it makes sense in the context of the restricted calorie ketosis dieters who need to avoid it. GT doesn’t mention this context, and inflates his assertion to include everyone. Since GT’s carb insulin dogma rejects any form of dieting other than ketosis as ineffective it makes sense to avoid exercise. But only for him and his devoted LCHF acolytes. It makes no sense for me, or for HCLF dieters, or for non-obese cultures like Kitavan/Okinawan/French/Japanese, or for almost every pre-1900 culture, or for calorie counters, or for Weight Watchers, or for Cordain-style Paleos.
I’ve read enough of GT’s NYT assertions to get his Atkins-like drift on exercise, salt eating and carb insulin. That’s why I recommend that you read at least one standard nutrition text, if for not other reason than to understand that GCBC dogma is a very narrow view of the world. I don’t like having the pyramid or vegetarianism rammed down my throat, but I now know that a lipid is distinctly different from cholesterol, as well as the functional differences between VLDL, LDL and HDL. I didn’t know that before.
thhq, when you said “Of course I didn’t read Good Calories Bad Calories!” can you see how I somehow got the idea you didn’t read Good Calories Bad Calories? 😉
About Taubes and exercise, I certainly didn’t get your idea that he sees exercise as “the devil and should be avoided, especially by anyone trying to lose weight.” What particular passage(s) of his support your conception of this? Where does GT actually say “Exercise is useless?!” I took him to mean only that you can’t exercise your way out of the wrong diet. That was indeed my case. I was running half-marathons and doing 150-mile/day cycling climbing up to 15,000 feet of mountain passes in a day. Of course I was “carb-loading” according to the conventional wisdom of the day. Despite all this exercise I was still growing love handles and my A1c was creeping up, at 6.2% at the end of this heavy-duty sports stage of my life. Of course I wrote all this off as “bad genes” because after all I was eating “the right diet.” Certainly I feel exercise is important. For me, BG-wise, like I said earlier, it’s 15% of the picture. I do 8–10 minutes of resistance exercises each day and walk 5–10 miles every other day, sometimes run HIIT with 15- to 30-sec sprints. For me this exercise makes the diff between 70s and 110s BGs, but mainly it makes me feel GREAT. About what you say on Dukan, Thompson, Manore, yes, yes, understood all that ages ago. Where you say High protein diets come with strong warnings on reducing exercise.” again thhq please let me remind you NO high-protein super-hypocaloric diet is more than a **temporary fix** lasting only weeks. Please refresh your memory with my previous post on that.
thhq, in general, it strikes me you harbor some sort of animus against Taubes I can’t quite fathom. I honestly don’t recall most or even any of the things you say he said. If you can post actual direct quotes from him, I’ll stand corrected–I’m perfectly fine with that! But really what can I say? His LCHF proposal worked and keeps working splendidly for me. Good Calories Bad Calories literally saved my life or at least, all else being equal, greatly extended it. When you “recommend that I read at least one standard nutrition text,” thhq, I DID read plenty of similar of government-industry dogma and that’s what got me in trouble in the first place! Oh, as far what you say “I now know that a lipid is distinctly different from cholesterol,” thhq where did THAT come from? Cholesterol IS a lipid!
In general blood sugar will go down with exercise, but the opposite does happen with some people. My blood sugar used to go up too much every time I went to the gym, there was even a time I had to take a pill to control my sugar when I exercised. As I have made some improvements in my diabetes this no longer happens. This is one reason yours could have gone up.
Rebecca, you’re right, that was very true for me. And like it did for you, my BGs have gotten a lot better with my recovery through the years. BG spikes had to do with how long I strenuously exercise beyond the aerobic zone which causes us to kick into glycolysis, with our livers kick out glucose to quickly repair rent muscle tissue and otherwise try to make up for anaerobia. My answer it to make only brief forays into the anaerobic zone, leaving it again before my bod decides to go glycolytic. E.g. I do 2–3 minutes of crunches/supermans/pushups 3–4 times/day. And when running, I do full-bore sprints for only 15–30 seconds then spend ample time to recover back into the aerobic zone. Which pretty much describes mild HIIT – High-intensity Interval Training 🙂
If GT hadn’t bashed calorie counting and exercise I wouldn’t have so much fun picking at him. Eades is much worse, and it was one of his vicious ad hominems on Keys that piqued my interest in reading the works of the most important nutritionist rather than spending more time reading blogs of guys selling books and supplements. I worked as a research scientist (pulp & paper) for over 30 years and that affects my attitude too. I’m used to testing assertions fairly and accurately, both by people peddling chemicals and my own strange notions, and usually rejecting them unless they answered real needs (new products, improved performance, higher production, or lower cost). On rare occasions an assertion made it to the level of testing, and on extremely rare occasions one of those tests resulted in a permanent change.
The behavior I saw in the peddlers who failed a test duplicates the HFLC criticisms of Hall’s ward study. There were always immediate claims of unfairness in our testing, and a proliferation of new samples usually appeared to waste more of our time and money. These guys never walked away admitting that their products were dismal failures. Their lives were vested in their assertions, and we were the morons, not them.
Regarding GT and exercise, this passage parallels what I read in GCBC, though it was written earlier and apparently recycled into the book. This is the story of a man who got fatter by exercising:
“It’s difficult to get health authorities to talk about the disconnect between their official recommendations and the scientific evidence that underlies it because they want to encourage us to exercise, even if their primary reason for doing so is highly debatable. Steve Blair, for instance, a University of South Carolina exercise scientist and a co-author of the AHA-ACSM guidelines, says he was “short, fat, and bald” when he started running in his thirties and he is short, fatter, and balder now, at age 68. In the intervening years, he estimates, he has run close to 80,000 miles and gained about 30 pounds.
When I asked Blair whether he thought he might be leaner had he run even more, he had to think about it. “I don’t see how I could have been more active,” he said. “Thirty years ago, I was running 50 miles a week. I had no time to do more. But if I could have gone out over the last couple of decades for two to three hours a day, maybe I would not have gained this weight.” And maybe he would have anyway. If we trust the AHA-ACSM report he co-authored, there is little reason to believe that the amount he runs makes any difference. Nonetheless, Blair personally believes he would be fatter still if he hadn’t been running. Why?”
Read the rest to get the full context.
http://nymag.com/news/sports/38001/index1.html
This was not my experience, nor is the experience of others who have lost weight by exercising. [IMO this man was not counting calories and ate more than he exercised over 30 years. He didn’t take into account the slow loss in metabolic rate with age and kept eating like he was in his 30’s.] You can construct any defense you like for GT, but when I read something that directly contradicts my own experience I’m not inclined to buy that man’s books. I’ve got better things to do with my time and money. But like I said, I’ve got lots of time to quibble about GT. It’s a favorite pastime.
Here’s my short version summary on lipids. A lipid is a blood-soluble structure made of phospholipid, triglyceride and cholesterol, with a protein outer coating. The structure varies according to the function, and density varies with protein content. VLDL’s transfer triglygerides and contain the least protein, LDL’s transfer cholesterol out to the cells and contain the most cholesterol and intermediate protein, HDL’s recycle cholesterol back to the liver from dying cells and contain the most protein. The presence of a lot of HDL means the bloodstream is carrying low overall cholesterol concentration.
thhq, witnessing your growing anti-Taubes rant, forgive me for “fun” not jumping to mind. About GT’s view exercise, again, just can’t see how you feel he’s against it. About calorie-counting, if You have the time and the inclination to do it, then why not? You have time on your hands, as you say. I counted them for a while–even wrote a spreadsheet and plugged meals into it using USDA Nutrient Database data–and learned a lot from it. And it did help confirm I was on the right track. But as a life-long exercise, nope just can’t see doing it! Somehow homo-kind soldiered on for millions of years without counting calories, and my non-cal-counting grandparents and many of their peers lived to ripe old ages, late 80s and early 90s and older. In fact, in America, life expectancies have stalled and even reversed in some cohorts (e.g. middle-aged white men) and health expectancies have been going down for a long time even though we more of us than ever are diligently counting calories. There’s clearly other factors at play here besides failure to add up the grams of fats, carbs and protein we tuck into our maws.
About each camp trotting out the “scientific” research and reams of anecdotal data, yes, agree. I trust just about none of it, including Hall’s recent strange abortive effort and whatever few reports out there that find in favor of LCHF. Please revisit my post for you yesterday on “Why Most Published Research Findings Are False” or go straight here.
http://journals.plos.org/plosmedicine/article?id=10.1371/journal.pmed.0020124
The best we can do is sift through the different approaches and try them for ourselves and see which works best and get regularly tests. It’s not easy. It takes time and stick-to-itiveness. It takes careful recording and plenty of reflecting on the data you collect on yourself. The current state of blood biomarker tests is far from perfect. But it offers us the best hope to learn what food- and lifeway truly works for us.
About Taubes’ purportedly dim views of exercise, I read his piece in the New York Mag link you posted. He does abundantly caution the reader to not overestimate its role in weight control. But he also writes: “… [There are] excellent reasons to be physically active…We might just enjoy exercise. We may increase our overall fitness; we may live longer, perhaps by reducing our risk of heart disease or diabetes; we’ll probably feel better about ourselves.” Thhq, reading this, how could you ever construe what GT says to mean “…exercise is the devil and should be avoided”?
Thhq, finally, your statement “A lipid is a blood-soluble structure…” is wrong. You confuse “lipoproteins” with “lipids.” Lipids are *not* blood-soluble. That’s why our bods need to tuck them into lipoproteins which *are* blood-soluble. These large sphere-headed “ferries” then deliver lipids (e.g. fats, sterols) to cells all around our bods via lymph and blood. What you list–VLDL, LDL, HDL–these are all lipoproteins, NOT lipids. Which leads to one of the big failings in the standard lipid blood panel. To repeat from a yesterday post to you: These panels tell us only the levels of lipids, free, in LDL, HDL, etc. They don’t measure the actual number of lipoproteins that carry these lipids. E.g. do you have many smaller more oxidized lipos which are thought to be atherogenic? Or fewer larger “fluffy” newer, less oxidized lipos, considered to be relatively non-atherogenic? No way to tell based on the current default measures.
wbryanh you’ve really skipped over the observation that GT bears a grudge against exercise because it intereferes with Atkins weight loss ketosis. You’re not supposed to do exercise. The preferred metabolism route for fats is staying completely sedentary. This is key to understanding why GT piles up his typical mound of ancient research reports and anecdotes attacking exercise as a valid weight loss technique. My personal experience pretty much matches Ancel Keys 1959 predicted metabolic effect of 70 calories per mile walked at my weight and walking speed. I was sustaining 2 lbs of weight loss per week (on the scale) by walking 10 miles a day and restricting food. You need to track calories daily/weekly/monthly to lose weight this way. Keys called this method of weight loss Scientific Reducing in 1959, it’s called calorie counting now.
I find after 8 years of weight maintenance that I can carry calorie totals in my head (food and exercise), and I mark them down at the end of the day. I total counts using exchanges – units of 70 calories – a methodology I learned when carb counting to control diabetes and very similar to Weight Watchers points. A very simple methodology. When I walk into a Italian restaurant and have an order of pasta with a glass of wine and bread I know exactly what I’m doing to maintain my weight. I prefer this to the technique that you use. I like pasta and bread and I’ll eat your portion for you thankyouverymuch.
You are correct. I meant soluble lipoprotein and said lipid, which is insoluble. Doh. Your original assertion though was that VLDL, LDL and HDL are cholesterols and they are not. HDL for instance is 50% protein, 30% phospholipid, 17% cholesterol and 3% triglyceride according to my text, though other people publish somewhat different compositions. Now a question about what the lipid panels actually test. You say that the measurement is a test of ONLY the lipid associated with each lipoprotein? Not the protein and cholesterol?
Um, I don’t think so. I’ve read Good Calories, Bad Calories- (4 times, in fact!)- and I never remember Gary Taubes saying this about exercise. I think you’ve got that wrong. What he does say is that exercise usually raises appetite, so some people eat more, thereby making it difficult to maintain a reduced calorie, weight loss diet. (Of course, exercise can also make a person more insulin sensitive; which is why I think it works for you, thhq; but we are all metabolically different, and exercise alone doesn’t work for some people; especially possibly very obese people). Gary Taubes talks in his book a lot about how the body adjusts to calories and movement, as it tries to hang on to its fat stores. For instance, if you eat less, you tend to move less (the body is trying to conserve energy); or if you move more, the body feels the need to consume more calories. The book basically explains a lot about the mechanism of hunger, and how that applies to weight loss; which I think is phenomenal, as many books don’t touch on this issue. As far as I know, Gary Taubes doesn’t have anything “against” exercise. And it’s perfectly possible to exercise on a low carb diet. I exercise pretty much constantly- (my job requires it). I find it much easier on a low carb diet; partly because I digest my food better, so I have more energy to move. Also, I’m not distracted by that constant niggling hunger that I had when I ate high carb. I’m not saying everyone will feel the same as I do on this diet- there is no “1 size fits all”- but I just want to dispel the myth about low carb diets and exercise.
What you say Morgana, plus to put another way the insulin-sensitizing effects of exercise, exercise literally “feeds” you. The nutrients–e.g. BGs, lipo-ported fats, etc–are coursing around in your blood, and exercise “opens” the cell doors and lets them in. So often I’ve felt peckish when heading out for a walk or run and lose all appetite and feel great when I’m walking.
Um, NO, thhq, what you say here is dead wrong: “Your [wbryanh’s] original assertion was that VLDL, LDL and HDL are cholesterols…” I said that nowhere. Look again. You won’t find this. I do say “E.g. measuring lipids measures only the levels of lipids, free, *in* LDL, in HDL, etc…”
I am beginning to understand how you can misread and contort what others say.
You ask “You say that the measurement is a test of ONLY the lipid associated with each lipoprotein? The answer: Yes. Fats and sterols are lipids. The lipid panel measures only lipids in lipoproteins. The standard lipid panel looks just at total amounts of triglycerides and cholesterol spread out in some unknown number of lipoproteins. We should directly measure the # and size of lipoproteins themselves so we can better assess atherogenicity. Researchers are developing methods to do just that, including VAP and NMR tests. But last I heard these tests are not yet ready for prime-time.
About Taubes on exercise, you say “…GT bears a grudge against exercise because it interferes with Atkins weight loss ketosis. You’re not supposed to do exercise. The preferred metabolism route for fats is staying completely sedentary…” Thhq, Do you have GT quote(s) that say just those things? Would you mind posting them here? Going forward, it’d really help if you just post actual author quotes instead of giving us only your interpretation of what who-and-who said. And again, GT wrote: “… [There are] excellent reasons to be physically active…We might just enjoy exercise. We may increase our overall fitness; we may live longer, perhaps by reducing our risk of heart disease or diabetes; we’ll probably feel better about ourselves.” Thhq, reading this, I think most people would understand that GT is most definitely NOT anti-exercise. But if you’d rather, just keep ignoring direct quotes like this from Taubes and others and instead keep plopping here what you “think” Taubes and others said. Just don’t be surprised if I stop paying attention. I am glad though your weight-loss method worked for you. Anyone who loses 50 pounds and keeps it off deserves kudos. I know a few people who got fluent in a exchange point system and are very happy with it.
er… change to “not the protein?” The cholesterol goes with the other lipids, as you say. Wish this blog would allow editing.
And in attempting to answer my own question, I found a method used by Johns Hopkins
Click to access l13_c_met_lipids.pdf
I may screw this up, but here’s what it looks like to me:
Total cholesterol, triglycerides and HDL (with the non-HDL cholesterols rendered non-reactive) are measured separately using different series of reactions which release peroxide. The peroxide concentration is measured after treatment with peroxidase to get a color change, of which the intensity is detected by a spectrophotometer (UV?). VLDL is derived by dividing triglycerides by 5, and LDL is derived by subtracting HDL and VLDL from total cholesterol.
So the test is done on the cholesterol in the serum. It measures the cholesterol associated with each lipoprotein, but does not measure the lipoprotein concentration itself.
Thhq, cholesterol and triglycerides have little or no solubility in blood. Maybe testers need first to liberate the lipids from lipoproteins, have them enter serum in the lab before testing them? Anyway, the issue’s really about the atherogenecity of the lipoproteins themselves, not their lipid cargo. Esp as the lipos age, oxidize, get smaller.
http://www.sciencedirect.com/science/article/pii/0891584995021736
Once again wbryanh I stand corrected. I have put the words of my doctor “HDL is good cholesterol, LDL is bad cholesterol” in your mouth, and your version is much more correct than his. This doesn’t get us any further than your proving that I am a moron, but maybe I learned something….if I don’t forget it before my next blood panel…whenever that is…
As far as finding you some choice GT comments on exercise, here’s his summary of the New York magazine article earlier cited, in a chat with Jimmy Moore
“The only real way to test it would be to do a randomized controlled-trial and those are difficult to interpret because as soon as you instruct people to exercise or diet in these kinds of studies you get all kinds of unpredictable psychological and interventional effects. The trials that have been done suggest that exercise has no effect. And as I pointed out in my article in New York Magazine, the world is full of plenty of people who exercise diligently and continue to gain weight from year to year, including several of the world authorities on exercise and weight loss.
If you look at animal studies, it’s pretty clear that animals respond to exercise by eating more and the exercise has no effect on fat accumulation. And while it’s true that part of the job of fattening geese and cattle is immobilizing them, it’s not clear that those examples are relevant to real life. It’s not that I don’t think exercise is good for you because, Lord knows, I do enough of it — as my back and my arthritic knees will attest. I’m just not so sure that the causality goes in the direction that you think it does.”
http://livinlavidalowcarb.com/blog/taubes-is-weight-loss-from-exercising-or-are-you-exercising-because-you-lost-weight/2734
Compared to the straw-man failed weight loss exercisers GT pictures, my personal trial produced steady weight loss, and the causality went exactly where I expected it would at the rate of two pounds a week for six months. This is just the way Ancel Keys predicted that it would go if I used Scientific Reducing. Maybe I’m misreading something (and you’ve seen that I’m prone to that), but it also appears to me that GT does not even accept the idea that sedentary animals that get fat can be compared to humans…
I don’t see a lot of support for exercise in that quote, but I’m sure that you can find some sunshine. I’ll find more quotes if you like, but I might have to go to the library and dredge around in their cc of GCBC, if they still have one.
OK thhq, I reread the exercise sections in GCBG, and GT’s NYMag piece and transcript of Jimmy Moore interview you posted. I see the confusion now. You did not read all of GCBC, but just the sections on exercise. You lack the default context and conditions GT presented to properly understand what he wrote about exercise and weight gain.
To be clear, GT doesn’t deny exercise *per se* burns calories and fat. In GCBC (pg 260) he gives this quote from researcher Russell Wilder: “The patient reasons quite correctly that the more exercise he takes the more fat should be burned and the loss of weight should be in proportion…” Nowhere does GT assert that someone who 1) starts exercising AND 2) eats the same or less caloric load as during his/her pre-exercise days will still gain weight. That’d be silly.
GT most discusses exercise on pp 259-269. In the preceding copy, GT discusses the default conditions in which some people who exercise a lot still gain weight. He assumed we’d bear in mind the default context and conditions he previously and amply laid out. These include: 1) eating very high-carb SAD, 2) not counting calories thus eating *ad libitum*, and 3) doing sustained strenuous workouts. Under those conditions, of course many dedicated exercisers will struggle with weight. Those three conditions give an ideal prescription to keep us mired in full-blown glycolysis, keeping many of us, esp the insulin-resistant and in metab syndrome, in a cycle of madly chowing and madly exercising. Who among us here doesn’t know at least one person who went/is going through that discouraging process? Including me, thhq, as I posted to you about earlier. All my running and cycling, and I still got love handles and T2D.
Thhq, here we see the risk of picking snippets out of his treatise on this complex topic. In GCBC, GT lays out a long buildup, giving context and conditions, to finally present his carbohydrate hypotheses starting only on page 355. If you take time to read GCBC from the beginning, his exercise hypothesis will make sense to you. You’ll see it doesn’t at all refute your own experience. You stick mainly to aerobic–not anaerobic–exercise which preferentially burns fat, You do count your calories and so keep a lid on how much you eat. You do eat whole foods, not the SAD. Taubes default conditions with which he developed his exercise-weight gain hypothesis in no way applies to you.
wbyanh, I’ve given you TWO long passages where Taubes berates exercise as a tool for weight loss. The NY Mag piece predates GCBC, and is recycled into it, and the strategy is the same. The NY Mag piece is written in his awful, disingenuous, ingratiating prose (another reason I can’t read GCBC – I’m used to reading Proust, not hack biographers – 800 pages of this journalist-speak would drive me up the wall), and softens the blow for the general audience. The Jimmy Moore piece, before a friendly audience, cuts to the chase, and GT explains what he was up to when he wrote the NY Mag piece:
-He admits INTENTIONALLY picking N=1 examples of people who gained weight exercising. Where’s Jack LaLanne? Where’s Ancel Keys? Where’s durianrider? Where’s ME? It’s as if all of us who have lost weight exercising don’t exist. There is no counterpoint, just the examples that gained weight. I call this hard evidence that GT IS a cherry picker. [I expect you to ask me again to read all 800 pages of GCBC so I’ll get it. That’s not happening. I ‘ve got all I need right here.]
-He derides the use of controlled studies to test his assertion that exercise is useless for weight loss. Everyone already knows that, studies are expensive and hard to control, it’s like the sun in the sky, and if you don’t believe it…like I said earlier, but now it’s GT actually saying it.
-He talks about exercise as something that damaged his body. He’s cherry-picked himself on this one. I’m sorry it didn’t work out for him like it did for me. Exercise HEALED my body – not just the blood tests, but the weight loss, the higher HDL, the lower blood pressure, etc. GT is calling exercise destructive, not selling it as critical or even useful to lose weight. Right after that he talks about how animal sedentary obesity is not comparable to human sedentary obesity, implying that sedentary behavior is possibly OK (but not coming right out and saying that, just wheedling and insinuating it in his awful way – I’d like to hit him in the head with a copy of Dr. Atkins Diet Revolution at this point…at least Dr Atkins doesn’t beat around the bush about how to get the best results from ketosis dieting).
When I came into my doctor’s office after counting calories for a year, bringing my blood tests into line, and losing 50 pounds, my doctor shook my hand. When I read what GT wrote, and listen to his attitude about what he wrote via Jimmy Moore, I’m not seeing ANY support for what it took me a year to accomplish using exercise. I’m not getting a pat on the back or a handshake from GT for what I did. I’m just another cherry that GT intentionally overlooked when he was carefully picking his tree.
You found the book, used it, it helped you, and that’s great (though you could have saved a lot of painful reading by just using Diet Revolution). If you had lost weight the way I did, you might be more sympathetic with my objections to GT’s assertive “my way or the highway” mentality. As one very healthy vegetarian told me “If GT was right I’d be dead”.
thhq, you completely miss the point in my previous post. Please reread it and try again.
Or thhq maybe don’t bother to reread my post. At this point, you’ve made it so abundantly clear you harbor an animus to this man which goes way beyond “fun” as you earlier called it. You persist to think those few actual GT quotes you bothered to post has him actually say anything categorically bad about exercise regardless of context and conditions in which the exercise is done. You keep irrelevantly discussing things that refer to GT’s style that you find objectionable rather than sticking to facts. Here thhq you say “The NY Mag piece is written in his awful, disingenuous, ingratiating prose (another reason I can’t read GCBC – I’m used to reading Proust, not hack biographers – 800 pages of this journalist-speak would drive me up the wall)” Well thhq, that’s your *opinion.* Full stop. I think you can find many people who feel far differently from you about it. You say “He talks about exercise as something that damaged his body, the closest GT statement I could find that even comes close to what you are talking about is this from that 2008 Jimmy Moore interview: “It’s not that I don’t think exercise is good for you because, Lord knows, I do enough of it — as my back and my arthritic knees will attest..” First, GT actually SAYS he regularly exercises. If he truly felt exercising was useless and even damaging why then would do it? Second, he doesn’t blame exercise *per se* for the damage. He leaves the door open to the possibility that he could be doing them wrong.
Once again thhq you simply refuse to ackowledge the direct GT quotes I’ve posted for you because they don’t suit your pre-conceptions. You pride yourself on rigorous intellectual remove, yet it’s so clear you let your emotions influence and even pervert so much of your thinking. Well then fine. Please just go on irrationally hating on Taubes convincing yourself you’ve somehow supplied real evidence that justifies anything at all, meanwhile wrapping yourself in your intellectual science-y cloak. I won’t stop you! But I will no longer waste my time to continue to post solid information you persist to completely ignore.
I give up wbryanh. You have asked me to read GCBC and I will not do that. I don’t need to. I realize that this book is very special to you, and that GT is very special to you, but you treat this like GCBC is the Bible and GT is Jesus. It’s like you are personally affronted because I do not worship these holy things. Thanks for the discussion and the schooling on lipids anyway.
Sure thhq, you can assume those things or anything you want if it makes you feel better. Far be it from me to try to disabuse you of your high-flown notions. But, bottom line, you have found a system that works for you, at least according to the health measures you have chosen to get to date. You certainly have to work at it but, from all you’ve said, you are enjoy enduring success where many (most?) do not at this time. In all seriousness thhq you deserve all the pride and happiness you feel in that achievement! Please be happy. Take care. –Bryan
And you misunderstand…it was fun to jib-jab on this subject, but I’m tired and need a rest for a while. Back to Thompson and Manore for a reread, or a few more longevity studies.
I’ve read and reread your comments wbryanh. My chief objection is that the NY Mag article has to stand on its own. In rereading it I realized that GCBC predates it, and that it is the GCBC exercise chapter with some modification. It has to stand on its own nevertheless. For every million people that read it in the NY Mag, maybe 1000 bought GCBC, and maybe 100 of them read it from cover to cover. It is not reasonable to say that the people reading the article should be familiar with GCBC in context, and be able to quote chapter and verse to support GT’s assertions. GT has the bully pulpit in NY Mag before the mass audience, and what he says has to be taken at face value.
I don’t see this as an entirely negative approach. GT has challenged CW, and for some people this is the shock treatment they need to deal with their obesity. From what you’ve said it helped you in that way. And there’s no doubt in my mind that HFLC is an effective way to reduce weight.
There is a strong negative effect though. The average reader, who does not go on to buying and reading GCBC, is left with the impression that exercise will cause them to gain weight. They might as well have another stack of pancakes and watch TV for all the good going for a walk would do them.
Four years later there is no reduction in US obesity rates. This despite the best efforts of GT, Oprah, Dr. Oz, Pritikin, Atkins, calorie counters, Weight Watchers, Dukan, South Beach, etc etc etc. That’s the really SAD thing. Despite these wake-up calls from so many concerned people no one is paying attention to their very real health problems.
thhq- do you have a link to this NY Times article, so I can read it? (You may have posted it; if you did, I didn’t see it, and things can get lost so easily in this huge comment section). I seriously don’t remember Gary Taubes saying anything bad about exercise. What he does debunk is the “eat less, move more” mantra, explaining why that doesn’t work for the majority of people. It all fits together with that link that you posted recently (which was interesting, thanks)- about how the body tries to hold on to its fat stores. “Eat less, move more” can work temporarily, but the problem is, either it is too difficult to maintain indefinitely- (people either become hungry again and feel the need to eat a normal amount), or the body conserves energy on a low calorie diet, so people burn less, or even have a hard time exercising.
What might also confuse the issue is that- in terms of pure calories alone- it has been discovered that exercise burns off fewer calories than one might think. There is science to back this up- (if you want a link, I can try to find one). So, exercising alone will not enable the majority of people to lose weight, or at least not much weight. However, It DOES help one maintain weight, i.e., you’re less likely to put on more weight if you exercise. But it can also raise appetite, so that can be problematic for some people, as they would need to keep a calorie deficit if they have lots of weight to lose. (As we’ve already established, exercise *can* also help with insulin sensitivity so some people might actually lose weight through exercise).
Gary Taubes writes a lot about fat versus energy expenditure too. What happens is when people with metabolic syndrome become overweight or obese, they often become low in energy. The body is unable to feed its cells, and unable to mobilize it’s fat stores, so these people often have low energy. In many instances, when they lose the weight, their energy returns and they feel the desire to move around again. The fat, as well as the lack of energy, are not *causes*; rather, they are symptoms of the underlying metabolic problem.
It’s a rather complicated subject, so it’s hard to summarize in a short interview or magazine article (or even in a post in a comment section like I’m trying to do now!) How does one make a complicated subject simple, after all? This may partly explain the misunderstandings and misinterpretations of Taubes’ writings.
Morgana, here you go. Just to make clear, the link thhq gave is from NY Mag, not The NY Times. Here it is, titled “The Scientist and the Stairmaster:”
http://nymag.com/news/sports/38001/
Evidently thhq also confuses the New York Times, with an international circ in the millions, with the much more localized NY Mag. He said “…For every million people that read it in the NY Mag…” Yet per the Wiki, NY Mag has a circ under 409,000.
https://en.wikipedia.org/wiki/New_York_(magazine)
Morgana, this from you: “…’Eat less, move more’ can work temporarily, but the problem is, either it is too difficult to maintain indefinitely- (people either become hungry again and feel the need to eat a normal amount), or the body conserves energy on a low calorie diet, so people burn less, or even have a hard time exercising.”
I agree totally with it, at least when eating HCLF. During my measured cal-counted HCLF period (March–July 2007), I had to ride serious herd on myself to keep from overeating, likely because I was in glycolysis all the time except–as thhq recently discussed–during long sleep nights when we settle into ketosis. This frequent hunger was likely because our bods can store only ~ 2000 cals of carbs at a time (in glycogen aka “animal starch”) which is less than a day’s worth. Thus, when tuned for glycolysis, our bods send out the “fill’er up” signals after just a few hours. Hence “three squares a day.”
When I went full HFLC at the end of July 2007, I was able to circumvent what you describe above. I still cal-counted for a while, but in time I no longer needed to, I began to feel sated at the appropriate times. Once I was regularly in full deep ketosis (~2008-2009), I started doing intermittent fasts, lasting from 18 hours to 3 days. But that time, my bod was used to burning fat, and since we carry around many dozens of thousands of fat cals, the bod feels less urgency to quickly go into conservation mode. I know this for myself by repeatedly measuring my total weight/body fat % over the fast periods, and even for the 3 day fasts, I always steadily lost both total fat AND body fat %, showing that even during fasting, my bod was preferentially burning fat even after three days, NOT cannibalizing muscle for protein. I never fasted beyond 3 days. I’ve fasted many hundreds of times since then, and felt only twice that hunger led me to break the fast. To head off metabolic down-regulation during fasts, I continued to do lots of aerobic exercise and short bursty resistance exercises, making sure to keep them short enough in duration to not kick off glycolysis. Deep ketosis and steady aerobic and light HIIT together worked magic for me. During one 3 day fast, I walked *40 miles* (roughly a third of that each day) and felt an incredible combo of deep calm and great mental sharpness and making fantastic cognitive connections. During my long walks I kept stopping to scribble notes and filled over 20 pages in that time! In each fast, after the initial metab transition period (typ at 15–21h), I never felt hunger until fast-end.
wbryanh- yes, when I was high carb, I, too, felt something similar to what you describe. I got hungry more often and had to eat more often, but oddly enough, I felt both extremes more. Eating lots of carbohydrate would fill me up so much that I actually felt bloated and full, but then a few hours later I would be hungry again. When I first went low carb, I sometimes thought I hadn’t eaten enough, since I didn’t have that really full feeling I got from carbs. It turns out I had; I just had to re-learn what “hungry” and “sated” felt like. I also now do intermittent fasting every day- (between 14 and 16 hours usually), and eat 2 meals, 1 “brunch”, and a dinner. My digestion is much better this way. I am intrigued by your 3 day fasting; I’ve been reading about that, and am interested to try it. According to a Dr. Seyfried, it’s a good way to boost your immune system and “clean out rogue cells”, which can help prevent cancer. I’m a little bit afraid to do a 3 day fast though; partly because I’m already a bit underweight, and don’t want to lose more; mostly because I have naturally low blood pressure, and am a little worried it might get too low, which could be uncomfortable (or maybe even dangerous???) Since I’m pretty sure I already burn fat rather than sugar, I think I could manage it otherwise. If you have any tips or information about it, I’d be interested in hearing it!
Dr Jason Fung treats his patients with fasting. Here is a link to his website.
https://intensivedietarymanagement.com/ There is a lot of information about fasting.
Thank you Rebecca for reminding me to catch up on Jason Fung. I think his writing is very good and approachable, and love how how explains the manifestations and underlying mechanics of fasting and food desire. E.g.:
“…95% of us have never, truly been hungry in the sense of starvation…much of what we perceive as hunger is actually a learned behaviour…hunger starts in the mind…If sweeteners were the answer, we would not have this obesity epidemic, would we? It’s not like people aren’t eating sweeteners. How many people do you know that have tried sweeteners? 95% of everybody? How many people lost significant weight? 2%?…”
Right on!
Hi Morgana. Yes, if you’re underweight and have low BP, I’d certainly take it slow on fasting. When I started fasting, I was well in the BMI range, had just 10–12% body fat, and BP was 90/60. (You can buy scales that measure BF% – I have a Tanita.) Even without fasting, got the occas episode of lightheadedness when I rose quickly, maybe suffered a bit of orthostatic hypotension. Thus, I *eased* into fasting, starting by eating earlier and earlier at evening and breaking fast later and later the next day, that let me sleep for most or a lot of it. So it went, 14hr, 16, 18, 24, etc. till I got up to the three days. For maybe 1–2 years, I frequently felt a “want-to-eat” challenging in the 15–21h stage, but now no longer. Now it’s unchallenging throughout.
Diet-focused folks often abuse the word “cleansing,” but with fasting that may actually be the case! Fasting enhances autophagy, in which our bods, not getting calories from the outside, start to dismantle the molecular flotsam bobbling around in our cells’ cytoplasm (fluid). A less cluttered cytoplasm allows the zillions of metabolic processes that occur within to proceed more smoothly. It’s like cleaning your room–you can get to stuff faster. But even more important, since metabolic processes are often so tightly choreographed.
https://en.wikipedia.org/wiki/Autophagy
wbryanh- thanks for the info! Yes, I would be most interested in fasting for autophagy; I don’t want to lose weight. (I wish there was a way to fast without losing weight). Sometimes I’ve thought maybe I should start with just a 1 day fast first, and see how that goes; however, I’ve done a lot of reading on the subject, and apparently, the first two days are the hardest to get through; after that they say it gets easier, so it seems a shame to stop before the third day. Also, according to Seyfried, you have to fast at least three days to get any benefit. So, yeah….I’ll keep researching the subject, maybe someday I’ll try it. Until then, the daily 14-16 hour fasts seem to be working well too.
Morgana, you’re welcome! If it’s any comfort, even visibly thin people often have enough discretionary fat to last for quite a long time, well beyond three days. But again, bottom line, you need to feel comfortable with it. It took me two years to start to truly fast. What is your body fat %? For women, the healthy range is 15–25% I’d get a reputable scale that gives you your body fat % in addition to your total weight. I bought my Tanita scale at BB&B for $25 and it consistently measures 2% BF above that of the hydrostatic dunk tank. If the DEXA scan is the platinum standard for body fat percent measurement, the dunk tank is the gold standard.
As far as how long it takes to get through the tough part of the fast, it really varies with each person and how deep into ketosis that person is to begin with. For me, the tough stage was ALWAYS in the 15-21h range. After that I was nearly always home free. Now I don’t even suffer any tough stage any more. Btw, I’m not convinced all of us need to fast a minimum of three days. I let my glucometer and how I feel be my guides. If I’m getting readings consistently in the 70s and feel terrific to the point of sublime, I know I’ve fasted enough 🙂
thhq- silly me: in my rather long winded post, I realized I forgot to mention one of the most important bits! And that is, with overweight people who are lacking in energy- (this applies to that paragraph I wrote about energy)- sometimes it’s been advised that they lose the weight first (with a low carb diet), and then exercise later. This is because, as I explained above, once they start losing the weight, the energy often returns naturally. This might be part of the misunderstanding with Taubes’ views on exercising.
Sorry to get them mixed up wbryanh. We could spar over this one too, which was in the NYT.
GT gets a lot of high visibility press coverage. Agreed?
@morgana, getting some weight off certainly will give an obese person more ability to exercise. For most people reducing carbs helps, but reducing fats can work just as well. IMO it’s the calories (fat AND carb) that need to be reduced first and foremost to get weight loss started, followed by increasing exercise to keep it going.
I prefer to exercise at low intensity to preferentially metabolize fat over carbs, but it takes a lot of time to get much of an effect. What works even better is sleeping. When you’re as close to idle as you can get, Thompson and Manore state that 90% of metabolism is fat. Unfortunately the metabolic rate is low, approaching RMR, so you have to do a lot of sleeping with very minimal eating to lose weight steadily.
Here, Kevin Hall calls it a theory:
“Journalist Gary Taubes berated nutrition scientists for not understanding the seemingly simple concept of controlling diet variables. He chastised the field for altering multiple diet components at once and said that controlling variables is something that even
“school children are supposed to understand”
The failure of nutrition scientists to understand this basic concept
“has led to what may be another of the great misconceptions in modern nutrition research”
Mr. Taubes then exposes the horrendous misconception:
“carbohydrate-restricted diets are ‘valuable tools’ in the arsenal against overweight and obesity, but they’re just one of the dietary tools.”
Why was such a seemingly reasonable statement proclaimed to be a “great misconception”? Because, in Mr. Taubes’ view, the carbohydrate-insulin theory implies
“that the only meaningful way to lose fat … is by reducing the amount of carbohydrates consumed.” [bold mine KH.]
Doubling down on this claim in his most recent book Why We Get Fat, Mr. Taubes states that
“any diet that succeeds does so because the dieter restricts fattening carbohydrates…Those who lose fat on a diet do so because of what they are not eating – the fattening carbohydrates.”
At the time, I read these proclamations with great interest. I had just begun collecting data from a carefully controlled metabolic ward study which is the first to avoid the confounding nature of changing multiple macronutrients at once. Thankful to have an understanding of clinical trial design equal to an average school child, I also realized that our study would directly test Mr. Taubes’ version of the carbohydrate-insulin theory which has become greatly influential.”
http://www.weightymatters.ca/2015/08/guest-post-dr-kevin-hall-asks-is.html
And this is precisely what launched the Hall ward study we are discussing, which was meant to give the “theory” a fair test.
But you can see how Taubes berates his critics for questioning it. For that reason I call it an assertion. For Taubes, this thing he thought up is like the sun in the sky, gravity, a signed publishing contract, or Biff’s sports almanac. It’s not allowed for anyone to test it or question it. IT’S SIMPLY TRUE AND IF YOU DON’T BELIEVE IT YOU’RE A MORON.
Which is why everyone trained as a researcher instantly questions it.
thhq, did you read Good Calories Bad Calories?
Thhq, no I haven’t read the Keys or Thompson books you mention. But I’m not running on about them either. I don’t trash-talk books I haven’t actually read. That’s why I asked you if you had read it before you started unloading on it. Hall’s study was ambitious. But I repeat, it is RIFE with caveats. He used a small and unusual cohort: obese normoglycemic people. Not T2Ds or pre-T2Ds. The “low-carb” side was definitely not low-carb at 140g carbs/day. Perhaps most egregious, 6 days is almost certainly too short a time to allow for full keto-adaptation. About Taubes’ carbohydrate-insulin hypothesis, I remain quite unconvinced Hall’s study disproves it. Insulin levels dropped for both the low-carb and low-fat groups, more so for the low-carb group. The diff in the LC and LF drops wasn’t much, but then how can we expect there to be? All subjects were insulin-sensitive to begin with, and then they started eating hypocaloric diets with an 800cal/day shortfall, making them even more insulin-sensitive. In short, what does it all prove? Not much I’m afraid! Frankly the whole methodology’s a bit bizarre. If you don’t want to hear these caveats from me, go to Guyenet’s site and read the comments on the Hall study. So many readers took issue with Guyenet’s study he did a followup post five days later. There he tried to address the concerns of his readers and ends up fielding many more concerns. Even Guyenet admits a better study is needed.
So thhq, let’s leave Hall’s ward and re-enter the real world. If carbs are fattening, then why are there lots of people chowing high carb diets who stay thin? Why does that Chinese farmer eat mainly rice yet not get fat? The principal answer likely is that–provided you never entered metabolic syndrome to begin with–the less food you eat and/or the more exercise you do, the less the body cares the source of the calories be they from carbs, fats, or proteins. The closer to subsistence you eat, the hungrier your cells are for the nutrition thus the less insulin you need to dispose the energy, even carb energy, into the cells. Thus your serum insulin level stays low enough not trip the fat-storage switch.
So that’s fine thhq for people in developing countries who do hard physical labor and can afford only a subsistence diet. We live in developed countr(ies) where food and food-like products are cheap and all around us. In such a case I’m not surprised you need to count your calories to stick to your eating plan. Thanks to LCHF, I don’t have to bother with that headache. I enjoy natural satiety and I still lost 62 pounds (230 to 168) and body fat dropped from 26% to 10%, in addition to the other health improvements I list elsewhere in this forum. Most of all *normalized* BGs! I’m not saying LCHF is for everyone. Each of us really should experiment and see what works best. But this foodway lets me live my life AND enjoy great health! Really what more can I say?
I don’t know where this will land wbryanh, but thanks for the dialectic. We’ve achieved the same ends blood-wise by completely different methods.
So now that we’ve arrived at healthiness, what’s the best path to a healthy and long life? I didn’t come into this thread to bicker about GT, though that is one of my favorite pastimes. It was more an interest in the HCLF cultures and persona that attracted me. There’s a lot of modern information on longevity for those cultures (Japanese/Okinawan, eg) and persona (Keys and LaLanne, eg). But there’s very little on LCHF that is contemporary or relevant. Guyenet’s information on traditional Inuits comes from the early 19th century, and shows lifetime in the 30-40 range. What do you know on this subject?
Sure thhq, I’m always happy for constructive convo. It always leads me to think about what I’m doing and better sort it out, and often points to new things to consider. I know you feel you’ve arrived to a healthy place blood-wise, and maybe you’re right, but still I’m curious to learn your C-Peptide and your body-fat percent. I’ve long thought that ancestral cultures span the macronutrient gamut from extreme HCLF to extreme LCHF, so why then is diabetes and other chronic diseases soaring all round the globe? This conundrum led me to research other influences, esp. environmental toxins, esp those in our own homes and everyday products we consume. As far as Guyenet riffing on ancestral-living Inuit living short lives, I assume this is what you’re referring to:
http://wholehealthsource.blogspot.com/2008/07/mortality-and-lifespan-of-inuit.html
First note this is “the ages of death of a traditionally-living Inuit population during the years 1822 to 1836.” Guyenet also includes caveats: “It’s possible that life expectancy would have been higher before contact with the Russians, since they introduced a number of nasty diseases to which the Inuit were not resistant. Keep in mind that the Westerners who were developing cancer alongside them probably had a similar life expectancy at the time.” Thhq, I’m mainly impressed at the fact a few of these Inuit actually made it into their 90s, given their incredibly challenging environment!
Also since WW2, we started adding iron to most carb foods. The idea was to prevent anemia. But iron messes with the gut biome, and also directly causes diabetes. So if you want to make a person more insulin-sensitive, just have them donate blood.
http://diabetes.diabetesjournals.org/content/51/4/1000.full
“In summary, blood letting led simultaneously to decreased blood HbA1c levels and to changes in insulin secretion and insulin resistance ”
Carbs in the US affect iron levels mostly because they are “enriched”. Whole grain carbs are not enriched, plus the bran blocks iron absorption. Pre-WW2 some people used molasses or cast iron pans, or ate a lot of meat, but more people had lower ferritin levels than today, so there was likely less diabetes.
Which makes me wonder. The rice diet was started pre-WW2, so the rice used was probably not enriched. If the same diet was done after WW2, the rice likely would have been enriched, and would it have had the same results? The rice diet was a super-super-low iron diet.
Actually, it’s not just the iron (which is linked to metabolic issues, like diabetes). Rather, it’s the B Vitamins that are known have an affect on appetite.
Although McClain et al. 2015 recently showed that high iron intakes (simulating a high meat diet) are linked to increased appetite, enriched foods themselves have been linked to obesity and increased appetite (Zhou et al. 2014) because of the B vitamins. Thiamin was once known as the “appetite vitamin” (coined by Cowgill) and niacin has been linked to increased appetite, according to Zhou et al. If you do a Google Images search for “ironized yeast” you will find vintage advertisements for pills that were high in B vitamins and iron used to increase appetite and put on pounds. In fact, the discovery of B vitamins happened because it was shown to increase appetites in rats.
Bakers and millers were initially against enrichment before WWII, but right around the time the US Dietary Guidelines were written, grain lobbyists began to become the most vocal proponents of enrichment. The lobbyists pushed the FDA to approve significant enrichment increases during the 1970s, which were finally approved in 1983. It is interesting that Pritikin’s had health issues soon after 1983. To this day, grain lobbyists are the main supporters of food enrichment in the US.
Since 1983, a single slice of bread has as much appetite-stimulating B vitamins as a medium sweet potato, or a cup of beans—and significantly more iron than ever before. The sweet potato is obviously more satisfying due to its mass. Also vitamins can be associated to food tastes, which might provide some advantage to enriched rice consumption (who knows).
More products also became enriched with the new 1980 US Dietary Guidelines (the guidelines were specifically written to encourage enriched grain consumption). When you look at the vitamins that are actually added to the enrichment formula, each one seems to have literature linking it to stimulated appetites. I doubt it’s a coincidence.
At any rate, enriched white rice post-1983 was very different from enriched white rice pre-1983. And the post-1983 diet correlates with increased appetites throughout America.
See Zhou et al.’s series of studies between 2010-2015 linking niacin via enrichment and appetite. Zhou mainly focussed on niacin, but the other B vitamins in the enrichment mix are known to be appetite stimulants as well.
The reason this is all important is because when Osbourne and Mendel discovered B vitamins in the early 1920s, they realized that rats lost their appetites when they were fed nutritionless refined foods. At the time this was considered an innate protective measure to prevent an animal or human from being addicted to nutritionless food. So, if you were manufacturing food, and you wanted people to keep their appetites up, you’d find ways to add those B vitamins to refined food.
And that’s exactly what they did. After 1983, the lobbyists significantly increased the dose of B vitamins (and iron) in refined grains and people had bigger appetites for otherwise nutritionless foods.
Duck, very interesting! Can you supply links for us to follow up on this “Vitamin B drives appetite” stuff? Thank you!
Sure…
http://pmid.us/PMC3932423/
http://pmid.us/PMC2874142/
http://www.nature.com/hr/journal/v34/n12/abs/hr2011133a.html
http://www.biomedcentral.com/1471-2458/10/746
http://dx.doi.org/10.1017/S0007114513001815
I can’t vouch for the effects of niacin on metabolism that they focus on. But, the correlations to B vitamin fortification are striking to my mind—particularly when we match it up to the historical contexts. The amounf of B vitamins in fortified food is very high now. Again, a single slice of enriched bread has about as much B vitamins as a medium sweet potato or a cup of beans. It’s crazy.
High iron intake isn’t doing anyone any favors and could be related to metabolic issues, but we recently found evidence that rats can have organ iron overload (say in the liver) even on a low iron diet. And obese people can be truly iron deficient. That implies that the iron overload in various organs can come from mineral deficiencies—say a deficiency of copper, that would otherwise be protective of such iron mismanagement.
At the moment, we are trying to investigate how quick the effect on appetite is. Anecdotally, we’ve seen some people report that if they make food out of enriched flour, they will eat much more than if they make the same meal with non-enriched flour.
One interesting study on the subject was from 1933:
• “Appetite and Choice of Diet. The Ability of the Vitamin B Deficient Rat to Discriminate between Diets Containing and Lacking the Vitamin,” by Leslie J. Harris, Janet Clay, Florence J. Hargreaves and Alfred Ward (1933)
The scientists ran comparisons between deficient diets and enriched diets (often using Marmite, which is rich in B vitamins) and various flavors to see if the rats associated memories of flavor associations.
Interestingly, sometimes the rats did, in fact, have flavor preferences that mislead the rats when palatability was very high. But, in general, on a real foods diet, the data implies that animals naturally lose their preference for non-nutritious foods as they become deficient and naturally gravitate towards foods that have B vitamins in them. This would likely happen seasonally, of course.
Taken together, you can see why non-fortified countries seem to have an easier time with all this. Their less-nutritious food isn’t laced with the very vitamins that signal safety to our bodies.
Duck, thank you for the links! I will look at them soon –Bryan
Forgot one, Bryan.
Vitamin paradox in obesity: Deficiency or excess?
http://www.ncbi.nlm.nih.gov/pmc/articles/PMC4549666/
…Also, I thought this paper was interesting.. It reveals the lobbyist group led the charge to increase fortification in the 1983 decision:
The Enrichment Debate (1977)
http://journals.lww.com/nutritiontodayonline/Abstract/1977/07000/The_Enrichment_Dabate.5.aspx
Doctors opposed the increases, but the grain lobbyists eventually pushed it through in 1983.
I’d also point you to this 1933 study:
Appetite and Choice of Diet. The Ability of the Vitamin B Deficient Rat to Discriminate between Diets Containing and Lacking the Vitamin, by Harris et al. (1933)
If you read through that study, you’ll learn that Vitamin B deficient rats crave foods enriched with B vitamins (though they can apparently be fooled under the right circumstances, which is why food education and traditions are obviously a factor).
The fact that rats crave the taste of B vitamins, when they are deficient, is crucial because obese people are known to be deficient in many B vitamins, for various reasons. So, this would explain, among other things, why obese people may be addicted to enriched foods. They are trying to obtain the B vitamins, but their body isn’t absorbing or metabolising them. Inability to metabolize (synthetic) B vitamins can be due to a number of issues, though copper deficiency is known to affect methylation.
One potential link to iron is that B vitamin deficiency is associated with inflammation, and iron fortification is known to promote inflammation in the gut.
Cheers.
@Duck – doesn’t this mechanism, as described in the papers imply that if one wants BOTH vitamin B3 and non-obesity then the way to eat is like this:
1) Divide food into 2 parts: B3 rich part (B3 supplement, meat, enriched flour) and B3-poor part, containing foods low in B3. Assure that you have a sizable B3-poor part, enough to supress appetite.
2) Eat B3 rich foods or supplements first.
3) Wait as long as necessary for the hunger to appear and develop.
4) Eat B3-poor foods – this surpresses hunger.
Thus you end up with both B3 vitamin and no hunger. But this requires giving up on a concept of a meal – a complex mix of everything together – and replace it with precisely timed feedings of separate types of food. That would be difficult culturally and commercially.
GTR. Sorry, no idea. Zhou is mainly focused on niacin (one of the fortificants they significantly increased in 1981). But, Cowgill coined thiamine the “appetite vitamin” and riboflavin is known to have appetitie-stimulating effects as well. The early studies showed that the animals were only stimulated to eat enriched foods when they could taste the vitamins and were deficient in those vitamins—which I would think would be rather common on a poor diet, since most B vitamins come from our gut flora. Obese people have abnormal B vitamin metabolisms as shown by many other studies (and Zhou too) so who knows what’s going on.
Zhou’s overload theories aside, I find it all particularly interesting for the fact that before enrichments were added to foods, people were known to lose their appetites eating nutritionless foods as they slipped into deficiency. Same thing would happen to animals in a laboratory. It’s only when the taste of enrichments (usually as brewer’s yeast in the early days) were added to the foods (and to rat chow) was the nutritionless food able to become a staple. The early studies showed that only a taste or bare adequacy was needed to stimulate appetite. And the brain could learn to crave flavors associated with that stimulation. That’s mainly what I’ve been focused on. The taste of enrichments enable a person or an animal to eat refined foods—otherwise, they would lose their appetite as they became deficient, or be compelled to crave B vitamins elsewhere. When the animals were vitamin B replete, they would be happy eating some nutritionless foods, until they became deficient, and then they would eat foods that tasted like B vitamins. In other words, it’s a protective mechanism. Zhou briefly mentions appetite stimulation, but he seems mainly focused on the abnormal metabolisms of B vitamins in obese subjects.
Those who were obese eating nutritionless foods before fortification seem to have found other ways to stimulate their appetite with the taste of B vitamins (such as with yeasty beer, for instance). And I’d imagine those in unfortified countries would likely have to find a way (multivitamin for instance) to stay replete in B vitamins in order to keep themselves from losing their appetites, if they truly wanted to eat nutritionless foods as staples. A deficiency changes your tastebuds to crave or accept foods with that vitamin or mineral.
Nice bit of history! I was not aware of this about the B vitamins. Also interesting about empty calories. The standard thought is that we overeat empty calories, but I can’t say I’ve ever eaten a lot of plain rice no matter how hungry I am.
It is interesting that Zhou would use iron as a stand-in for meat though. Meat, and protein in general, tends to be an appetite suppressant. Too much meat is toxic of course, as has been mentioned, but it also just makes most people full. Fish and eggs do the same thing, though I think maybe even more so.
Which is another thing about the 1980’s. There WAS a huge push to eat lots of grains … the infamous food pyramid! And to eat less meat. But something else also changed. They tried to scare everyone away from eggs. Egg consumption dropped drastically, while at the same time we were eating more of about everything else.
So when I was a kid, we ate cookies. But they were either homemade, or else looked a lot like homemade. They were made with butter and eggs. You ate ONE cookie or maybe two … there were very filling. Usually with a glass of milk because kids always got milk with everything.
Now like as not the cookies are egg-free. Often low in fat too, and no dairy either. And you can eat the whole package easily. There is no “stop” button on most packaged foods these days. This saves the manufacturer some money, makes the food keep longer, and allows the consumer to ingest way more calories than anyone needs.
Sweet potatoes and beans seem very satiating to me though probably because of the fiber. Fiber fills your tummy, but it also keeps digesting longer and will keep you more satisfied into the next day. The butyrate from the digestion is actually feeding your gut cells. Modern processed foods are also often very low in fiber (even more so in the ’80s) which would encourage one to eat more often.
Zhou didn’t use iron for meat. Zhou is mainly focused on B vitamins and appetite. McClain et al. 2015 used a *very* high poorly absorbed non-heme iron intake to simulate the the highly absorbable heme iron from meat. That seems to be how they simulate iron absorption from meat. The idea was to get ferritin levels up to what is seen in humans on high (cooked) meat diets.
On a side note… My understanding is that there is a ceiling of heme iron you absorb in one meal (~2mg), but cooking meat transforms a good chunk of it to non-heme. And that (and eating meat too often) may be one of the many ways one can get iron overload as there is something called the “meat effect” where meat significantly increases your non-heme iron absorption. Traditional cultures that were high meat tended to eat their meats raw, which may be protective of iron overload due to the heme ceiling. And the microbes are supposedly not bloomed by all the raw heme meat going through the colon due to the antimicrobial porphyrin ring on heme that is otherwise destroyed by cooking. In other words, the iron perhaps becomes more available to pathogens in your colon when you cook meat and destroy the porphyrin ring. Although, eating raw meat can have it’s own issues. 🙂
Ah ok, I got the incorrect researcher.
Interesting that cooking would change the absorption so much. There isn’t much info on humans and non-cooked meat.
The upshot for me though, was that looking into a “Happy Meal” … between the enriched bun, the bit of meat patty, the soft drink, and the fries, the poor little kid gets a major iron overdose.
“between the enriched bun, the bit of meat patty, the soft drink, and the fries, the poor little kid gets a major iron overdose.”
Kids need iron, actually. But the more iron you eat, the more copper you need to utilize that iron—otherwise that iron just promotes inflammation when it’s not utilized properly.
So, iron is just one piece of the puzzle. Most of the fortified iron isn’t absorbed, but what isn’t absorbed causes inflammation, as explained here:
And the more inflamed you are, the less iron you absorb. And during inflammation the body will also keep iron out of the blood, which makes it go into organs and tissues. During chronic inflammation, this is problematic.
Rats deficient in B vitamins will crave the taste of B vitamin enrichments. Inflammation promotes B vitamin deficiencies and methylation issues. Obese people are known to have B vitamin deficiencies and inflammation—mind you this happens on a diet high in enriched foods.
Gut inflammation decreases one’s ability to absorb these micronutrients, but the point is that the B vitamins are craved and so foods fortified with lots of B vitamins are eaten since they are very rich in B vitamins. Because the iron is inflammatory, the fortifications aren’t well absorbed and the cycle of craving, increased appetite, and deficiency continues.
Does B3 vitamins, including niacin, and appetite, especially for carbohydrates, have something to do with NAD+/NADH ratio? Carbohydrate consumption tends to lower NAD+/NADH ratio to quite low levels, to increase it to healthy levels you can either lower calories, do some fasting, takie niacin, nicotinamide, nicotinamide riboside, or oxaloacetate.
So what rats without niacin did might not be a prevention of bad habit, but a simple NAD+ management via lowering calories, while rats with niacin had their NAD+ managed by niacin, thus could afford to eat more without problems at the cellular levels.
…Also if you look at the studies on tastebuds and deficiencies, you’ll find some very interesting findings. For instance, loss of taste (Hypogeusia) is a sign of a micronutrient deficiency (such as copper or zinc). The tastebuds physically change with various deficiencies.
Loss of taste is particularly problematic and common in the elderly, and this can reduce their appetite. Unfortunately, this puts them at even further risk of micronutrient deficiencies.
Heathertwist, very interesting, thank you for this! I haven’t so much explored the iron element (chem joke haha). Yet ANOTHER novel factor introduced to our environment after WWII. I’ll definitely be reading more about what may well be chronic iron overload from wheat-based food “fortification”– To be clear, the Rice Diet did *not*, on average, resolve diabetes, regardless who may be claiming what. Far from it! The average fasting blood sugar (FBG) for folks after 22 weeks of the Rice Diet was 155 mg/dL! That’s still diabetic! Normal fasting BGs are 75–95. If you want to see these results for yourself you can ask Denise to send you the Rice Diet study–she offered to do this for anyone interested in it. You’ll find the table giving those number on page 360. You note that Kempner started the rice diet before WWII. I’m curious to see the results before and after the war. –Bryan
The other is that the levels of blood sugar required to be considered diabetic have been decreasing as medical knowledge advances. What did they consider to be diabetic blood sugar levels when Kemper did the rice diet?
Rebecca, excellent Q! I also wonder that. Kempner & Co also had the problem of much poorer BG measurement. Direct measure of blood glucose didn’t come along until the late 50s, and not in common use until 1981. Before then, urine strips were the best tool, and they didn’t register until BGs hit 180mg/dL, the concentration at which the kidneys started passing sugar into urine.
N=1short term experiment….
Day #1,
Lunch moderately LCHF (some potato salad)
Dinner strict LCHF
Next day fasting blood sugars at 4.8. All good.
Day #2
Lunch HCLF lunch, whole meal bread
Dinner LCHF
Next day fasting blood sugars at 6.1
So day #1 diet wins, just not sure how sustainable it is to remain low carb. Or what percentage carbs represents the sweet spot.
I have tried HCLF for three days in a row to no real effect. Possibly the type of carbs are of importance. Maybe gluten doesn’t help blood sugar levels.
Glad you enjoyed it!
I agree the Rice diet didn’t “cure” diabetes but it did allow some folks to stop using insulin and lowered their blood glucose. Mind you these were folks that needed to inject insulin, not just folks with a bit of high blood sugar. The limits on what is acceptable blood sugar have gotten lower in the past decades.
Diets like Pritikins and McDougall have brought down blood glucose nicely for a lot of people, including some of my relatives. I don’t know that I’d call it a cure though … the person will revert if they go back to their old diet. The thing is, the modern versions of LFHC all ALSO specify “unefined” starches and to avoid “processed foods” … so it’s hard to get any stats on successes from people eating white rice.
The older Asians I’ve seen in the US are typically still thin and active and eating plenty of white rice. However, they also make an issue of the kind of rice they buy, and “American rice” is considered pretty bad. Oddly, the rice headed for the Asian markets around here is grown in California, but is packaged for Korean or Japanese or Chinese markets, and is not enriched.
http://www.dietandfitnesstoday.com/iron-in-white-rice.php
Instant or parboiled rice (the kind more Americans cook) has the highest iron content: 6mg per cup? Which is almost half the recommended daily intake. What is weird to me is that the rice at PF Chang’s also tastes to me to be parboiled … it’s about as far from “rice” in China as it can get.
Anyway, at one point my fasting bg was up to 120. I started donating blood, and also cut down on things like homemade molasses beer and cooking in iron pans, and fewer steaks. I avoid any “enriched” foods, but don’t especially avoid carbs (I’m big on white rice and sushi!). Now my fasting bg is down to 83.
I did have my ferritin and hemoglobin measured and they were on the high side. If you donate blood they will always check you for anemia and tell you if you are low.
Hey wbryanh, just a quick note on the average fasting blood sugar after the Rice Diet and Pritikin: keep in mind the average includes the (small but existent) minority of people who got worse (often MUCH worse), the people whose blood sugar didn’t change, and the people who experienced dramatic improvements. The fasting blood glucose for those who improved was often much lower than the averages reported in the papers, and frequently in non-diabetic ranges, especially with Pritikin’s diet. Reporting averages unfortunately dilutes the full range of change and can give a misleading picture. From what I’ve observed, the people who do well with low fat do *very* well, and the people who do poorly with low fat often do *very* poorly (a number of genetic, environmental, health-context, lifestyle, etc. factors all contribute to which camp a person will fall in). There are definitely people who have returned to non-diabetic levels eating very low fat — the McDougall website has a collection of individual stories here –https://www.drmcdougall.com/health/education/health-science/stars/ — so it certainly is possible!
Neisy, thank you for stepping in! Any change you can post here the post-study BGs on each study subject for the Rice Diets and Pritikin regimes? (I think we can rightly term these “regimes” given the study leads used whips and other stiff coercive methods to ensure compliance for some of the subjects:-) ) It’d be great to be able to see how many, and how great, the outliers are.
But more to the point: Does extreme HCLF *really* work on a par to LCHF for resolving high blood sugars? For the Rice Study, you say:
“More than half of those 100 diabetic ricers—63%—actually saw their fasting blood sugar drop by at least 20 mg/dL during the diet. Only 15% had their blood sugar go up significantly. The remaining 22 saw little to no change.”
But what were the actual starting BGs? And the post-study BGs? That’s what we really need to know to compare efficacy of HCLF to LCHF.
I realize we have a paucity of LCHF studies. Thus must rely on the giant raft of anecdotal data out there. You can find countless accounts of people who actually *normalize* their BGs–as is, get them down to 75–95mg/dL *all the time*–when they go on LFHC. I am one of those many people. My BGs have been normal for nine years, and now I’m 55. An age where my BGs should be getting inexorably worse no matter what stunning physical and dietary gymnastics I perform.
In general, I’m not ready to accept the idea that these very HCLF diets are anywhere near as good as lowering BGs as LCHF. This makes me question the suggestion/implication that the two ends-of-the-fat/carb-macronutrient-spectrum are equally “magic” in their salubrious effects. I need to see more evidence before I can accept that extreme HCLF offers anywhere near as much magic as LCHF. I’d love to see it too, because I find your argument intriguing, but still need more support IMHO to accept the idea we can put HCLF on the same level as LCHF to drive into remission chronic disease–at least for diabetes. Thanks for listening Neisy! Hope to see your answer when you can write back. –Bryan
I think the LCHF or LFHC issues everyone is pondering over depend largely on the individual what kind of results you will get. In the past LCHF did wonders for me. A bit over a month ago I switched to LFHC to see what would happen. I keep my fat under 10% and pretty much eat only whole grains like oats and other whole foods with tiny amounts of bread here and there. Most foods made from flours, and white rice will spike my blood sugar. A big bowl of oats and a banana for breakfast and my blood sugar is fine. To lose weight on a LFHC diet you have to stick with whole foods, cut the fruit to very small amounts, no dried fruit, or nuts, seeds and avocado. So when people say it doesn´t work for weight loss you have to know what they actually do. I am getting down to those last few pounds that are hard to lose, since I started LFHC I have actually lost a few more pounds.
After a month I did my lab work. Total cholesterol 169, tiglycerides 92, VLDL 18, HBa1C 5.2% etc…. everything good. Every individual has to test on themselves what works and what doesn´t work.
If you want to believe one theory or the other fine, test it on yourself and see what happens.
How long did the switchover take? I think there may be an adjustment period in going from one diet to the other. Certainly there is a lot of talk about the ‘low carb flu’ when moving to HFLC diet.
It took no time at all. I never had the so called low carb flu when I started eating that way either.
The reason I ask is because I find the HCLF diet has the opposite result for me. I.e. Send fasting BS levels up. But it may require more persistence.
Hi Rebecca. Were you in a diabetic state before you went HCLF? The Rice Diet most or all the subjects were diabetic going in. Same thing I believe for the Pritikin studies. And did you get your C Peptide tested? Your A1c looks OK (4.6% or lower is ideal), but your reasonable BGs may or may not be at the expense of chronically high insulin output which incurs its own chronic disease risks, Alzheimer’s among them. All that said, whole foods certainly help whether it HCLF or LCHF. Also, I’d consider the C Reactive Protein test, a very good biomarker for chronic systemic inflammation. Mine went WAY down after going whole-food LCHF. It was 4.4 (inflammatory), now 0.6 (anti-inflammatory).
Yes I am diabetic. I take medication but I take the same amount of medication on the LFHC as I did doing Low carb high fat. That to me seemed very strange but if I stick to whole foods it works. I am going to check my c-peptide to see what my insulin is doing. C-reactive protein could be lower but it was only 2 and up to 8 on the lab ranges was considered normal.
wbryanh, heathertwist- Yes, I see a huge amount of bias against red meat in our current culture, and many of these so-called “studies” condemning red meat I think are so wrong! The mentality seems to be “we know that meat is ‘bad’, now we just have to find a way to prove it”. Also, quite a lot of these scientists in some of the recent well-publicized studies were actually vegans, or at least had some kind of conflicts of interests.
In any case, heathertwist, I know what you’re saying- that seafood is very important- but I’m not ready to say that mostly meat diets can’t be healthy too; I’m sure I’ve read that they can be! I wish I could find a link proving what I’ve read about the Sioux Indians. I know I’ve read that they were in excellent health, back in their heyday- (before the time of the white man). I myself am sort of like Peter Attia- (you posted a link about his diet); I tend to eat more poultry and fish too (mostly due to the expense, as well as the fact that I simply often crave fish). But some people I know don’t like fish so much and eat more meat, and they seem to be in very good health.
wbryanh- this is from memory, so may not be totally accurate, but I recall Weston Price visiting parts of Africa where they ate more meat centered diets (though there may have been lakes around too; he didn’t mention it though). Also, parts of Australia that were inland. I’m pretty sure he visited quite a few inland places, and some where they only ate meat without dairy and fish, because at the end of the book he made the comment that those meat diets *only* worked if they ate the offal too. So, even he was aware that just muscle meat wasn’t good. One more thing: the fat of wild animals on their natural diet also contains Omega-3 (was that what you were asking about, regarding fish consumption?)
wbryanh- I’m sure there was another point that you made that I wanted to comment on, but now my mind is a blank; I’ll go have another look and see if I left something out. (It’s been a long day…..)
Morgana, @heathertwist — Guys, about “red” meat, I’d like to emphasize, the studies on it nearly completely lack any granularity. Possibly to the point of meaninglessness. There’s a huge diff in diff sources, types and preps of meat. None of the studies separate out for animal source of meat (lamb, cow, goat, etc), type of meat (low-load muscle meat, eg tri-tip; high-load muscle meat, eg shanks and chuck; and organ meat and their diff types.) and how the source creature was raised, eg grain-fed, grass-fed. Until recently the studies didn’t even distinguish between processed meat (charcuterie) and fresh meat, which was frankly crazy for these researchers to not resolve out. And the studies still don’t distinguish between fresh whole meat like a cut of steak, and *ground* meat, the latter which almost certainly harbors a higher level of microbes like pathological forms of E. coli like the O157:H7 variant.
All that said…I don’t eat much red meat. But not for the purported pathogenic compounds that it allegedly harbors. Rather to focus on what I perceive to be the greater need for the amounts of the nutrients we get in shellfish, finfish, eggs, and non-cow dairy. I simply steer toward the animal flesh of the greatest nutritional value so I can get all my micros without chowing too much protein. The meat I stick to AMAP are organ meats, esp chicken livers and, when they are available, hearts from grass-fed lamb. And, to a lesser degree, lamb shoulder and shanks, and tongue mainly from beef and buffalo, and brain, usu from pork and goat. The actual amounts of these meats are small, and these satisfy me completely and my medical tests come out excellent.
Morgana, what you said: “…One more thing: the fat of wild animals on their natural diet also contains Omega-3…” I more I think about this, the more I realize that ancestrals, no matter where they lived, likely met their relatively modest needs for long-chain w-3 (EPA, DHA) from a variety of sources. There’s of course the animal brain I mentioned earlier, which are likely our most largest and densest source of terrestrial w-3s. Morgana, as you say, the pastured wild creatures will have it, though they generally are lean, low in total fat, but again we don’t need a lot of w-3. Heather (or Morgana?), as you pointed out, very few ancestrals lived far from some water source, fresh or saline. Land mollusks like snails are a source of w-3s. So are insects, which are still a part of most diets around the world:
http://www.sciencedaily.com/releases/2016/01/160111122520.htm
Bottom line: it’s not that I think red meat per se is necessarily bad for us–esp fresh organ meats and high-load whole muscle meats from pasture-raised animals. Rather, it’s that seafood, eggs and non-cow dairy offer nutrients profiles we need without chronic protein overload. –Bryan
I agree there aren’t good studies. Like I said, I’m looking for examples of a culture or even individuals that eat a “mostly meat” diet and are doing well. I think it’s a fair thing to ask. Some have made the point that there has never been a vegan society that did well long term … but in fact we have examples of that (and examples where veganism DIDN’T work so well). Denise gave a good rundown of vegan or near-vegan diets that have done well in studies.
And we have a number of examples of seafood diets that work well in the long run, where the individuals have healthy hearts, good joints, etc. into old age.
But I issue this challenge occasionally and so far no one has actually come up with an example of a mainly-meat-eating culture that’s very healthy. Actually I have the same challenge for wheat-eating cultures … I haven’t seen any culture that eats mainly wheat as a starch that is doing well.
I was thinking of Mongolia, where they do “eat the whole animal” and eat loads of fermented foods. Their lifespan isn’t very good though (it’s gotten way better over the last 40 years), and they have high rates of heart disease and cancer.
http://donmatesz.blogspot.com/2012/09/grass-fed-animal-products-prevent.html
Hi Heather, @morgana —
Heather, looks like to me we tend to meet at the same place on red meat, if maybe from different ideas for why we should make it a relatively modest part of our foodway.
And you’re right, I also can’t think of a high-red-meat eating society that lived exceptionally long lives. Except maybe the Swiss? Average life expectancy there is 81/85 for men/woman at birth:
http://www.bfs.admin.ch/bfs/portal/en/index/themen/01/06/blank/key/04/04.html
They eat a lot of dairy and meat. I don’t hear much about fish in their diet.
https://en.wikipedia.org/wiki/Swiss_cuisine#Foods_and_dishes
I’d definitely be chary to use Mongolia’s life and health stats as any kind of guide for foodways. Many Mongolians were indeed pastoral nomads until the Soviet Union roped the country into its cordon sanitaire 90+ years ago. Since that time, the USSR, through its puppet socialist gov’t in Ulaanbaatar, sought to settle these nomads in cities and towns, and of course this added grain based foods and all kinds of processed foods, largely replacing their pastoral diet. Most urban Mongolians:
http://www.bluepeak.net/mongolia/ulaanbaatar-life.html
are as likely to chow processed Chinese and Russian crap from the local supermarket as mutton off the steppes.
The Soviets also swept through the country and razed nearly all the Buddhist monasteries, destroying a vital anchor of Mongolian life. These severe dislocations and traumas, which sheared away their traditions, plunged many of these proud but now impotent people–once rulers of the largest empire on earth–into existential crisis. This led to an explosion of alcoholism there, aided by the the vodka the Soviets brought in:
http://www.npr.org/templates/story/story.php?storyId=112485545
On top of that, almost half the country’s population lives in UB, which now vies with Delhi, Beijing, and Tehran, for the title of most polluted city on Earth.
http://www.slate.com/articles/health_and_science/medical_examiner/2013/03/worst_air_pollution_in_the_world_beijing_delhi_ahwaz_and_ulaanbaatar.html
The next largest cities, Erdenet and Darhan, are big Soviet-era mining and industrial centers. So you can imagine the toxins that abound in those environments.
For very *many* reasons, Heather, much of Mongolia is quite UNhealthy. Whether or not they eat the high-red-meat pastoral diet.
Heather, about Don Matesz, I’m sorry to say, but I no longer pay much attention to him. I check his site once a year or so and always come away sorely disappointed. I respect his decision to switch from “paleo” (whatever that even means any more) to a plant-based diet. Only so much of what he does is so sloppy and lacks so much rigor he appears to me little more than a shill flogging his newfound foodway.
His post on the Mongolian foodway illustrates that. Matesz kicks it off saying:
“Mongols eat a diet largely composed of milk products, meat, and fat from free-ranging, organic, grass-fed animals. They consume few plant foods because few edible plants grow in the cold continental climate of Mongolia.”
As “evidence” for this, he links us to a Chinese government site–anything but an academic study. First, we should suspect anything that comes from the Chinese government, which till recently told us Beijing’s air was fine to breathe. Next, it’s not even clear if chinaculture.org discusses Mongolians living in Mongolia, or China’s own ethnic minority living in Inner Mongolia.
Even so, Matesz appears not to have closely read his own link! It makes clear it discusses the *traditional* diet and not the modern Mongolian diet that largely replaced it:
“…The Mongolians’ nomadic way of life determined their diet, which traditionally consisted mainly of the meat, milk and other dairy products provided by the livestock which they tended…today, the diet of the Mongolians has been expanded to include vegetables as well as pasta and rice…”
Further down Matesz says: “Most of them eat a WAPF low-carb primal paleo grass-fed animal fat dream diet…” Which for the reasons I supply above, is complete nonsense.
At that point Heather, I–once again–stopped wasting time at Vital Wisdom. –Bryan
I actually know someone who lives in Mongolia and I asked him about that. The guys he knows eat lots and lots of sheep and bread. He has a housekeeper who bought them “a sheep” and promptly processed every piece of it for eating. He is married to a Mongolian. He loves the culture. By all accounts, their diet is still mostly meat and dairy. And grass-fed. Yes: it’s exactly what WAPF would recommend. And what I tried to do here.
Their lifespan has increased in the last 40 years, Russians or no Russians. But the thing is: when you look at the times of Genghis Khan … the Khans had the same set of issues. Whether it is meat or wheat or the combo I don’t know, but shoot, the Pacific Islanders just do not have the same set of issues. Ever.
So whatever Matesz says … he’s pretty accurate in that post according to other sources. I would point out that the Japanese diet is getting replaced even more by the Western diet … but the Japanese are still doing ok. I’m still looking for the specific things that make people “not do ok”.
wbryanh, heathertwist- about red meat: I’m totally frustrated!….I *know* I’ve read about healthy native peoples who ate high animal food diets. I’ve just spent ages trying to find links on the internet, but no go. What I see is mostly very conventional, highly biased information, and frankly, a lot of crap and stupidity based on nothing like science of any kind.
In any case, heathertwist you said that wheat is a confounding factor, and it is. For instance that Otzi character is exactly what the Paleo people use as an example of all the detrimental effects of a grain based diet! There was a definite decline in health when humans switched to agriculture…..so it most probably wasn’t the meat per se. (As I mentioned earlier, I’ve only read about an association between grain- mostly gluten- and arthritis/joint problems, not with meat. Do you have a link for this? If you posted one already, sorry, I must have missed it). It’s difficult for me to see by what mechanism meat could cause joint problems; especially if one is eating the joint meat, and using meat on the bone, and collagen and connective tissue…..I would think this would be healthy, and actually prevent these problems?
The main problem is that most of the healthy Paleo-style meat eating hunter gatherers are cultures of the past. Most modern day meat eating cultures also eat dairy and fish, both high in taurine, so we can’t really compare the effects. However, there are a lot of healthy meat based groups of people around: the French come to mind- (well, traditionally; they’re beginning to succumb to obesity and other problems due to more junk food in the diet). Other healthy groups of meat eaters are the Austrians, and, though many people don’t seem to know this, in some parts of the Mediterranean they eat lots of red meat- (in some parts of Spain and Italy that I’ve visited. Last I checked, the Spanish were healthiest of the Europeans). And wbryanh mentioned the Swiss, also true.
Then the other problem is that modern day cultures who eat meat also eat things like gluten, vegetable oil, processed food, sugar, etc.; all confounders, so there isn’t really much we can prove one way or the other there. I do know personally people who are doing well by eating lots of meat; my father, for one. Though he’s not as old as your mother (heathertwist), he’s in great shape for his 80+ years, looks very young for his age, his brain is sharp and he has no joint problems or arthritis. I also have a cousin who lives mostly on meat and almost no vegetables or fiber, and he’s very healthy; no health problems that I know about.
In any case, the most renowned healthy meat based cultures were hunter gatherers of the past, and unfortunately, I just can’t find the link to prove it. The early explorers wrote about them, but this older information is not readily available on the internet. They were various African tribes, many American Indian tribes (like the Plains Indians, among many others; as I mentioned, there were many centenarians among the Sioux), and the inland dwelling Australian Aborigines. In fact, on observing their excellent health, and seeing they were free from cancer, one of these explorers had the theory that the key to cancer prevention was to eat more fresh meat, like the native people! (It wasn’t Steffanson, who also wrote a book, it was someone else, who’s name eludes me now. I’d love to read that book though).
I’ve also read that the Brazilian gauchos traditionally ate a mostly beef diet, but I can’t find any information online as to what their health status was like. I don’t know much about them….
So, basically, I’m not really convinced that meat eating people are less healthy, because I’ve read so much that states otherwise.
Since I can’t find the perfect link to prove my point- and I’m tired now, I just spent too much time looking around!- I’ll leave you guys with this:
http://www.sarahwilson.com/2012/08/how-to-live-to-100-eat-pork/
Hi Morgana, @heathertwist —
Morgana, thank you for working so hard to track down those healthy ancestrals who eat high animal-sourced diets, (by which you mean high *terrestrial* animal-sourced foods that give red meat right?) I hope you find it–I’m curious!
Your point about being too many confounders to truly suss out the effects of dietary elements–it is for me right on. Not just within the diet, but also so many factors outside the diet, which include pollution, rates of substance abuse, toxic living places and workplaces, and persistent stresses in societies due to poverty, inequality, lack of rule of law, and corrupt governements. I am not sure there’s any group left on Earth we can look to and say “yes, these people enjoy better/worse health than x solely due to the things they do eat/don’t eat.” Again, to look at the Swiss, who eat loads of cheese and sausage and evidently not a lot of seafood, yet enjoy some of the longest average lifespans on Earth. So many factors at play here, which include, for the Swiss, a pristine environment and a very peaceful and ordered and prosperous society.
That leaves us, nutritionally speaking, new pioneers. We study what anthropological, nutritional, biochemical, and genetic evidence we can find, and make ourselves into our own Grand Experiments. And test, test, test. I feel I am very much one of these pioneers because I eat 80% fat, 15% protein, and 5% carb foodway, compelling me into a more or less permanent deep ketosis. This is evidently an uncommon macro balance even among ancestrals, some shoreline Inuit who regularly chow loads of maktaaq being rare examples who eat similar macro balances. So how will this macro balance work for me in the long term? The jury may still be mostly out, but we may already start to see glimmers of the answer. It will make nine years in July I’ve been in deep keto, and I do and feel fabulous at 55. I walk and run as far as I want and as time allow–today just walked eight miles with 40 pounds of groceries and sundries in my pack. And now I sip a seriously fruit-forward malbec, nibble a sharply barnyardy goat tallegio, and write to you! –Bryan
Riffing off of this….
According to my Swiss cookbook, the Swiss were known to use cheese slices as a substitute for bread.
I’ve been drinking a lot of Walla Walla Vintners malbec lately, which is very fruit forward (more than the Argentines or French Cahors) but not at all sweet. I like malbecs for their astringency, so slowly sip them with meals rather than gulp them down. From time to time I take on the even more tannic Madiran and Irouleguy, grown down near the Spanish border. Not many people can stand to drink them, so they’re harder to find.
I’ve also been hitting the Salish seafood a lot. Fresh steelhead, mollusks and crab. It’s saddening to be the only one digging on the beach, then pass lines of cars waiting in the McDonald’s drive thrus on the way home. I don’t have to worry about my favorite spots getting overdug anyway…some of those quahogs must be 40 years old…
Thanks for this thhq. It was nice to read it.
I like Malbecs, and definitely like them fruity and full-bodied but not sweet.
As kids we went to the beach with pails and trowels to dig up loads of steamer clams, steam them in a huge pot, and dunk them in melted butter and fresh mashed garlic. So simple and satisfying. I can’t remember feeling so pleasantly full eating anything else, not at all “drugged.” –Bryan
Another big fan of Malbec here!
“I’ve also been hitting the Salish seafood a lot. Fresh steelhead, mollusks and crab. It’s saddening to be the only one digging on the beach, then pass lines of cars waiting in the McDonald’s drive thrus on the way home. I don’t have to worry about my favorite spots getting overdug anyway…some of those quahogs must be 40 years old…”
Nom! Salish diet!
“The Salish cornucopia includes a great abundance of roots, greens, berries, nuts, apples, seeds, flowers, honey and tree sap, tree bark, fresh plant sprouts, spruce tips, deer, elk, bear, pheasant, ducks, geese, freshwater eel, bullheads, trout, bass, and sea foods including seaweed, crab, seal, whale, sea urchins, mussels and clams, salmon, cod, halibut, and the small fish they call the oolichan. Together these foods and medicines provided a healthy balance of nutrients.”
https://www.culturalsurvival.org/publications/cultural-survival-quarterly/salish-feast-ancient-roots-and-modern-applications
Super-high taurine diet, along with slow carbs and loads of good polysaccharides.
My observation is that the high-taurine foods are more satisfying. Pair a big platter of clams and a good bottle of wine, and you have a feast! Well, that’s what I had for Valentine’s day … the clams were simmered with onions and garlic, probably not too unlike what the Salish would have done with their wild roots.
I also got a book on Japanese Donabe cooking. Their typical broth base (dashi) is made with shaved dried fish (bonito) and kelp, with some roots and greens added, plus some seafood, poultry, or meat. The “carb” level varies, but wow, is it ever satisfying!
IMHO, you seem to be too quick to dismiss the calorie restriction aspect and the eventual weight loss of these diets as the reason for the ‘therapeutic’ benefits. I noticed you mentioned that weight loss doesn’t correlate with the results in multiple places throughout this blog post. Is calorie consumption not a confounding factor in these low fat studies?
Are you familiar with the Dr. Roy Taylor of Newcastle University diabetes reversal studies? Within a week of a very low calorie diet, hepatic insulin sensitivity and intra-hepatic fat returned normalized while plasma triglycerides halved. In 7 days after just 1.3 kg average weight loss! In obese people, that’s a rounding error. See the link to the study below. I should also mention that despite the diet containing approx 75% sugar, the study participants produced ketones. That’s how compliance was monitored.
Calorie restriction seems to be a simpler explanation than your ‘Macronutrient Swampland Fat Spectrum’ theory.
http://link.springer.com/article/10.1007%2Fs00125-011-2204-7
Here’s a quote from the Kempner Rice Diet in Hypertension study:
“It is not unusual for the weight to decrease
more or less markedly during the first
twenty days. The reason for this weight
loss may be that the amount of food given
does not cover the caloric requirements;
in this case the amount of rice, fruit and
sugar must be increased unless reduction
of weight is indicated.”
This is probably sufficient to reverse liver insulin resistance and alter the hypertensive state.
Are there not examples of insulin sensitivity improving on a ‘swampland’ diet? How do you explain all the Mediterranean diet studies?
Hi Leonard,
Thanks for your comments! I generally agree that calorie reduction is a confounder (both for these studies and for low-carbohydrate studies that lead to spontaneously decrease in calories). Weight loss and calorie reduction is probably a big reason anyone on Kempner’s diet saw a drop in triglycerides, for instance, since most studies using high refined carbohydrate/low fiber intake show the opposite, regardless of fat level.
That said, I’m not sure the confounding is still relevant *years* into the diet, when people’s weight has stabilized (and their energy intake has presumably normalized) but the benefits of the diet remain — as several of the studies in this post demonstrate.
More importantly though, the reason I’m not ascribing the results to calorie restriction is that we have some pretty convincing, direct evidence that dietary fat increases insulin secretion when eaten with carbohydrate (versus the carbohydrate being eaten alone), especially in diabetics. There are a number of other mechanisms (like postprandial blood lipids) that may also play into the etiology of the diseases discussed here.
As for your second point, there are absolutely ways to improve insulin sensitivity when you’re still in the Swampland! They just aren’t a result of raising or lowering dietary fat. The crux of this post is that the therapeutic effects of reducing fat (or reducing carbs) aren’t really seen until we hit the extreme ends of the macronutrient spectrum. Things like the Mediterranean diet improve food quality, introduce a higher phenol and antioxidant intake, reduce low-nutrient/heavily process foods, and bring a number of other changes that will reduce disease risk or lessen existing conditions.
In other words, I’m not saying the only way to improve insulin sensitivity is by eating very low fat or very low carb; just that if we’re going to see a direct effect of macronutrient manipulation, those zones are where it’s gonna happen. 🙂
Denise, just because the weight is stable, doesn’t mean a person is no longer calorically restricted. CR doesn’t mean keep lowering calories and losing weight in perpetuity, does it?
From wikipedia: “Calorie restriction (CR), or caloric restriction, is a dietary regimen that is based on low calorie intake. “Low” can be defined relative to the subject’s previous intake before intentionally restricting calories, or relative to an average person of similar body type.”
So yes, they can still be CR years after the initiation of the diet.
As for “direct evidence that dietary fat increases insulin secretion when eaten with carbohydrate (versus the carbohydrate being eaten alone)”. May be it’s only a problem with repetitive exposure and caloric excess, so the issues could still be caloric excess/restriction and not fat consumption.
thanks.
Do you have a source for dietary fat being insulinogenic? The data I’ve seen – a long time ago, so I can’t easily provide a source – showed an insulinogenic effect from dietary fat only for women, and not for men.
Hi Denise, Thanks for your reply and really interesting work. Must be exhausting responding to so many comments. Looking forward to your part 2.
My point was that there could be a much simpler explanation for the results observed. Given that macro-nutrients and calories are dependent variables, how does one determine the underlying cause of the reversal of these diseases? Looking at other studies and seeing common elements I guess.
I think the problem with this discussion is that it seems to lack a framework or model of disease. Gerald Reaven’s lifetime of work has provided us with such a model. Insulin resistance, and the resulting hyperinsulinemia, most likely is the underlying cause of the diseases studied with the low fat diets mentioned above. From what I can tell this is where the history, biology, epidemiology and clinical data meet. Here’s one example in a study by Reaven mentioned by Stephen Guyenet:
http://press.endocrine.org/doi/10.1210/jcem.86.8.7763?url_ver=Z39.88-2003&rfr_id=ori:rid:crossref.org&rfr_dat=cr_pub%3dpubmed
http://wholehealthsource.blogspot.com/2015/06/insulin-resistance-predicts-variety-of.html
How do we reverse insulin resistance and so the resulting diseases of hypertension, heart disease and diabetes? And does reversal imply cause?
Successful studies and examples of reversing or at least decreasing insulin resistance has one thing in common: substantial cut in calories and ensuing weight loss. From the Mediterranean diet, to low fat (vegan or otherwise) to low carb, to intermittent fasting, to juice fasting (ever see the documentary fat, sick and nearly dead), to bariatric surgery, insulin resistance is decreased and when enough weight loss is achieved it is completely reversed. There are even anecdotal evidence of chemotherapy patients reversing diabetes and hypertension from not being able to eat.
All of this together seems to imply that overnutrition is the cause of insulin resistance. And in susceptible individuals (South asians as a well known example), less overnutrition is required to induce this metabolic abnormality. That’s why BMI and obesity are not perfect predictors of metabolic disease. Some low BMI people are insulin resistant, whereas some obese are not.
My sense is that food quality is less important than quantity. Usually when “quality” rises, quantity decreases. Mediterranean diet for example. Another confounder?
An interesting aside to your discussion above (certainly news to me) is that multiple sclerosis might fit in this framework. I wasn’t able to review Swank’s study. It’s much more obvious when it comes to hypertension, heart disease and diabetes (and maybe some cancers) as opposed to autoimmune diseases like MS.
The ultimate point is that many of today’s well known diet gurus are right in practice, but for the wrong reasons. Reaven plus Roy Taylor seems like a very reasonable model of these diseases.
More Taylor:
Click to access BantingDiabeticMed.pdf
http://link.springer.com/article/10.1007%2Fs00125-008-1116-7
Finally, if you don’t mind, here’s a simple counter-example cherry for your fat spectrum theory:
Aborigines going back to hunter gatherer lifestyle reversed insulin resistance (cited by Michael Pollan in one of his books). Is it quality or quantity? (See table 1 page 2) Greater than 10% fat consumed on average over the 7 week period, but notice how low calories were. Similar to Kempner’s diet (8 kg loss in a bit over two weeks for C.K. 51 year old male, see Figure 1 on page 2 of “Treatment of Hypertensive Vascular Disease with Rice Diet” by Kempner), weight dropped very quickly.
Click to access traditional-lifestyle-helps-Aborigine-diabetes-.pdf
Sorry for the long comment. Thanks again.
Neisy, about what you say here “…we have some pretty convincing, direct evidence that dietary fat increases insulin secretion when eaten with carbohydrate (versus the carbohydrate being eaten alone), especially in diabetics.” Did you ever answer psychohist’s question about the source(s) for this direct evidence? You may have, I just couldn’t find it. Anyway I’d really like to see this evidence too when you get a chance. Thanks –Bryan
Leonard, you say:
“…despite the diet containing approx 75% sugar, the study participants produced ketones.”
Ketosis on a high-sugar diet seems hard to believe, but in the New England Journal of Medicine I find:
“Kempner prescribed a diet composed primarily of rice and fruits. It was low in calories, fat, protein, and sodium (<30 mmol per day) and caused ketosis, weight loss, and a decrease in blood pressure.”
http://www.nejm.org/doi/full/10.1056/nejmsa0903829
Denise, anyone… What is going on in publications/physiology?
It seems that any time the human body is using fat stores for energy, ketones are produced. It’s not specific to very low carb. So any calorie deficit will produce ketones. Occurs during fasting as well.
Mine did, mostly because I am not sedentary anymore. I’m enjoying being high calorie, high fat AND high carb in the exact center of the swamp.
Hi Denise. Thank you for a fantastic investigation rendering into an extremely good article. I´m from Stockholm area and would like to hand you a Nobel prize but sorry I´m not on the committee and can´t find a suiting prize either; but there should be one bettter than the economy prize.
You serve an aspect where we can see similar results in many senses with two kind of opposite diets LCHF and LFHC. It could be making sense of why Dr Kelley/Rodriguez could make opposite types of diets to treat cancer and from what I gather getting results. In the western “either or”-type of thinking (dialectical logic) these things usually leads to conclusions like “confusing…so it doesn´t matter how you eat”. In chinese medicine thinking this is more easily understood even though they would have different explanatory models on how to regulate health with diet. I´m looking very much forward to your part 2.
Peter Torssell (Bach chin med, Jiangxi university)
Denise, Are you familiar with the work of Dr Richard Johnson (U of Colorado, Denver)? He wrote “The Fat Switch” which gives a detailed account of the role of fructose–not glucose–in leading to hypertension and diabetes. Hope you can comment on his findings?
Sincerely,
“Have no idea what to think– or eat–anymore”
Truly impressive work done here. But is it low-fat, or is it low-saturated-fat? If I have whole food plant-based low-fat diet and add nuts and seeds to make it like 50/35/15 (carbs/fats/protein), is the magic lost? Should I just experiment, add nuts and seeds, then ditch them and do the blood work? How do I know which is better?
Dr. Fung has expressed a difference of opinion to your ideas you presented here in your post: https://intensivedietarymanagement.com/thoughts-on-the-kempner-rice-diet/
He mostly expresses a different interpretation of the same data. I do agree that his interpretations seem more plausible.
Both veganism and ketonic diets can lead to selr-righteousness in susceptible individuals.
You are confusing cause and effect! I’ve become vegan because I was self-righteous.
Whether it’s the chicken or the egg (sorry, vegans, that analogy probably sets your hair on end), veganism and self-righteousness go hand in hand. I read an article (on how easy it is to eat vegan) on another blog tonight, wherein the author stated, “But once we accept that veganism is an unavoidable step on the path to an ethical and authentic life, it soon becomes clear that experiences of social awkwardness are trivial compared with the significance that veganism brings.” The author then went on to recommend dumping friends and relatives that didn’t espouse the cult of veganism. I thought that had to be the ultimate in self-absorbed, irony-challenged, self-righteous smugness. But then, I read the comments, wherein one of her friends had written, “Great article. So nice to see an article on veganism that doesn’t bash non-vegans”. Aaaack!!! It’s enough to make one want to go out and eat a 20-ounce piece of prime rib washed down with a fifth of Scotch.
Hey, watch it… I happen to be a Militant member of PETA..!! That’s PETA as in People Eating Tasty Animals. 🙂
Hahaa! Dunno how I missed this gem of a mini-thread till now. Annie, your idea to “eat 20-ounce piece of prime rib washed down with a fifth of Scotch…” Makes me wonder about the fourth caloric nutrient. Does the acetaldehydic diet cure self-righteousness or make it worse? –Bryan
After the preview of the post title some time ago, I was afraid the post would be full of apologetics for low fat quasiveganism. I’m pleasantly surprised to see the admission that it’s not the feel good things like whole foods and micronutrients that are what’s important, at least in these cases, and that the data suggest that fats have to be not just low, but extremely low, to provide these benefits.
I myself am a ketogenic paleo proponent, but I have noticed indications over the years that a very low fat diet might work for weight loss, not least because I was extremely thin on such a diet in my own youth. It’s interesting to see some of the older studies on the matter, even if the methodologies aren’t perfect.
I do have to point out that these results are not actually inconsistent with the carbohydrate insulin hypothesis for obesity.
I loved Taubes’ “Good Calories, Bad Calories”, but one of the weaknesses in that book is that he never really examines where the fat comes from, that is driven into the fat cells by insulin. He seems to assume that it can come either from dietary fat or from fat produced in the liver from blood sugar, but left unaddressed is the fact that the insulin spike is relatively short lived, while fat production from large amounts of carbohydrates takes longer.
I would suggest that in fact, obesity requires both sufficient carbohydrates to produce the insulin spike, and sufficient dietary fat to provide a high level of circulating lipids to be driven into the fat cells. On a low carb diet, you don’t store fat because you don’t get the insulin spike; on a very low fat diet, you don’t store fat because there’s no fat to be stored.
In this article in the Hyperlipid blog (http://high-fat-nutrition.blogspot.com/2015/10/protons-and-ultra-low-fat-once-more.html) which is way over my head, at the end he compares with charts
how very low fat and very low carb affect HgA1c.
Hi Denise,
Can you please read this, possibly groundbreaking, aritcle: “Iron Fortification, Disease, and Obesity: An Update with Data Refinements,” paying attention to this passage:
… and tell me if you think it’s more than a little plausible that one important benefit of a lower-fat diet (depending, perhaps, on which fatty foods we’re talking about) is a reduction in absorbed iron and therefore inflammation and therefore hypothalamus damage and therefore appetite?
Further, it occurs to me that because white grains are fairly bland, many (but not all! and this may explain yet another portion of the differential results) people who eat a low-fat, grain, legume, tuber, etc., diet will probably eat whole grains instead of fortified grains—thus dramatically reducing their iron intake while increasing their intake of copper.
Finally, let me point that Kempner may have had greater success with non-iron-fortified rice than could be obtained in North America now with iron fortified rice.
This was very interesting. Looking forward to see everyones thoughts.
That link about iron fortification was very interesting! (And I’ve read, though I don’t know if this is true, that high iron levels might be correlated with heart disease as well). This fortification theory might partly explain why some European countries, who also eat moderate fat and carbohydrate- i.e., “mixed diets”- appear to be quite healthy- (there isn’t so much food fortification in Europe). I would also like to point out that soy is an endocrine disruptor as well, aggravating the situation even further.
Hi Denise,
Can you please read this, possibly groundbreaking, aritcle: “Iron Fortification, Disease, and Obesity: An Update with Data Refinements,” paying attention to this passage:
… and tell me if you think it’s more than a little plausible that one important benefit of a lower-fat diet (depending, perhaps, on which fatty foods we’re talking about) is a reduction in absorbed iron and therefore inflammation and therefore hypothalamus damage and therefore appetite?
Further, it occurs to me that because white grains are fairly bland, many (but not all! and this may explain yet another portion of the differential results) people who eat a low-fat, grain, legume, tuber, etc., diet will probably eat whole grains instead of fortified grains—thus dramatically reducing their iron intake while increasing their intake of copper.
Finally, let me point that Kempner may have had greater success with non-iron-fortified rice than could be obtained in North America now with iron-fortified rice.
I apologize for the double post, Denise. I didn’t realize your comments were paginated, and was looking for my comment on the older comments page where my comment didn’t appear.
As I’ve explained in another comment (might be in moderation). It’s not just the iron. The B vitamins added to enriched foods are known to have appetite-stimulating properties. And the levels of the B vitamins (and iron) were significantly increased in 1983 by lobbyists pushing the FDA. High iron diets have also recently been shown to increase appetite as well.
The entire enrichment formula (particularly after 1983) seems to be designed to increase appetites. See my other comment when it posts.
Swampland is an interesting analogy – a stagnant mix of land and water. Yet the macro-nutrient ratios particular to swampland need not be endured where the mix of each meal is toward one pole or another. For example fruit in the morning, HCLF for at lunch and LCHF for dinner. The body then has 12+ hours to digest and and deal with the fats that don’t mix with the carbs. This woe was promoted with the Fit for Life diet. I call it cycling – as in moving from McDougall to Paleo. Sitting at one end or the other can be a problematic as sitting in the middle/swampland. I don’t know if this cyclical diet has ever been tested. Mixed versus partitioned meals. I mean you don’t find swampland in nature, which I would assume tends toward mono-meals.
“swampland (I assume you mean HF/HC or MF/MC) does not occur in Nature”. But it does. See my note on human breastmilk, at an average of 52% fat, 42% carb. For comparison, as I noted, a cake doughnut is 51% fat, 44% carb. And, while analysis of Paleo trash midden and skeletal remains gives us a good idea what foods our Paleo forebears consumed, we don’t know if the starchy tubers were consumed with the lean red deer, or the fatty sea mammal, or if they were separate meals.
One of the mysteries of Pritikin is, Why didn’t he convince the medical community?
Bad science seems to have been part of the story.
Here’s an exerpt from a letter by Pritikin to JAMA, 1984:
—————
To the Editor.— Since 1976, JAMA has consistently reported the Pritikin Program unfairly….The so-called Pritikin diet used in the study was neither the Regression diet used at my centers and in all my research since 1974 nor the Maintenance diet described in my books meant for asymptomatic patients….Hutchison’s subjects consumed twice the fat and three times the cholesterol permitted on my more lenient Maintenance diet for well people!
http://jama.jamanetwork.com/article.aspx?articleid=391685
—————
Really, really bad science… dishonest, even.
Testing something else and calling it the “Pritikin diet” should be beyond unethical.
That depends. If the study is on intention to treat – the only way to control massaging of the data to get the results you want – then it has to take into account people who don’t manage to adhere to the diet. Excluding nonadherers is far worse science.
Excellent research and excellent detail. I just listened to your interview on latest in paleo. From Oregon City… Keep up the great work. Billy
etc. … and from minger’s recent twitter posting: “if “Eden” = a place free from both vegan AND low-carb dogma, then yes, I would love to go there! ;)”
hate to say it, but she’s moving away from the low-carb, high-fat nonsense because she’s learning more and more about nutrition …
Denise, I LOVE YOU! Seriously, I wish there were more people so dedicated like you! Thank you for all this work, can’t even imagine how long it took!! Any yay, I’m so glad to FINALLY see confirmed what I had been suspecting all along, that both extremely are actually working…. You’re the first person I know of that actually put together all the research…. We needed this badly! You’re such an enrichment for the nutrition community! Couldn’t be more grateful for this! 😉
But goddamit I just can’t leave swampland… 😀 (I’m a former vegan as well haha)
Daniela
(https://www.facebook.com/Detoxyourlifecoaching)
PS: Oh and I almost forgot, I love your writing style and sense of humour! Keep going! 🙂
With regard to the Inuit’s high fat diet – it’s all about the genetics
https://www.ucl.ac.uk/news/news-articles/0915/170915_Inuit_diet
How the Inuit adapted to Ice Age living and a high-fat diet
The Inuit diet is an example of how high levels of omega-3 fatty acids can counterbalance the bad health effects of a high-fat diet. Fish oils were thought to be protective as the Inuit have a low incidence of cardiovascular disease, but having discovered their special genetic adaptations to this diet, the researchers from UCL, UC Berkeley and the University of Copenhagen say the benefits of the Inuit diet cannot be extrapolated to other populations.
Click to access Science-2015-Fumagalli-1343-7.pdf
Greenlandic Inuit show genetic signatures of diet and climate adaptation
http://www.npr.org/sections/thesalt/2015/09/17/441169188/the-secret-to-the-inuit-high-fat-diet-may-be-good-genes
The Secret To The Inuit High-Fat Diet May Be Good Genes
Inuit Study Adds Twist to Omega-3 Fatty Acids’ Health Story
http://news.berkeley.edu/2015/09/17/what-the-inuit-can-tell-us-about-omega-3-fats-and-paleo-diets/
What the Inuit can tell us about omega-3 fats and ‘paleo’ diets
These genetic mutations in the Inuit have more widespread effects. They lower “bad” LDL cholesterol and fasting insulin levels, presumably protecting against cardiovascular disease and diabetes. They also have a significant effect on height, because growth is in part regulated by a person’s fatty acid profile.
Nielsen noted that this is some of the clearest evidence to date that human populations are actually adapted to particular diets; that is, they differ in the way they physiologically respond to diets. Just as genome sequencing can lead to personalized medicine tailored to an individual’s specific set of genes, so too may a person’s genome dictate a personalized diet.
“People ask themselves whether they should be on a Stone Age diet, for example. The response may well depend on their genome,” Nielsen said
Huh…..is this true then of the Masai, the Samburu, the Sioux Indians, Somalian shepherds, the Tokelauans, the French, the Greeks, the Swiss…..I could go on and on……
Morgana, yup, agreed. About the Inuit fat and glucose gene variant studies, a lot of noise signifying … not much. If I had time, I’d research the vested interests behind these studies, or at least those who reported on them. Who rely on uncritical readers to propagate them.
There is no proof, little if any cause and effect diet research out there. There is just a lot of stuff that points us in different directions, and raises interesting scientific questions. I thought the purpose of blogs is to be able to explore issues.
Rebecca, you’re quite right about the lack of proof. The best we can do is try different foodways, track them as carefully as we can, and measure as many health metrics as we can. I was dx’ed T2D in 2007, and after failing on HCLF, I changed to LCHF in July 2007 with intermittent fasts and constant paring down of engineered foods and non-food products. My BGs and health measures have been improving ever since, and it’s a manageable and even very enjoyable lifestyle. Denise’s examination of the extreme LFHC diet is intriguing and Peter over at Hyperlipid proposes some fascinating biochem to explain how it works:
http://high-fat-nutrition.blogspot.com/2015/10/protons-and-ultra-low-fat-once-more.html
Thus I find extreme LFHC it a very interesting academic exercise AND a possible fallback foodway if I somehow lost access to high-quality dietary fat. However I’m not yet convinced HCLF can effect permanent metabolic corrections any more than HFLC can so for now still see it as just an alternative therapeutic diet that works for SOME people but far from all, and likely truly normalizes the BGs for just a minority. Plus, there’s other factors besides macronutrients, esp the massive amounts of hormone-disrupting chemicals in very many mainstream products we come in contact with every day.
Have you seen these studoes on HCLF diets and reversal of diabetes
http://carbsanity.blogspot.com/2014/12/vegan-ma-pi-diet-bests-conventional.html
http://www.hoajonline.com/internalmedicine/2052-6954/2/3
http://www.nutritionandmetabolism.com/content/11/1/39
http://onlinelibrary.wiley.com/doi/10.1002/dmrr.2519/pdf
http://www.ncbi.nlm.nih.gov/pmc/articles/PMC3477773/
Click to access mr_119.pdf
It just goes to show you can find studies supporting positive results of HCLF and also LCHF for treating disease conditions. Some people will do well on one or the other or maybe even both. I have done well trying both extremes. The point in all of this is, I think, read and decide for yourself if you want to try different dietary regimes. And then pay attention, if it works for you and continutes to work great. If not change. No scientific evidence is going to come out anytime soon detailing a diet for whatever ails us. It is still experimentation time and will be for a long time to come.
Rebecca, I agree. Totally. No study can account for the myriad inputs in our daily lives and our genetic diffs, esp for effects over the long term, over which chronic disease usu develops. Nor will they ever mean much until we greatly refine genetic testing and suss out what the genes actually do, AND if we can convince a meaningful sample of people to agree to live for years in completely and precisely controlled circumstances and submit to around-the-clock observation. Oh, and employ a really smart and completely unbiased research team to develop the methodology and conduct the experiment totally funded by unvested interests. Are you holding your breath for all of that? Neither am I.
Are any of these clinical trials, and which ones? I’d be interested in reading any that are.
Psychohist, all the OP’s links appear to refer back to the same Ma Pi 2 study/studies done in Cuba several years ago.
Correction: these include Ma Pi 2 studies also in Italy, Ghana, and possibly China. But all refer to the Ma Pi 2 diet.
SO – if the same diet get the same results in multiple studies what does that say about the diet?
What it strongly suggests is that my LCHF foodway (80% fat, 15% protein, 5% carb) works far better for me than Ma Pi 2 would. See Table 1 here: http://www.researchgate.net/publication/260212681_MA-PI_2_macrobiotic_diet_and_type_2_diabetes_mellitus_pooled_analysis_of_short-term_intervention_studies. Over the same three week time period, for mean glycemia (mmol/L) for Ma Pi 2 study subjects across the four countries, they started out lower than me (9.0 vs my 9.5) and after 21 days finished much higher than me (6.1 vs my 5.0). All my other blood panel numbers normalized too.
The Ma Pi 2 21-day mean of 6.1 mmol/L is still firmly in the pre-diabetic range. My 5.0 is in the normoglycemic range (4.2–5.3). In three weeks, I dropped from diabetic to normoglycemic.
The book Proteinaholic by Garth Davis MD takes a very intelligent look at the research, and he certainly knows how to evaluate and interpret research studies and makes it clear how he does that.
Davis is a vegan with an agenda
Yes he is, but he was not in the past, he used to believe high protein was good. He does not recommend people go vegan or anything like that, he is clear it is up to each person to decide for themselves. He does do a good evaluation of the relevant research out there
Rebecca, I looked at the doctor’s FB page. It’s very hard not to see him as a strident vegan very much tied to his agenda, however late in life he may have come to it. Even the title of his book gives me pause. We’ve long heard about “sugar-holics” and “carboholics.” But whoever heard of a “proteinoholic?” I googled it, and just about all the top hits relate to this doctor’s book. Not a phrase used in general parlance. Nor have I EVER felt the need to binge on meat the way I often did for baked goods.
Proteinaholic is a turn of phrase it in no way applies that people are binging on protein. He himself is now a firm vegan, he does not say it is for everyone in his book, but yes he absolutely believes it leads to better health. None of us believe everything we read let alone on blogs. Look at all the reports on research studies by reporters they often get it wrong and are not very often qualified to be able to tell good research from bad. My only point was that if people want to know more about research in these areas the book is very well written in that sense and for those who want to know about both sides of the diet spectrum this is a good one. I read the book.
Read the studies – they were metabolic ward studies.
And yes, meant to say Rebecca, I agree absolutely we should be able to–it’s vital for us to–explore issues! For that I found Denise’s to be one of the best, along with Mark’s Daily Apple, Hyperlipid, and many others. I just take issue with folks who make unsubstantiated assertions using merely correlative evidence. Unfortunately, turning correlation into causation is a huge problem, not just among citizen bloggers but even with the most highly placed professionals.
wbryanh- yes, my problem with the whole thing is that this study was obviously biased from the outset. Basically, the whole tone of the article was “we know that high fat diets are damaging, so let’s try to figure out why it’s not harming the Inuit”. When I see such blatant bias, the whole thing loses credibility for me. This is just not scientific. But, it happens all the time I’m afraid.
Logically, it does make sense that the Inuit would need a high fat diet, as they need to get enough dietary vitamin D since they have a harder time getting it from the sun. However, this does not necessarily make high fat diets “damaging” for other people, as there are plenty of native groups living in warm countries who also consume a high fat diet and don’t have chronic disease.
Morgana, per your post, I went back and reread the OP’s links. I though it was the OP who wrote “…can counterbalance the bad health effects of a high-fat diet.” But you’re right, he/she copied it from the UCL piece. Another example of how even a solid-rep entity like UCL can be trailing-edge, can mindlessly parrot CW. Even CW like “dietary fat is bad” which a raft of new research seriously challenges.
The extreme LCHF discussion is very interesting, esp as I start to see emerge biochem mechanistic theories for why it might work (see recent Hyperlipid post). But mainly, I’m wary of the pure macronutrient focus. Human nutrition and health is richly multifactorial. Looking just at one of those factors–here, macronutrients–gives too much potential for confounding factors. Esp these days in our horrendously complex daily environment with 100k novel chemicals since ~ 1945, many of which are estrogenic, are hormone disruptors, which promote chronic cell wall impermeability which helps lay the groundwork for metabolic syndrome, the gateway to much of today’s global scourge of chronic disease. Plus, until recently, food insecurity and subsistence diets were the norm. People had to adapt to what was available, whether LCHF, HCLF, or anywhere in the “swampland.” Viewed through the ancestral lens, a macronutrient “magic-at-the-ends-swampland-in-the-middle” approach, while very interesting, may, in the end, not be relevant. At best it may be something that illustrates proximate causes in a new way, but serves only to confirm and underscore the ultimate causes for our modern nutriment mess. Today’s chronic hypercalorism and chronic environmental toxicity may offer, at bottom, the main explanations for what led us to our current foodway and chronic disease problems. Still, the nerd in me looks forward to Denise’s Part II! –Bryan
I think we should be wary of ascribing too much importance to micronutrients, especially if the data is pointing us to macronutrients as the important factors, as does the data in Denise’s column here.
Psychohist, I agree we should be wary of ascribing too much importance to any “nutritionism” in general, be it macronutrients, micronutrients like vitamins and minerals, phytochemicals, etc. At least at this still early stage of our knowledge of them. I can’t agree though that macronutrients are necessarily the important factors. Completely absent from this discussion: the effect of hidden undeclared toxins present in so much modern food, esp hormone disruptors like BPA and phthalates.
Charles, where in these studies does it actually spell out HOW the genetic variants in Inuit better adapt them to a high PUFA diet? I saw this flurry of announcements about this a month or two back, but none of them explained exactly how the Inuit better utilize PUFAs than the rest of us. In fact, that Berkeley link you give says “…knowledge about the genetic basis of human adaptation to cold climates and lipid-rich diets <>…” the UCL link you give says : “…genetic mutations found in nearly 100 percent of the Inuit are seen in only 2 percent of Europeans and 15 percent of Han Chinese, which means <>…” Charles, first, none of us can synthesize the base PUFAs (linoleic acid, the 18C Omegas 6 and alpha-linoelic acid, the 18C Omega 3). Plus, and more to the point, if the Inuit are already eating loads of EPA and DHA (the longer chain O-3s), then why would they even *need* to synthesize these. To me the reporting on this discovery is exceptionally lacking, even quite poor, and certainly confusing. Any light you can shed on this, I’d appreciate it.
Argg. WP clipped the text between the angle brackets in two places. Replace above with this:
Charles, where in these studies does it actually spell out HOW the genetic variants in Inuit better adapt them to a high PUFA diet? I saw this flurry of announcements about this a month or two back, but none of them explained exactly how the Inuit better utilize PUFAs than the rest of us. In fact, that Berkeley link you give says “…knowledge about the genetic
basis of human adaptation to cold climates and lipid-rich diets REMAINS LIMITED…” the UCL link you give says : “…genetic mutations found in nearly 100 percent of the Inuit are seen in only 2 percent of Europeans and 15 percent of Han Chinese, which means they would SYNTHESIZE O-3s DIFFERENTLY FROM THE INUIT…” Charles, first, none of us can synthesize the base PUFAs (linoleic acid aka the 18C Omega 6 and alpha-linolenic acid aka the 18C Omega 3). Plus, and more to the point, if the Inuit are already eating loads of EPA and DHA (the longer chain O-3s), then why would they even *need* to synthesize these. To me the reporting on this discovery is exceptionally lacking, even quite poor, and certainly confusing. Any light you can shed on this, I’d appreciate it.
Did you look at the ACTUAL study I linked to?
Click to access Science-2015-Fumagalli-1343-7.pdf
Greenlandic Inuit show genetic signatures of diet and climate adaptation
You were born with 2 eyes and 1 mouth – maybe you should read before you speak.
??? Charles, I just cited out of that. Here: “…knowledge about the genetic
basis of human adaptation to cold climates and lipid-rich diets remains limited…”
If you could stow your snide comments and actually answer the question, I’d appreciate it.
Sure it says “Greenlandic Inuit show genetic signatures of diet and climate adaptation” Big whoop. Doesn’t go into HOW this is supposed to work, AFA I could see. Thus, my original question to you.
Charles, let’s break that Berkeley study down more. Here’s the meat of it with my questions IN FULL CAPS:
“Previous studies have attempted to understand the genetic basis of human adaptation
to local environments, including cold climates and a lipid-rich diet (1). A recent
study found evidence that a coding variant in CPT1A, a gene involved in the regulation of
long-chain fatty acid –REGULATE HOW?–, has been the target of strong positive selection in native Siberians, possibly driven by adaptation to a cold climate or to a high-fat diet (2). Another study found evidence that adaptation to the traditional hypoglycemic diet of Greenlandic Inuit may have favored a mutation in TBC1D4 that affects glucose uptake –AFFECTS GLUCOSE UPTAKE HOW? AND HOW IS THIS SUPPOSED TO RELATE TO LIPID METAB?– and occurs at high frequency only among the Inuit (3). However, knowledge about the genetic basis of human adaptation to cold climates and lipid-rich diets remains limited…”
Where’s the takeaway here Charles? In your view? All I see is that researchers found a few gene variants in this Inuit that relate to lipid and glucose metab. In itself, purely correlative. But if these researchers have any idea how the products of these genes are supposed to work mechanistically, they didn’t share it with us. Unless I overlooked it.
Charles, if you can cite the CAUSITIVE evidence in the links you furnished above, then great. Otherwise your claim “With regard to the Inuit’s high fat diet – it’s all about the genetics” is unsubstantiated.
Charles, where in these studies does it actually spell out HOW the genetic variants in Inuit better adapt them to a high PUFA diet? I saw this flurry of announcements about this a month or two back, but none of them explained exactly how the Inuit better utilize PUFAs than the rest of us. In fact, that Berkeley link you give says “…knowledge about the genetic
basis of human adaptation to cold climates and lipid-rich diets REMAINS LIMITED…” the UCL link you give says : “…genetic mutations found in nearly 100 percent of the Inuit are seen in only 2 percent of Europeans and 15 percent of Han Chinese, which means they would SYNTHESIZE O-3s DIFFERENTLY FROM THE INUIT…” Charles, first, none of us can synthesize the base PUFAs (linoleic acid aka the 18C Omega 6 and alpha-linolenic acid aka the 18C Omega 3). Plus, and more to the point, if the Inuit are already eating loads of EPA and DHA (the longer chain O-3s), then why would they even *need* to synthesize these. To me the reporting on this discovery is exceptionally lacking, even quite poor, and certainly confusing. Any light you can shed on this, I’d appreciate it.
It all comes down to give your body the tools to be healthy. Low fat or high fat, low carbs or high carbs etc., get your minerals and vitamins and fat in the right portions. Miss one take more greens, miss one take more fat, miss one take more carbs etc.
Protein Power had a good discussion on insulin and it also went into the influence of the different macronutrients on insulin and glucagon. This is what the Eades stated in the book:
large amt of carb and small amt protein elevates insulin the most and quite significantly — they give it a 9
Carbs by themselves they give a 5
Carbs plus fat they give a 4
Protein, Protein and Fat, High protein and low carb they give a 2
Fat they give a zero. Fat is invisibule to insulin.
So the most deadly diet is high carb and moderate protein: Burger with fries and a coke comes to mind , rather than white rice and juice.
Burger with fries is a high fat diet, which will leave you dead by mid 70’s. High carb moderate protein would be more like sweet potatoes, rice and fish. Like Okinawans and Japanese ate (traditionally), leaving them dead in their mid 90’s. Both diets are deadly but I’ll take the high carb moderate protein for the extra 15-20 years of life.
What’s the ETA on Part 2?
Thanks Denise.
I don’t think there is a simple solution to this whole conundrum. This is a universe that insists on having dietary paradoxes.
Physicists will have developed a grand unifying theory explaining quantum gravity and the origins of belly-button fluff before we come up with a full dietary mechanism for how heart disease develops and the miraculously curings from contradictory diets.
The only common thread to all successful intervention regimes is the word ‘intervention’. Which makes me think it is not about the macro-nutrients at all, but the fact that someone is actually caring.
I think we can conclude from the Sydney Diet Heart Study, that high Omega 6 safflower oil is bad, but I have a feeling that if Denise Minger was handing out free kittens to all the people in the intervention group, and smiling at them while taking their blood pressure, the Sydney Diet Heart study results would have been instead certain proof that high PUFA dietary intervention works spectacularly well!
What the most successful dietary intervention studies seem to show is that good care, strong motivation and convincing pep-talks from an eccentric researcher really work.
I am aware of a concept called ‘small study’ effect. It is the notably larger effect that is always obtained in smaller studies. As we scale up a study, it is understandable that the special attention the intervention patients get is less. We put this down to ‘bad’ science in the small study, but maybe ‘bad’ science means good medicine?
Yes, it is just the placebo effect – but it is a drug you cannot have too much of!
It would be interesting then to run an intervention trial using a traditional witch doctors, kittens* and homeopathy. I am sure that such a trial would produce amazing results providing the patients in the intervention group were getting heaps of attention.
* the witch doctors and the kittens will be kept separate!
Gordon, thank you very much for these new (to me) things to think about! And I am still totally LOL at this: “… if Denise Minger was handing out free kittens to all the people in the intervention group, and smiling at them while taking their blood pressure…”
Presumably no diet study can ever by placebo controlled (i.e. blinded), and is it possible that when someone changes their diet pretty massively, they get a very strong placebo effect?
I haven’t looked through all the comments, nor all of the text in the post, so please forgive me if this has already been covered in the blog post or comments. I’m thinking about how the patients fare on such low nutrient diets. I understand that an “all-fat diet” such as many low-carbers strive for may lack in magnesium and other necessary stuff, but the rice diets and fruit-rice-sugar diets and such appear to be totally lacking in a lot of nutrients! I’m working really hard to get all the nutrients I need while on a nutrient dense diet with a slightly negative energy balance to lose weight but not lose health. I cannot imagine staying on one of those diets for very long helped anyones levels of anything. How do you think they coped?
“I haven’t looked through all the comments, nor all of the text in the post, so please forgive me if this has already been covered in the blog post or comments.”
What you’re really saying is: “My question may have been answered in the blog post or the comments but I’m too lazy to read through it all but I want you take the effort and answer my question anyway.”
No, you’re not forgiven; read the whole post and comments.
They’re weight loss diets, for God’s sake! No one eats like that forever. Atkins is the same thing. You only do HFLC until you accomplish the weight loss then HOPEFULLY go back to a normal diet and maintain.
I have been on diets like that and actually they worked very well for me. Mine were “body builder” diets … uber low fat, with some very lean protein, starch, and vegies. What didn’t work for me eventually was the social aspect (how to eat out?) and I lacked good fats, I think. I seem to need fish oils or my skin gets too dry and I don’t think so clearly. I’m trying it again now with a few tweaks. So far so good. I feel way better … more energetic, stronger.
The 10% fat isn’t far off from some of the traditional diets. The human body is quite able to synthesize most kinds of fat, but some people don’t digest fats all that well, and I think I’m one of them. I just try to make sure that the 10% is the essential fatty acids, not the stuff my body can easily make or has already stored.
Now, I’m using white rice as my main starch, and I’m not particularly avoiding fruit or sugar. So how is my blood sugar? Just fine, thank you.
Long term … I guess I could add more olive oil or ice cream now and then. My diet is more Japanese than Mediterranean though, so maybe it would be more sesame oil. But mostly I’m happy where I’m at. I’m eating loads of my favorite foods, though maybe cooked a bit differently.
Now as for those Norwegians … back in the day, the Norwegians ate a seafood-centric diet, as did the Japanese. And the Irish and English. And much of Asia. The mammal-wheat/barley diet is new to much of the world, and hasn’t been very successful that I’ve seen. I’m beginning to think though, that the “fat” issue is somehow separate, and with the less than 10% fat, even the mammal/wheat diet is less harmful.
I’m rather content with my current high fat way of eating, having attempted vegan and even fruitarian diets in the past. Campbell’s “China Study” was once my “bible,” but Gary Taubes changed my mind. However, I’m not above experimenting with changes just to see what might happen. I have no need to lose weight, nor any real health problems to fix. However, if I did decide to try “taterism,” I’m worried that my teeth would start to decay again like they did when I was gulping down smoothies made from 10 bananas and assorted fruits for breakfast, lunch, and dinner. With all the glowing results from very low fat diets you’ve posted above, did any of the researchers comment on side effects to oral health?
I wonder whether Steve Jobs had good teeth.
In years past I’ve tried several diets that worked really well for me. I.e. I ate about what I wanted to eat (not hungry), digested food well, and was skinny. Unfortunately all of the failed after some period of time … either I stopped losing weight, got depressed, or my skin got too dry. I had a very hard time figuring out what the common thing was between these diets, since all were very different philosophically. Nor why they stopped working.
So now I think I have it … all were (the way I implemented them anyway) very low fat, and as it turned out, yes, low calorie. It’s hard to get high calorie without a lot of fat.
What messed them up, I think, were 1) Wheat: on one of them, you could start eating wheat again after 8 weeks, which was exactly where the diet “stopped working” for me. 2) Lack of ANY fat: I needed something for my skin at least and 3) Lack of fish oils (fish oils make my brain happy). 4) Dairy. Dairy affects me in weird ways, and when I re-introduced it, the diet also stopped working.
So I’m trying again, while JUST concentrating on fat calories. It’s not hard for me to keep the fat calories low if I’m eating “basic” foods and not packaged ones. A big bowl of noodles and kimchi with shrimp and broth works fine for me. I add some oily fish and sesame for skin health.
What I’m finding is that same sense of well-being I had in the old days! What I’m finding is that some of my diets in the old days, although I FELT like I was “eating anything” in fact I tended to eat food I made myself and the actual fat content was lower than I thought it was. For instance: If I make a bowl of rice noodles in a pot of boiling water, and add some frozen shrimp and a cup of frozen peas and some chopped mushrooms and some broth concentrate or Tom Yum mix … it’s a really great huge bowl of noodles. And the fat content is very low. Even adding some salt pork, the fat content is low.
So a lot of it is about cooking styles and ingredients. That is where the 78-year-old grannies win. My own Mom is 90, and she mostly eats things like … cook some chicken feet. Save the broth. Now boil a bunch of vegies in the broth, eat it with noodles or rice or something. She acts like she eats anything, but if you look at her food, it is in fact low fat. She doesn’t digest fat well at this stage of life, and she has gotten skinnier.
Anyway, thanks Denise! This has really helped my thinking about all this. The one thing I fear though. The “food combiners” may end up being correct! Maybe one day we need to be low fat, while the next day we need to be low carb. A meat day, and a non-meat day. Sigh.
Well whaddya know….
Just after I post a similar string on your old Ancel Keys thread, you dug deeper and found his predecessors.
Now start a string on Eat Well and Stay Well and I will be happy. I’ve just gotten to the part about Scientific Dieting, which was Ancel’s name for what I lost all my weight on (and kept off for 8 years). Calorie counting. Remarkably his counts for walking and bicycling are almost exactly what I use. His taste – and attitude – toward wine are similar to mine.
I guess that if you do research for a living for 40 years, your mind runs in a similar channel as Ancel’s. The thrill of running an experiment on yourself, then analyzing the results. Paleo brought a lot of things to the table for me, but nothing was along the lines Taubes and Atkins intended. Things like digging clams, picking berries, walking for hours for no apparent reason, reading books about Catalhoyuk and Salish basketmaking. Things a Paleo would DO.
An actual Paleo needed ketosis like a fish needs a bicycle. It’s the LAST action that saves you when starvation stares you in the face. If you want to live to be 100, Robert Atkins can help you with your obesity, but Ancel Keys is who you want to follow for the long haul. Or Julia Child. Or the Okinawans. Or Lawrence Ferlinghetti. Or Jack LaLanne.
You’re not a Paleo if you think HFLC is the only way to live a long healthy life.
You’re a Luddite.
Some say that digesting animal fats and proteins require an acidic medium, while digesting vegetable sources of carbohydrates requires an alkaline medium.
The theory goes that while we are omnivores, we still need to eat exclusively like a carnivore or a herbivore at each meal, otherwise bad reactions occur in the stomach and intestines. eg. fermentation occurs, and less nutrients are absorbed.
Therefore we should never eat egg sandwiches, or spaghetti bolognaise, or roast beef and potatoes etc.
Perhaps that explains the magic of the macronutrient extremes…?
I am trialling eating fruit in the morning and animal foods like mature cheddar and chicken liver pate in the afternoon to see if I can get the best of both worlds!
Hopefully I can have my fruit and eat meat too!
Note they also say that some salad vegetables can digest in either acid or alkaline mediums.
“Some” say and “they” say? I’m not sure where the idea came about that humans evolved eating their carbs separately from their protein and fats. There is no real evidence of that from the archaeological record. Of course, we don’t know for sure in what combinations or in what order they ate the foods whose residues are found in their trash middens and on cave floors. But as difficult as it was during some periods of the Paleolithic to get enough nutrients to survive, such finickiness on the part of opportunistic omnivores does not seem like a good evolutionary strategy. Further, people living the Paleo lifestyle in historical times were extensively documented by European explorers and they never remarked on what would have been to them an extraordinary segregation of foods. You think foragers and gatherers never popped some berries and a juicy grub or two in their mouths at the same time while working? Pemmican and some other traditional foods were a mix of fruit, meat and fat. And some of the primitive Amazonian tribes discovered in the 20th century ate starchy carbs and “Paleo” beer with their feasts that celebrated the hunters’ skill in bringing home a good-sized kill. And what about omnivorous animals that eat the plant materials in their kill’s innards along with the flesh and innards?
As of 2005, Americans were eating about 50% of calories as fat, per the 2008 study by USDA on dietary trends 1970-2005.
Click to access eib33_1_.pdf
34% came just from fat added to processed foods such as ice cream, chips and pastries. I estimate another 15% from naturally occurring fats in meats, eggs, nuts and fatty vegetables like avocados.
That puts us squarely on the high fat side of the swamp.
In 1970, when Atkins launched his attack on the low fat American diet it was a different story. People got his message and disregarded their concern with eating low fat foods (though not the unpleasant part about reducing carbs). The outcome was less than perfect. Carb consumption increased, though not as much as fat consumption. Calorie consumption increased. The internet and e-mail were invented to augment sedentary time. The net result was an epidemic of obesity. We now eat high fat diets but it’s made our health much worse.
It baffles me that the HFLC community is still focused on defending Atkins’ 1970 tirades. Switching all the fat Americans currently eat from hydrogenated vegetable oil to butter and lard won’t make anyone healthier. HFLC needs to be used as intended: shock treatment for getting obesity under control. But it needs to be applied to current conditions, not some nostalgic Luddite trip back to 1970.
Keys interest in heart health went way beyond population studies. His 1959 book Eat Well and Stay Well is essentially a practicum on how to eat and live in order to reduce CVD risk. He spends 28 pages of the book discussing mortality effects – sex, exercise, salt, fat, stress. He discusses the benefits of unsaturated fats here and there, in particular their effect in stimulating the liver to eliminate cholesterol.
None of this flows in a highly organized fashion. It’s the result of 20 years working as an academic nutrition researcher, and you get wisdom where you find it. For instance, quoting a section pertaining to heart failure from “Salt and Heart Disease”,
“Salt restriction is important for the patient with heart failure because it helps control oedema. In heart failure the heart is sluggish in moving blood along the veins to the arteries with the result that a back pressure builds up and fluid tends to accumulate in the body. This waterlogging (oedema) is both distressing and a serious complication. The extra weight of the oedema fluid, which may range from 20 to 60 pounds or more, means that every movement of the body demands excessive work from an already overburdened heart. Fluid in the lungs interferes with respiration and the patient may literally drown from oedema of the lungs.”
In reading this I immediately thought about Robert Atkins. When I read that he had gained 60 pounds in his last 9 days I couldn’t believe it. Given Atkins serious heart problems, Keys offers a plausible explanation for Atkins death. It is unfortunate that his wife did not permit an autopsy. We would then know whether he had recently suffered a coronary event, or whether he had drowned in oedema fluid.
According to all I’ve heard and read, Atkins had medication-induced edema, and it happened after he was in a coma. (His cause of death was slipping on ice). Medications can sometimes cause drastic effects; I know this, because at the end of my mother’s life she grew to about twice her size, rather quickly, also due to edema from medication. I saw a documentary about Robert Atkins, and they showed him not long before he died; he looked healthy, of normal weight, and energetic. His wife said people were out to get him during his life (I don’t remember her exact words, so this is not a quote)- and she was appalled that the rumors continued after his death. Which may be a reason why she did not want an autopsy. He should be allowed to rest in peace.
I don’t doubt that medication could induce it, but most of the fluids probably came from an IV bottle. The result is the same. The heart can’t move the blood to the liver and kidneys. If the blood can’t move the fluids have to stay in the body.
I’m trying to be dispassionate about this. As someone who worked as an industrial research scientist for over 30 years, I admire Keys because of what he accomplished as a dispassionate researcher. He was not being sentimental when he developed his high calorie density paratrooper rations, nor was he being sentimental when he created the Med Diet. These were BIG accomplishments that resulted from projects that had highest priority.
The more humdrum day-to-day stuff of research involves testing small-time theories, most of which are slashed to ribbons and disposed of as quickly as possible. I was called upon to do that a lot. It was usually with eager salesmen trying to sell their product by attacking their competitor. I acted as a first screen to politely propel them back out the door before they could waste the time and money of people in operations. Having done that for years, my outer defense shields go up when I see people like Eades, Taubes and Atkins committing ad hominem attacks on their competitor Keys (Eades called him an old drooler, not a tactic you should resort to after someone has had a stroke at age 98). By unfairly attacking their competitor they set themselves up. They’re too eager to sell their books and products, and their theories unravel under minimal scrutiny. I’ll give Eades credit for piqueing my interest in Keys though…a year ago he wasn’t even on my radar.
If the HFLC community cannot leave Keys to rest in peace, I have no qualms about leaving Robert Atkins to rest in peace. Keys was interested in CVD mortality. Based on my familial history, so am I. His wife’s paranoia has deprived me of mortality data on THE most important HFLC supporter. In the absence of that I am left with substantial evidence that Atkins died with a weak heart and a history of severe CVD problems. These may or may not have been a result of HFLC, but it is enough for me to kick HFLC out the door as a strategy for long and healthy life. There are several better proven routes which are promising. Keys Med Diet may not be the best but it’s a contender, along with Cordain’s Paleo Diet, Okinawan and Jack LaLanne.
So….what? You’re starting rumors about Atkins just as a sort of revenge, because other low carbers said things you didn’t like about Keys? This is ridiculous, sorry! If someone says something inaccurate about Keys, by all means, feel free to defend him (as I did with Atkins), but there’s no reason to say things that are untrue about his “opponent”. I think we should all be interested in searching for the truth.
And while we’re speaking of ad hominem attacks against an “opponent”: you do realize that Keys sometimes did this himself, right? Apparently, a Dr. Yudkin had very different theories about heart disease than Keys did (he believed it was caused by sugar)- and apparently, Keys managed to discredit him. The way I heard it, calling someone a “Yudkin” was an insult, back in the day.
Read the next section. Keys was a bit of a blowhard (look at how he blows off ketosis – like waving a red flag in the face of the HFLC advocates), and pretty full of himself when recommending a good bottle of wine. But he had a sense of humor that Taubes, Eades and Atkins lack.
I just finished up a stint as an executor. I’m not getting any younger, and I’m looking for a best strategy for a long and healthy rest-of-my-life. I don’t see the evidence for HFLC being anything beyond a weight loss strategy to deal with obesity. I don’t see any evidence for raw veganism either. If you know something better than Ancel Keys Med Diet, or Cordain’s Paleo, or the Okinawan sweet potatoes, show me. That’s why I came. Right now I live in the exact center of Denise’s Swampland. I could go for more carbs, or more fat, but I’m not seeing a compelling reason to live out on extremes either way.
thhq- I wasn’t criticizing your diet, I was only irritated by personal remarks about the low carb leaders. I’m personally not convinced that “swampland” is such a bad thing…..at least, many healthy populations seem to be eating both fat and carbohydrates, and doing fine that way.
And may I also add that low carb does indeed have benefits other than weight loss, at least for some of us! I am actually a thin person, and I’m not looking to lose weight, but I’ve had digestive issues my whole life. I was inspired to go low carb after reading the book “Life Without Bread”; it was written by 2 doctors, and chronicles all the health problems that Dr. Lutz was able to eradicate in his patients while having them eat low carb. The diet really helped me a lot, not just for digestive issues, but for all kinds of other things as well.
Thanks. I really need evidence for a larger HFLC group than just one person. Do you know of any other HFLC groups studied besides the Inuits?
I have the same feelings about exercise as you do about bread. I worked in Bordeaux, France for 2 years and lost 15 pounds. I was eating ad libitum. Bread, couscous, pizza, fries, pasta, duck (the wonder food), all kinds of seafood, beef occasionally, rich desserts, pastries, and red wine. I was walking an hour each way to work, and constantly wandering around exploring the town. When I moved back to the US I regained all the lost weight and more. 6 years later, when I finally had to lose the weight (obese and diabetic) I started walking again and the weight came off fairly easily. I was able to reduce high blood sugar with carb restriction, but after losing 25 lbs my ability to handle carbs without glucose spikes came back. Because of these experiences I’m not inclined to shift macronutrients to extremes.
One thing about slipping on ice. I did it a lot living in the Midwest, and hurt my shoulder pretty badly in one fall. Falls become more damaging as you age and I feel for Dr. Atkins in this regard.
thhq: Well, aside from myself, I do read about many other individuals who swear by the LCHF diet, and claim it got their health back in order. As for traditional native cultures: there are the Sioux Indians (and I believe, other Plains Indians). They lived mostly on buffalo meat, ate lots of fat (think: pemmican), and were noted for their exceptionally good health. There were many centenarians, back when they were still eating their traditional, mostly meat diet (sadly, this has changed now). Other examples are the Masai and Samburu cultures, in Africa, who ate mostly meat, milk and blood. They were also very healthy. Then there are other northern cultures like the Mongolians, the Siberians, etc. Also the Sami (native Swedish), who apparently were also very healthy. And it’s probable that our ice-age ancestors ate mostly LCHF, and hey, we survived this long!
I don’t mean to imply that you need to change to this diet, especially if your own diet is working for you. But obviously, LCHF works for many people. By the way, I also exercise a lot; I find it very important (and my job requires it). Even still, I think I have some carbohydrate intolerance. Back when I ate high carb, I didn’t measure my blood sugar regularly, but I recognize now that I had symptoms (all gone now that I’ve gone low carb). Even though I’m thin, diabetes and hypoglycemia run in my family.
thhq, you’ve spilled loads of words here, a lot of them around macronutrient balances. Let’s make it simple shall we? Try different diets. See which works. Ancestral foodways range from high carb (e.g. Kitavans) to high fat near near no carbs (e.g. Inuit). In nearly all cases though, the food was organic/pesticide free, non-GMO, fresh, locally produced. Stick to that AMAP. Make sure your food is as pure as possible. Best is the least done to your food between it was raised and when it gets to your kitchen. LFHC works for some. HFLC works for others. For me HFLC works worked wonders. I’m at 80% fat, 15% protein, and 5% carbs. I’m 55, been HFLC for 9 years, feel great, enjoy great blood panels, and feel utterly satisfied. I can’t imagine going back. The whole thing about what food culture figure said what about another food culture figure–it just doesn’t materially contribute to the goal of improving our health.
Thanks. I do have a leaning toward Paleo, though I see it as a lean meat and seafood (especially fresh mollusks like oysters) approach rather than fatty meats. But I strongly believe that there’s a greater benefit comes from activity, rather than macronutrient balances. I like this piece by Cordain.
Click to access Exercise-Like-a-Hunter-Gatherer-Organic-Physical-Fitness-Prescription-The-Paleo-Diet.pdf
Extended exercise turns on my metabolism, and anything available in my bloodstream is used for fuel. I can eat cake or steak and my TG’s and blood sugar are the same. Whether it’s fatty acids, proteins or glucose it all gets turned into carbon dioxide.
An exceptional review by Denise, and she’s not even a biochemist or a physician !
Thank you for broadening our horizons and shattering private biases and doctrines.
Waiting for your second part.
Thank you also for mentioning the Randle cycle on Ben Greenfield’s podcast – certainly opens a new gateway to looking at the relationship between carbosis and ketosis and the plasticity of our physiological adaptations.
I now regard Terry Whals’ MS ketogenic protocol not as a contradiction to Swank’s work, but rather, complementary.
Both represent the two extreme ends of the the % fat consumption pseudo-opposites.
Douze pointe
These series of books are not really rare, and are considered out of date.
http://www.volumelists.com/detail.php?ser=Life%20Nature%20Library
However, they do have pictures of how people looked in the environment the lived in and why/how the adaptation helped them to survive. Was the diet optimal? Did the diet or the environment made them that way. Diet was mentioned in the ones I read- The Desert, The mountains, The Forest, and Australia. . One example listed is the Mountain dwellers diet of potatoes, beans in some areas, end ancient grains, and not much meat or fat at all They could not afford to eat their llamas. They were said to have cracked feet, eyes because of lack of fat. They were also hungry and overworked.Chewing the coca leaves at least kept them in a state where they did not feel the hunger or cold as much. But they were addicted. Also in the book the yak butter in Tibet kept those people warm. They at least had enough Yak to eat. Also in those books plants, and many animals are shown as adapting. That what make subspecies. The word epigenetics was not mentioned in those books, but still saying adaptation is enough of an explanation. .
Dr Weston Price of course noticed the changes in how the nest generation of those people looked, and Price said it was the change in diet, Disease was also mentioned in Price’s book and those Nature series books. The Nature book said if those people left the mountains, they got tuberculosis. but were subject to whopping cough there. Those in Iceland have a long history of putting babies out in the cold, but kept warm to prevent tuberculosis. Studies do seem to indicate sunshine and fresh air will reduce infection.
So which mountain dweller-Peru, or Tibet was healthier, or did both of them have different problems?. Some in Tibet were eating meat/fat and some wheat, potatoes. Of course, in all those places, the peoples religion played a big part of what was eaten, as much as availability and social status and even if male or female.
“That morning he had advocated lighter lunches and now he ordered nothing but English mutton chop, radishes, peas, deep dish apple pie, a bit of cheese, and a pot of coffee with cream, adding, as he did invariably, ” And uh- Oh, and you might give me an order of French fried potatoes.” When the chop came he vigorously peppered it and salted it. He always peppered and salted his meat, and vigorously, before tasting it.”
Sinclair Lewis, describing the eating habits of George Babbitt.
I’ve been thinking about Ancel Keys at the University of Minnesota. He doesn’t write as well as Lewis (or later, Garrison Keillor), but he has the same sharp wit. He taught and researched nutrition in the land of Spam, Betty Crocker and recent Scandinavian immigrants. He discusses the training table of the Golden Gopher football players ca 1940 at length in Eat Well and Stay Well:
“The team player’s diet is apt to be built on the same philosophy as the old Chinese idea – if you want to be big and strong you eat the muscles of big and strong animals – plus the notions of nutritionists who believe that whatever grows baby rat meat faster is better. So they are stuffed on the biggest (and most expensive, therefore fattest) steaks to be found, they guzzle gallons of milk, and nowadays may be plied with vitamin pills as well.
This is an indoctrination into adult dietary foolishness. When the rowing blues leave the university and no longer are forced to keep in training they soon turn into heavy business men; not much later the atheromata are in full bloom in their arteries.”
I think more than a little bit of this high fat animosity creeps into the national diet studies later on. Keys next door neighbor in Italy Marti Karvonen led the Finnish section of the Seven Nations Study. Here’s his description of the Nordic White Diet, which would have been familiar to Keys in Minnesota:
He remembers Finland in the ‘50s. “In those days, in the winter time, we had bread, potatoes, milk, and pork with layers of fat on it. There was nothing green seen on the table — maybe the table cloth.”
Click to access AncelKeys.TONICS.pdf
This is where Keys was coming from. Direct observations of bad diets resulting in bad CVD outcomes.
It would be interesting to see someone do thesis research on the psychopathy of the HFLC community towards Ancel Keys. One could start with Ancel’s summary dismissal of ketosis and build from there:
“Severe epileptics were once treated with a high fat “ketogenic” diet so as to overwhelm them with fat in their diet (80 per cent of calories) to the point where the fat could only be incompletely “burned” in the body and the “smoke” of this incomplete combustion, the “ketone bodies”, would accumulate in the blood. This is a heroic measure, only justifiable as a last resort in uncontrollable epilepsy. Fortunately, this is practically never used today. The basic physiological unsoundness of the “ketogenic” diet is well recognized. New drugs are available that do a great deal more for the epileptic patient.”
This was written ten years before Atkins Diet Revolution. Keys hadn’t realized that ketosis could be used to treat another chronic illness – obesity. But Atkins and his later followers wouldn’t let up on Keys. It got sillier and sicker as they fabricated and cherrypicked their ongoing smear.
Atkins may have first read about ketosis in Keys book for all I know. If he had accepted the “heroic measure” statement maybe we would have been spared Taube’s insulin theories and ad hominem attacks like this one from Eades:
https://proteinpower.com/drmike/2007/11/04/jack-lalanne-vs-ancel-keys/
We’ll see who drools last. But first Eades has to make it to 100 on HFLC.
So…. does this explain that loud mouthed Australian guy and his bananas ?
Yep.
Norm: I think you must mean Durian Ryder? (Yes, he is a loudmouth, ha ha). Personally, I think there is something “not quite right” about him. He may be thin, but he doesn’t look particularly healthy to me; his skin doesn’t look very good. Also, he seems rather hyper and a bit “mental” in my opinion; I’m not sure that he’s the picture of health. I’m not saying all low fat diets are bad, I’m just not sure that Durian Ryder’s particular diet is a good one. I wonder if he has too low cholesterol.
Lol! Durian Rider would put you to shame im Anything athletic. You should keep uninformed opinions to yourself. He and his diet is nothing short of incredible, eating nothing but carbs for 11 years straight and having that level of fitness is amazing. As far as his personality and skin, blaming anything on diet is rediculous because we’ve all seen horrible looking people eating types of diet and the same can be said for mental health.
How the heck do you “know” that Durian Ryder would put me to shame in anything athletic? I am also very fit and athletic, thank you very much! So you should also keep “uninformed opinions” to yourself. It’s fine to disagree with what I say, but criticizing me- when you don’t even know me- is just crude.
I just doubt there are many around who are at his level of fitness. Let alone many reading health blogs.
Hear, hear, Morgana! Zach’s totally out of line here. You should feel free to give your impressions here. And of course Zach has no idea your fitness level–that’s just meaningless blather. At this link is a guy who shattered the record for the 100-mile Western States run and he professes to eat low-carb:
For that matter, how do we KNOW Durian Rider eats what he says he eats? Who’s the 24/7 fly on the wall to verify his claims? It’s possible that in the beginning, he actually followed his diet. Then all excited as he is wont to get, DurianRider started wildly flogging his foodway as the panacea and he got his franchise going. Now he’s locked in to his party line, even if he’s quietly discovering that he needs more fat/protein and is eating it. We just don’t know!
Finally, I’m very suspicious of anyone who claims we should take supplements as a general rule. Here he promotes Vitamin B12 injections: https://www.youtube.com/watch?v=arElYUnWrho
No thanks! I’ve been LCHF for 8.5 years and it’s been a lifesaver!
Lol! That guy eats high carb when he does his races. Whatsup with low carbers and not doing any background research whatsoever?
Also yea, no low carb/paleo gurus push supplements. Except omegas, protein powder, stimulants, vit d, magnesium, k2…. I could go on forever. Guarantee the average low carber takes 5x as many supps as vegans.
Sure Zach. DR may chow a lot of carbs for his hard rides. Fast carb recovery meals make sense for heavy resistance training where you’re rending muscle tissue. Mark Sisson makes that clear at Mark’s Daily Apple.
But what does DR eat at other times? Who’s a fly on the wall watching him? Just sayin. Remember Zach this mouthpiece now has a following and so has pressure to sell a consistent message.
About supps, Sisson also sells his line of supps, but he very low key about it in his blog, and makes clear that it’s best to get all nutrients through food. I was diag’ed T2D in 2007, been LCHF for 8.5 years, stopped all supps 6.5 years ago, and now have completely normal blood panels including normal BGs.
About these your sentences: “Whatsup with low carbers and not doing any background research whatsoever?” and “Guarantee the average low carber takes 5x as many supps as vegans.” these are mere words you just pulled out of your backside, the first a mere opinion and the latter with zero substantiation. Zach, maybe you should heed your own admonition?–“You should keep uninformed opinions to yourself.”
Hahaha! Sisson makes his living selling supplements from rubes who are dumb enough to buy overpriced garbage.
Durian has youtube daily for 6 years or more. He puts on fruit fests with thousands turnout. He talks the talk and walks the walk without a doubt.
Don’t be jealous you can’t lose those lbs on low carb. It’s just not how our bodies were designed to work. You should follow some of this blog posts advice!
“Don’t be jealous you can’t lose those lbs on low carb.” Zach there you go again, blathering on without a clue of my situation, just like you did with Morgana. I lost 60 pounds on LCHF. Effortlessly.
As for “Durian has youtube daily for 6 years or more…” you underscore my point. DR now has a following and so feels a pressure to maintain a consistent message. As far as you saying “He puts on fruit fests with thousands turnout.” so what? That still doesn’t tell us what chows down behind closed doors. Finally Zach you say “He talks the talk and walks the walk without a doubt.” As though your preceding meaningless statements somehow even begin to support this claim.
But Zach, please feel free believe what you want to believe. Far be it from me to try to disabuse you of your cherished religious fervor. Just please don’t confuse your beliefs with anything remotely to do with rigorous science and sound nutrition.
You can say the same for Mark Sisson or anyone else pushing a diet philosophy. What an uncouth thing to say, you are basically slandering someone just because your jealous of them.
As for my thoughts on diet, they are based on sound science like this blog post shows. A high carb, very low fat diet is key to health and longevity. Science AND history back this up. Paleo is a silly fantasy fad that is ruining health on a giant scale.
Let’s compare two vegetarians, Durianrider and Hitler. Both self-righteous, quarrelsome and antagonistic. Avoiding animal foods does not turn someone into some saintly person who respects HUMAN dignity.
I won’t dispute that HFLC does exactly the same thing. I spent some time looking for a video of the screaming matches between Atkins and Pritikin, but couldn’t find one. One of the MANY keys to health and longevity is serenity. Living out on polar extremes – dietary, religious, political, etc. – and fighting your “opponents” all the time because they are “wrong” only shortens your own life.
Whatever else he was, Hitler was a genius so I’m not sure where you going with that.
Zach, your logic fails are legion. First, maybe you should learn what “slander” means before you plop it out here. Look it up hotshot: http://legal-dictionary.thefreedictionary.com/slander
“… someone tells one or more persons *an untruth* about another… ”
So where am I saying “untruths” about Banana Guy? Right, NOWHERE. I’m simply calling out what we DON’T know about him. And you’re right, we don’t know what any food- and lifeway advocate eats behind closed doors–including Mark Sisson, Robb Wolf, John MacDougall, Dean Ornish, and on. We are then left to sort out and make sense of their messages. To look not just macronutrients and whether the food is plant- or animal-sourced, but also nutritional biochem, genetics, including epigenetics and microbiome genomes, and anthropology including paleo- and cultural anthropology. Most of all, we need to see how a given foodway works on each and every one of us. That includes how well we can tolerate the foodway.
Here Zach you sail right off the deep end: “…A high carb, very low fat diet is key to health and longevity. Science AND history back this up. Paleo is a silly fantasy fad that is ruining health on a giant scale.” First, science backs up NOTHING you say. Under clinical observation, few if any people stayed on Kempner’s Rice diet more than a few years. And as far as “resolving diabetes” the average fasting blood sugar (FBG) for folks after 22 weeks of the Rice Diet was 155 mg/dL! That’s still diabetic! Normal fasting BGs are 75–95. This Rice Diet is hardly a ringing endorsement for completely resolving diabetes. I was T2D in 2007, and since *normalized* my BGs with LCHF, averaging 90 mg/dL. Zach, Denise will send you Kempner’s report on this if you care to bother to check it for yourself. Swank’s protocol is more interesting, but still the sample rate is small (150 and diminishing) and self-reporting after a short study period. And who independently verified what data Swank & Co entered into the logs? Again, we have to remember that when a researcher gets very invested in a theory and spends his life working on it, all too often the data can start to magically reflect that desired outcome. Same case with Morrison’s post-war study: small sample rate (50 control, 50 on LFHC diet), self-reporting, no independent verification of nutritional data. About the Pritikin diet, looking at the study Denise gives, (http://ajcn.nutrition.org/content/29/8/895.full.pdf , Table 2, pg 895), the average post-study FBG was 136–still diabetic! Same thing for a Pritikin 1983 study: post-study FBG average is 133 mg/dL. (http://care.diabetesjournals.org/content/6/3/268.short) About the Esselstyn diet results, you can read Denise numerous caveats about this, to which I add that the average study period was under four years and looked just at CVD, not all-cause mortality.
The fails just keep on coming. Most people find these diets very difficult to adhere to over the long term. Most include vitamin and mineral supplementation. Maybe funniest of all Zach, none of the studies Denise cites in detail support the vegan lifestyle your beloved DurianRider so stridently touts except that from Esselstyn. Your concluding sentence “Paleo is a silly fantasy fad that is ruining health on a giant scale” could not be more meaningless, ridiculous and even dangerously wrong. For the hundreds of millions of people on Earth who now suffering from serious sugar metabolism dysfunction, based on the “science” I’ve seen the low-fat high-carb diet will hasten their sickness and death compared to the low-carb high-fat foodway.
Lol, you type up all that just to show your ignorance in your last sentence. FAT is the reason people have issues with sugar. It’s a shame diabetics like yourself don’t know the simple facts that fat, mainly pufa causes diabetes.
You can not cure diabetes with a low carb diet, only “manage” it. You can cure it if you rid your tissues of pufa. That is what these people are doing. You should try it!
P.S. I never said veganism is the answer, I just find it funny that “banana guy” has more athleticism than any paleo guru out there.
Ummm, “science AND history”??? Citations, please, on both. Or even on either.
Zach, please take a moment to reflect on how insane this your comment is: “FAT is the reason people have issues with sugar… ” Zach, I ate HCLF all my life to 46 and *became* diabetic. I went LCHF and my BGs then *normalized.* Are you trying to tell me I imagined my recovery? That my glucometer and my HMO are all telling me the same lie for nine years? You can find countless accounts of other people with the same experience. Please get a grip Zach. The only redeeming shred you said is about PUFAs. We should reduce those as much as reasonable. Esp Omega 6, esp by cutting out veggie/legume oils.
Nothing “cures” Type 2 diabetes. Any more than ceasing to drink poison “cures” you from the effects of that poison should you start drinking it again. Zach you will not be able to furnish even a single link to any clinical study that consistent, reliably, irrefutably shows that any diet, LFHC, HFLC, whatever, “cures” T2D across a cohort.
Gee I wonder why other cultures eating hclf their whole lives don’t developed diabetes? Maybe because they actually eat whole foods and no oils or fortified grains.
Fats, mainly pufa absolutely do cause diabetes. Sugar and carbs are only a secondary effect.
When you were HCLF what did that look like? McDougall and others are extremely low fat, less than 15%. It’s not an very varied or interesting diet as a result, but many swear by it as having turned around any blood sugar issues.
So possibly you were in what Denise refers to as swampland. And go out of on the left rather than the right.
I skipped carbs yesterday out if curiosity. Fasting blood sugars went down from the usual 5.5 to 4.8.
Zach about this from you: “Gee I wonder why other cultures eating hclf their whole lives don’t developed diabetes? Maybe because they actually eat whole foods and no oils or fortified grains.” See my response to your “bubble” comment, where chronic disease is soaring worldwide.
About pufa I agree they contribute to the problem. In particular omega 6, and all rancified pufa. We should stop consuming veggie/seed/legume oils. Ditto for fortification, which may contain undeclared toxins acquired during their productions, e.g. heavy metals and estrogenics like BPA and phthalates. Companies in China make most micronutrient supplements. I disagree that sat fats and mono fats “cause diabetes.” These do not oxidize as easily as pufa, esp the sat fats, and so are a very clean fuel. Zach if you eat a lot of fiber you are in effect eating fat. In our colons, our gut flora ferments much of the fiber into short-chain fatty acids which directly nourish the endothelial lining of our colons. When you eat excess carbohydrate–carbs that can’t go to directly build/repair muscle or get made into glycogen–the liver converts that glucose into palmitic acid– a long-chain (16C) saturated fat! That’s why people who chow excess carbs get fat.
The “fortification with heavy metals” that really makes a huge difference is iron. The reason PUFAs oxidize is largely because iron acts as a catalyst. If the US and some other countries, large amounts of iron are added to white flour, masa, breakfast cereals, and most processed foods. But not to whole grain foods.
With saturated fat, the fat is usually attached to red meat, which is high in heme iron, the most absorbable kind. Saturated fat also makes fortified iron in, say, bread, more absorbable.
The iron in fruits and vegies isn’t very absorbable at all.
So iron messes with insulin levels:
http://diabetes.diabetesjournals.org/content/51/8/2348.full
To the point where people who are accidentally overdosed with iron and no other changes develop diabetes.
I think this point gets ignored in most of this conversation about health. The Maasai may have been drinking blood and having lots of saturated fat, but in fact their diet was super-low in absorbable iron, to the point they were borderline anemic.
http://realhealthtalk.com/regulating_iron.html
We’re working hard on regulating the amount of fats and sugars … but who is looking into iron levels? Right now half the world is anemic, and the other half is iron-overdosed.
So maybe the modern increase in the incidence of hemochromatosis is real and caused by our overprocessed food supply, rather than an artifact of better diagnostic tools? Anemia used to be the common problem — I remember my late Mother (born 1913) telling how rural folks used to treat her and other relatives’ anemia with apples or other fruit that had an old iron nail inserted so the fruit’s acidity could transfer the iron into the fruit.
Yes, it’s pretty hard even to pin down what is “iron overdose”. It used to be believed that no one would overload on iron, because the gut has an intricate mechanism to prevent iron from going directly into the blood until needed. Some people with a weird gene though, circumvented that.
However, ANYONE can absorb too much iron if it’s the wrong type. Iron overdose is common when, say, a kid eats iron pills. Or someone makes beer in an iron pot … this is common in Africa and causes iron poisoning. I kind of think that the sailors in the old days ate a LOT of iron, between the iron pots, iron utensils, the molasses rum and beer, and salt beef … which may be why they got scurvy so easily. On the Lewis and Clark expedition, they aimed for 9 lbs of meat per day per person, and also cooked in iron pots. “Bleeding” was, according to Lewis, just exceedingly effective to cure a lot of ailments, and he was really very observant and a good doctor. But probably all of them were also iron overdosed.
But no one really knows how much iron a person SHOULD have. Diabetes increases as soon as ferritin goes over something like 116. But less than 300 is considered “normal”. A lot of iron gets sequestered in the liver, spleen, heart or brain, and that can’t be measured without an MRI.
I think anemia was a real issue when people routinely had hookworm, roundworm, and tapeworm. Almost everyone did back when. Also some people have internal bleeding. Or a super-low-iron diet. The backwoods folks in the South mostly had hookworm until “shoes” became common (and worm medications).
There can also be other issues. If you have a chronic infection, for example, your body can decide to “hide” the iron and make you anemic. I think this happened to my Mom. She IS anemic and her blood levels of iron are low. But her skin is grey … she sequesters the iron by depositing it on her skin, which then gives her skin cancers. She takes iron pills AND eats a lot of meat AND eats iron-enriched foods. Yet she is “anemic”.
The reason your body hides the iron is that it feeds the worst kinds of microbes. Lately it’s been found that lowering iron levels is a great way to kill staph. Actually that IS how many antibiotics work. They are basically iron-chelators and thus starve the bacteria.
9 pounds of meat a day? Geez. I know folks that run 100-milers and that would last them a good 2 weeks even on a hearty 10-ounce steak a day. I remember reading some time back that depriving harmful microbes of iron would kill them, but, still, even into my 20s, TV commercials were full of warnings about “iron-poor blood” and we were exhorted to eat more liver and take a spoonful of iron tonic every day. Strange how the body handles an element that’s essential to health but can be easily overdosed. My brother developed hemochromatosis at an early age and routine bleeding was one of his treatments. Maybe those old-time barber-surgeons were on to something with their leeches and lancets.
Yeah, I’m not sure what to make of the 9lbs of meat either. Granted they worked hard … but so do a lot of guys these days too. The only thing I can think is that either it was digested differently, used differently, or they had a high parasite load.
Lewis was a careful researcher though and apparently a good doctor. He got 40-odd guys and one gal and baby through the wilderness for 2 years, with only one death (from appendicitis!). He made a lot of notes about edible foods and what the Indians ate, because his mandate was to find if the land was habitable by Europeans. His mother was an herbalist and he was also trained in the doctoring of the day.
So his thoughts about all that meat … was likely just pretty “normal” for the day. They didn’t generally have all that much starch. It was easier to hunt buffalo than to find ground tubers (they did trade with the Indians for starches). So likely their bodies were good at turning protein into sugar as needed, but maybe the process isn’t all that efficient.
It would be interesting to compare their diet with say, the Chinese railroad workers (who I imagine were also pretty well documented). The Europeans, I’ve heard, got huge rations of beef, along with potatoes. The Chinese:
“The workers insisted on eating Chinese food: rice, dried vegetables, dried oysters, dried abalone fish, and some pork and poultry. Much of these foodstuffs came from California sources, such as fresh vegetables. They also drank tea and hot water with occasional wine and opium. The Irish or white workers were fed mainly meat and potatoes along with whiskey. The Chinese diet and especially the use of boiled water reduced the outbreak of dysentery and other diseases.”
http://web.stanford.edu/group/chineserailroad/cgi-bin/wordpress/faqs/
So these are two groups of very hard workers. One eating mainly rice and seafood and tea, another eating beef and potatoes and whisky. However, they had other habits that make it hard to gauge the diet: the Chinese boiled their water before drinking it (as tea), and also apparently were big on taking baths.
BTW in the Asian stores I’ve also noticed the large amounts of dried foods. I’m guessing this is going away as more people have freezers, but there are just huge quantities of dried stuff. Lewis and Clark brought a little “storable” food but it was a newer thing. (L&C salted their meat, and didn’t store vegies much that I could see). The Chinese had it down to an art. Dried food is easy to transport and stores for a long time. Most of the Asian food though is based on rice and vegies, and seafood. The pork and chicken is more of an additive, and very little beef. (Which of course depends on WHERE in Asia we are talking about).
Anyway, both groups of workers apparently did a good job at laying track. Probably there are pictures to compare the two groups physical appearance.
BTW, as to iron overdose … there is an interesting case of the Orkney sheep. These are sheep that happened to eat mainly seaweed for about a hundred years, because that’s where they grazed. Anyway, they adapted. The seaweed chelates copper, turns out. So the sheep now hoard copper. If grazed *without* seaweed, they tend to die from copper overload.
I kind of think something like that happened with at least some genotypes of humans. With sheep it only took 120 years or so. There are a number of foods that block iron absorption … notably dairy, tea, chili, whole grains, and yes, seaweed. So it would make sense to me that some people developed the knack for hoarding the mineral, which was rather rare in some diets.
Anyway, humans seem to vary more when it comes to handling iron than does say, a mountain goat or a gorilla. But our diets vary more too.
@zach I wouldn’t be typing this if it wasn’t for someone eating a diet of apples and carrot juice. Carbs, particularly grains, have fuelled human progress. I believe this is due in large part to their portability, which is a problem with fresh foods like oysters, peaches and bananas. But that’s not where I was going with the Hitler comparison…it has a little bit to do with what you call genius…
Going to extreme carb dieting appears to produce frenetic activity in some people, both physical and cerebral. In the case of durianrider this has not produced much more than a lot of ranting (I think of Hitler especially here, https://www.youtube.com/watch?v=y2fl-sHUwrc ) and bike tire spinning. Entertaining or irritating depending on how you look at him, but harmless. He hasn’t risen to any great achievement – no iPhones or VW’s – but neither has he come up with V2’s, death camps, amphetamines or blitzkreig.
As for high meat intake, there is supposedly a limit to how much heme you can absorb in one meal:
This kind of makes sense. However, there is the well known meat effect in iron absorption, where eating meat significantly increases your absorption of non-heme iron. When you cook meat, it’s possible to transform ~20% of the heme into non-heme iron. So, you absorb ~2mg of heme and then you absorb more of the cooked non-heme. Taken all together, you would absorb more iron from cooked meat than raw meat. And if you ate the cooked meat with non-heme foods, you’d absorb even more iron on top of what you get from the heme and non-heme in the meat. The point being that a meal of pure raw meat and blood might limit the amount of iron you absorb compared to a Western meal.
That might explain why carnivorous cultures always preferred raw meat. Obviously animals too.
Colon cancer is associated with heme iron, but there is some recent evidence that it may have something to do with pathogens consuming heme iron and causing issues.
Where it gets interesting is that cooking meat destroys the porphyrin ring around heme iron and as it turns out, porphyrins are antimicrobials. So, this implies that eating raw meat perhaps makes the heme iron unavailable to pathogens.
Antimicrobial properties of porphyrins (2001)
So, this might explain why carnivorous cultures preferred raw meat. Incidentally, the Inuit had anemia with their high (raw) meat intake, but they also had infections and vitamin deficiencies that affect iron absorption.
wbryanh said: “About pufa I agree they contribute to the problem. In particular omega 6, and all rancified pufa. We should stop consuming veggie/seed/legume oils”
It’s possible that linoleic acid is likely only bad for you if you consume it in isolation. If you eat linoleic acid in whole foods, it’s a totally different ballgame.
For instance, the !Kung eat significant quantities of Mongongo nuts, which are really high in linoleic acid. If linoleic acid in whole foods were deleterious, we should see it in the !Kung. However, mongongo nuts are extremely rich in Vitamin E (565mg per 100g of Mongongo nuts). All that Vitamin E in the Mongongo nut is protective against the damage from linoleic acid:
Protective effect of vitamin E on linoleic acid hydroperoxide-induced injury to human endothelial cells (1991)
It seems like perfect luck, but in reality the nut makes all that Vitamin E so that its own linoleic acid won’t go rancid in the Kalahari heat. So, the protective nature of the whole food is for the benefit of the plant/seed/nut/animal, and whatever consumes that whole food just happens to take advantage of that homeostasis. You are what you eat.
It’s such a simple concept, but few ever really stop to think about it this way. Whole foods have self-protective mechanisms in place that consumers of those foods get to take advantage of when they eat whole foods.
As best as I can tell, the idea that we need to eat more Omega-3 and less Omega-6 (i.e. the fish oil craze) comes from Bang & Dyerberg’s erroneous and now debunked observations that the Inuit were free of heart disease.
The Fishy Origins of the Fish Oil Craze
And this is even further problematic because even if the Inuit really were quite healthy eating lots of Omega-3, it’s believed that they have very different fat metabolisms than we do. In addition to the CPT1a genes, it was also recently discovered that the Inuit evolved unique genetic adaptations for metabolizing omega-3s and other fatty acids.
So, the conventional wisdom on Omega-3:6 ratios may not be all it’s cracked up to be when we look at them in the context of whole foods.
Duck, I find *lots* of issues with your post. E.g. your claim that Bang and Dyerberg’s work is debunked–far from it. Also, we can draw zero diet conclusions from the Inuit gene-variant studies. More on these in another post. But these don’t take away from your excellent main point:
“Whole foods have self-protective mechanisms in place that consumers of those foods get to take advantage of when they eat whole foods.”
As much as we learned about nutrition in the last 100 years, we’re still scratching the surface on our bods respond to the complex matrix we get with whole food. Makes me think about the complex interactions between microbes in our gut flora. We’re fast learning who those little players are, but we don’t yet know much about how they play off each other to contribute to our health. Some feel an optimal gut flora balance is very important for optimal sugar metabolism due to proper insulin signaling among other hormone-driven comms.
Another example of Mother Nature’s exquisitely honed Grand Plan: The usefulness of Omega 6 (w6) for fattening up for the winter. Nuts, esp in temperate zones, usually have a lot of w6 which contribute to temporarily stiffening our cell membranes, making them slightly less permeable than usual, raising general resistance including insulin resistance, leading to more blood glucose being stored as fat. This way we lay in more fat coming into winter, giving us a little extra insurance during a season when it can be harder to find food. *In general* the closer you move to the equator, the lower the pufa in nuts. Mongongo nuts are an exception, they are quite high in w6 for being in a subtropical climate. Thus high in protective Vitamin E as you pointed out. It doesn’t appear to be uniformly healthy for the !Kung San either. During peaks in the mongongo seasons, San postprandial BGs soar in the 160s. Guyenet hypothesizes this high p-p BG is due to lack of acclimatization when moving from seasonal low carb to (relatively) high carb diets (more mongongo fruit). But because the researchers did not follow up later in that high-carb season, we don’t know if the San metabolism adjusts or not. High w6 remains a possible driver for the Sans’ high p-p BGs. Here’s Guyenet’s post:
http://wholehealthsource.blogspot.com/2010/11/glucose-tolerance-in-non-industrial.html
And Duck, do you have free link to specific nutrient content of mongongo nuts and fruits? E.g. where you got the “565mg Vit E per 100g” factoid? The link you posted is behind a paywall. Thanks –Bryan
Here is one nutritional report on mongongo nut –
http://www.naturalhub.com/natural_food_guide_nuts_uncommon_ricinodendron_rautanenii.htm
Thank you Rebecca! I’d like to try these nuts btw.
Duck, on to Bang and Dyerberg’s debunking debunking. You say this: “…Bang & Dyerberg’s erroneous and now debunked observations that the Inuit were free of heart disease…” First the “evidence” you cite is another of the many awful confused science-tripe pieces, topped by click-baity but wrong titles, we too often see in the Webloids which alas includes Slate. Second, in the end, author Elizabeth Preston, even relying on her weak dissenting evidence, doesn’t even claim the B&D results to be necessarily wrong! More research needed!
E.g.: “…Bang and Dyerberg were nutritionists, not cardiologists; they didn’t examine anyone’s heart themselves…” First, B&D weren’t cardiologists. So what? That, in itself, doesn’t invalidate their work. They drew the Inuit blood and brought it back to Denmark for analysis by the appropriate experts. And as filled with flaws lipid panels are, certain analyses of them linking serum lipids to heart disease, such as the Total Cholesterol/HDL ratio, are generally considered reliable:
http://www.mayoclinic.org/diseases-conditions/high-blood-cholesterol/expert-answers/cholesterol-ratio/faq-20058006
Also bear in mind the Inuit that B&D studied ate a mostly or completely an ancestral diet. There was only ONE other comparable study the author cites: “…a report published by a Danish doctor in 1940 also described high rates of heart disease in the Greenland Inuit…” That’s it? What are the details on that report? How clinical was it? Did *this* doctor look directly into the hearts of the Inuit? remember serum tests were much cruder then. The other report she referred to have modern Western diet confounders.
Then there’s this garbage: “…What matters most to a disease researcher, Fodor says, is overall mortality: “the number of corpses you count.” A study found that from the late 1960s to early 1980s, Inuit died from all causes at twice the rate of Danes—hardly a lifestyle to aspire to…” Well no kidding! Life was rough up there in the “unforgiving” land as the author earlier noted. From which main causes did these Inuit die from? Infectious diseases. Accidents? Why didn’t the author give us the breakouts?
Duck, as flimsy as this reporting is, the author does include this disclaimer: “ [Researcher JoAnn] Manson believes that answer [linking w3 and heart disease] could easily go either way. “The vast majority of researchers who really know this field believe the jury’s still out,” she says. IOW Duck, again, we simply don’t *know* that Bang and Dyerberg arrived at the wrong conclusions.
About the fish caps. The reporting can lead us to assume that fish oil caps are, nutritionally speaking, an exact replacement for fresh fish. That is ridiculous. Omega 3 oil rancidifies exceptionally quickly, starting the moment the marine creature dies. It’s already well along in oxidizing by the time you can detect it with your nose–especially when it stuffed in a gelcap that you swallow which previously sat for up to weeks on a shelf at ambient temps. Also, most people take WAY too much w3. Both the main polyunsats–w6 and w3–are very prone to rancidification, w6 somewhat less so. Instead of ramping up our w3 to near pharmacological levels with the caps, we instead should LOWER our w6 to keep a reasonable w6/w3 ratio meanwhile minimizing our total poly fat intake.
So what’s a good w6/w3 balance? The ancestral-living Inuit had the lowest ratio, ~0.7. More common ancestral ratios run 1:1 to 6:1. The !Kung San chowing on their w6-rich mongongos may run near the high end of that. Meanwhile, in the SAD, replete with veggie and legume oils, the ratios can run 40:1 to 60:1! Duck, bear in mind the higher the ratio, the stiffer the cell membranes, setting the stage for metabolic syndrome and chronic disease. Above a certain ratio, yes the w6/w3 certainly CAN matter.
Duck in your concluding sentence: “…the conventional wisdom on Omega-3:6 ratios may not be all it’s cracked up to be when we look at them in the context of whole foods…” You are right! Because, sticking just to whole foods, it’s almost certain you’ll never go up into a harmful w6/w3 ratio.
Duck, about the Inuit gene variant discovery, this work is very interesting but concludes nothing about diet and health. I went through this with Charles Grashow elsewhere on this forum. Search on this string:
the genetic basis of human adaptation to cold climates and lipid-rich diets REMAINS LIMITED
to see my answer to him.
I saw the flurry of articles a few months back, but none explain exactly *how* the Inuit are supposed to better utilize PUFAs than the rest of us. That NYT Zimmer link you posted comes closest:
“The researchers found several genetic variants at different locations in the genome that were unusually common in the Inuit… several …occurred within a cluster of genes that direct construction of enzymes called fatty acid desaturases [FADS]…”
Trouble is Duck, even here, the only logical FAD adaptation here can be for the Inuit to *down-regulate* fatty acid desaturation. This because after all they’re getting all their long-chain (EPA, DHA) w3s from all that blubber they chow. IOW, the Inuit don’t have to *make* as much long-chain w3. This doesn’t at all disprove the fact we all, Inuit and the rest of us, need EPA and DHA and their health bennies, and that you benefit from getting it from diet. We generally aren’t very efficient at making EPA and DHA from the parent 18C w3, namely alpha-linolenic acid (ALA).
Finally Zimmer includes but then you get this caveat: “…natural selection might not have favored the FADS variant but a neighboring, as yet unknown piece of DNA that conferred evolutionary advantages…”
I thought that the Inuit had traditionally minimal- (or even non-existent) heart disease; but in more recent years, they’ve been adding Western foods to their diet, so they now have more health problems (and death) than ever before (?) The problem is that the link about the Inuit and heart disease takes place too late in time, after they were exposed to Western food. Often when a Native culture goes suddenly from their old diet to eating more modern foods- even if only a few of those foods are introduced- they have even more health problems than the rest of the population. So I’m not sure if those studies were accurate of much of their existence. It sounded like a bit of speculation anyway- (i.e., “they probably had heart disease that was not diagnosed, or overlooked”). That doesn’t really prove anything, in my mind, about the Inuit.
My personal theory is that people are so convinced about the diet/heart hypothesis (i.e. that saturated fat causes high cholesterol, which causes heart disease)- that every time a paradox crops up (and there are many of these!)- they have to find something to explain it away. Usually, they find some mechanism that is supposedly “protective”. With the French it was red wine, with the Masai it was suspected that they had a genetic mutation (with the Inuit too), with other cultures it was all the anti-oxidants they ate, or the garlic they ate, whatever. So the same with the omega 3 fish oils. Maybe these foods aren’t “magic foods”; instead, maybe the whole hypothesis is wrong?
In any case, I’m not quite sure if I “buy into” the whole omega 6/ omega 3 thing. Oh, I agree with wbryanh that seed oils are not good (I stay away from them myself). Mostly because they are highly processed and turn rancid very quickly (and I’ve read that some of them are correlated with cancer). I’m not sure if it’s the omega 6 part that makes them “bad”; (could be, that’s open to debate).
In any case, I agree, Duck Dodgers, about omega 6 in whole foods as not being a cause for concern. (I had also read before that the vitamin E is protective). In looking at populations of people who eat nuts, they seem to be very healthy, and nuts seem to possibly even be protective against heart disease- (of course correlation doesn’t equal causation, but at least it’s clear that nut eating people don’t seem to be dying off). At least I’d like to believe this of course, because nuts are one of my favorite foods and I eat them often! My guess is that in terms of whole foods, the O-6, O-3- (if it’s a problem at all) is probably self regulating.
“Fishing” for the origins of Fodor’s “Eskimos and heart disease” DEBUNKING story.
Morgana, right on! You wrote: “I thought that the Inuit had traditionally minimal- (or even non-existent) heart disease; but in more recent years, they’ve been adding Western foods to their diet, so they now have more health problems…”
Regarding the “debunking” studies, esp Fodor’s “Fishing” for the origins of the “Eskimos and heart disease story” we may find something rotten. And not in the State of Denmark.
Ironically, the debunkers, and an all too credulous and sensation-hungry media, hang their hats on this “seminal” Fodor study, which you can read here: http://ottawa.ctvnews.ca/polopoly_fs/1.1814937!/httpFile/file.pdf
Is this a case of “the shark calling the herring black?” We’ll see! What I’ve found so far:
Fodor et al provide a list of 60 references. I’ve reviewed to date 35 of those refs. So far Morgana I find an undeniable pattern that is just what you say: Early Inuit and even early non-Inuit native living ancestrally have lower CAD. Later Inuit and non-Inuit natives adopting a more “western” lifestyle have higher rates of CAD.
At first blush, this evidence (to date) seems to contradict the authors’ own conclusions! But let’s be clear what the Fodor report does and does NOT say. The authors do not outright *deny* the ancestral high-fish Inuit diet lowers CAD risk. They conclude simply that “ this hypothesis lacked a solid foundation.”
I will share later my ideas why the authors would present their findings in such a muddy way.
Meanwhile there’s more. In their report I found a decision flowchart that shows the authors narrowed evidence inclusion down to “10 papers related to 10 studies.” Strangely, I can’t find such a list anywhere in their report even though I’ve read it several times. Did Fodor et al accidentally leave out that list out?
In the meantime, I’m trying to come up with that 10-paper list, based on that superset of 60 refs. I’m using the filter that Fodor et al included to winnow down to those 10 papers. Here’s that filter:
– No relevance to Eskimo population
– No direct measurement performed in study population (i.e. metaanalysis, review paper, etc.)
– No assessment of CVD or CAD in study population
– Full article nonaccessible online
Then I read this from the report: Table S1. Evidence regarding low incidence of CAD in Greenland as cited in Bang, Dyerberg et al publications 1971-1980
Morgana, this lists seven papers. At least five of them fulfill the inclusion requirements above. Does this mean then that as many as *half* the the 10 papers Fodor et al use to debunk the Inuit diet-low-CAD hypothesis come from the *very same authors* whose research the integrity of which Fodor calls into question?!
Fascinating!!
Today I emailed the doctor seeking that list of the 10 studies.
Stayed tuned!
wbryanh- yes, keep me posted, I’m curious! But, yes; I have read in many different places, from different sources, that the early Inuit were free from heart disease (and other diseases of civilization). But later on, they had even more problems than most because when native hunter-gatherer type cultures change their diet suddenly, they often become even more sick than the general population because they’re just not well adapted to the modern diet. Many people have unfortunately used their more recent health problems to “debunk” the original observations.
Having said that, I’m still not sure that the “protective factor” is the fish- (it might be, as epidemiological studies show that fish eaters are very healthy)- or the omega 3/ omega 6 ratio- (it could be, but I’m not sure there’s enough credible scientific evidence proving that it’s important)- or, and this is my own theory, that maybe the diet-heart hypothesis is wrong, and high (natural) fat diets do not cause heart disease? There seems to be a lot of evidence that refined sugar may be implicated in heart disease. Apparently, this was documented and known about even back in the 70’s, but it’s been covered up….. just like the tobacco industry covered up knowledge about tobacco!
Morgana, good timing on your response. Just had a lovely 30 minute talk with one of the leads on that study. She couldn’t remember the 10 papers off the top of her head, nor where they are supposed to be listed in the report. She said she’ll reread he report tonight/over the weekend and get back to me. I hope I’ll hear back from Dr Fodor too. He’s retired from Ottawa Heart but Media Relations forwarded my enquiry to the doctor and promised “a very quick response.”
Hi Morgana! Study second-lead Efythia Helis sent me the list of the 10 papers that she and Fodor et al used in “Fishing” for the origins of the “Eskimos and heart disease story.”
This confirms the Fodor meta-study offers nothing conclusive about CAD/CVD in Inuit eating ancestral foodways. The vaunted 1940 Bertelsen paper, though the authors discuss it at length in their Intro, actually *failed* to make their final cut. Very interesting!
To refresh your memory, Duck posted a Slate link on Nov 24th as evidence to debunk observations that the Inuit were free of heart disease. Here are the two links to that Slate article and the Fodor study:
http://www.slate.com/articles/health_and_science/medical_examiner/2014/08/does_fish_oil_prevent_heart_disease_original_danish_eskimo_diet_study_was.html
Click to access file.pdf
Dr Fodor’s retired to Europe and no longer answering Qs on this meta-study. But the study second-lead Efythia Helis emailed me this morning. From her mail:
“…the 10 studies we identified are listed in supplemental tables S3 and S4. Table S3 presents information regarding the only study we identified that used direct measurements on the Eskimo population (Reference # 28). Table S4 lists information from 9 studies that presented data on CVD status in Eskimo/Inuit populations in Canada and the US (references 22,23,29, 30,31,32, 33, 34, 35). In total, 10 studies, listed in two separate tables, which clearly can be confusing. We split them like this, since it was only the study by Jorgensen et al (#28) that used direct measurements on the actual study population…”
Morgana, note they include exactly *one* paper that directly measured the Inuit for CAD/CVD, and it’s from 2008! Even Jorgensen et al admit: “The prevalence of markers of CHD was not different from that in Western populations. The Inuit is a population undergoing rapid social and health transitions, with the emergence of cardiovascular risk factors, and there is a need for critical rethinking of cardiovascular epidemiology in this population.”
Note the authors do *not* include that 1940 Bertelsen paper in their final cut. They discussed it at length in the Intro, yet the evidence in that Bertelsen paper somehow didn’t rise to the level of evidence to make the cut. Very interesting!
You can see those 10 refs starting on page 16 at the CTV link.
I’ll finish reviewing the refs and then post my ideas on why these study leads chose to represent this info and highlight certain aspects–like finding flaws in a 1970s Bang and Dyerberg–in the curious way that they did. –Bryan
Very interesting! Thanks for the update.
My conclusion soon Morgana. Stayed tuned… –Bryan
I have no clue why the Inuit have any relevance in regards to anyone’s diet, regardless whether they were healthy or not.
For one, no one could or would replicate a traditional inuit diet of seal blubber, polar bear organs and fermented fish. Swapping them out for ground beef and a ton of fat is not even in the same ballpark.
Also they did not just decide to eat that way because of health reasons. That was a several thousand year adaptation to extreme living conditions. Even if the average low carb enthusiast could replicate an Inuit diet, their physiology is so different that they would probably get real sick real fast.
Bottom line, even if they were a healthy culture, which is not proven, that means nothing because the diet and lifestyle cannot be replicated so it has no relevance on a traditional VLC diet. If they were unhealthy eating their traditional diet than that proves very bad for anyone eating a watered down version.
Morgana, Fodor et al’s “Eskimos and heart disease story” feels more than ever like Fodor’s retirement gift to Big Pharma. No doubt Pfizer, Merck, Astra-Zeneca, and other statin producers love them a tasty dish that casts doubt on the CVD health bennies of a high-fish diet. The less healthy our diet, the more money we fork over for their drugs. In turn, Big Pharma spreads a bit of the wealth to many academic researchers, including Fodor during his active work life.
Four author/researchers worked on this study. But I’ll refer just to Fodor. He shaped and had the final word on the study direction and contents: http://ottawa.ctvnews.ca/polopoly_fs/1.1814937!/httpFile/file.pdf
Fodor’s stated goal: to determine if there was enough evidence to support the “Eskimo diet and low CVD” hypothesis. In the Intro, Fodor sought to debunk studies Bang and Dyerberg did in the 1970s, studies viewed as seminal to show fish-eating Inuit have lower CVD. Fair enough–those studies do appear to have methodological flaws. And who doesn’t love a juicy debunking story? Especially a largely unquestioning and headline-hungry press?
The sad thing is, Fodor fails to discuss a very valuable pattern his sources studies reveal: a whole-foods diet high in actual high omega-3 food may actually lower CVD significantly. In the 10 studies Fodor uses, the trend is abundantly clear: The further back in time you go, the less CVD the fish-eating Inuit had. Why didn’t Fodor call this out? Maybe because it didn’t suit Pfizer et al?
In the Intro, Fodor muddies the waters, jumping between fish and fish oil caps. He conflates the two, implying an equivalency even though by publish date (2014) we had plenty of evidence to suggest fish oil caps may not offer the same therapeutic benefits as eating actual fresh fish. Fodor utterly fails to discuss these diffs. He very easily could have. In his list of 60 total refs, if you look at the 50 studies that failed to make the cut, you find many of them for cohorts taking fish oil caps. Overwhelmingly, these suggest that the caps had little or no impact on CVD over the non-cap taking controls/cohorts. Why did Fodor ignore that glaringly obvious pattern?
Further down the Intro, Fodor says this: “More recently, a number of studies have confirmed what Bertelsen ascertained more than 70 years ago, i.e. that the prevalence of CAD among Eskimos in Greenland and other Inuit populations in Canada and the US is similar or higher compared to that of non-Eskimo/Caucasian populations.” This statement may be outright wrong. Bang & Dyerberg wrote in 1980: “…Berthelsen (1940), does not even mention [CAD]…” http://link.springer.com/chapter/10.1007%2F978-1-4757-4448-4_1#page-1
If true, how could Bertelsen have “ascertained” that those Inuit had western-level CVD rates?
Fodor concludes: “We conducted a literature review to assess whether there was sufficient evidence to support the ‘Eskimo diet and low CAD” hypothesis. Our conclusion is that this hypothesis lacked a solid foundation.” Problem is, Fodor doesn’t distinguish between earlier ancestral and more recent Inuit diets that are heavily influenced by western foods. He lumps them together under the vague rubric “Eskimo diet.” We have no direct measures of Inuit CVD before Bang and Dyerberg, whose work Fodor sought to discredit and conveniently drop from the pool of papers he considered for this study. Thus we have *no* studies that give direct measures for Inuit eating a predominantly ancestral diet. That leaves only direct measures of *modern* Inuit who follow an increasingly western diet and lifestyle (e.g. drinking, smoking).
We’d be naive to think that Fodor’s many links to Pharma couldn’t influence his research design in subtle, even overt ways. He was Founding President of the Canadian Hypertension Society which gets heavy Big Pharma sponsorship, esp Merck. https://www.hypertension.ca/en/chc. Fodor received honoraria from AstraZeneca, Merck Frosst, Pfizer and Schering for conferences and advisory boards. http://www.totalbodyhs.net/2011/11/08/conflicts-of-interest/ On his CV, he lists major research that’s funded by Big Pharma, e.g. the 2001-2002 AVALON study funded by Pfizer. Should we be surprised then that Fodor came out ardently in favor of Big Pharma’s products? E.g. he says in 2007: “The efficacy and safety of [statins] is outstanding…” http://www.curezone.org/forums/am.asp?i=822300 even though we’d already started to see efficacy and safety concerns emerge about statins since the 1990s. http://www.ncbi.nlm.nih.gov/pmc/articles/PMC2849981 .
Fodor published the “Eskimos and heart disease story” study not long before he retired to Europe. I reached out to the retired Dr Fodor and failed. The Institute’s media contact Vincent Lamontagne said he forwarded my questions to Fodor, assuring me “Dr Fodor very quickly responds to questions.” When I heard nothing for 10 days and followed up, Lamontagne then informed me the Doctor would not take questions after all, leaving the unenviable task to the junior leads.
Sadly, Fodor’s close ties to large corps is an ever more common pattern we see among academic researchers. In this era of dwindling government and foundation funding, research institutions had to start turning more to Big Biz for funds. http://www.universitybusiness.com/article/big-business-research As Dr. Edwin Gale says: “Money from drug companies is the oxygen on which the academic medical world depends.” http://www.medscape.com/viewarticle/751433 We shoud all be aware of this very troubling dynamic when we review any health and medical research.
My thanks to junior lead Efythia Helis for fielding my questions. –Bryan
wbryanh- Wow, thanks for that long and detailed analysis! That doesn’t surprise me that they’ve been looking at Inuit eating a more modern diet; I had suspected that. I did not know about the ties to the drug companies though. I have also read in a few places- (I think in books, and I can’t remember where, so I can’t send a link unfortunately)- that in epidemiological studies it’s been found that eating whole fish is more effective than fish oil (like you said). It’s suspected that there is a synergistic effect of all the nutrients together in whole fish, which is different from just extracting and isolating the oil. Some have even gone so far as to say that it may not be the omega 3 after all that causes the protective effect, but possibly some other compound that we don’t know about yet. In any case, the Mediterraneans and the Japanese eat quite a lot of fish too, which might partly explain their low risk of heart disease.
You’re welcome Morgana! I’ve been trying to find the actual 1940 Bertelsen text on Greenland Inuit CVD, I’ve heard such wildly divergent things, from “western-levels of CVD” to “no mentions of CVD.” Morgana, *someone(s) is/are *bullsh*tting us! But who? I’m trying to find the source text to settle the matter once and for all. I emailed Fodor study junior lead Eftyhia Helis about it. She responded with this: “This 1940 report is with Dr. Fodor’s files, which, unfortunately, I have no access to at the moment…I do not think there is a translated version of this…” Next stop–my local library to try to get that volume of “Gronlandsk medicinsk statistik og nosografi.” When I finally find it, I’ll OCR it and run it through Google Translate and see what we get. If it’s short enough, I’ll plop it up here for all of us. –Bryan
Morgana, about the “Eskimos and Heart Disease” study, one of the junior leads, Effy (Eftyhia Helis), is super nice and helpful. So I invited her to join in here and address whichever points she felt like addressing. That’d be great if she could join in. –Bryan
Dr Otto Schaefer’s 1959 observations http://www.ncbi.nlm.nih.gov/pmc/articles/PMC1831365/pdf/canmedaj00812-0101.pdf might be of interest …
Jonathan Christie- I had a read, thanks, that was interesting!
Jonathan, that article is excellent, thank you! One of the best pieces I’ve read to describe researcher direct observations on the unusually robust health of ancestrally-living Inuit. Anna, please note at the top of page 386, the discussion on Vitamin C, how these Inuit consumed almost *no* Vitamin C and yet showed no signs of scurvy or other connective-tissue pathologies. Schaefer also reminds us that even in 1959, folks challenged Ancel Keys’ ideas on dietary lipids (page 387). –Bryan
Bryan,
interesting about inuit and vit C. I can’t remember now where I’ve seen that, but people who eat more carbs also require more vit C intake. May be it’s because “Glucose Modulates Vitamin C Transport ”
http://jn.nutrition.org/content/130/1/63/F7.expansion.html
or this “Hyperglycemia inhibits the uptake of dehydroascorbate in tubular epithelial cell”
http://www.ncbi.nlm.nih.gov/pubmed/16118484
Anna, yes I was going to write to you about that! That’s another great example of nature’s uber-intelligent plan: Animal-sourced food is very low in both carbs and Vitamin C. So whatever the ancestral dietary “playing field” the competitors are fairly well matched matched.
I came across that ~5yo when I first came across the Inuit paradox. Our C RDA is 90mg/day but going on memory, seems like Inuit do fine on ~ 15mg/day, which they get mainly from, I think, muktuk. That blubber is one of the few animal-sourced foods I’ve heard of to have measurable amounts of C. C and glucose are very similar molecules, indeed and I think plants and many (most?) animals make C from glucose. https://en.wikipedia.org/wiki/Vitamin_C . I believe it’s a four-step process, and we lost the ability to do that last step not so many millions of years ago. Anyway, C and glucose complete for the same GLUT1 transmembrane transporters. https://en.wikipedia.org/wiki/GLUT1. Anyway, again going on memory, all cxns welcome.
Anna, on a totally diff topic for a moment, was the Indian side of your fam part of the migration to Astrakhan in the 17th cen? I find it a very interesting bit of Russian history few people hear about. Thanks for indulging my curiosity. –Bryan
Not about carbs, but another thought is that the need for Vit C varies depending on the need for anti-inflammatories.
Most of the information about scurvy was obtained on sailing ships in the last few centuries. The sailors at the time lived mostly off salted meat, dark rum, and hardtack. Their cooking pots were mainly cast iron. What you have there is a diet super-high in oxidants and inflammatory factors. Further, the sailors typically lounged around half-clothed in the sun.
So the body uses Vitamin C to handle all of the above. A lot of Vit C is used just to handle UV rays on the skin. Vitamin C also reacts with the iron (from iron pots, dark rum, and salt beef). And for some percentage of people at least, wheat is also inflammatory.
According to Adv in carbohydrate Chem & biochem page 141, whales are mainly neu5ac, which if true would make them less inflammatory than beef. Fish are mainly neu5ac too.
Anyway, your average Inuit wasn’t running around half-clothed or eating beef or swigging rum or cooking in iron pots. So quite possibly their need for Vit C was a lot less.
Heather,
Great point about vitamin C and UV. Thanks.
Duck and Bryan,
Thank you guys for your patience and dedication in debating the inuits and ketosis, it was very informative. And thank you to everybody else who contributed to the Inuit discussion. I’ve learned a lot.
Anna thank you and thanks for your questions too. I learned a lot from everybody! Fair to say, a huge amount. I don’t know if this means you’re leaving us now, but if you are then I hope Anna do skorogo! –Bryan
“Anna, on a totally diff topic for a moment, was the Indian side of your fam part of the migration to Astrakhan in the 17th cen? I find it a very interesting bit of Russian history few people hear about. Thanks for indulging my curiosity. –Bryan”
Bryan, the indian side is not blood related, but via marriage very recently.
Ah, Anna, congratulations! –Bryan
Now who’s telling the truth? The truth about the findings of Dr. Bert(h)elsen? The only person before Bang & Dyerberg to extensively observe Greenland Inuit who still lived and ate ancestrally?
This matters because many Inuit diet debunkers love to cite this Danish study. A study few of them actually *read* because there doesn’t appear to be an English translation. So who knows where they got their citations from? One such debunker is vegan diet promoter John McDougall, who grandiloquently calls Dr. Bertelsen “…the father of Greenland epidemiology.”
https://www.drmcdougall.com/misc/2014nl/feb/grassfed.htm
Duck you said: “…As best as I can tell, the idea that we need to eat more Omega-3 and less Omega-6 (i.e. the fish oil craze) comes from Bang & Dyerberg’s erroneous and now debunked observations that the Inuit were free of heart disease. [Debunked by this Fodor study] The Fishy Origins of the Fish Oil Craze…”
Should we believe Dr Fodor, the lead on the “seminal” meta-study of meta-studies “debunking” the CW of low IHD in the Inuit? Or should we believe Bang & Dyerberg?
In his report Fodor says: “…Bertelsen … described *frequent occurrence of CAD in this Inuit population*…” http://ottawa.ctvnews.ca/polopoly_fs/1.1814937!/httpFile/file.pdf
By contrast, Bang & Dyerberg wrote this in 1980: “…Berthelsen (1940), does not even mention [IHD]…” http://link.springer.com/chapter/10.1007%2F978-1-4757-4448-4_1#page-1
Please note per the Wiki, CAD = IHD. https://en.wikipedia.org/wiki/Coronary_artery_disease
wbryanh,
The point is that Bang & Dyerberg screwed up, and their errors are what started the fist oil craze:
Fish oil and the ‘Eskimo diet’: another medical myth debunked
Here is the actual study that finds the problems with Bang & Dyerberg’s research:
“Fishing” for the Origins of the “Eskimos and Heart Disease” Story: Facts or Wishful Thinking?
Sure, you can explain all this away, but lots of people fell for Bang & Dyerberg inaccuracies. At least admit that they made some big mistakes. The rest may in fact be “wishful thinking”.
Sorry, Duck. Again, you give -nada-.
If you read carefully, I never said B&D was right. What I am saying:
**you haven’t shown anything that firmly concludes anything different from what B&D concluded**
In that Minnpost link you gave, author Susan Perry gives these studies to support her case. So far, all FAILS.
http://www.ncbi.nlm.nih.gov/pubmed/22968891. Study done with supps only. Not the real marine life that real Inuit eat. Huge diffs. As I explained earlier.
http://onlinelibrary.wiley.com/doi/10.1002/14651858.CD003177.pub2/abstract. Meta-study from data collected in 2002. Quite possibly most if not nearly all their data comes from Inuit eating SAD. Stuck behind paywall. No details on that data.
http://www.sciencedirect.com/science/article/pii/S0828282X14002372. Again, meta-study stuck behind paywall. Used data “…which accumulated on this topic during the past 40 years.” You can be sure most if not nearly all their data comes from Inuit eating SAD. In any event, stuck behind paywall. No details on that data.
Duck, you say “…at least admit that [B&D] made some big mistakes…” I don’t know, Duck. Did they? Do you know? Have you actually read their study? Did they conclude things beyond what their methodology would allow them to determine? Some say they do. They can say whatever they want. I’ve seen so many agenda-driven meta-studies with statistical p-factors hacked to a fare-thee-well that AMAP I go right to the primary sources. In this case, I haven’t read the B&D report–that’s behind a paywall too. Abstract’s here:
“The plasma-lipid pattern, including quantitative lipoprotein electrophoresis, was examined in 130 Eskimos (69 females, 61 males) — hunters and/or fishermen, and their wives — in the northern part of the west coast of Greenland, and consuming a predominantly meat diet rich in polyunsaturated fatty acids. Most types of lipid were decreased, compared with Danish controls and Eskimos living in Denmark. The most remarkable finding was a much lower level of pre-β-lipoprotein and consequently of plasma-triglycerides in Greenlandic Eskimos than in Danish controls. These findings may explain the very low incidence of ischæmic heart-disease and the complete absence of diabetes mellitus in Greenlandic Eskimos.”
BTW, there’s a strong positive correlation between cardiovascular disease (CVD) and diabetes:
http://www.heart.org/HEARTORG/Conditions/Diabetes/WhyDiabetesMatters/Cardiovascular-Disease-Diabetes_UCM_313865_Article.jsp/#.VlUiGHarSUk
with plenty of mechanistic data to support that correlation. B&D report a “complete absence of diabetes mellitus in Greenlandic Eskimos.” Duck you do not need to peer inside the body to learn this. A simple blood test works fine.
Duck, would you start making an effort to provide actual relevant evidence that’s not stuck behind paywalls? This is disappointing and starting to get boring. Thanks for considering.
And your final sentence: “The rest may in fact be “wishful thinking”…”
Duck, maybe that’s your wishful thinking?
“The low mortality in Greenland from IHD and the low presence of arteriosclerosis of the aorta and coronary arteries seem well established…” (4)(8)
Footnote (8) goes to Inuit autopsy studies. Not mere blood work and other indirect measure. This get right to the heart of the matter (harhar).
Click to access 1182.full.pdf
Duck, I’m curious to learn if this wind up in the Fodor meta-study you cited. And how many of those other studies in his meta-study tap into autopsy studies.
This evidence is stronger than just about anything I’ve seen so far.
wbryanh said: “I saw the flurry of articles a few months back, but none explain exactly *how* the Inuit are supposed to better utilize PUFAs than the rest of us”
Well, those new genes were just discovered, but the CPT1a gene was discovered awhile ago and that has been documented a bit better. If you take the time to investigate their CPT1a gene, you’ll find that studies have shown that 68% of Eskimos have an autosomal recessive mutation that results in a “CPT1a deficiency,” which is known to cause hypoketotic hypoglycemia (i.e. low ketones and low blood sugar). They prefer to snack constantly because of this—though it’s mainly only dangerous to children (who were traditionally breastfed carby human milk until ages 4-6).
It’s been awhile since I looked into this, and don’t really care to look into it again—so I’m only pointing you in the right direction. But, if I remember correctly, the FAs can’t (easily) get into mitochondria in cells that have CPT1a (such as the liver), but it sounds like they CAN get into mitochondria in cells that have CPT1b and CPT1c. CPT1b is prevalent in skeletal muscles, heart and brown adipose cells (good for thermogenesis in a cold environment), while CPT1c is mostly in the brain, though little is known about CPT1c. Again, if I remember correctly, this implies that their livers are protected from burning too many FAs as FAs are preferentially shunted to muscles and other organs. Or something like that. It’s been awhile.
Anyhow, the point being is that there is a fair amount of research covering how they burn fatty acids very differently than Westerners do. And therefore, they make a lousy proxy for Western metabolisms who generally do not have their unique genes.
Duck, just checking. This is what you saw, is that right? –Bryan
http://www.adn.com/article/20141129/clues-emerging-about-arctic-gene-diet-and-health
“…studies have shown that 68% of Eskimos have an autosomal recessive mutation that results in a “CPT1a deficiency…”
Duck, this is interesting stuff which I’ll be diving more into. In general, these gene variants–mainly missense mutations?–appear in general to “gate” the ingress of FAs into the cytoplasm–at least for liver cells. Which makes sense for a diet extraordinarily high in extraordinarily oxidizable w3. This presumably spares the sensitive mitochondria from oxidizing events in their midst, minimizing damage. In a sense it’s like insulin gating the ingress of glucose (also oxidizing) to the cytoplasm, with the same goal, to minimize stress on the mitochondria, though obviously by a diff mechanism.
That’s my initial take of it anyway. Will dig into it more later.
I don’t doubt the Inuit experienced several SNP variances over their thousands of years living in their harsh frigid environment and eating their ultra-low carb high w3 diet. But Duck for you to make the leap that “…they make a lousy proxy for Western metabolisms who generally do not have their unique genes” is a stretch at best. You can’t know it is a “lousy proxy.” None of us know it at this point. You may well be vastly overstating, even erroneously, stating the case. E.g., we don’t know how successfully Non-Inuit and Inuit can up/down-reg when placed in the others’ environment. If you know of any systematic examinations of that, please share. It is wrong to imply that Inuit nutrient metabolism as being so fundamentally different that it can’t offer the rest of us any nutrition lessons. Especially when we include the Inuit experience in a larger examination comparing different ancestral diets.
And how do these SNPs even relate to the premise that kicked off this thread? The validity (or lack thereof) of w6/w3 balances?
A few posts back you said: “…the conventional wisdom on Omega-3:6 ratios may not be all it’s cracked up to be when we look at them in the context of whole foods…” That’s when you introduced the Inuit w3 topic by saying this: “As best as I can tell, the idea that we need to eat more Omega-3 and less Omega-6 (i.e. the fish oil craze) comes from Bang & Dyerberg’s erroneous and now debunked observations.”
Duck, the SNP changes I’ve heard about to date doesn’t *distinguish* between the dietary fats. These Inuit SNPs may preferentially deliver ALL fats to non-liver cells–sats/monos/polys. This doesn’t mean ideal w6/w3 balances aren’t similar across differently groups. Westerners may not be seeing the benefits of fish caps for other reasons besides a presumed irrelevancy of the w6/w3 balance. Esp when we consider the near pharmacological amounts of rancid fish oil in the caps, and people still chowing w6-bomb veggie/legume oils, also all too often rancid.
Btw, for the record, per that ADN link it’s “68% of *indigenous people of northern Siberia*…” Not all of Inuit-dom. That matters because the Siberian and NA/Greenland Inuit diverged 15,000 or more years ago.
http://www.adn.com/article/20141129/clues-emerging-about-arctic-gene-diet-and-health
wbryanh,
It wasn’t that hard to find a copy of the Fodor study that calls Bang & Dyerberg into question.
Click to access file.pdf
Bang & Dyerberg based their supposition on casual observations that coronary atherosclerosis in Greenlandic Inuit was ‘almost unknown’ and that they consumed large amounts of omega-3 FAs. Except that it was known, as the Fodor paper shows. So yeah, they made a mistake and what’s problematic about it is that their speculation kickstarted the fish oil craze.
Anyhow, it makes no difference because even if they were healthy at one time, they don’t metabolize fats the way that we do making them a very poor proxy for Western metabolisms. Here’s two studies on CPT1a that I quickly found that wasn’t behind a paywall. But there are many others besides this one, should you take the time to look.
Genetic polymorphisms in carnitine palmitoyltransferase 1A gene are associated with variation in body composition and fasting lipid traits in Yup’ik Eskimos (2011)
Polymorphisms in Genes Involved in Fatty Acid β-Oxidation Interact with Dietary Fat Intakes to Modulate the Plasma TG Response to a Fish Oil Supplementation (2014)
No, they are not like us.
“Duck, just checking. This is what you saw, is that right?”
I’ve seen that article before. It’s a good summary of the research. Basically the gene is only problematic for babies and young children who can have trouble fasting. The CPT1a mutation is believed to be related to their ability to generate significant body heat from their high PUFA diet. And it’s also believed to be related to their known preference for constantly snacking.
“I’m curious to learn if this wind up in the Fodor meta-study you cited”
I don’t have time to pick this apart. See the full text of the Fodor paper here (Free download).
Like all of the other Eskimo researchers, Otto Schaefer says
“The traditional diet of Eskimos contained large amounts of proteins, lesser amounts of fat than generally assumed [29-30] and only small amounts of carbohydrate, mainly in higher complexed form as glycoproteins, and therefore not rapidly absorbable.”
pmid.us/PMC1940978
Why all the fuss when even Schaefer says they weren’t LCHF? We can’t replicate their high protein diet.
Thanks Rachel, I’ve wanted to read this study. Only will you point out for us which page on which we’ll find the quote you gave us? You know, the one that starts with “The traditional diet of Eskimos contained large amounts of proteins…” I searched on it in that link came up empty. Thanks for your help Rachel. –Bryan
Rachel, found it. To make clear, the quote you cite (see below) doesn’t support what you say here:
“…even Schaefer says they weren’t LCHF…”
The Inuit could still be eating mostly fat, as Ho et al say in their Canadian Inuit report from the same year:
“Approximately 50% of the calories were derived from fat and 30 to 35% from protein…”
Here’s that quote you cite, from near the top of the second column on page 737:
Click to access canmedaj01654-0029.pdf
“…The traditional diet of Eskimos contained large amounts of proteins, lesser amounts of fat than generally assumed (29-30) and only small amounts of carbohydrate…”
–Bryan
Conventional wisdom says that hookworms promote anemia. There are a few problems however…
The association makes sense, helminths eat blood, blood contains iron, iron is reduced in blood, therefore helminths promote anemia. However, the helminth load may be determined by the iron available, or the body will withhold iron in tissues to lower iron in the serum in response to helminths. The results may be the same as chronic anemia triggered by bacterial infection.
In other words, it could just be that helminths cause anemia of chronic disease. Apparently it takes heavy infestation to cause significant blood loss, and heavy infestation means damage to the gut and poor nutrient absorption, which means the anemia may be just as likely to be due to micronutrient deficiencies as blood loss.
The US government was sufficiently convinced of a helminth-anemia link that it carried out a huge program to eradicate helminths.
So helminths metabolize the human-sourced iron and also encourage re-absorption of iron in the human gut, so that enough remains to feed them. Makes sense. It appears to be an efficient, low-waste process.
Helminthic anemia impacts women most, especially pregnant women—but again this could be anemia of chronic disease. Even light infection was found to reduce serum iron in pregnant women. Anecdotally, helminths appear to be more of a net benefit, on avg, than a problem, for males. It is indeed complex.
wbryanh: I have a suspicion that “Zach” actually might BE Durian Rider himself! Durian Rider has a habit of lurking around nutrition websites using various pseudonyms. I think this is why he got so emotional when I made a comment about him- (and somewhere else in the comment section, someone posted an Anthony Colpo link about Durian Rider; he got very emotional there too). In any case, both “Zach” and Durian Rider have the same method for promoting their diet: they use Durian Rider’s thinness and “fitness” to claim that it’s the best diet in the world. Durian Rider also likes to make videos where he finds an “opponent”- someone who eats low carb, or maybe just someone who promotes meat eating- and he basically just laughs at that person, saying they are fat. No science, no intelligent conversation, just ad hominem attacks. But doing that on the comment section of a blog over the internet is truly inane, since he has no idea what we look like or how fit we are! If he could see me, he would see how utterly laughable his comments to me were. In any case, I did not answer his last comment about me because I felt that it didn’t warrant an answer- (although what he means by “especially people who hang around fitness blogs”- what he’s trying to imply here (?) it’s totally illogical. This is purely an emotional comment).
Morgana, yes, could be. In the beginning “Zach” seemed a bit more reasonable or at least civil. But seems like now he’s just shrilly issuing empty statements.
Troll!! Probably best not to answer unless you’re hungry for your fair share of abuse …
Jon, I’m not *quite* ready to write Zach off as a contrarian for contrarian’s sake. He does seem to genuinely believe in HCLF. But that’s just it–belief. If he continues to blurt out dumb stuff unencumbered by rigorous science, then yes I will ignore him. If he gets truly insulting, I expect Denise will ban him. That said, I’m very concerned about the pro-HCLF/anti-LCHF message that some people promote. I feel HCLF can be quite dangerous to hundreds of millions of people. Type 2 diabetes is soaring all round the world. I’ve yet to see a HCLF study that even comes *close* to normalizing blood sugars. At the very least, people serious about this need to get glucometers and give the foodways a fair shake and see how they do. For me, it’s LCHF and has been for nearly nine years.
WBryanh, how can you say that? The article outlined several studies/dietary programs that cured diabetes. Right? And then there are many more modern studies and clinical results that have underlined these. I’m not aware of any studies where HFLC has cured diabetes as opposed to manage the condition by avoiding carbs. So the exact opposite of what your saying is what’s published.
Cjarman did you go to those links Denise gave? All I did was cite the results right out of the tables you find there. Any fasting BGs above 125mg/dL indicates diabetes. All the fasting Bgs results I found there are above that. If you find differently, I’ll stand corrected.
http://www.mayoclinic.org/diseases-conditions/diabetes/basics/tests-diagnosis/con-20033091
I read the article a while back. And from memory it suggested that diabetes was being cured with the likes of the rice diet. Neil Barnard, McDougall, Furhman and Esselstyn all make similar claims.
For example
http://care.diabetesjournals.org/content/29/8/1777.abstract
Are you aware of studies claimed HFLC can achieve the same?
Cjarman, as far as “curing” Type 2 diabetes, not only do I see no “cure,” in the main I don’t even see full reversals. It’s there. Take a look.
Cjarman, dunno how much clearer I can be. Regardless of “who” is claiming “what,” the numbers in those charts that Denise posted say “diabetes!” The limits are in that Mayo Clinic link I posted for you. My own n = 1 tells a similar tale. Before LCHF, my Hemo A1c was 7.0% which equates to an average BG of 170. After starting LCHF, my A1c and quickly dropped, both to 90. It’s nine years later, I’m 55, and my A1c/FBG are *still* 90. That’s a whole lot better that the typical post-study results in any of the studies Denise cites here. I lost 60 pounds, I feel great, I have tons of energy, I sleep better, I *think* better. The so-called “scientific” studies and say and conclude all the things they want. I know what works for me. Like I said above, people should not get caught up in these studies here or most any of the studies–they are full of confouders and mitigating conditions that we’ll be ferreting out and batting around till the cows come home. People should be testing themselves and *see for themselves* which foodway works best for them. Glucometers are cheap, test strips getting cheapers, and it’s an extremely valuable investment in your long-term health. If you do this and follow LFHC and your BGs stay at 75-95 mg/dL all the time and you feel great, then wonderful, why change? But if your BGs are high, you are not at your target weight/BF, you still get the afternoon sleepies, you don’t wake up refreshed, then try LCHF.
What does HFLC look like in your case? What percentage carbs? I find that if I go HFLC I’m unable to tolerate even a single piece of fruit! Then, when on LFHC, adding in some fats can bring on a yeast bloom.
Of late I have tested my blood sugars. What pushes it up is both high fat or high fructose (both result in a reading of 6.1).
On high carb I drop back to 4.8, but don’t find that way of eating terribly interesting…
Craig (Craig right?), I eat 80% fat, 15% protein and 5% carbs. I calc’ed this from pulling the nutrient data from the USDA Nutrient Database and pouring it into a spreadsheet in which I made up menu sheets. The fruits I eat mainly are berries (esp straw-, rasp-, black-), avocados, and olives. About your BGs, how often do you test them and when? Even now, because I continue to be my own Grand Experiment, I test at least 4x/day–at waking, late morning (to check morning effect), 90m after lunch (my first and often only meal of the day) and at ~ 1900. Your 4.8 mmol/L equates to 86mg/dL which is normal. That you get that BG on a high-carb diet (I’m assuming you mean primarily glucose e.g. starch) suggests these invoke a powerful insulin response in you. Which leads to another concern: chronically elevated serum insulin. There’s increasing thought that chronically high serum insulin can be as bad for you (though in diff ways) as chron high BGs. The top test for that is the euglycemic clamp but that’s beyond most people’s resources. But you can get a proxy test for that called C-Peptide. You should aim to have that low, even below 1 ng/mL. Some H-Gs have this as low as 0.2ng/dL. About your higher BG (average right?) of 6.1 mmol/L (= 109mg/dL) on high fat/high fructose, do you mean when eating high fat and high fructose together. Or do you get this same number whether you eat high fat low fructose or low fat high fructose? –Bryan
Ok – so that is a very low carb diet your on. I’ve typically done about 100-200 grams of carbs when on LCHF. I can feel very much a heavy diet so I typically will skip breakfast and that seems to work ok.
With the 6.1 reading, that’s either or. I wouldn’t dare try mixing the two.
I used to have a high sugar diet, but have given that up about two years back.
It’s all very confusing really. Our traditional diet varies depending upon how far back you look. Presumably we were like other primates and lived primarily on fruits. During the paleo period I can’t see a high carb diet as being feasible in a temperate climate. And with agriculture came the high starch diet…
These three I’ve all experimented with, yet remain undecided. And there doesn’t seem to be a happy medium.
I’ve more energy on a high carb diet. But more focus and endurance on a high fat diet.
My fear is the paleo/HFLC diet will result in insulin resistance or some other metabolic damage, as I’ve witnessed first hand how little carbs I can tolerate when on such a dietary plan.
cjarman66: I don’t think you need to worry about insulin resistance or metabolic damage on HFLC, or on a Paleo diet. There are anecdotes of modern day aborigines, or Inuit, (among others) who reversed their diabetes and other health problems by going back into the wilderness and eating their native (i.e., “Paleo”) diets. If you feel that you aren’t able to process high amounts of carbs as well on a lower carb diet, it could be that the diet naturally lowers insulin levels; which is a good thing, as too much insulin in the system is also damaging and can cause many health problems. Many people who eat the SAD diet have normal blood glucose levels, but their insulin is above the roof. In this case, it is better for these people to eat fewer carbohydrates, at least for a time. (It’s been labeled “Diabetes in Situ”). If you want more information on this, check out Amy Berger’s website; she has a series of blog posts called “It’s the Insulin, Stupid”. It’s a lot of reading, but I found it quite fascinating. She’s also quite humorous as well.
My concern is born of the fact that even s piece of fruit will cause a feeling of sugar overload when eating a low carb diet. Possibly it’s too low carb and sets up the insulin resistance as Mark Sisson points out.
cjarmann66- do you mean that a piece of fruit will cause high blood sugar? Or just a general feeling of eating too much sugar? And does that happen with all carbohydrate foods, or just fruit? The reason I’m asking is that I’ve also read that high blood sugar levels can be caused by foods that you are intolerant to. I don’t know, but if you notice that with certain foods, it could be something to look into. It’s likely that if you don’t eat those foods for awhile, your body becomes more sensitive to the effects- (this is why when people check for food intolerance, they go on elimination diets, then incorporate the foods back in, to see if they notice effects).
Anything with fructose. Even grated carrot! But anyway I’ve had enough of low carb for now. I determined to find a balance. Skip breakfast, some complex carbs at lunch, fats at dinner and repeat.
MS writes:
14. Go low carb, but not too low carb.
Huh? Isn’t low-carb the greatest and most effective path to insulin sensitivity? Partly because it’s often the easiest way to lose weight, low-carb eating can and usually does improve insulin sensitivity. But when you go very low carb, low enough to start relying primarily on ketones and free fatty acids for energy, your peripheral tissues enter an insulin-resistant state to preserve glucose for the parts of the brain that require it. This is normal, and as long as you don’t try to eat a high-fat, high-carb diet, this physiological insulin resistance should pose no harm.
Read more: http://www.marksdailyapple.com/25-ways-to-improve-your-insulin-sensitivity/#ixzz3rPqvOgkv
The exact opposite actually. Since a high fat diet causes insulin resistance, a low carb diet will automatically cause insulin resistance. The fastest way to become insulin sensitive is to go on a very low fat high carb diet. Ridding the tissues of fat and allowing insulin to do its job.
Hi Zach, yes I’m across this argument. And have gone down the LFHC route and yes I agree that insulin sea usury improves. And it would want to! As all those carbs would be overwhelming otherwise.
In my experience however, you need to hit that less than 15% fats level. Otherwise it doesn’t work.
It’s as if the cells are fueled by fats or by glucose but just not both at the same time. And that the middle ground is not a balance point, but rather an unholy mix.
Less than 15 percent fat I find tolerable for only two or three days. Then something in me starts screaming out for something more substantial.
The HFLC route also has its downsides, presumably the lack of glucose for the brain…
What seems to work best for me is a period or fasting, followed by a moderate carb load, then the fats, then the fasting period again. Mixing the carbs and fats, or following fats with carbs ain’t great.
In their own, both routes, in my experience, have a honeymoon period that lasts only so long.
Denise might talk about cycling between the two next up.
I agree that fat must be kept below 15 and ideally below 10% of calories for it to be most effective. Once pufa is cleared though I have found no issues with going back to a more mixed diet as long as fat is kept mostly saturated.
I find a starched base diet to been extremely satisfying though. Stir frys, soups, stews, pasta, etc. They all can be made with little to no added fats but hit all the satiate on signals. Not avoiding sugar also helps feeling satisfied.
I like both, but don’t like exclusively one or the other….
Craig, the Jason Wyrick testimonial, it’s an anecdotal n = 1, with lots of info and context missing. What are the details on his before-change and after-change meals? Could be cutting out all that pasta and moving to leafy greens and legumes, Jason actually *reduced* his carbs along with fat/protein. BTW, eating excess protein is like eating ultra-low-GI carbs. Our bods can’t store excess protein, so must break it down into and our liver turns ~ 3/4 of it to glucose. Cutting down excess protein cuts carbs too. Reducing his overall caloric intake and his subsequent weight loss I’m sure improved his insulin sensitivity. He was able to do that by cutting out highly processed foods, designed to push our evolutionary hot buttons, and replacing them with whole foods. But, again, on his plant-only high-carb diet, we don’t know if he’s generating loads of excess insulin to cover that steady stream of carbs. I’d like to know his C peptide number.
https://www.drmcdougall.com/health/education/health-science/stars/stars-written/jason-wyrick/
He’s not alone. The diet definitely addresses the problem. The theory being that intramyocellar lipids obstruct the action of insulin. Are you aware of this theory? There’s an overview of it here http://youtu.be/OZEXimc9YPs
and here http://youtu.be/es4PFR5GZTY
So it’s clearly more than an n=1 phenomena.
And is it the less carbs and more greens? The rice diet would suggest otherwise.
Craig, to answer your comment starting that includes: “…Our traditional diet varies depending upon how far back you look. Presumably we were like other primates and lived primarily on fruits…” I agree, and it also depended on where you lived. There are groups following ancestral high-carb foodways like the Kitavans, and they do just fine, or did. The Northern Greenland Inuit who lived ancestrally ate almost NO carbs. We evolved into very opportunistic omnivores, to handle almost any macronutrient mix. It’s just that in our modern times, other novel factors have damaged our ability to properly dispose of serum glucose into our cells/mitochondria. Since the end of WWII 70 years ago, Dupont, Monsanto etc have creating over 100k novel chemicals, some, even many of which, like BPA and phthalates, are estrogenic (i.e. our bods think they are estrogen). Our bods respond to perceived excess estrogen by increasing cell membrane resistance to nutrient/waste ingress/egress. Chronic exposure to estrogenics –. chronic cell wall stiffness –> chronic insulin resistance (IR) –> metabolic syndrome in which IR and insulin keep leapfrogging up. When the beta cells (which make the insulin) cry “uncle” you get Type 2 diabetes.
Craig, re Jason Wyrick et al, what you say: “diet definitely addresses the problem.” Let’s be clear on what *part* of the diet addresses that prob. Jason went from eating a lot of processed calorie-packed crap to eating whole foods with lots of fiber and micronutrients. That allowed him to *reduce overall calories* and so lose weight, likely the single biggest factor in normalizing his BGs. What if he ate such a diet of whole foods, with the same # of cals, that skewed high fat low carb? Point is, the *quality* of the food is much more important than its macronutrient mix. You see that reflected in the fact that both sides, the HCLF and LCHF folks, can trot out endless numbers of compelling testimonials to support their respective sides. As far as whole foods vs processed foods, Kempner’s Rice diet is a poor defense for processed foods. As I said to Zach: “The average fasting blood sugar (FBG) for folks after 22 weeks of the Rice Diet was 155 mg/dL–still diabetic! Normal fasting BGs are 75–95. This Rice Diet is hardly a ringing endorsement for completely resolving diabetes. I was T2D in 2007, and since *normalized* my BGs with LCHF, averaging 90 mg/dL.”
re the Michael Greger vid, here’s the meat (nut?) of what I got from it:
1) high insulin response to meat;
2) Intramyocellular lipids lead to muscle cell IR, and;
3) “preliminary study” from 1927.
Let’s first address 1) meat’s high insulin response. Here’s the link to the Holt study MG mentioned, full text is free: http://www.ncbi.nlm.nih.gov/pubmed/9356547 . It makes sense. Meat is protein-rich and cells need insulin to help them take up amino acids, protein’s building blocks. That’s one of the reasons I limit protein to a modest 15% of total cals (remember, I’m 80% fat, 15% protein, 5% carbs)
Now 2) intramyocellular lipids. MG merely discussed the IR problem they cause. He fails to definitely show *where* these intramyocellular lipids come from in the first place. At 4:45 MG cites “sat fats as esp lipotoxic and IR promoting Well guess what Craig? If you eat excess carbs, your liver turns these carbs directly into *demon saturated fat* and ships them back out into the blood! Specifically it transforms to palmitic acid (a 16C sat fat).
Finally 3) the prelim study from 1927 on a very small cohort to support his claim that a high-fat diet lead to diabetes. Here’s the first page of that study:
http://archinte.jamanetwork.com/article.aspx?articleid=535594
Alas the rest is behind a paywall. Craig, if you have the full text of it, will you please send it? Thanks. Please understand given the study’s prelim status and the primitive assaying tools we had at that time and the small cohort, I can’t put much stock in this study at this time. Also remember it flies in the face of my own experience. I was diabetic on HCLF, and *normalized* my BGs after going LCHF.
re the Jane Esselstyn vid, I started watching it, but I’m sorry Craig, as soon as she asserted (and I quote) “…[glucose is ] … the only thing your brain eats, glucose, that’s it…”, she lost credibility with me and I didn’t want to waste further time on it. Her claim flies in the face of well established fact that the brain also burns ketone bodies. Here’s one of zillions of reputable sources to show that. What’s mystifying is that Jane is an RN and had to learn that: http://watcut.uwaterloo.ca/webnotes/Metabolism/fatKetoneBodyMetabolism.html
Lol! What kind of bubble do you live in? Billions of people eat a diet of high carb/low fat and have no issues with western disease. It’s only been an issue once western diets high in fat have been inyroduced. Most of the world lives off of a grain of some sort. Rice, corn, wheat, barley, potatoes and other starchs are not just a side dish, they are the bulk of the calories around the world. Every single blue zone culture eats a high carb diet.
Did you even read this article? There were people a hundred years ago curing type 2 diabetes with a sugar diet. There are people now like Neil Bernard who cure diabetes on a all carb diet. It’s been established. I honestly have no clue how this is not common knowledge. The paleo/low carb sphere is like this tiny microcosm of people really living in the stone age when it comes to research.
Zach, good lord, don’t you even think before you hit Enter? “Diabetes, cardiovascular disease, and cancer are among a group of chronic diseases that accounts for most deaths in all regions of the world except South Asia and sub-Saharan Africa.” That’s straight out of this:
http://www.prb.org/Publications/Articles/2007/GrowingGlobalChronicDiseaseEpidemic.aspx
When you have to live on a subsistence diet, and have to do a lot of physical labor through the day, your bod cares a lot less where that calorie is coming from be it from a carb, or fat, or protein. But then those people often suffer from a lot of nutrient-deficiency conditions like kwashiorkor and iron-deficiency anemia.
And Zach when are going to start giving us links to back up your wild claims? Where does it show Neil Barnard or anyone else “cure” Type 2 Diabetes? “Common knowledge” doesn’t cut it pal. About your claim: “There were people a hundred years ago curing type 2 diabetes with a sugar diet.”Let me turn your question back to you Zach: Did YOU even read this article? Maybe you’re thinking of another article? Maybe you conjured this out of thin air? Because I sure didn’t see anything in Denise’s piece to support that wild claim. Kindly point that part out to us OK?
What about this?
https://www.drmcdougall.com/health/education/health-science/stars/stars-written/jason-wyrick/
89mg fasting is pretty good right? I’d say that’s a cure. This guy eating a very high carb diet.
@Zach – “Every single blue zone culture eats a high carb diet.”
That is factually untrue. Most traditional societies are relatively low-carb compared to the modern SAD diet. But it’s always relative.
Consider the Okinawans who, prior to WWII decimation of pigs, fed most of their sweet potatoes to the pigs. Yet immediately after the war, without many pigs around, they ate more of the sweet potatoes.
Even then, their diet was so calorie-restricted that their total carb intake was still very low. More important might be the fact that traditionally Okinawans cooked almost everything in nutrient-dense lard.
People that frequent health blogs are usually sick and woefully out of shape. Especially ones that eat high fat. Not me though, I’m lean as fu*k, it’s all them carbs.
Btw I eat dairy so I can’t be durian rider. 😛
Zach great for you that you are “lean as f*ck” as you put it. Btw, how old are you? I mean chonologically? As for your comment “People that frequent health blogs are usually sick and woefully out of shape.” Of course you can’t possibly know that. It would help us all if you stopped yanking stuff out of your derriere.
“Zach”- you eat dairy? Really?!!!! What about all that (gasp) saturated fat? Aren’t you worried about getting diabetes?
Here’s something to ponder: back in the past, diabetes was actually called “sugar diabetes”. If you look at the words “diabetes mellitus”, the word “mellitus” is from the Latin word for honey. Gee, why did they use words like “sugar” and “honey” to describe diabetes? Could it be that it had something to do with sugar, and nothing whatsoever to do with fat?
Yes because sugar is excreted in the urine. Odd that you know the mean ing of the word but nothing about it. Interestingly doctors over 150 years ago found that by giving their patients butt loads of sugar, they would stop excreting it in urine and effectively curing diabetes
Btw I eat low fat dairy.
“Zach”- yes, it was sugar being excreted in the urine, NOT fat. The copious urinary output is the body’s attempt to rid itself of the sugar in the bloodstream. (And yes, some doctor’s did taste the urine). In 1798, a Dr. John Rollo discovered that carbohydrate diets caused a higher output of sugar in the urine, whereas protein lessened it. Therefore, he put patients on an “animal diet”. This was the standard of treatment for diabetes for many years, until the discovery of insulin.
And “Zach”, by the way, you make all these ridiculous claims, but never support them! Who were these people feeding their patients loads of sugar to “cure” diabetes? I even googled it, and found nothing. Oh, but by the way I did find loads of links explaining how people with diabetes type 2 have carbohydrate intolerance, and that they can help themselves by reducing dietary sugars! So, if you want to make a case for something, you’re going to either have to be a little more specific, or post a link, or something. Instead, you resort to ad hominem arguments; (hmmmm, just like Durian Rider).
Lol, dude you don’t even understand the basic mechanisms behind the “carb intolerance”. Do you think some people just all of a sudden eat too many carbs and become diabetic? If that was the case all of Asia would be dead.
Fat blunts insulin effectiveness. Fat causes diabetes, not sugar.
Lol, there you go again, just being insulting, but not actually saying anything of substance, with no support to back up your claims! If you’re trying to criticize *me* for not “understanding the mechanisms of carbohydrate intolerance”, well, I was writing what doctors and researchers have to say about the subject. So I guess they’re all wrong, huh. (And by the way, I’ll mention one more time that after looking, I did not find any evidence that feeding diabetics sugar will cure them).
And I never said that all people eating a high carb diet will “just suddenly get diabetes”, you put those words in my mouth. I only said that fat has nothing to do with it. The traditional Asian diet is a whole foods, non-industrial foods diet, and they did not eat a lot of sugar. And the Masai, the Inuit, the Mongolians, the Siberians, the Sioux Indians (all those high fat people) also did not get diabetes!
http://www.sciencedaily.com/releases/2011/08/110814141432.htm
Zach- wow, finally, a link! (I so prefer intelligent conversation to mud-slinging insults). Interesting study; but, the problem with it for me is that they used rodents instead of humans. In fact, our own Denise Minger debunked it (and studies like this). Here is a guest post she wrote for Mark’s Daily Apple:
http://www.marksdailyapple.com/does-a-high-fat-diet-cause-type-2-diabetes/#axzz3rb005nnt
They called it “diabetes mellitus¨ because when the urine was sweet tasting, sometimes sugar spills into the urine and before blood tests they probably tasted the urine.
yes, the more I read about nutrition, the more confused I get about what to eat… today I’m kinda sick, and ate gluten free toast with butter, and hot pepper, rice with tomato sauce, low carbing, if I stick with it makes me lose weight, but it is really hard, not eating carbs effects my mood really negatively, I’m allergic to casein and gluten, so that complicates things further, eating rice sounds great..I think if I want to lose the 30 to 35 lbs that I kept on post kids, I just need to eat less, I bought into the theory that it is not the calorie intake that counts, but low and behold, last time I had the same dry cough as today and ate only toast for a week I’ve lost 10 lbs in a week… but during my 2nd pregancy I had gestational diabetes which I absolutely kept under control by eating low carb and walking after meals,
confused to the max though by this blog post, but Denise your writing style is so funny that confusion or not it was worth reading it just for the nerdy entertainment factor, my husband is reading it now, and laughs out loud reading each of your funny nerdy jokes, thank you for being honest and dig deep into each issue, science in not static, otherwise it stops being science but becomes a dogma
yes, the more I read about nutrition, the more confused I get about what to eat… today I’m kinda sick, and ate gluten free toast with butter, and hot pepper, rice with tomato sauce, low carbing, if I stick with it makes me lose weight, but it is really hard, not eating carbs effects my mood really negatively, I’m allergic to casein and gluten, so that complicates things further, eating rice sounds great..I think if I want to lose the 30 to 35 lbs that I kept on post kids, I just need to eat less, I bought into the theory that it is not the calorie intake that counts, but low and behold, last time I had the same dry cough as today and ate only toast for a week I’ve lost 10 lbs in a week… but during my 2nd pregancy I had gestational diabetes which I absolutely kept under control by eating low carb and walking after meals,
confused to the max though by this blog post, but Denise your writing style is so funny that confusion or not it was worth reading it just for the nerdy entertainment factor, my husband is reading it now, and laughs out loud reading each of your funny nerdy jokes, thank you for being honest and dig deep into rach issue, science in not static, otherwise it stops being science but becomes a dogma
Hi, just to let you know toast and rice does not sound like low carb, when people do low carb they avoid bread of any kind, all grains and legumes for starters. But sounds like you might do very well with the high carb low fat diet.
When it comes to the subject of carbohydrates in particular, I haven’t found a better study than this one: http://www.ncbi.nlm.nih.gov/pmc/articles/PMC3402009/ in helping me to choose what, if any, carbohydrates to eat!
It’s the BEST study, bar none , I’ve ever read on the subject..!! Personally, I heavily base my philosophy of eating on this study, and I’ve read many studies/books on the subject!
I read the article you left the link for and it was interesting. What I find that makes me question it is the fact that the diet studies may have been comparing apples to oranges. There are many so called low carb studies but many have a wide range of what they consider to be low carb, the same is true of low fat studies. A diet comparing a diet of 50 grams of carbs is very different to one using 100 or more grams of carbs. The same for low fat, 25% fat, 30% fat versus 10% fat. You cannot say anything about them in comparison terms unless the are comparing the same amount of fat or carbs. This is an issue that has to be discussed whenever you are comparing different types of diets – something the authors of this paper do not do.
Skyking, thanks for this paper. Makes good sense. My initial read is that, in essence, the cell walls lower carb density and retard carb absorption and even prevent us from absorbing some of those digestible carbs. E.g. carbs that may be tucked inside cells with lots of cellulose in the membrane. Cellulose, we can neither enzymatically digest it nor ferment it, so appears we need highly acidic stomach juices, even physical pulverization of the food, to liberate the carbs contained therein. All this adds up to our GIs powerfully moderating our absorption of what ends up being fewer carbs. All good in my books.
All that said, Melissa McEwen gives and interesting take on Spreadbury’s paper here, suggesting we created acellular carb foods early on:
http://huntgatherlove.com/content/acellular-versus-cellular-carbohydrates-and-endotoxins
She suggests humankind began to high process carby foods earlier than we conventionally think. That we ate highly acellular carbs even well before the Ag Rev. This suggests other factors are at play to promote our modern-day carb intolerance epidemic. AND possibly that we initiated lots more carb intolerance in those very early days. And of course couldn’t know that since we lacked the tools to measure it. –Bryan
Someone mentioned this paper, but I can’t find the comment now to give credit:
http://www.ncbi.nlm.nih.gov/pmc/articles/PMC3402009/
It’s an amazing paper, and maybe explains a whole lot. The idea is that foods where the plant cells are intact, feed microbes differently than cells that are pulverized. Hence whole steamed rice is very different from ground rice flour. This causes signalling such that eating a ground-grain diet may cause obesity, where eating steamed whole grains does not. Eating a sweet potato is not at all like eating a slice of bread.
Now another thing that massively affects microbes is *iron*. One thing about white sugar: it doesn’t feed yeast well. This is the principle behind homemade root beer. It’s very sweet, but because there is no nutrient, the yeast die out before the alcohol level gets very high or the bottle explodes. Iron also has a massive effect on insulin levels in the body. Plant-based iron isn’t absorbed easily, but the iron in iron-fortified foods (processed foods) or in meat can be over-absorbed. Mix iron with starches or sugars though, and the microbes go nuts, and your insulin levels go nuts too.
One thing in common about all these uber-low-fat diets is: they contain whole plant cells and are also very low in fast-absorbing iron. Pritikin allows whole-wheat bread but seems to encourage whole grains. Whole wheat is also an iron-blocker (as is brown rice). Low-carb diets generally don’t have bread or pasta at all. But swampland diets are generally loaded with ground grains and also with high-heme meat.
I’ve been posting the link to this study and commenting on it on various sites, which is where you may have seen it. For some strange reason, strange to me anyways, is that it gets very few responses from readers. Perhaps because it’s too long and most folks didn’t bother reading it, and/or because some well-known blogger/tweeter didn’t post it first…?!
I haven’t commented because I’m still trying to grok the implications! Thank you for posting the link
I suspect few people actually read through it or understood it. I’ve sent some papers that were far easier to people I consider smart, but they just couldn’t follow them. This one took some work for me to follow too. It’s worth it though … there are some interesting gems all over in it.
I guess everyone is too used to the predigested quickie versions. The ground grains of the writing world!
Chris Kresser and others have featured this study in the past, but as I remember, it didn’t generate a huge amount of discussion even back then. Probably you are right, most people don’t want to take the time to read it. The hypothesis makes a lot of sense from an evolutionary perspective.
But I wish folks would be more rigorous in discussing the consumption of grain among Paleolithic people and historical hunter-gatherer cultures. The archaeological evidence is pretty clear that Paleo people, even the earlier, not-quite-modern-man types, did consume grain. It would have been an amazing coincidence, not to mention a risky survival strategy, if people in several different, widely-separated regions suddenly woke up one morning 10000 years ago and said, “Hey, see that tall grass over there with the seed heads that we’ve never noticed before? Let’s give up gathering and hunting, settle down, and use it as the basis of our diets!” Man has always been the ever-opportunistic omnivore, eating whatever was available, or he would not have survived. That being said, think of how utterly different those wild grains were from our modern ones, and how seldom they were available. Like any wild food, they were eaten in season. They took a lot of energy to gather and process. The “berries” were much smaller than modern versions. And they probably didn’t taste all that great. One theory on the development of agriculture, at least in the Near East, is that Paleo man started storing the wild grain for hard times, discovered that it easily propagates, and the process evolved from there.
The paleo people did consume grain. So did the Medieval Europeans. But hardly anyone actually ground grain into a fine flour. THAT was expensive. If you look into history, you see most people ate “gruel” … which is a kind of long-boiled whole grain mash. Most of it was barley,not wheat (wheat was harder to grow). Also once you grind grain into flour, it goes rancid quickly and molds too.
So rich people … yeah, they had flour, and bread. And also it was common in certain cultures and places. But rich people were noted for being less healthy in general, so it doesn’t say much.
Now the history of *bread* … the Egyptians may be the first bread-makers. But they made it in order to make *beer*. When you grind grain and make it into bread, it turns out to be really awesome for making beer. Later people started eating the bread by itself.
http://ancientegyptonline.co.uk/beer.html
Well, who knows. But the point is: bread feeds microbes very differently than gruel does.
So I would challenge anyone here: take a cup of whole grain (any grain except white rice) and boil it until it’s chewable. And eat it.
Brown rice is the best, but try eating a cup of boiled whole wheat. You CAN do it, and in some times and places people do it. But most Americans won’t. If you do, it will fill you up quickly and you will eat a whole lot less calories than if you ate white bread or whole wheat bread.
The paleo people ate grain, but it was whole grain boiled or parched. In order to really grind grain you need millstones, which are way too heavy to schlep around. You can grind small quantities on small stones, but it’s not a fine grind. Or it was pre-fermented, as you see with the native Americans. They processed corn with lye before grinding it, which changed the digestion also (and incidentally made it easier to grind and the B vitamins easier to absorb).
In the Bible, it was stated someone in debt, their millstone was not to be taken. There is a lot of work to process grains, and the industrial revolution (machines ) changed how grains were processed-resulting in flours deprived of nutrients, but with a longer shelf life. . A few B vitamins were added.later, but did not make up for was originally in the grain and the fermentation process. The Egyptians also make a lot of cakes-honey and fruits being added.
http://www.sciencedirect.com/science/article/pii/S0305440383710186
http://classroom.synonym.com/foods-eaten-during-ancient-egyptian-festivals-9968.html
“fine flour” was mentioned in the Bible, and Egyptians had a type of fine/white flour, as further milling had to be done.(yes more time consuming and more expensive) Some people today report that they have less problem with white flour,as the brain parts are harder to digest,due to the protein content, or that they do not have the bacteria necessary to digest the fiber. Too much fiber seems to be a problem with some.
http://www.ancientegyptianfacts.com/ancient-egyptian-diet.html
In the “Little House” books, the “Long Winter” they faced starvation and had to grind wheat into a flour using a coffee grinder.
Yes, the Egyptians are a super-interesting case! They (and the Mesopotamians) were about the first people ever to eat large amounts of wheat and barley, and to grind it. It was all non-GMO, whole wheat, organic too. And they left lots and lots of mummies so we can judge their health.
Basically they were in really bad shape, compared to other peoples living at the same time. They had very narrow skeletons, which is likely a sign of lack of Vit D or K … and it certainly wasn’t a lack of sun. One interesting mention in the Bible is that the Egyptian women felt threatened by the Israelites, because the Israelite women could give birth so easily, they would soon outpopulate the Egyptians. Hm. The Israelites were herders more than farmers.
The richer Egyptians had more meat and plenty of honey. But so did the the nomadic people surrounding them. I think ground grains, esp. wheat/barley, have a unique health risk.
Rice (according to SkyKing’s article) appears to not always have the same effect. But another thing about wheat is that it is high in fructans, which break down into fructose. Rice breaks down into glucose.
Also, apparently the Egyptians were mostly vegetarians … they had plenty of fish, but tests on mummies show they didn’t eat fish or meat much.
https://www.insidescience.org/content/what-did-ancient-egyptians-really-eat/1630
There are billions of people in the world that eat mainly one starch their whole lives … rice or wheat or yams or millet. The wheat-eaters seem to have the most health problems. Denise’s take on the China Study points that out nicely!
Dr Google says many mummies were riddled with atherosclerosis …
You might find the book “The Leopard’s Tale” by Ian Hodder interesting to read. It’s about the excavation of the early neolithic village Catalhoyuk, and a detailed description of life right on the transition from paleo to neolithic living ca 9000 BC. Cattle (auroch) were not yet domesticated, and required large hunting parties (based on the wall drawings – the inhabitants were prolific painters in their cave-like stack houses). The bones in the middens are mostly smaller animals like sheep and goats. The dwellers were pre-pottery, and cooked on hearths and in tightly woven cooking baskets heated with rocks. Grains were gathered and stored. I had the the impression that they were mostly eaten whole, and probably roasted, since hot rock basket cooking would do little more than soften the grain (not hot enough or long enough to cook the starch and make it digestible).
Reading this changed my view of Paleo. These people were not eating Bronto burgers and ribs, bombing mammoths with rocks, spearing seals, or chasing buffalo on horses. They were stalking small animals and birds, and stealing their eggs and babies mostly in the springtime, traveling ever longer distances from their dependable water source town to find them. There are shells present, evidence of long distance travel (ca 100 miles) and the beginnings of trade. Some of the animal babies were probably being spared and becoming modern domesticated animals.
If these people were in ketosis it was not from eating HFLC, but more likely from being on the edge of starvation all the time. They ate anything they could find that they could digest (though it’s apparent that they were headed towards agriculture), and lived in the place most conducive to survival (ie not the Arctic or the high plains). If they were doing heavy lifting and sprints it was as infrequently as possible. Mostly they were walking, gathering more than hunting.
I suspect that grain was probably gathered more to feed animals rather than to eat, since animals can digest the starch beta linkage without needing to have it cooked.
Humans were eating grains long before they had animals to feed. The feeding of grains to animals came with the transition to agriculture. You’d want to have your animals stationary and where you could watch them fatten if you were feeding them grains. Early pastoralists, who might have been the intermediate stage between hunter-gatherers and agriculturalists, took their flocks to pastures to eat grass. They didn’t feed them grains. Even today, grain feeding of cattle comes at the end of their life cycle — they eat range grass until they are brought to feedlots for finishing.
Eating grains is not beneficial to humans unless they are cooked. We cannot gelatinize/rupture the starch cellules to release the starch molecules in our bodies. Ruminants can break down the cellules with enzymes and time, but we can’t. The starch has to be heated above its gel point (ca 50-70C) before we get any food value. As evidence of this, both the caloric value and glycemic index of raw cookie dough are about half that of baked cookies. The uncooked flour in the dough is essentially indigestible particles, of which only a little bit can be digested in the lower GI tract. The same is true of raw potatoes vs cooked potatoes. Without cooking a human might as well eat straw (cellulose – that’s the source of indigestible beta linkages, not starch) as grain.
By 9000 BC maybe the people at Catalhoyuk were eating a significant amount of their daily calories as grain, but I doubt it. They did know that to get any calories out of grains they had to be roasted, but they didn’t have even simple technologies (milling and fireproof cooking vessels) we take for granted. On the other hand, animals like cattle, sheep and goats will eat grain in preference to straw. If you were going to tame and fatten animals on a year-round basis grain would be an easy food to collect and store.
Humans and near humans have been eating grains since there were humans, long before they domesticated any animals, even the dog. The archaeological record is clear on this. When proponents of no-grain diets insist humans did not eat grains until the advent of agriculture, they undermine their credibility because they are ignoring the scientific evidence. Critics of the Paleo diet get a lot of mileage out of the no-grainers’ refusal to acknowledge the scientific evidence. And yes, humans can digest raw grains; perhaps not so well as some animals, and perhaps not without chewing them very well and/or grinding them. They can, and do. I have myself done so, as I am sure many other commenters have. For years, one of my favorite breakfasts was a mixture of raw oats and raw wheat germ, soaked in raw milk with honey. It worked very well for me. I did strength training, ran marathons and weighed about 118 lb on a 5’6″ frame. But I seldom eat grains these days, cooked or otherwise. I agree that grains are not an ideal food for humans, but they are an even more unnatural food for cattle. We are omnivores, cattle are not. Omnivores are opportunistic eaters, and can process just about anything, at least in small quantities. While primitive man ate grains (occasionally and sparingly), wild cattle do not eat grains.
And btw, there is also scientific evidence that humans were cooking food at least 400,000 years ago. So to say that a Neolithic people lacked milling and cooking technology is simply inaccurate.
All I can say is read the book and draw your own conclusions. Mine conclusion is that the technology of grain preparation for human consumption was not very advanced by 9000 BC. 5000 years later, Egyptian and Mesopotamians had moved on. Oxen were being used to move big things, and IMO these animals were primarily grain-fueled. These weren’t goats and lambs skipping around the hills. Millstones, pottery and metal tools had been invented which didn’t exist in 9000 BC. People were still cooking on open hearths or in pits the way they did 400,000 years ago. Only now they were doing it inside. From the soot deposits on their ribs it must have been like living inside a chimney.
Being an archaeology buff, I am sure I’ll enjoy the book. I’ve requested a hold on it from the local library. However, I fail to see why you feel that the level of technology and food prep at one Neolithic site — Catalhoyuk was a Neolithic, not Paleolithic, site, and by no means even the oldest of the Neolithic sites — determines the use of grains or the effectiveness of cooking methods in other locations around the world in Paleolithic times. These Neolithic villages housed agricultural societies in a temperate climate. Their accomplishments in no way detracts from the performance of humans in earlier, more environmentally challenging conditions. The toolkits and lifeway debris of earlier cultures indicates that they were experts at exploiting their environments. As archaeology advances, our level of knowledge shows that Paleolithic peoples were far more advanced than the images of the grunting caveman that prevailed in the early 20th century. Think of how drastically our image of Neanderthals has changed since that time. And how we’ve come to realize that the ancestors of today’s indigenous Australians had watercraft capable of open-ocean voyages 50,000 years ago. Should we think these people weren’t advanced enough to exploit all the food resources their environment provided? The evidence they left behind says , “not so”.
Actually, mill stones have been found in much older Neolithic sites than Catalhoyuk. There is a 12,000 year-old site in what was Kurdistan where the excavations have exposed mill stones and troughs for grain processing. And Paleolithic grinding stones (with flour residues) go back a good 30,000 years. Might be helpful to read more than one book….
What nonsense about cattle not eating grains! What do you think silos are for? Cattle don’t spit out their corn kernals, nor do pigs or chickens. Why do you think the Bible says do not muzzle the ox on the threshing floor? No one was worried about them eating chaff, they didn’t want the oxen to eat the grain. But the cattle have an entitlement to grain for the work they do. That’s the point of the commandment.
Technology moved in fits and starts. Maybe someone even had a wheel in 9000 BC, and I don’t doubt that some people in other areas were crushing/milling grain to make it more edible. But at that point in human history you had to use what you found locally on habitable sites. That particular village was sited on a lake/swamp, and the evidence is that a lot of animals were eaten, probably attracted to the available water the same as the humans. Other sites might have had an abundance of grains and suitable rocks (Catalhoyuk from what I recall had a lot of clay, which was useful for interior stucco, but not for milling grain). On the coastlines and rivers why bother with any of that stuff if you have infinite fish, water birds, tubers, berries and mollusks.
And list off some books. I only came across this one while I was researching kilims. My Paleo education comes from books like this and a trip to Lascaux, not from Mark Sisson or even Loren Cordain. I’ll read their blogs but I’ll never spend a dime on their books. Primary sources are better than “a filter of a filter of a filter with random unsubstantiated opinions” thrown in IMO.
The basket weaving techniques and decorations used in central Turkey ca 9000 BC are almost identical those used by North American Indians. Coastal Salish tribes used hot rock cooking baskets well into the 19th century. The Siouxans and Inuits were not Paleo at all, but rather regressed Neolithics who migrated from Asia. Their Neolithic knowledge of agriculture transferred directly into Inca and Aztec culture. In the high latitudes survival required living as what Cordain considered “Paleo”, but is dissimilar from the true Paleo culture of Africa and Asia Minor. Warmer climates produce a much wider range of human foods than buffalo, pemmican and seal blubber.
Who said that domesticated cattle didn’t eat grain? I said it is not a natural food for cattle. Just as doughnuts and sodas are not natural foods for humans, despite the quantity of them we consume.
So when a wild cow (or auroch) eats wild hay it spits out the seeds? Come on. Oats, milo, barley etc all grew wild in the Mideast. Ruminants aren’t picky eaters. That is their NATURAL food.
Wild hay??? Hay is a manufactured product, consisting of all sorts of green stuff from crop harvesting. Wild cattle eat grasses. Grains are, of course, one type of grass, but the seedhead portion of wild grains is pretty insignificant compared to the grain that is fed to cattle today. Cows have the elaborate digestive systems they do to digest the fibrous, cellulosic portions of the grasses, not the unnatural grain-based diet most of them eat today. Why do you think there is a premium on grass-fed beef?
If I can’t say “hay”, what should I say? A WILD GRASS PLANT BEARING A SEEDHEAD? OK?
There’s a premium on grasslot beef because of the unsustainable land area required, vs the cowschwitz approach. https://en.wikipedia.org/wiki/Harris_Ranch
I prefer my beef massaged with beer, with fat marble that melts on the warm plate before cooking. But that’s a notch up from even grasslot and I only eat it on an expense account.
Oh that is so funny. When I was growing up, “grassfed beef” was the CHEAP stuff, and sales guys would try to talk us into buying the premium corn-fed beef. It costs a LOT to feed a cow corn.
As for “unsustainable land use” … growing a cow on grass is about as sustainable as it gets. There are many acres of not-farmable land, which will grow the heritage Longhorn cattle just fine. They are the descendents of the cattle brought over by the Spaniards on their ships. They got loose and were in huge herds, like the buffalo, by the time white people even noticed them. Some people are using the same trick now, to avoid the big brush fires that happen when grass grows unmown.
Where I live, farming isn’t very profitable, but grass grows good and it’s been traditional for landowners to pop calves onto the land just to mow the grass. Then a few years later they harvest the beef. But it is very lean beef, not the stuff you buy in the store. To make it fat they may “grain finish” it. But these days they can sell the same cow at a premium as “organic grass fed beef: never fed grain!”
Grass-feeding is sustainable — it’s how Nature has fed hooved animals for eons. You are reading too much vegan propaganda. It is the raising of vast amounts of grain to feedlot-finish cattle that is unsustainable. Yes, wild cattle may consume incidental amounts of wild grain when grazing. They also consume incidental amounts of insects and soil, but that does not make them bats or earthworms. Concentrated grain feeding of cattle, per the US agribiz model, is evolutionarily unnatural. As for wild hay — perhaps it was eaten by the bovines being stalked by the packs of wild poodles roaming the earth in Paleolithic times.
I’d agree with you on nearly everything. Your elaboration of grain use through the ages will, it is hoped, encourage folks to be more accurate in discussing grains vis-a-vis the Paleo lifestyle. It just weakens the case for the Paleo diet, and leads some people (many of whom need no encouragement) to stereotype and ridicule the Paleo lifestyle when its proponents assert that Paleo peoples “did not eat grain”. Your point about beer making is great. I ‘ve even speculated that maybe the reason people started using grain regularly was due to their experience with fermented grain when some of their stored whole grain got wet. There is archaeological evidence that, even before the Egyptians made beer brewing an art, other peoples were making beer of sorts. Even some isolated and recently-discovered (19th-20th century) peoples make primitive-style beer. Where I would take exception to your comments is the implication that using intact grains is difficult or unpleasant in modern cuisine. In fact, the use teff, farro and such (steamed, boiled or otherwise prepared in intact form) is very trendy among celebrity chefs. And those grains can be as tasty as brown rice. Still, modern peoples are far more dependent on grain than can be justified if taking an evolutionary approach. And I wonder if the grinding process also makes some of the non-grain, “Paleo-friendly” flours less desirable as well? Doesn’t grinding break down their cell walls, too?
Yes, I agree whole grains are trendy right now. Also the use of a whole lot of different kinds of grain, some of which are quite tasty! I actually had a lot of experience with whole wheat though, because I inherited a 50-lb container of it from a previous housemate, and we were poor enough that we loved the free food. NO ONE though, would eat it. We tried cooking it various ways, but there is just something about whole wheat berries that didn’t work for us.
Nationally, whole wheat berries simply aren’t ingested much, at least not by anyone I’ve met.
I agree in principle with the idea of a “paleo” diet, in terms of looking to see what our ancestors ate. The issues are as you pointed out … what they ate isn’t what we may THINK they ate. Also there was a wide variety of diets. And not all the cultures were equally healthy. Or thin, or long-lived. It is interesting reading the journals of Lewis and Clark. They were studying the native Americans, and apparently Lewis was getting a reputation as a healer so they came to him with their illnesses. Lewis commented that the natives had a high rate of joint problems (arthritis, sounded like). He also commented on which tribes seemed healthier than others.
I think that the grains were collected mainly to feed and domesticate animals, before efficient cooking methods were developed to allow human consumption. Living in France I saw this attitude towards fresh corn, which is disdained as a food for humans and grown mainly for animal feed.
The poor opinion of corn in many European countries is a relic of the early racist view of the Native Americans that used it as a staple food. Europeans of the 15th-19th century also shunned many other New World foods. Yet, 80% of the world’s current food production is based on New World species.
I don’t think so. Europeans had no problem co-opting tomatoes, squash, potatoes, peppers, etc etc etc. so racism has nothing to do with it. I think in the case of corn they were just copying modern American livestock feeding practices, and didn’t have any French tradition of eating corn-on-the-cob, creamed corn, cornbread, etc. Molasses was similarly hard to get in a French grocery store. They know what it is, but don’t have any use for it, so no one buys it.
Much of the corn grown in the US is fed to livestock, and so is a lot of the wheat.
http://corn.osu.edu/newsletters/2011/2011-18/feeding-wheat-to-beef-cattle
The problem with grain is overfeeding, not a animal’s revulsion to eating it. In the wild, most of the plant (oats, barley, milo, etc.) is roughage with very little weight in the seedhead.
They did no such thing as co-opting those crops, not for a few centuries after they were introduced to them. It took a lot to get them to accept tomatoes and chilis. Tomatoes were thought to be poisonous for a long time, then were avoided because they were thought an aphrodisiac. Molasses (unless made into rum) was also despised as the food of nonwhites (indigenes and slaves). Food preferences today still reflect the attitudes of a less-enlightened past, if we dig into their historical basis.
It didn’t take much time for Europeans to adopt new world beans, chocolate, potatoes and the whole cucurbita family. This year I grew musquee de provence, French pumpkins, instead of the regular jack o’lantern version the squirrels attack. Good eating AND fall ambiance without the rodent damage.
And I say co-opting, you say (fill in the blank), let’s call the whole thing off. I’m open to your term, whatever it is. You’ve already said these plants amount to 80% of something in Europe. And let’s not forget Asia, which took almost every Central American exotic fruit and made it their own, along with the tomatoes, peppers and yams. Is this also racist?
I think it’s racist to refuse to eat culturally accepted cuisines too. Not in the old days of molasses and corn, but right now. The Paleo that stalks out of an Indian restaurant (or never sets foot inside) because there’s no meat, the food is cooked in PUFA’s, and evil naan bread touched his lips, is a racist. The vegan that refuses reindeer hot pot, or southern fried chicken, or schweinhaxes is a racist. Beyond that, unless it’s due to extenuating circumstances like allergy or religion, it’s rude social behavior. When I lived in France I started drinking wine, because to refuse the wine was an insult to the host.
It is true that in the US, large amounts of corn are fed to cattle. Makes for nice fat steaks! But in order to do that, the cattle have to be fed large amounts of antibiotics, because too much grain will kill a cow. Or a goat. Handfuls of grain may be fed to animals now and then, but until very recently, ruminants got their main food: which is grass and twigs.
http://www.pbs.org/wgbh/pages/frontline/shows/meat/interviews/pollan.html
The plaque on Neanderthal teeth clearly shows that they DID eat grain, and probably they ground it too. What I was saying though is that in general it was not in the large amounts we use, nor was the grinding to so fine. If you soak wheat berries and then grind them on a molcajete, you can make them into a nice little flatbread. But it won’t have the same glycemic properties or quick digestion that disrupts the gut microbes (as talked about in SkyKing’s article). For one thing, the grain is whole. For another, it’s often soaked, possibly fermented and partially sprouted. If you are grinding grain by hand, it’s a whole lot easier when it’s soaked plus you don’t get flour dust flying all over your cave. The corn in America was soaked in lye, which also made it digest differently (nixtalamization).
When “milling” was invented, the paradigm changed. You brought your sack of grain to the miller, who then milled all of it and took part of it in payment. At some point they also learned to remove the husk and make white flour, which doesn’t go rancid so quickly. When that happened it massively changed the digestibility of grains.
Your point about cattle and grain is absolutely correct, as I had noted in responding to another commenter. For human consumption of grain, it would seem that it never was as large a part of the diet for Paleo peoples. It’s logical that hunter-gatherers would treat it like any other seasonal food until late in the Paelolithic era, when they might have begun storing it. Other than finding grinding tools, it is probably hard to tell from DNA, dental residues and such exactly how they processed the grain (soaking, sprouting, etc.) before eating it. It’s interesting that Hodder, in the Leopard’s Tale, points out that, during some phase of the settlement at Catalhoyuk, the human inhabitants consumed raw, whole (unground) grain.
“Living in France I saw this attitude towards fresh corn”
Well, France actually banned the cultivation of corn back when pellagra was an issue. So, that explains why it’s not popular there.
I just read that paper; it was very interesting! I have always believed this theory, that modern industrial foods are the culprit of obesity, and it is plausible that these foods, over time, cause leptin resistance. It would be interesting to see if soaked and fermented grains have the same effect on the microbiota; traditionally, many native cultures prepared their grains in this way- (and some modern day hunter gatherers do this)- and these people were/are also healthy and not obese. I guess they weren’t able to check that in this particular study. I think they definitely need to do more research, it all sounds very interesting!
One last thing: I have read that rats and other rodents have a lower tolerance for fat than humans, which may partly explain why fat seems to be less of a factor with humans- (unless it’s combined with lots of refined carbohydrates).
Hyperlipid has point out that lab rodent high-fat diets are so high in trans-fats and sucrose that no conclusions can really be drawn about the effect of a high-fat diet in rodents – the experiments seem designed to fail the LCHF diet. Peter feeds his own rat – Ratty! – a high fat, whole food diet much as the family eats and the last time he mentioned him, he was slim and in good health.
Jonathan Christie- good point. My guess is if they fed them a whole, “real foods” diet, they would be in much better shape. That’s a huge problem, in general, with many of these scientific studies: they are too reductionist. The people involved seem to only be focused on macronutrient content. They don’t seem to take into consideration that feeding them industrial crap that doesn’t resemble real food might have a different effect, and therefore, we can’t really base any conclusions on that.
LCHF diet studies are generally rife with funding and researcher conflicts, so I suspect they mostly do actually know exactly what they’re doing and choose Crisco and sugar to make LCHF look bad – that way, they attract food industry funding and share in that stupendous cash flow which buying corn and selling corn chips generates. Kendrick’s Doctoring Data and Goldacre’s Bad Science have turned me into a conspiracy theorist!
I actually emailed a study researcher. I asked why the high fat used to feed those rats in that study was hydrogenated fat. He wrote me back that rats would only eat hydrogenated fats. Not sure that is true, but that is what he told me.
That’s a crock of BS! Those cheap fats are artificially hydrogenated (saturated), like all the fake margarines and many cooking oils. So we are supposed to believe that rats will only eat fake fats? Rats will eat both saturated and unsaturated fats. They are omnivores, like humans. Try feeding your pet rat a bit of cheese (natural saturated fat). I bet Mikey the rat liked it. Then offer him an almond (unsaturated, i.e.,un-hydrogenated). I bet Mikey the rat liked that, too. Sadly, I think sometimes technicians and scientists will say the most ridiculous stuff to people they think are non-scientists. Medical folks seem to do this as well.
Skyking, I don’t think the paper’s too long. But it’s a tougher read than it needs to be. That’s what’s maybe keeping the readers away. Spreadbury needed to do more editing IMHO.
E.g. what he says here: “The interindividual variability in ‘Western disease’ incidence in a population eating Western foods is affected by genetic and other factors, but it is mostly these secondary factors that the epidemiology of industrialized populations would be studying if the root causes of metabolic disorders were now present throughout the population.”
What a mouthful!
Took me a while to realize Spreadsbury was saying we need to get out of our navel-gazing and compare western cohorts to hunter-gatherer cohorts, not just comparing different western cohorts. That way, we can more clearly see the universal SAD-driven root pathologies that way overshadow any genetic diffs. –Bryan
I hope Peter at Hyperlipid will have something to say about all this. Thanks to Hyperlipid, I tend to look at things from the perspective of the mitochondrion.
Taubes has a way of puffing himself up in the media, which makes him a target, especially of nutrition and physiology academia. His carb insulin assertion fits the circumstances and was for a time undisprovable. Unfortunately he uses that assertion to gain credibility, and starts to say things that are more easily disproved. Things like exercise causing weight gain and the impossibility of weight loss or weight loss maintenance without extreme carb reduction. In my own case these assertions are demonstrably false. Most of the participants in the NWCR (including me) exercise and eat LFHC, which is further disproof of those assertions.
thhq, however may you feel about Taubes personally, however you interpret his behaviors and motives, please remember the concept that insulin stores fat is shared by very many folks in the research community. Simply search on “insulin and fat storage” and you will get many hits for scholarly works. I’m not saying anyone of them are right. But it’s not a radical idea. Furthermore, what Taubes discusses WORKS for me–as best I can tell. I’m been LCHF for nine years, I’m 55 now, and my blood panels and other vitals (HR/BP, weight/body fat%) are great, and most of all I FEEL great! Do I know if some hidden health gremlin lurks in me? Of course not. Same with you. You say HCLF works for you, but how many of your vitals do you regularly measure? We know you have no idea of your fasting insulin level. What about HR/BP/body fat%. Point is thhq, not you nor anyone else has absolute proof that any one food- and lifeway works. In the absence of that, I choose LESS over MORE. No supps, minimize ingredients, stick to iert matierals like glass and stainless steel, for my cooking implements, bare minimum ingreds in soaps, etc.
thhq- has Gary Taubes really said that exercise “causes weight gain”? I find that very hard to believe. What I know he has said is that exercise can raise appetite, which may thwart the weight loss efforts of some people. Basically, the “eat less, move more” mantra doesn’t work for a great majority of the population.
However, exercise can promote better insulin sensitivity- (maybe not with everyone); I suspect this may be the reason why exercise works so well for you. However, this does not disprove the carbohydrate-insulin theory of obesity: in my opinion, it actually helps confirm it.
Yes he has said that exercise causes weight gain in the NY Mag article (which is a slightly modified form of what he published in GCBC), has carefully selected N=1 examples to make his case, and confirmed that this was his intent in an interview with Jimmy Moore. It’s all discussed on the previous page, and that’s where the links are.
I don’t think my weight loss should be used to confirm GT’s carb insulin assertion. That needs a ward study, not another N=1. If I had gained instead of losing weight by exercising I would have confirmed his weight gain assertion though…at least as an N=1. If you want to see population results on the benefits of exercise for weight loss and maintenance start with Rena Wing’s NWCR.
I’ve been thinking a lot about why GT is so hard for me to read. I think a lot of it is because he doesn’t start with an abstract. In 30 years of writing research reports it took me 10 years to learn how to do this. In front of a very familiar audience you can get away with not having an abstract sometimes, but with a mixed audience no one knows where you’re coming from. If you summarize right up front, then use your work to back up your assertions everyone is on the same page. If you do it well, you can skip lots of graphs and the obligatory literature dump, and be done with a new action plan everyone agrees on in time for lunch.
If Gary had prefaced the NY Mag article with something like “The HFLC ketosis diet is very effective for weight loss. The best efficiency for fat burning in ketosis actually results from reducing exercise, which may surprise you”, and then launched into examples which show this, we would all have been on the same page. But instead he starts right off with N=1 examples of exercise-fail and the literature dump.
Because he isn’t right up front on ketosis benefitting from reducing exercise, he ends up saying that exercise is something that causes everyone to gain weight. Even though I know where he’s coming from, and that he’s fighting the obesity crisis, I’m rankled that he’s ignored millions of us who have lost and maintained weight by exercising outside of ketosis. Despite what he may believe Weight Watchers, calorie counting, Jenny Craig, LFHC and other non-ketosis dieters increase their weight loss rates when they exercise.
What’s worse is the effect this discouragement has on someone who quits exercising after reading the article, and who will start to gain weight as a result unless they change something else. A good abstract that lays out ketosis right at the beginning would prevent the misunderstanding.
Journalists don’t write the way scientists do. Narrative writing engages the audience by building drama, and ends with the conclusion. In contrast, a well written research report starts with the conclusion stated as clearly as possible. That’s what the audience expects, because they usually need to discuss it and act on it, then move on.
When you write a research report you’re not trying to tease your audience with plot twists and turns. They won’t sit still for 200 pages waiting for the fat lady to sing.
thhq- huh….maybe it’s just me, but I really liked his writing style in Good Calories, Bad Calories. What he did was he wrote about the whole history of weight loss research, so it was a slow revealing, and a lot of the “meat’ came at the end. I guess I also prefer that he doesn’t “tell you what to think”, by writing out his hypothesis; rather, he gives you all the different evidence- (on both sides, not just the research that fits with his opinion)- so you can make up your own mind. One of his main points was that before World War 2, there was a lot of very high quality research coming out of Germany. Unfortunately, after the war, we just broke with that history, so a lot of the initial research has been forgotten. Which of course has slowed down the attempts recently to get to the bottom of the obesity epidemic. Franky, I notice this a lot in nutrition science! It’s like everything that was researched before has been forgotten, so how can we advance if it’s like starting anew each time? (Or, sometimes “nutrition science” doesn’t fit with what we know about anthropological data….that sort of thing). People seem to be too reductionist, or one-sided….In other words, Gary Taubes’ writing is less like a scientific study, and more like a history lesson that connects all that went before, but has been lost.
In any case, I still haven’t seen anything that Gary Taubes supposedly said that was anti-exercise- (not even on the link you sent, are you sure you sent the right one? I found something about salt, which I had already read before). I might try to re-read the exercise chapter in GCBC again, just to be sure. I’ve also never heard anyone say that exercise disrupts fat burning during ketosis (?) Not Atkins, Gary Taubes or anybody…..I’m not saying they never said it, just, it’s a new concept to me. On the contrary, I find I have to sometimes kick myself out of ketosis while doing strenuous exercise, otherwise I just get too skinny! I don’t feel like I *have* to do this though; I do it purely for aesthetic reasons.
Don’t know if Gary Taubes ever said “everyone gains weight” with exercise- (I still haven’t seen this in writing)- but if he did, then I would disagree with that statement. I do agree with his theory that people get hungrier when they exercise- (I sure do!)- but I don’t gain weight. I actually tend to lose with too much exercise, even if I’m eating more than when I’m sedentary. But this also fits with his general theory, that it’s less about “calories” per se, and more about hormones, metabolism, etc.
Morgana, thank you for saying so much that I failed to. And phrasing much of it so well. I too feel Taubes’ approach is one of a reporter, examining all sides, presenting evidence from all sides, never dogmatically. It’s so true what you say here:
“…It’s like everything that was researched before has been forgotten, so how can we advance if it’s like starting anew each time?…”
For me this is a genuine mystery. E.g. how could we forget the success William Banting and his many low-carb followers enjoyed in the 19th cen Victorian England?
https://en.wikipedia.org/wiki/William_Banting
As well as the success that Joslin doctors enjoyed with LCHF diets at the turn of the last century and now Joslin appears to be turning back to, if still not near enough:
http://blog.joslin.org/2015/02/nutrition-revolution-the-end-of-the-high-carbohydrates-era-for-type-2-diabetes-prevention-and-management/
Even near the end of GCBC, Taubes terms his conclusions merely by the modest term “hypotheses.” What does “hypothesis” mean anyway? Per the google def, it’s merely “…a supposition or proposed explanation made on the basis of limited evidence as a starting point for further investigation.” You can see it here:
https://www.google.com/webhp?sourceid=chrome-instant&ion=1&espv=2&ie=UTF-8#q=hypothesis
The main place I fault GT is that his prose can be dense, be a slog. I could do justice to only 10 pages of it a day on average. Maybe in future if we could team up GT with Michael Pollan and MP’s awesome lyrical talent?
One final point. I’ve been a journalist for thirty years, and understand the problems and pitfalls with reporting in periodicals versus books. Given how these pubs must abridge the info to fit into a short writeup–often simplifying to the point of being wrong–and an edit cycle that’s often out of the hands of the interviewee, we should put a great deal less weight on what Taubes said in periodicals than what he says in his books.
Morgana, rereading your post, this is esp jumping out at me:
“Gary Taubes’ writing is less like a scientific study, and more like a history lesson that connects all that went before, but has been lost.”
Perhaps I missed something, but doesn’t Gary Taubes use selective history though? If carbs caused everyone to gain weight, then how does he explain that Americans were once thin eating a high carb diet?
As far as I can tell, Americans consumed roughly 56% carbs / 12% Protein / 32% Fat in 1909, and consumed even more carbohydrates during the 19th century.
Click to access 169.full.pdf
Click to access 907.full.pdf
As you can see from Figure 1 in the first paper, American’s total carbohydrate consumption fell ~30% between 1889 to 1961. And the papers show calories decreased too.
Unless I missed something (entirely possible) Taubes seems to have skipped right over that part of American history. This ignored historical data implies that there is something else causing significant weight gain in Americans.
Duck, iirc, Taubes does go back to before 1920, before sugar was cheap and readily available. Before WWI, people used mainly molasses as a sweetener, and even that was pricey and used sparingly. Also, we started refining flour in ~ 1920, making those carbs faster to get into our systems meanwhile stripping out its nutrients.
About you saying “As far as I can tell, Americans consumed roughly 56% carbs / 12% Protein / 32% Fat in 1909, and consumed even more carbohydrates during the 19th century.” do you have a source for that high carb chowing in the 19th century? This source here:
http://onlinestatbook.com/2/case_studies/sugar.html
shows a more or less linear increase in sugar consumption from ~ 5lbs/yr/person in 1802 to *100* lbs/yr/person in 2000.
About the two papers you link to, the studies go only to the mid-60s, at least a decade before we introduced ultra-cheap high-fructose corn syrup that quickly ended up in everything, and 12–15 years before McGovern et al established official dietary policy across the land.
“we started refining flour in ~ 1920”
Sorry, I don’t understand that. We started refining flour well before that, in the 19th century.
The high demand for white flours during the 19th century were said to be responsible for the dyspepsia epidemic.
“Before WWI, people used mainly molasses as a sweetener”
Yes. Honey too.
“do you have a source for that high carb chowing in the 19th century”
Yes. Figure 1 of the first source I listed goes back to 1899. It shows a 30% reduction in carbs to 1961. The whole point of the Dietary Guidelines was to reverse that trend. Americans came to see bread as fattening, and they were eating less flour than ever before. The source is clear that Americans ate mainly complex carbs at the turn of the century, but as you can see, total carb consumption plummeted by ~30%.
I thought one of the biggest criticisms of Taubes is that he didn’t do a very good job of distinguishing the difference between complex and simple carbohydrates. Of course, there is a difference.
Anyhow, Stephan Guyenet showed what carbohydrate consumption did during the 20th century (see his chart at the bottom of this article):
The Carbohydrate Hypothesis of Obesity: a Critical Examination
As you can see, Guyenet’s calculations match up with the sources I’ve referenced. Carb consumption only increased by ~25% after the Dietary Guidelines. So, we never got back up to the level of carbohydrates that America had in 1889.
I’m not sure why it would be surprising that Americans were high carb in the 19th century. There were no factory farms and grains/porridges were a big part of early American life, going back to the American Revolution. By the 1960s, America had one of the lowest levels of flour consumption of any Western country. Again, this is why the Dietary Guidelines were written—to reverse that trend and to re-align American carb consumption with its historical norm and with other Western countries.
So, again, I have to wonder how Taubes and others have missed all this history.
Whoops, I meant to say that Figure 1 of the first source I listed goes back to 1889.
My granddad talked about his diet as a kid, back in Germany in 1890 or so. It was oat porridge and potatoes, and lucky to get it. Plus whatever vegies they could grow, and goat milk. He did eventually take a job as a servant in a castle where he could get “meat every day”, but he counted himself lucky.
There was a huge gulf between what “rich people” ate and everyone else, and there weren’t all that many rich people. If you look at the pictures, a number of the rich were quite obese and sick (Henry 8 comes to mind, and Ben Franklin, and Genghis Khan for that matter).
Still, when granddad moved to the US circa 1930, he could eat anything he wanted and so could grandma. Neither got fat, or cancer, or high blood pressure, and grandma lived to a healthy old age, died at 96.
Duck, in your first post, your question: “If carbs caused everyone to gain weight, then how does he explain that Americans were once thin eating a high carb diet?” Then you follow with this: “As far as I can tell, Americans consumed roughly 56% carbs / 12% Protein / 32% Fat in 1909, and consumed even more carbohydrates during the 19th century.” You conclude your post with this: “Unless I missed something (entirely possible) Taubes seems to have skipped right over that part of American history. This ignored historical data implies that there is something else causing significant weight gain in Americans.”
First Duck, I agree with part of your last statement: “…there is something else causing significant weight gain …” I think there are other factors besides macronutrient balances that affect us. A big concern are the ubiquity of estrogenic hormone-disrupting compounds such as BPA and phthalates in so much of what we handle and consume. These days we are *constantly* exposed to them. More on these endocrine disruptors and other factors in another post. We’ll be busy enough covering the possible confounders here. Let’s start with “thin eating a high carb diet.” The closer you are to eating a subsistence diet, the less the macronutrient mix matters. The closer to a subsistence diet, the hungrier for calories your bod’s cell are, and so the less insulin it takes to admit those calories–be they from carbs or fats–into these maximally receptive cells meanwhile staying below the fat-storage threshold. Americans in 1889 did a lot more physical labor than today and food cost a much bigger part of the budget than the mere 11% it does today. Look how thin Chinese people were a few gens ago. Rural Chinese farmers ate mainly rice and greens yet stayed thin because they ate comparatively little and did lots of physical labor. As China grows more prosperous, obesity and diabetes there is taking off, and they still love to eat noodles and rice. Going back to the 19th cen, if you look at people of comfortable means who could regularly eat their fill, obesity WAS in fact a problem. Taubes starts GCBC with the example of William Banting who started a low-carb movement in England in the 1860s. This is well documented. Your questions and comments focus on America and this is in England. But the physiology is the same.
Duck, if we could somehow adjust for the subsistence diet confounder, would we find that Americans really *did* get fatter from 1889 to 1961? Might they have even gotten a little thinner? It’s possible. I don’t know as if we’ll ever know this for sure. I’ve never seen obesity rates for those years. Have you?
For the two AJCN reports, the data starts at 1889, missing all but the last 11 years of the 19th century. That’s important because we were well into the period of producing great surpluses of ever more refined flour and plenty of sugar. Here’s this from GCBC on pp 96–97: “It wasn’t until the mid 19th century that white flour became suitably inexpensive for popular consumption…sugar was also a luxury until the mid 19th century.” Other readings suggest that flour truly took off starting in 1875 when we saw a spate of process refinements over the next 25 years to the turn of the century and then “…mills after 1900 manufactured breakfast cereals and special pastry, cake, and pancake flours—some including leavening ingredients. Marketing specialists realized that the best way to sell flour was to make it easy to use. General Mills introduced “Bisquick” in 1930.” You can read about those here:
http://www.encyclopedia.com/topic/Flour_mills.aspx
http://www.angelfire.com/folk/molinologist/america.html
As for your statement “The high demand for white flours during the 19th century were said to be responsible for the dyspepsia epidemic.” Duck, do you have a link for the ‘”dyspepsia epidemic?” I could not find any such discrete event. But many of my search results found “Graham Bread” as the Dyspepsia Bread.” Graham bread is *not* a white bread but rather it’s made from non-sifted whole-wheat flour. https://en.wikipedia.org/wiki/Graham_bread. That only makes sense since this bran bread is high in fiber, roughly a fifth being indigestible cellulose: http://medical-dictionary.thefreedictionary.com/Wheat-bran. White flour has only a fraction of the fiber of whole wheat; see here the two entries in the USDA Nutrient Database:
http://ndb.nal.usda.gov/ndb/foods/show/6546 (white)
http://ndb.nal.usda.gov/ndb/foods/show/6543 (whole wheat)
As for sweeteners (sugar, molasses, honey, etc), Duck, again, I refer you to that table from Guyenet et al showing a *20-fold* increase in US sugar consumption since 1820 as refined cane and beet sugar production kept rising and becoming more affordable. Table 1 at that first link you supplied earlier (http://ajcn.nutrition.org/content/14/3/169.full.pdf) shows a similar pattern to Guyenet’s table: a dramatic increase in sugars (Antar et al call it “simple CHO”). The “complex carbs” (wheat, corn, flours, cereals, potatoes) appear to have steadily gone down in that time. Still Duck, to say that “American’s total carbohydrate consumption fell ~30% between 1889 to 1961” tells only part of the story at best, and may even be misleading. As a percentage of total calories, carb consumption fell less, only from 58% in 1909 to 48% in 1961. And that’s assuming these studies are even correct–they come with many caveats. These are not ward studies, but rather calculate macronutrient balances indirectly, using the food supply, and had to resort to different info sources, which those researchers may have used their own methodologies to collect their data. The data in the Antar study trends in eerily consistent straight line curves through the years, not at all what you’d expect during disruptive events like the Great Depression (1932) and WWII (1942–45), both times of rationing and food shortages which tend to favor carb-rich plant-sourced foods. Interestingly, the Antar studies disclosure includes: “This work is supported in part by grants from the Cereal Institute Inc…” Hardly a lack of conflict of interest!
The reason Graham bread was the “dyspepsia bread” is because Graham bread was the cure for dyspepsia. People weren’t getting enough fiber due to all the white flour that had become fashionable.
Rich obese people (like Henry VIII) ate significantly more meat and sugar than poor people. The peasant diet was mainly complex carbohydrates, dating back to Ancient times.
William Banting may have founded the low carb movement in the mid 1800s, but even Banting’s doctor didn’t believe that low carb was necessary for everyone. Dr. William Harvey stressed that Banting could have lost weight if he exercised more and ate less refined foods. Banting had an affinity for refined foods/sugar.
There really wasn’t much need for a Banting diet before refined sugars and flours entered the America diet. If there was, it would have been popularized much earlier.
“*20-fold* increase in US sugar consumption since 1820”
Sugar consumption? Or Sugar production?
My sources clearly showed that simple sugar was replacing complex carbohydrates. But simply looking at wholesale sugar production is misleading because most Westerners would have relied on local or backyard honey hives for their own sugar needs. For instance, In England in about AD 1350, honey cost approximately 7 pence per gallon (equivalent to 1.3 pence/kg), which is what the same volume of butter cost. (Rogers, 1866). This was much less than one would expect if it was a scarce and highly prized food item:
Mind you that people needed beeswax for all the candles they were burning before animal-fat candles became popular in the mid-1800s. Mead was also a very popular drink in the middle ages, leading up to the 17th century. It’s made by fermenting the final washings of honey from the comb in a solution with water.
Pointing to mollasses production, as some indicator that the American diet became sugar crazy, omits the fact that people have had access to their own local or backyard sugar production. This is the selective history I’m talking about.
“Rural Chinese farmers ate mainly rice and greens yet stayed thin because they ate comparatively little and did lots of physical labor…Americans in 1889 did a lot more physical labor than today.”
Offices are not new inventions. This line of thinking ignores the fact that sedentary occupations have been common for centuries (artisans, watchmakers, clergy, lawyers, scholars) and many Americans had slaves for their labor.
In the 19th century, one of the hallmark features of a sedentary life was a loss of appetite, particularly as people aged and could no longer do manual labor.
See: The Diseases of Sedentary and Advanced Life: A Work for Medical and Lay Readers (1885)
Incidentally, there is a strong correlation in the Western world between fortification of foods and obesity. Countries that fortify have significantly more obesity. As it turns out, before feed, rat chow, and carbs could be fortified, people and animals would lose their appetites when they ate refined grains, because the refined foods lacked the B vitamins that stimulate appetite. In fact, it was the appetite stimulating effect of B vitamins that led to their discovery by Osbourne and Mendel in the 1920s. Apparently the tastebuds crave the taste of B vitamins (this effect may be bypassed if you swallow B vitamin pills).
Once it was discovered, the ‘patent medicine’ industry quickly began to sell “ironized yeast” to encourage people to increase their appetites and gain weight. Most people were too thin and it was unpopular to be skinny and scrawny in the 1920s and 30s, as people wanted curves and vitamins were seen as the way to fatten up.
See: Ironized Yeast advertisements
By the 1950s, it was discovered that you could fatten animals with a combination of antibiotics and vitamins, and it could be done without much extra food intake. It only worked with a combination of antibiotics and vitamins. Just giving antibiotics or vitamins alone didn’t work. To this day, the combination is used to fatten animals.
France has a high rate of antibiotic abuse but their food isn’t fortified. This might explain why they have such a low obesity rate despite lots of refined flour. The B vitamins added to our refined grains are known appetite stimulants. It appears to be why food producers are so eager to add them to foods.
Without those fortificants, people would likely not have the voracious appetite for refined foods– the lack of vitmains (especially B vitamins) is supposed to result in a loss of appetite. It’s an innate and protective mechanism so that animals and humans do not gravitate towards nutritionless staples.
I doubt it’s a coincidence that the wholesale baking industry (not doctors) pushed to increase fortification in the 1970s along with the US Dietary Guidelines. It appears they figured out that they could sell more refined foods by adding appetite-stimulating vitamins to them.
It’s amazing nobody has noticed this. Everyone here talks about macronutrients, but nobody realizes that one of the macronutrients is now laced with appetite-stimulants, unlike in the 1800s when people lost their appetites. Banting loved beer and sugar. The beer was a good source of appetite-stimulating B vitamins.
Interesting stuff.
Duck Dodgers, wbryanh- Wow, you 2 have written “books”! All while I’ve been sleeping, then going to work- (I live in Europe, so I’m on a different schedule/writing plan from you probably). Hmmmm, where to begin? First off, when I said that Gary Taubes “delved into the history” in his book, what I meant was he wrote about the history of obesity research, not about every diet of every time period. I don’t see this as “selective writing”. His book is long and dense enough- (in fact, many people complain about this!)- it would be hard to include absolutely everything. And as far as I know, he never actually said that all people who eat a high carbohydrate diet automatically get fat; what he *did* say is that fatness is mostly caused by hormonal factors, and where obesity is found, it is generally found together with high carbohydrate diets- (i.e., not with hunter-gatherers who eat just meat and fat). Most of his book was a debunking of the “calories in, calories out” theory. In any case, according to the Weston A. Price Foundation, in the time period you were talking about, people did eat pretty many carbs- (this is confirmed by John Nicholson, though in England, in his book “The Meat Fix”). According to both sources, although people ate carbs, they also ate a lot of meat, fat, and offal, *and* they exercised a lot, many of them doing outdoor labor. When there is no metabolic syndrome, the appetite and energy expenditure regulates itself, and the body weight remains relatively constant.
In any case, during the 1800’s and early 1900’s, obesity and diabetes did exist, they were just more rare than they are now; the obesity epidemic as we know it hadn’t taken off yet. Around this time, many explorers noticed that hunter-gatherers in various parts of the world did not get diabetes, obesity, or other “diseases of civilization” that Westerners were getting- (appendicitis, gallstones, dental caries, constipation, diverticulitis, heart disease and cancer). Gary Taubes did write an extensive chapter about that (mentioning obesity and diabetes briefly, among all the other diseases listed). They also noticed that when these native people switched to a “Western” diet, these diseases started to crop up; some of them immediately, some of them took a generation or two, but there was always a distinct pattern. In this chapter, also, I would like to mention that he did speak quite a lot about “refined” versus “complex” carbs; partly because the theories of the day (Cleaves, Reaven)- were that the newer, refined carbohydrates were the main problem. But when Denis Burkitt- (not sure if I spelled it right) “discovered” fiber, these theories gave way to the general belief that disease/obesity is caused by lack of fiber rather than refined carbohydrate and sugar in the diet. (This fiber theory has never actually been proven, but it’s become a “fact” which people take for granted today). In any case, I was under the impression that Gary Taubes also implicated mainly refined carbs and sugar. (I know he’s currently working on a book about sugar, which should come out soon).
Duck Dodgers- I think your theory about B-vitamins is interesting; although I didn’t comment on it, I read your earlier posts on the subject. (Does it apply only to synthetic vitamins?) There could really be something in that, at least regarding Americans. The only thing is that I live in Europe, and the foods here are not fortified; however, I have seen first hand how obesity and diabetes is spreading like wildfire; quite sad, really. What I also see is that there are way more fast food places and sugary drinks, and people seem to be eating those things more.
Duck, again, I agree there are other factors beside dietary fat-carb balances driving our chronic disease and obesity. Likely many other factors, including environmental toxins (like the estrogenics I mentioned earlier), massive GI microbiome disruption due to routine use of antibiotics, massive external microbiome disruption due to antibiotic chemicals like triclosan impinged in everything from soaps to clothes, big changes to the gluten content of wheat since Norman Borlaug intensive selective breeding, and chronic disruptions of our circadian rhythms from working odd shifts and simply being able to stay up late due to cheap bright light. And yes Duck, for me that includes food fortification. These are just a few of the very many changes we’ve seen in our modern world, esp since 1945.
Still, these numerous other mitigating factors don’t necessarily exonerate HCLF. Just because many earlier peoples ate high-carb diets doesn’t mean they necessarily enjoyed better health than their LCHF peers. We can’t say that HCLF *didn’t* promote chronic disease like diabetes. We have too many unknowns. Until well into the 20th cen, acute conditions–deadly infections, workplace accidents, wars–killed way more people than chronic disease. In 1900 the average life span of an American male was 47 years. Plus, until recently chronic diseases were massively under-diagnosed. Diabetes is a terrific example. We didn’t have urine test strips till the ’40s, no glucometers until the early ’80s. Even today hundreds of millions of people unknowingly suffer from diabetes. Here’s a history of diabetes dx’ing: http://www.bjbs-online.org/pdf/pp83-93%20BJBS69(2).pdf
Duck, I do find issues with a lot of the evidence you present here. Before launching into all that, about “dyspepsia bread” you are quite right about it being used to help with dyspepsia! On that point I stand corrected. As far as people eating it to help with eating it to counter-effects of eating refined flour products, that could very well be the case–I just can’t say. I haven’t been able to find any history on it to support your claim. Do you have that link I asked for earlier? That’d be great, but if not, no worries, not gonna debate it.
About Henry VIII and Banting, yes, what you say appears to go along or at least not contradict what I said, when you bear in mind what I said about macronutrients mattering less when eating closer to a subsistence diet and doing more physical work. The passage you quote:
“(p.145) …In many villages the inhabitants live chiefly on potatoes and cider, and only eat meat occasionally in the course of the year, and yet in spite of this plentiful supply of “the means of respiration,” we seldom meet a “Banting figure” amongst them. It can easily, therefore, be understood why medical men have always earnestly recommended all corpulent people to take much exercise, to sleep little, and to undertake some mechanical labour.”
That is one man’s anecdotal observation, and his reporting is clearly not immune to error. These days I very much doubt we’d advise corpulent people to “… sleep little…” Could well be most of those villagers he observed did a lot of physical labor and ate closer to a subsistence diet, not necessarily due to lack of availability, but that a diet mainly of potatoes and cider is not very interesting. Not much “food reward” as Stephan Guyenet says.
As for what you say here: “There really wasn’t much need for a Banting diet before refined sugars and flours entered the America diet. If there was, it would have been popularized much earlier.” It’s easy to assert Duck, but we can’t know it for sure. It’s amazing how obtuse we can be for so long. Wealthy Romans drank out of lead goblets for 1500 years without realizing the lead drove their insanity. But again, I can readily believe that the increasing cheapness and availability of refined carbs drove matters to a crisis point.
About sugar consumption vs production and honey, Duck, can you seriously suggest that sugar (cane, honey, molasses, etc) pre-mid 19th cen was anywhere near as available as today’s sugar like HFCS, which you have to work to avoid?! What you say “In England in about AD 1350, honey cost approximately 7 pence per gallon (equivalent to 1.3 pence/kg), which is what the same volume of butter cost. (Rogers, 1866).” That may seem cheap, Duck, but 7 pence was an enormous amount of money in 1350. Per this site, a pound in 1350 had the spending power of nearly *7000* pounds today. Thus that gallon of honey today would cost 490 pounds! Butter has historically been expensive. So has beeswax. Per the wiki on it: https://en.wikipedia.org/wiki/Candle
“…Beeswax candles were expensive, and relatively few people could afford to burn them in their homes in medieval Europe…” Typically the candle-makers used animal fats.
As far as the link you posted: “Honey revisited : a reappraisal of honey in pre-industrial diets” the authors of this speculative study you cite (Allsop and Miller) are the first to admit its limitations: “…There are no precise figures for per capita [honey] consumption during most periods in history…” Even with all this, I’m ready to accept that for at least a few groups, honey may well have served as a main food source. Again, these groups likely did more physical work and ate closer to a subsistence diet. And again, their generally short life spans and lack of diagnostics prevent us from knowing if their HCLF diet promoted chronic disease or not.
Duck, about what you say here: “Offices are not new inventions. This line of thinking ignores the fact that sedentary occupations have been common for centuries (artisans, watchmakers, clergy, lawyers, scholars) and many Americans had slaves for their labor.” Duck, your line of thinking ignores the fact until relatively recently, a much greater part of the population *did* do a lot of physical labor. E.g. from https://en.wikipedia.org/wiki/Agriculture_in_the_United_States#History:
“In 1870, 70-80 percent of the US population was employed in agriculture.[15] As of 2008, less than 2 percent of the population is directly employed in agriculture.” And those few remaining farmers use many more “labor-saving devices” E.g. they replaced the ox-pulled hand plow with motorized tractors with air-conditioned cabs and cupholders for the 64oz Big Gulp sugar water.
About food fortification, it’s an area I want to research a lot more, and I appreciate all the links you posted on this! Duck, there’s so much to add to this discussion, including the common “more is merrier” mentality when it comes to micronutrients like Vitamin C and iron. Made worse by our RDAs which we determined in the 30s and 40s mainly through WAG (wild-ass guessing) Our need for these micros can vary hugely on specific conditions which is why we evolved to store many of the them, esp Vits A and B12, and to adapt to episodic shortages of them, e.g. potassium. More later Duck. Thanks for reading. –Bryan
I have to agree with wbryanh, that there is more to the obesity epidemic than B-vitamins and fortified food- (although I do find it an interesting concept and I think it may contribute). I finally had a look at that fortification link, and, though it’s interesting, it doesn’t explain everything. First off, it seems that the reasoning is that B-vitamins mainly stimulate appetite- (unless I missed something?) But that doesn’t explain why poor people who don’t have enough food and don’t eat lots of calories get fat. It has been documented that some Native American cultures who are very poor literally eat too little food. Though what they eat is mostly “industrial food”, white flours, sugars, government rations, they are eating too little, not overeating…..why do they get fat, or even obese?
Also, I’d like to give my own n=1, (and part of the reason why I’ve been interested in Gary Taubes’ work). Back when I was a young woman, I was anorexic for a few years. In an attempt to lose weight, I ate a low fat, mostly low-calorie but high carb diet. (This was back in the 80’s, when I didn’t know any better). I could not lose weight this way, so I reduced my diet lower and lower, to create a greater caloric deficit. During this time, I never ate more than 700 calories per day. Very often I would only eat something like 2 ears of corn for the whole day, or maybe 1 small container of blueberries, and that was it. All unrefined foods, and so few calories it couldn’t have been high in B-vitamins. And yet, I actually gained weight during this time! Luckily, I wasn’t anorexic for long, since it didn’t *work* anyway. And as soon as I started eating meat and fat again, and loads more calories, I lost the weight. At the time I just thought I was an anomaly, and that I was *weird*. However, when I read Good Calories, Bad Calories, I realized that something hormonal was going on with me- (it may not be like this for everyone). I personally think that in my case, it has something to do with eating fat. When I go too low fat, I tend to put on weight (the bad kind of weight too). With book titles like “Eat Fat, Lose Fat”, obviously some other people have noticed this phenomenon too.
A few more things: I live in Germany, and yes, the people do drink a lot of beer. However, they have traditionally drunk beer, but were not always fat; I have seen them progressively get fatter, but I don’t think they’re drinking more beer. In the Middle Ages people drank mainly beer, but there was no obesity epidemic then. Also, one of the observations that Weston Price made when he visited native cultures was that most of them ate far more vitamins and minerals than the people of his time; his main theory, aside from avoiding industrial foods, was to eat a “nutrient dense” diet. There was no obesity or diabetes among these groups (hence my question about “synthetic B-vitamins”). In the link, it was not specified that the B-vitamins only caused weight gain when they were synthetic; the implication was that generally too many vitamins, even from meat or vegetables, could be too much. (?)
wbryanh, you mentioned modern wheat as being a possible factor- (I definitely think it is!)- let me also mention that modern corn is not what it used to be either. It’s gotten much sweeter. Whereas it used to be a complex carbohydrate, it has now become quite high glycemic. (And in America corn is ubiquitous). In addition, soy is an endocrine disrupter, and soy, in this quantity, is a relatively recent addition to our diet. (Soy is also used to fatten animals). Also, in my lifetime, I’ve noticed that many fruits and vegetables have been bred to be sweeter. Some fruits that I remember as having a “complex” taste when I was young, I no longer like because they now taste cloyingly sweet. I absolutely think people are eating more refined sugar than ever before, because- not only have I read about it- but I’ve even observed it in my lifetime.
Hi Morgana! I haven’t dived into Duck’s fortification links yet, but will when I can carve out some more time. I suspect there’s a lot there, for reasons I wrote to Duck just now, about megacorps devising ways to drive us to eat ever more. About what you say here:
“poor people who don’t have enough food and don’t eat lots of calories get fat. It has been documented that some Native American cultures who are very poor literally eat too little food. Though what they eat is mostly “industrial food”, white flours, sugars, government rations, they are eating too little, not overeating…..why do they get fat, or even obese?”
I’d very much like to see the docs on it, because we simply can’t escape the basic thermodynamics. If we spend more energy than we take in, we have no choice but to lose weight! I suspect these kids don’t get enough healthy real whole food to eat, but WIC etc supplies them plenty of the the high refined carb and rancidifying omega-6-bomb veggie and legume oil loaded food-like substances. About you eating super-low-cal in the 80s, again, if you are taking in fewer cals than you burn then you simply have to lose weight, and you can down-regulate only so much and still be ambulatory :-). Maybe on your “cheat” days you ate more than you remember? But certainly your experience protein and fat and losing weight, that’s mine experience too, and I could stop cal-counting after a while.
About what you say here: “[The Germans] have traditionally drunk beer, but were not always fat; I have seen them progressively get fatter, but I don’t think they’re drinking more beer. In the Middle Ages people drank mainly beer, but there was no obesity epidemic then.” Morgana, they may not be drinking any more beer, but over the course of years, we can steadily become more insulin resistant forcing more the beer (and bread and pasta and other high carb foods) into adipose tissue.
About this you say: “the observations that Weston Price made when he visited native cultures was that most of them ate far more vitamins and minerals than the people of his time; his main theory, aside from avoiding industrial foods, was to eat a “nutrient dense” diet. There was no obesity or diabetes among these groups (hence my question about “synthetic B-vitamins”). In the link, it was not specified that the B-vitamins only caused weight gain when they were synthetic; the implication was that generally too many vitamins, even from meat or vegetables, could be too much. (?)” Morgana, vitamins we get from real foods may act much differently in/on us than the fortifying ones which can have novel formulation our bods don’t quite know how to deal with. In general, I have a tough time thinking that we need to carefully measure out the micronutrients we take in. Life just isn’t like that. Sometimes we’ll get loads of a given micronutrients, other times we won’t get it at all for a while. Thus our bods had to evolve ways to conserve, store and eliminate as needed. I certainly worry about micronutrient formulations like supplements and fortifications, and stopped ingest these in 2009.
About your corn comments, absolutely it’s gotten sweeter! I’m 55 and remember the solid super-starchy stuff from the 60s-70s you had to cook to eat. One day in the 90s, I decided on a whim to chomp into an ear and was amazed how good and sweet it tasted! About soy, I cut virtually all of it out, only eating organic locally produced non-GMO natto once in a while. Fermenting soy allegedly mitigates the estrogenic compounds (incl isoflavones) as well of course to reduce carbs. Definitely they’ve bred to make fruits sweeter and likely veggies, too, though no examples of those jump to mind at the moment (maybe some squashes?) About eating more refined sugar, how could we NOT be?! Truly we have to always work, to have our wits about us to not to take it in. E.g. Hebrew National Kielbasa dogs. In the supermarket, the Nutrition Facts panel shows they have no carbs, and indeed my BGs stay low when I eat those from the store. So one day I ordered the dog with the VERY SAME name at Costco’s food court (sans bun), and my BGs popped to 150. I went back to add to the court to get the bulk hot dog box, and learned from the label they jammed a load of HFCS into the dogs! That’s yet another example of where the food comps take every opportunity to sneakily press our evolutionary hot buttons to lead us to buy more of their junk. After all, it costs a fraction of a cent of HFCS to add a certain pleasant and enticing je ne sais quoi to the dog which may be enough to get you to plunk down $2 for another. You can NEVER win with these guys–except to leave the table entirely. Which I did. For years now, I almost never eat out, though I go out plenty with friends, but have only coffee/tea and that’s been working out super well.
wbryanh- Thanks for answering me. A few things:
1) I know I’ve read about poor people who become fat on an insufficient calorie diet. Gary Taubes mentions it in his book- (it may have been “Why We Get Fat”, not sure….”)- but I’ve read about it independently of Taubes. It was an American Indian tribe, (not the Pima, though they may have had the same problem). Possibly the Sioux. I would have to look up the link again, I don’t know where I saw it. I will do that as soon as I have time- (which is not today unfortunately, sorry….) Also, I saw a documentary a few years ago about Global Obesity, where they showed some very poor people, living at subsistence level who were obese. (The documentary might have been called “Globesity”?) They were eating crap, like soda, but they had too little food to eat. Basically, one of the problems with being poor is that- with little money to spend- they will often choose to spend it on cheap foods that will fill them up fast, like sugar, or starchy carbohydrates. I do not believe in the “law of thermodynamics” in regards to calories/fat burning. If you want to read a good book debunking the law of thermodynamics, I recommend Zoe Harcombe’s book, “The Obesity Epidemic”.
2) When I was anorexic, there were no “cheat days”; I was anorexic! A normal woman should consume between 1500 to 2000 calories, I believe; I cut mine down to 1000 calories (half), then, when that didn’t work, I went to about 700 on a “top” day- (on other days I ate even less than that. Also, one must keep in mind that I was exercising constantly). Anorexics control their calories to the point of obsession. And, I gained weight. I think it probably had partly to do with hormones; I was 21, probably the peak childbearing age, so I think my hormones might have been doing something crazy to compensate. Our bodies are not like a car that you fill up with gas, and then we have “fuel”; although our food does give us energy to burn, we also need the calories for certain processes within the body. When those calories are not forthcoming, the body will “ramp down” on certain processes- (whatever is “less important”), and the body will compensate in whatever way it needs to. (This certainly happened to me, in more ways than one). My theory is that people who eat too few calories may, in some cases, become extremely insulin resistant; almost like a bear in preparation for hibernation. (Animals that don’t have access to excessive food before winter will still gain weight- for instance, in captivity- if they are hibernating animals). Again, if you want to read about this concept of body processes versus low calorie diets, I recommend Zoe Harcombe’s book.
That doesn’t mean that reducing calories can’t help with weight loss; sometimes it does, sometimes it doesn’t. In any case, the hormonal aspect of fat gain- (not only insulin, that’s just one factor)- is also a very interesting subject, which I am still researching.
3) Yes, I do know that B-vitamins act very differently in the body when they are synthetic as opposed to when they are found naturally in foods. I was momentarily confused, because the link I had a look at also seemed to implicate diets that are high in meat, as well as the fact that presently, we eat more B-laden fruits and vegetables in the winter when traditionally these were unavailable. But Duck Dodgers straightened me out on that one, I think I understand the theory better now.
Finally, I meant to thank you for reminding me- (in another post of yours, on another subject)- that even lean people *can* fast, and that we have more fat preserves than we may realize. That’s true; and actually, I have absolutely no problem with 16 hour fasts, and don’t even have any blood pressure effects. So, yeah…..maybe I’ll give it a try sometime. In any case, wbryanh, I have enjoyed having a good “this and that” with you.
I kind of wonder if there isn’t a “hibernation switch” that gets thrown. If you look at omnivores like, say, bears … they are very thin when they get out of hibernation. They eat like mad, and get bigger again, but not obese. Come fall they overeat again, and they store a lot of fat, which gets them through the winter.
Now, during the winter you don’t want a lot of muscle … it’s expensive and eats calories. So to get ready for hibernation, you need to store fat … lots of fat.
In the fall, what bears eat tends to be a lot of fruit, and honey if they can. That’s when the fruit gets ripe and there is a lot of it. In the spring, there are grubs and fish (salmon!) and greens. I’m not sure where tubers fall in there. They are typically available all the time. Bears are also active in both fall and spring, gathering food.
But at any rate, it makes sense to me that there is some epigenetic switch that tells the bears when to make muscle and when to make fat. Possibly the “poor people food” of THIS era hits that switch, where the “poor people food” of a century ago did not. I’ve certainly known obese people that really don’t eat all that many calories, and then people that eat huge meals.
To find those foods though, might mean testing each food type individually?
Beer is an especially interesting case. Yes, it is full of B vitamins, and has been traditionally used to “fatten up” people. The monks that brewed beer were noted as being fat in the plays and stories of the time, and in fact when they look at the bones in abbeys … the monks that brewed beer were fat, while the ones that made say, brandy, were not.
One other thing about beer though, is *hops*. Hops are a narcotic and antibiotic in their own right, and in beer, it helps raise the ethanol content by suppressing the lactobacilli. But the hops also give you that nice “beer buzz”.
Through much of European history, both beer and cider were drunk throughout the day, in preference to water. Both have vitamin B and plenty of calories, though usually not so much in the way of sugars. The dead yeast are a calorie source too, in unfiltered beer? We don’t drink unfiltered beer much these days, but if you make homebrew there is a nice layer of yeast at the bottom of each bottle.
Queen Victoria was into her beer and also she was rather obese. She had a 50-inch waist.
“Give my people plenty of beer, good beer and cheap beer, and you will have no revolution among them” – Queen Victoria
heathertwist- Thanks for joining our conversation; you’ve posted some interesting ideas, which has given me “food for thought”. I like learning things I didn’t know about before.
Thanks! This blog has some of the most interesting and intelligent people that I’ve heard from in a long time.
Also, the dyspepsia epidemic of the 19th century was well known to be caused by eating too many refined foods. Again, the fiber-rich Graham bread was a cure for dyspepsia. John Harvey Kellog used fiber-rich cereals at his sanitarium to cure dyspepsia.
But the 19th century diet that became too high in refined flour was known to cause an interesting side effect. It resulted in constipation from lack of fiber, but it also caused a loss of appetite.
…and…
The second source goes on to explain that the appetite might change considerably depending on what was presented in the meal. Osbourned and Mendel showed the same thing in the 1920s, only they figured out that the appetite-stimulating factor was the B vitamins. This is why pellagra (a B vitamin deficiency) causes lack of appetite. So, we might deduce that Banting’s beer drinking is what stimulated his appetite. I wouldn’t be surprised if the obese Depression-era children were given yeast cakes (or yeasted breads) to stimulate their appetites. Yeast cakes were the main B vitamin supplements before B vitamin pills and wafers were created.
The effect is supposed to only happen when the subject is deficient in B vitamins, but obese people are now known to have micronutrient deficiencies. And, of course, people surviving on mainly white flour during the 19th century would have been deficient in B vitamins. So, it all makes sense in terms of appetite.
Today, companies fortify water with B vitamins (Vitamin water). It’s unlikely done for health purposes. More likely it’s done to stimulate the tastebuds. Tastebuds are well known to change with deficiencies. For instance, people who are deficient in copper or zinc do not taste the offending metallic taste of those aqueous minerals.
Hi Duck, thanks, looks like you can ignore my request for links in my post to you of 3 minutes ago 🙂
“Does it apply only to synthetic vitamins?”
The early literature on B vitamins suggests that the “reward” side of the appetite-stimulating effect is mainly about the vitamins hitting the tongue of deficient animals. If you swallow B vitamin pills (and you have good methylation) you might not crave the taste of B vitamins the same way because you might not be deficient. Animals will naturally gravitate towards B vitamin flavors when they start start to become deficient from eating nuritionless chow. They will tend to avoid the completely nutritionless foods as they become deficient. And they can “learn” about these tastes and create preferences for them (See Harris 1933, in my other comments). In other words, the animals can be “educated” to associate the taste of B vitamins with other flavors that are associated with them (i.e. you can remove the enrichments and the animals will still associate the flavor with those enrichments, even if the enrichments are removed). The “education” side of the equation might be equivalent to say, “dietary guidelines”.
“The only thing is that I live in Europe, and the foods here are not fortified; however, I have seen first hand how obesity and diabetes is spreading like wildfire; quite sad, really. What I also see is that there are way more fast food places and sugary drinks, and people seem to be eating those things more.”
Obviously sugar can be quite addictive, caloric and not very filling. But there are probably other ways for companies to stimulate appetites without techinical enrichments (besides sugar). Yeast extracts are a “taste” of B vitmains. Marmite, an enriched yeast extract, is known to stimulate appetite. It’s actually banned in Denmark because it contains enrichments. But, of course, drinking beer is a B-vitamin yeasty flavor, so that too should stimulate appetite with a meal. You get the idea. Just the yeasty umami flavor added to processed foods can stimulate appetite if the tastebuds are trying to guide us to obtain these vitamins.
A single slice of enriched bread is laced with as many stimulating vitamins as a medium sweet potato—and almost as many B vitamins as a cup of beans. The sweet potato and beans are far more filling than a slice of enriched bread.
Anyhow, all of these diet gurus, like Taubes, seem to have overlooked the main difference between refined carbs in the 19th and 20th century in American. Everyone focuses on just macronutrients, but that misses a big part of what happens to appetite when you eat truly unenriched and nutritonless foods as staples.
“Duck Dodgers- I think your theory about B-vitamins is interesting”
I wouldn’t call it my theory. Dr. Ss Zhou, et al. (from the studies I mentioned, above) is the one who figured it out. I just extrapolated his ideas into various points of history. It’s his theory though. You’d have to look at his studies to see the details and correlations, etc.
Ok. Everyone calm down. 🙂 I don’t think that fortification is the only factor in obesity. I never said that.
Obviously obesity is multi-factoral. However, I think that fortification is a majorly overlooked factor that everyone has been oblivious too. But, once you look at the correlations and the history, it becomes apparent that fortification in developed countries are now only done to sell more food. If the fortifications were not there, you would eventually lose your appetite trying to eat mainly refined foods—as what happened during the dyspepsia epidemic.
@wbryanh, I don’t think anything can ever “exonerate” any diet. 🙂 The way I see it is that grains, and wheat in particular, were always considered to be the healthiest foods from the days of Hippocrates right up until the 19th century. Hippocrates recommended wheat, barley and periodic bloodletting for good health. Bloodletting waned in the 19th century, but for all we know it may have been protective of some Western diseases like diabetes.
Borlaug wheat seems to be a distraction. Yes, it’s a sub-par wheat, but unfortified countries seem to do well on it. For instance, according to FAOSTAT, France consumes 40% more wheat, as food, than Americans do—and it’s unfortified. They produce predominantly semi-dwarf hard winter wheat. But the French have one of the lowest obesity levels in the developed world and very little Non-Celicac Gluten Sensitivity (good luck finding gluten free menus in France). So, while Borlaug is a poor specimen of wheat, it doesn’t seem to be deleterious for unfortified countries. 72% of Pakistan’s daily caloric intake per capita comes from unfortified wheat and they have one of the lowest obesity rates on the planet (5.5% in 2008). It would seem that unfortified Borlaug wheat does not cause obesity.
Anyhow, enough about that. I agree it’s all very complex and multi-factoral. Fortification is just one of many factors. We agree.
Here are my basic notes for when you decide to research this:
Zhou et al, found the correlations, but I have no idea if his theories on B vitamins are right or not. He seems to think that niacin overload is to blame. Apparently most researchers think that obese people have micronutrient deficiencies, but Zhou says obese people may be storing unmetabolized synthetic niacin. Either way, Zhou et al references that B vitamins like niacin are known to be appetite stimulants, but he doesn’t go into detail. I also found research that obese people are deficient in thiamin, but at the same time store lots of thiamin in their cells. (Don’t ask me what that means). Zhou also points out that obese people have high serum folate levels, which is indicative of unmetabolized folic acid from fortification. There is some research saying that high serum folate is associated with increased appetite. At any rate, obese people certainly have abnormal B vitamin metabolisms. It’s plausible that obese people are deficient in micronutrients (despite high serum of some B vitamins) which may make them crave the taste of B vitamins. Again, I have no idea if Zhou’s research is right or not, but his correlations are eye opening to say the least. To my mind, the appetite-stimulating effect is very interesting and could explain a lot about the paradoxical history of weight gain in the US.
Anyhow, Scientists during the 1920s knew that when animals are fed pure, nutritionless flours and refined grains as staples, the animals quickly lose their appetite and lose weight.
In other words, humans and animals have a natural tendency to become less hungry when fed deficient and nutritionless food. It’s an innate, protective mechanism to prevent the cravings of nutritionless staples. In the early 1920s, George Cowgill found that B vitamins could increase the appetites of mice, rats, pigeons and dogs. He coined term “appetite vitamin” for vitamin B1 (thiamine). Small amounts of dried brewer’s yeast (for B vitamins), were soon commonly added to the feeds of cattle.
The key thing to understand is that Thomas Osborne & Mendel discovered that they only needed to provide a taste via a “small daily dose” of B vitamins to stimulate appetite and make the rats gain their weight back. Osborne later said…
Soon “ironized yeast” was sold as an appetite stimulant. In addition to thiamin, riboflavin and niacin are now known to be appetite stimulants in deficient animals.
In 1933, Harris et al. published an exhaustive study observing the appetites of rats and vitamin-enriched foods. The experiments showed that rats deficient in B vitamins overwhemingly craved the taste of B vitamins, but could be “educated” to associate the vitamins with flavors.
Before WWII, bakers were mainly against enrichments because it made the product expensive and people were suspicious. It was the military that made enrichments commonplace by requiring their addition for War purchases during WWII. The enrichments were useful for soldiers who needed to survive on combat rations for weeks at a time (the Russians just used whole wheat with great success).
But somewhere after WWII, bakers—represented by the American Bakers Association—began to realize that enrichments would help them sell more flour. With carbohydrate consumption falling, they set out to raise enrichment levels. The first thing they did was get congress to pass the Vitamins and Minerals Amendments. The new law prevented the FDA from classifying excessive levels of vitamins or minerals as a drugs.
Next, in the mid-1970s the ABA convinced the FDA to triple iron enrichment levels. It was known as super-enrichment. William H. Crosby (the father of modern hematology) wrote two letters in JAMA expressing his outrage for the ABA’s move. Crosby wrote:
In 1981, the ABA finally succeeded in convincing the FDA to raise enrichment levels on flour to where they stand today. At the same time the ABA also lobbied the government to “educate” the US population to eat enriched grains via the Food Pyramid. Rice enrichment levels were not raised, however flour enrichment levels for iron and B vitamins were increased significantly. Thiamine was increased ~28% from the previous average range. Niacin was increased ~33% from the previous average range. And iron was increased by ~38 increase from the previous average range. The industry also expanded enriched flour into virtually all wholesale refined grain products. The total amount of iron compounds in the US food supply increased by 19-fold from 1970 to 1987. The FDA no longer has much control in regulating how much fortification goes into foods.
To this day, the ABA lobbies the government to promote enriched foods. Take a look at the ABA’s press releases and annual reports and you will see that they are firmly committed to lobbying enriched foods to the US dietary guidelines committee.
As far as I can tell, iron fortification is poorly absorbed and mainly just causes lots of inflammation in the gut. It’s not very good at solving anemia (they would have fortified with copper if they were trying to solve anemia). However, Progesterone receptor membrane component 1 (PGRMC1) as an iron binding protein in yeast which co-purifies with progesterone binding proteins in the liver and ovary. Makes me wonder if the adding free iron to yeasty dough results in something that would otherwise not happen with phytate-bound iron.
If I think of anything else, I’ll let you know. Thanks for listening!
(Again, I agree this is just one factor. Yes, obesity is multi-factoral, I know).
Duck, to correct the record, things are not so ducky in France. You say: “Borlaug wheat seems to be a distraction…the French have one of the lowest obesity levels in the developed world and very little Non-Celicac Gluten Sensitivity…”
Actually, France and the US have roughly the *same rates* of celiac disease, about 1% of the pop:
http://www.afdiag.fr/intolerance-au-gluten/la-maladie-coeliaque/
http://www.medscape.com/viewarticle/770529
The French link says: “One estimates that one person out of 100 can develop this disease in Europe. The prevalence seems to be identical in North America. In France only 10–20% of the cases to date are diagnosed.” (“On estime qu’une personne sur 100 peut développer cette maladie en Europe. La prévalence semble identique dans le continent nord-américain. En France, seulement 10 à 20% des cas seraient aujourd’hui diagnostiqués.)
About obesity, Duck it is relatively low in France as you say, but strong cultural eating norms–like no snacking ever between meals–may have been largely responsible for that suppression. As these norms have eroded since the 1990s, obesity begun to soar in France, doubling from 1995–2004. See here: https://en.wikipedia.org/wiki/Obesity_in_France
The same norms may have also suppressed rates of diabetes in the past, but it too, greatly increased in a decade, from 2.6 to 4.4% (“En 2000, le taux de prévalence du diabète était de 2,6%. En 2006, il était déjà à 3,95%. En 2009, il atteint les 4,4%”)
http://www.afd.asso.fr/diabete/chiffres-france#
Duck, you say “I don’t think anything can ever “exonerate” any diet. :)”
If you mean “no amount of meta-analyses, systematic reviews, RCTs, and cohort, case control, historical, anthropological, and molecular mechanistic modeling studies can exonerate any diet,” then I agree with you!
All those things above have great value. But our best option is for each of us to test each food- and lifeway on ourselves, tracking what we consume and do as carefully as feasible. To cut out of our lives as many modern complex products as possible, e.g. plastics, chemical-filled soaps, shampoos. And to get as many health measures as we can wheedle out of our docs and we can do at home.
Duck, thank you for getting me fired up about this fortification angle. At least one thing you said about it, that producers fortify in part to fire up our appetites, especially resonates with me. As Michael Pollan discussed, food producers went from being Mom and Pop shops serving their local communities, to huge multinational corporations beholden to their shareholders who always have the imperative to increase profits–a tall order when we should eat only so many calories each day. I will be diving down this rabbit hole as soon as time allows.
Another thing about “mom and pop” food … if you were say, Korean and living at a barely sustenance level, you would feed your kids food that kept them FED as long as possible. So you chose foods that kept them full and happy, whatever that was.
The modern food system is very opposite. You choose foods that let people overeat, so they buy more.
As Duck Dodgers has pointed out, the factors aren’t all that simple. For me I figure you have to adopt the entire cuisine … eat like a French person and see what happens. Eat like a Korean person. It’s more than just recipes … it’s about timing, food sources, additives, drinks (tea vs. coke?).
But I can say that well, a Korean or Japanese mountain person menu just makes you a lot more full for a lot longer than the typical American fare. I’ve never been able to pinpoint it to a macronutrient profile or set of allowed foods.
However, there ARE good studies that were done on say, chickens, which are also omnivores. I turns out that if you are growing chickens, you can have 3 food mixes. One makes fast-growing, very lean chickens. Second makes very fat fast-growing chickens. The third makes slow-growing lean chickens that don’t eat much.
The difference for chickens has to do with methionine. The methionine acts like a “stop eating” switch. If the food is too high in methionine, the chickens undereat and grow slowly, although they are healthy. If there is too little methionine, they overeat and get fat. If there is “just enough”, they grow fast but don’t get too fat.
So for people that get a lot of fish or eggs, they tend to have too much methionine? So they undereat? That doesn’t explain the Japanese yam-eaters though. I can tell you from experience that yams just plain fill you up (more so than a potato or bread, for sure).
Duck Dodgers- thanks for clarifying your position on the fortification issue! I guess I jumped to the conclusion that you were promoting that as the only/main cause to obesity; my mistake. I definitely find it interesting, and I definitely want to pursue it further, so thanks for giving information on what to look up. Frankly, I’ve been rather skeptical of fortified foods all along. And, yes, food companies will do all they can to get people to overeat; (adding sugar to food will have the same effect, which may be one reason why sugar is added to most processed food).
A.k.a. blood letting: the blood letting would have been a way to get rid of excess iron in the blood. Excess iron has been correlated with disease- (though, aside from the case of hemophiliacs, I’m not sure if it’s a correlation or causation). But this could have had an effect on health.
…and yes, the Pima were obviously eating lots more sugar and fat at the same time too. I just thought that the increased access to enriched flour was another “coincidence”, perhaps making them hungrier for all the other crap. Just thought it was interesting.
“Queen Victoria was into her beer and also she was rather obese. She had a 50-inch waist. ”
Great info there!
One thing I would point out is that the overwhelming majority of our B vitamins come from our microflora. Which means that someone eating fiber-rich complex carbohydrates should be feeding their microflora with enough fiber to avoid B vitamin deficiencies, particularly if their diet was sufficient in B vitamins.
But a queen eating lots of sugar and (white) flour and meat would likely have a B vitamin deficiency (particularly if obese) and in that case, the beer might stimulate appetite in her situation. And since she had access to unlimited food, she could satisfy that increased hunger.
At least in the 19th century, most peasants drank small beer all day, since the water was not safe to drink. Besides the fact that small beer is very weak, they probably didn’t have appetite stimulation if their guts were making sufficient B vitamins from all the fiber they were eating.
So, again, someone who has adequate B vitamin production in their gut should not have appetite stimulation from tasting B vitamins as far as I can tell.
Also, a poor person wouldn’t have access to unlimited food like a rich person would. So, even if they were actually hungrier, they just went hungry.
WBryanH said: “Actually, France and the US have roughly the *same rates* of celiac disease, about 1% of the pop:”
Oh, heh, I never said that France has less celiac than Americans do. I said they have less Non-Celiac Gluten Sensitivity. Gluten free options are extremely rare in France. I imagine that the inflammation from iron fortification makes it harder for Americans to digest gluten.
My reading on the subject is that virtually every country (with a few exceptions) has a ~1% celiac rate no matter what the diet is. The only reason why some countries have higher celiac is because it’s just diagnosed more in some countries.
True celiac is also believed to be rising all over the world, but nobody really knows why.
Anyhow, my point was mainly that the French (and Pakistan) eat far more Borlaug wheat but the non-celiacs there seem to have less problems digesting it. Here in the US everyone here thinks they have gluten sensitivity from Borlaug wheat. But, eat Borlaug wheat in France and somehow it’s not addictive nor as problematic. As I said, it’s extremely rare to find gluten free options in France. Yes, they have the same celiac rates, but not the so-called “sensitivity” we do.
Non Celiac Gluten Sensitivity is also believed by many to be a bogus disease. There’s no true biomarker for it. Not saying people aren’t sensitive to gluten, but the research is shifting to other potential causes (like ATIs or other gut inflammation). That’s why I think it’s curious that fortified countries seem to have gluten free options. In the US I think it’s a $10 billion industry. In France, nobody really cares much about it.
Not to mention the obvious, but they don’t add iron to bread in France.
Now, if you want to create a vaccine, what you do is to pair a protein (a bit of virus) with an irritant (adjuvant: like aluminum or iron). Then the immune system learns that the protein bit (the virus) is bad, because “obviously” it caused an irritation.
Frankly American baby formula and hamburger buns seem like custom-made vaccines to teach the immune system to hate casein and gliadin. Maybe not to the celiac level, but something like 30% of Americans have IgA antibodies to gliadin.
Celiacs actually have IgA immune factors to the tTG in bread. tTG also happens to hold your gut cells together, so an immune reaction to tTG is bad stuff … it means you attack your own gut cells and destroy the villi.
High IgA levels to gliadin… no one knows what that causes exactly. But disturbingly, the anti-gliadin IgA ends up in the blood, which means there is some gut permeability going on there too.
Now … I’m celiac. I get REALLY SICK off tiny bits of wheat. My family isn’t though. When I had to change my diet, I got depressed about the whole thing and stopped cooking with wheat just in self-defense. My family hardly noticed, and the deal was that they could eat anything they wanted when they went out. So my husband was happy to go out and get “real” pizza and my daughter would eat the birthday cupcakes happily. Both stopped though, because they said they made them “feel sick” compared to the similarly rich versions we made at home.
There could be multiple reasons for that. One might be just that I made them afraid of wheat. Although, this didn’t have any effect on them with dairy, which I also don’t eat. Other factors though:
— FODMAPS. Wheat is full of fructans, while rice flour etc. is not. Fructans are hard for some people to digest.
— Enrichment, bromine and other additives: white flour in this country is loaded with other stuff.
— Different breeds of wheat.
— Different cooking methods.
My daughter and husband routinely “cheat” when they go out and it’s difficult to find GF food. They often get ill as a result, though their “ill” is just a mild upset stomach. Anyway, my daughter did eat gluten-free when she was in France because she didn’t want to deal with the stress of an upset tummy. She would go into a restaurant, point to herself, and say “celiac”. The waiter would nod and they’d figure it out. It is way easier to be celiac in Europe than in the US.
What I’ve heard is that in Europe celiac is just a routine test (like we test for diabetes) so the people that have it know they have it. Maybe fewer people have the “minor” reactions to wheat because they didn’t grow up on iron-fortified baby foods.
Duck et al, this is a test post. Previous Reply efforts have apparently been failing.
Duck, again it’s wrong what you say: “…[The French] have less Non-Celiac Gluten Sensitivity [than the Americans.] First, sources estimate rates of Non-Celiac Gluten Sensitivity (NCGS) in the US and in France being roughly the same–up to 6%. Second, these can only be estimates because NCGS is notoriously difficult to diagnose. Which, interestingly, you DO allude to at the bottom of your post.
Those American and French links for NCGS:
https://en.wikipedia.org/wiki/Non-celiac_gluten_sensitivity
www dot topsante dot com
Weirdly, Rawfoodsos is weirdly not letting me post the full topsante link
Similar rates celiac and NCGS between the US and France only makes sense. Celiac disease is the frankest manifestation, the tip of the iceberg of gluten sensitivities if you go by what Dr Davis writes in Wheat Belly. And in your last post you do cite him for evidence. If celiac rates are similar in the US and in France, we should not be surprised to find the same for NCGS.
Duck, I’m not saying fortification plays no role. Like you, I believe it may play even a large role. What I am saying: You have no evidence to support your dismissal of Borlaug wheat strains to support your statement that “Borlaug wheat seems to be a distraction.“ It may be as you say. Or Borlaug wheat may play a very important role, as Dr Davis, Dr Perlmutter (author of Grain Brain) and many others assert. We simply don’t know either way. This can only be your opinion. So far you haven’t shown any real evidence to support it.
OK, this is the last of my of three-part comment. Sorry to break it up like this. These were originally one comment but Rawfoodsos was blocking *something* in the full comment. But the site wouldn’t tell me what, so had to guess at it.
Oh guys, I forgot to mention that Zhou believes that high meat consumption may contribute to the problems he describes, as meat is high in niacin (the B vitamin he focuses on most). In reality, you do see the correlations he mentions with countries that have high meat consumption and do not fortify. But, I agree it’s complex and I have no idea if he’s barking up the wrong tree or not. I only mention this because he does believe it’s possible to have the same end result from high meat consumption. I can’t quite follow his explanations, but I suppose it’s possible that someone with a compromised methylation cycle could end up storing (or not properly metabolizing) excess vitamins from a high meat diet. I really don’t know though.
B vitamins in food are supposedly only a minority of the B vitamins we get from our microflora. So, it’s possible that eating too much (muscle) meat results in some compromised B vitamin production due to lack of fiber. Just thought I’d mention it to clarify what Zhou said. Indeed, it’s complex.
As for the US government’s position on fortification, the US government does not require fortification. I believe individual states did at one time, but I think there may have been a court position that made it illegal to force fortification. So, the FDA’s position is that it’s “suggested” but not mandatory, and companies are free to create lots of fortified products, so long as they adhere to the suggested levels—even though fortifying virtually every product was not the original intention of fortification. The FDA has also said that widespread fortification is “not necessary” for the US.
So, it is possible to buy unfortified flour in the US (generally organic flour is unfortified these days) but the UK and Canadian governments do, in fact, require fortification for all white flour.
At the end of the day, what you see is that it’s the companies that want to fortify and add it to the Food Pyramid, and the government sort of goes along, maybe even reluctantly. The American Bakers Association leads a group of lobbyist groups known as the “Grain Chain” that continues to pressure the DGAC to promote enriched grains in the government’s MyPlate icon.
heathertwist said: “Maybe fewer people have the “minor” reactions to wheat because they didn’t grow up on iron-fortified baby foods.”
Yes, I had the exact same thought. Actually there are some who believe that autism may be a result of the enormous levels of iron in baby formula (note: not a reliable source).
Anyhow, I got in touch with one researcher about the high iron levels in baby formula and they wrote back:
That’s kinda scary.
I decided to look into this a bit further, and without much effort I came upon a pair of related papers.
Effect of iron on neonatal gut flora during the first week of life (1985)
Effect of iron on neonatal gut flora during the first three months of life (1985)
The studies concluded that compared to fortified cow-milk preparation, a low iron content in standard preparations of cow’s milk enhances resistance of the neonatal gut to colonization of pathogens.
There are also studies showing that high levels of iron in baby formula appears to have negative consequences on development.
What a mess.
And here everyone is worried about a little bit of mercury messing up gut flora …
Morgana said: “Though what they eat is mostly “industrial food”, white flours, sugars, government rations, they are eating too little, not overeating…..why do they get fat, or even obese?”
The Pima? While some got fat before enrichment (could be from any number of reasons, since we agree that obesity is multi-factoral), the health of virtually all Native American are well known to have deteriorated rapidly after the 1950s. In 1959, most Pima were still somewhat healthy eating lots of beans and lard-fried white-flour tortillas—part of their diet since the late 19th century when the government began giving them white flour as part of their rations. Hesse wrote in his paper, “The flour is almost exclusively of the non-enriched variety, and because it has a higher gluten content than enriched flour, it ‘makes better tortillas.’ Little enriched flour is sold at the trading posts.”
Within 10 years their health completely deteriorated. By 1971, the Pima had a very high prevalence of obesity and diabetes. The Pima were still eating their beans and lard-fried white flour tortillas, but they were now also indulging in soft drinks, enriched pastries, they were more sedentary, and they were eating considerably more enriched flour.
Morgana said: “I live in Germany…I have seen them progressively get fatter, but I don’t think they’re drinking more beer.”
Could be from any number of reasons. Nobody ever said that fortification or B vitamins are the only reason.
Morgana said: “In the Middle Ages people drank mainly beer, but there was no obesity epidemic then.”
Yes, though they would have been eating complex carbohydrates, which tend to have bitter tannins and fiber that are satiating signals. If we say beer is an appetite stimulant, then it’s probably mainly problematic if it entices you eat lots of sugar and white flour.
Morgana said: “Also, one of the observations that Weston Price made when he visited native cultures was that most of them ate far more vitamins and minerals than the people of his time; his main theory, aside from avoiding industrial foods, was to eat a “nutrient dense” diet. There was no obesity or diabetes among these groups (hence my question about “synthetic B-vitamins”).”
As I said, the appetite-stimulating effect is only true if the person is deficient in B vitamins (or, say, has abnormal B vitamin metabolism as Zhou suggests).
Morgana said: “In the link, it was not specified that the B-vitamins only caused weight gain when they were synthetic; the implication was that generally too many vitamins, even from meat or vegetables, could be too much. (?)”
I actually wrote Zhou and he did think that synthetic B vitamins are very problematic for some people. For instance, not everyone has the enzymes to metabolize (synthetic) folic acid. So, they build up unmetabolized folic acid in the body and the serum levels rise, even though the person is deficient (since they cannot use the folic acid well). I believe Zhou would call this “overload” even though the person is technically deficient.
I do not think you could easily get B vitamin overload from real foods. B vitamins from real foods are easily excreted. But the synthetic B vitamins are not easily excreted in some situations (like folic acid for instance). I believe Zhou thinks that synthetic niacin is particularly problematic.
To my mind, Zhou may have made some mistakes as he dives into the complexity. But, I think he was on to something when he pointed out the correlations and the possibility for appetite-stimulation.
At the very least, fortification makes it so that people can survive on nutritionless foods. If the fortification were not there, most people would lose their appetites eating nothing but pure white flour (as we saw with dyspepsia and Osbourne & Mendels rats and many other studies). On the other hand, I did see one study that rats deficient in thiamine may still crave sugar and fat, but still lose weight as their appetite diminishes.
And as I said wbryanh this is fine if you’re writing a fictional romantic history about nutrition. But we’re talking about the construction of GT’s carb insulin assertion. If this were scientific writing the assertion would be on page one in the abstract, FOLLOWED by the 200 pages of defense.
@morgana, no, GT does not say in the NY Mag article that everyone gains weight if they exercise. But he doesn’t cite examples of people who have lost or maintained weight. He’s biased the article by doing that. Do you understand that the article was written to be read in 5 minutes by someone waiting for a bus, not someone who would spent 12 hours deconstructing it on a blog? The immediate impression GT makes is that exercise is futile, and he says this in a judgemental and assertive manner.
It shows tremendous bias to cling to GCBC the way you (and wbryanh) do. If you cite that book, please cross reference the position of Ancel Taubes and other nutritionists and physiologists. Answer arguments with more than prooftexting and precisionism! Don’t presume that the rest of the world knows or cares about the GCBC chapter on exercise, or the section on the Pimas, etc etc etc!
thhq- I don’t think I’m unduly biased towards Taubes; the problem is, you’ve criticized things that he’s supposedly said, but I can’t find any evidence that he’s even said those things. Basically, I don’t really know to what you are referring…..the link you sent me was a New York Times article on salt, and I saw nothing in there about exercise or weight gain. And I can’t find any “chapter on exercise” in Good Calories, Bad Calories either; I looked at the table of contents today, and there was nothing- (unless there are a few words about exercise in one of the other chapters).
Basically, my stance on diet is pretty much where Denise Minger stands; it does appear that different diets seem to work for different people. I would never criticize someone for the way that they’ve chosen to eat. However, when people criticize low carb diets, I feel the need to defend them; partly because this way of eating works really well for me, mostly because there is enough slander and bad press about them anyway (mostly wrong, I may hasten to add). Likewise, if I feel that someone like Gary Taubes or Atkins is being misrepresented, I feel the need to defend them, for the truth. If I appeared dogmatic, I apologize. But I did read Good Calories, Bad Calories, so I know what Gary Taubes did and didn’t say. I see online bloggers constantly misrepresenting him, and this bothers me, partly because people tend to repeat what they’ve heard (even if they didn’t get it from the source).
In any case, I’m glad you lost weight and became healthy by exercising. This is truly great! Since this very positive thing has happened to you, why should you even care what Gary Taubes thinks of it? I say- (in a positive, non-criticizing way)- maybe just “let it go”?
I’ll leave you with this Morgana. If you haven’t read Dixon’s series on Keys you may find this interesting.
If GT, Eades, Sisson or anyone else in the HFLC community has done this kind of respectful discussion of the greatest 20th century nutritionist give me the links. This man’s association with George McGovern and the food pyramid is unfortunate, he does not deserve to be mocked and pilloried. Why did he live to be 100? That is the question to be answered.
In “Why We Get Fat”, Taubes explains that there’s little scientific evidence that exercise is a significant factor in weight loss. He does say that there are many health benefits to exercise, though.
As with anything, people respond differently to exercise. Since reading what Taubes wrote, whenever someone tells me that he lost weight through exercise, I ask further questions.
When someone starts an exercise program, I thind that the person changes other variables too. Usually they are changing their diet, meal schedule, cutting back on beer consumption, and sleeping more.
I’m guessing that when scientists are studying this in the clinic they have a control group and for the exercise group they are not changing a lot of different factors along with the introduction of exercise.
As well as mct oils
Fish oil and mcts seem to prevent fat induced insulin resistance tho….
Where is part 2? Thanks.
Denise, have you ever explored the notion of cellular/acellular fats (like it’s popular to do with carbs these days) in a carby meal? Aka, the difference between eating a bunch of walnuts vs the same amount of fat from an oil. The different digestion speed and pattern might very well create a scenario where there’s very little ffa released into the blood at any given time, thereby annulling the effect typically seen in research with starch+oil.
This is a test post
Groundbreaking work, Denise! Just mind-melting…
Noticed two typos:
*Of course, we humans are wont to err
*diet consisted of unprocessed natural food with no supplements, e.g. guar
Cheers! Looking forward to part 2!
I’m starting to get confused. . . Maybe that’s the point. So this is the girl that “debunked” the China Study? She seems to not know what she believes or thinks as she is constantly changing. It looks to me that she likes to be the rebel, the outlier, different to whatever group she happens to be in. At a young age, she decides to become a vegetarian, not for ethical motivations she says . . . So the reason is unclear. Then I guess when vegetarianism was too “normal” for her she decides to become raw 100% plant-based. This is when all her health problems started. She would have to be doing something pretty extreme for all her hair to fall out and teeth to be rotting in her mouth. Then she decides to write a critique on the China Study and join the paleo, low carb movement. Now that she is part of the paleo movement she now wants to come out and say “Hang on! I’ve just discovered all this information on the health benefits of a low fat, high carb diet!”
What shocks me is that she had not read earlier about all the scientific literature that supports a low fat, high carb diet. She could have read about it when she was vegetarian or when she was a raw foodist or in the very least when she decided to argue against the works on Dr Colin Campbell, Neal Barnard, John Macdougall etc. However, it looks like she is only discovering this information now. So basically my point is, while this girl chops and changes and goes from one diet to the next and one belief system to the next and writes lengthy blogs about each change . . . Millions of people are on a whole foods plant-based diet and are thriving . . . For years . . . She criticizes Colin Campbell for fudging his data to get the results he wants. However I think I prefer to follow the advice of a man who has 60 years experience in the field and has followed what he preaches for over 40 years, is fit and healthy today (in his 80s?) and is free of cancer, heart disease, diabetes, Alzheimer’s, arthritis etc. His children also follow a whole foods plant-based and so do his grandchildren! I’ve been on a whole foods plant-based diet for 6 years and I have had one cold in all that time when I was pregnant, apart from that I’ve been fit and healthy, had a great pregnancy and have since nursed my child for 11 months (who has never been sick). So I’m not sure what Denise Minger did that was so extreme that made her hair fall out and subsequently make her believe that carbs are bad and lots of meat and fat are good . . . But I will not be following her advice . . . on anything. Ordinarily I don’t mind if people disagree with a plant-based diet but people actually refer to this unstable girl as “evidence” that the China Study has been debunked.
Lily, you may genuinely and ardently feel you follow the right foodway for you. Millions feel the same way about grain-free LCHF. But your gratuitous put-downs e.g. “this unstable girl” are uncool and work against your message. That’s even before I clued into your logic fails and your apparent ignorance of Denise Minger’s remarkably well elucidated arc of her journey, her evolving dietary positions. Highly educated researchers also take serious issue with The China Study. e.g this: http://www.cholesterol-and-health.com/China-Study.html from Chris Masterjohn PhD. T. Colin Campbell fails to deliver a satisfactory defense, as Chris Kresser discusses here (http://chriskresser.com/rest-in-peace-china-study):
“Campbell’s response to previous critics of the China Study has been something to the effect of: “I’m a trained scientist. Therefore you should believe me and not my critics.” That is a weak argument – to put it mildly. You don’t need six years of graduate school to learn to think critically. Nor does having a lot of letters after your name make you immune to biased thinking or intellectual blindness. A lot of smart, educated people believed the cholesterol hypothesis for decades. But that never made it true.””
I’m on a similar track @Lily, and I’ll look into Colin Campbell. I don’t think either of the extremes -below 15% fat or below 15% carbs – is the best way to go for healthy longevity, though either of those diets works fairly well if they are not over or under eaten. I’d recommend reading Eat Well and Stay Well by Ancel and Margaret Keys if you can find a copy.
There are lots of ways to live a healthy hundred years, from Paleo to vegetarian, but there are a lot more ways to barely make it to a sick seventy. It’s not rocket science. Don’t pay attention to the picky precisionists who will say that you are an idiot because you are not a devoted acolyte of Taubes, Atkins, Sisson, Eades, Pritikin, Keys, McGovern, etc. etc. etc. It’s your health and you have to figure it out for yourself.
The five minute read leaves me with the impression that Campbell is another persona in search of acolytes and book sales. I give Denise Minger a lot of credit for looking at the broad scope of diets rather than taking the single rifle shot.
My dad made it to 88 on cookies, tuna sandwiches, pancakes, scrambled eggs, bacon and canned pears. Ancel Keys made it to 100 drinking wine, eating pasta and bread, seafood, fruit and lots of olive oil. My diet doesn’t need to be anymore complicated than those. What I do with my life between meals is what makes the difference between being healthy and unhealthy.
Bit off topic here. But whilst Denise was criticizing the China Study, (Which I personally haven’t read), she was also knee deep in nonsense and delusion during that time. She was referencing and recommending Anthony Colpo and Malcolm Kendrick. That’s right, Dr Malcomn Kendrick, the author of “The Great Cholesterol Con”. I actually read that book when I was into the Paleo/Cholesterol denialism ideology. Re-reading that book 6 years later I feel like I was seriously deluded because of my preference for certain food products.
I seriously hope Denise stops calling her a scientific blogger and seperaters herself from these Paleo pseudoscientist. It might be hard considering she occasionally gets paid by Sisson to write low carb defending blogs and even had a book published by this supplement salesmen “paleo” guru, but I think if she was honest she would separate herself from all of those hucksters.
Come on Denise. You were able to separate yourself from the crazy raw food crowd, I think you are able to separate yourself from the “paleo” crowd.
Duck/Bryan,
I did some ketosis reading to learn more and to refresh my memory, so I have a few points and questions to add to this discussion.
1. Duck, after all the reading, I agree with you, inuits were not in ketosis, according to our traditional definition of it. So we can’t really use them as a poster child for ketosis.
2. May be inuits are “better” at burning fat then us, that’s why they are adapted to produce much less ketones as a byproduct of their FFA metabolism? Inuits may well have evolved a mechanism to promote FA metabolism over ketones.
3. Duck, I don’t think inuits have difficulty fasting, their children may, but not adults. And Peter has a theory that it has to do with omega-3 metabolism, which they have a lot in their diet and which the CPT1a evolved to deal with.
http://high-fat-nutrition.blogspot.com/2014/11/the-p479l-gene-for-cpt-1a-and-fatty.html?m=1
4. Chronic cold exposure depletes glucose/raises FFA, so this mutation is an adaptation to Inuits’ cold surroundings and has to do with using UCP for free heat. There is more from Peter here:
http://high-fat-nutrition.blogspot.com/2014/11/coconuts-and-cornstarch-in-arctic.html
5. Another interesting point that has been touched upon here is how do we define ketogenic diet and if the level of ketones in the blood even matters. I like Peter’s definition from the link above: “ a ketogenic diet is essentially a fatty acid based diet with minimal glucose excursions and maximal beta oxidation. Exactly how important the ketones themselves are is not quite so clear cut.”
6. So yes, as Bryan said, can we thrive long term on persistent LCHF? Even VLC? Besides possible liver issues (that can be tested using AST, ALT, ALP), or thyroid issue (which I”m not concerned about either) are there any other known concerns/issues with VLC dieters who feel well on it?
7. I have an issue with medical tests, most of the reference ranges are based on people eating a “normal’ HC diet, not LCHF, so how useful are these tests? Besides, may be there are some things we are not even testing for? Basically, what is that we don’t know yet and how do we decide what’s best in this incomplete information environment? Can we go on how we feel and look 🙂 ?
8. I think fasting insulin so far is one of the best markers that correlate with longevity in population studies.
Anna, you are correct. The adults can definitely fast. However, typically the children cannot safely fast.
Additionally, the Inuit have always been known to snack constantly throughout the day, as first reported by Franklin in 1845.
The Alaska Dispatch News article I mentioned earlier states:.
Most adults can fast pretty well when they need to, but it sounds like their fasting doesn’t mix well with strenuous exercise.
Heinbecker showed that (rested) Eskimos could certainly fast in his studies during the early 1930s, but they struggles to make ketones. Perhaps they were just drawing down on fat stores. Only his fasting pregnant/lactating women were really able to produce ketones, but pregnant women are known to have exaggerated ketone production and Heinbecker’s subjects were well below what we would expect from pregnant women. His pregnant/lactating subjects weren’t ketoadapted because he said that due to their employment they were accustomed to eating a carby Western diet.
Anyhow, you get the idea. They have to be careful when they fast and they prefer to snack all the time.
A friend of a friend of mine got a license to kill a muskox in Alaska several years ago. He flew out to Nunivak, got in touch with his Eskimo guides and went out in a boat to go find the muskox.
He said that as they were riding this boat in rough seas, the Eskimo guides started pointing to the shore excitedly. They pulled into a little cove, jumped out of the boat, and started eating from a tub of cream cheese mixed with salmon. Then they used a small gas stove to make some tea. After a short bit they jumped in the boat and continued on.
His friend said that during the several days they were hunting for muskox, this same scene played out several times a day. He was perturbed, because even if they were getting close to muskox, the guides would drop everything and take a cheese and tea break. His interpretation was that the Eskimo Hunting Guide Union had strict rules about ‘break-time’ and these guides were just taking advantage of it. But they were probably just hungry. lol 🙂
Duck, may be they eat to warm up, not because they are “hungry”. It takes a lot of energy to generate heat there…
But either way, I doubt they have difficulty fasting any more then us. They should be even more adapted to survive the fasting, given the conditions they live in, especially if they indeed have a bigger liver, as you are saying, they can store more fuel.
Anna, I’ve had a chance to look more at your post. Honestly it’s one of the better ones I’ve seen recently. It does more to further the Inuit discussion than anything else I’ve seen here to date. Possibly even settle it for the purposes of non-Inuit contemplating a LCHF foodway.
Hyperlipid Peter sums it up esp well: “…Confirming that the Inuit are not poster boys for ketosis is a “so what?” moment for me. Using their P479L (i.e. for CPT1a deficiency) mutation to argue against ketogenic diets is more of a problem. It’s a massive dis-service to any one of the many, many people out there who are eating their way into metabolic syndrome to suggest that a ketogenic diet is a Bad Thing…”
Anna, I address your points here:
1) “…inuits were not in ketosis, according to our traditional definition of it. So we can’t really use them as a poster child for ketosis…” Anna, ketosis appears to mean different things to different people and we have no agreed def for it. I’m willing to accept the idea that Inuit aren’t drawing the bulk of their kcals from ketones. More like ketones + FFAs.
2) “…Inuits may well have evolved a mechanism to promote FA metabolism over ketones.” Anna: Agreed. We often say “ketotic” and “glycolytic.” But I hardly ever hear “lipolytic.” The CPT1a deficiency variant may have been allowed spread due to lack of selective pressure, having nothing to do with purported liver damage from extra fat load. Maybe the selective pressure was greater for the Inuit to quickly get FFAs from white adipose tissue directly to thermogenic tissue like brown adipose tissue. Greater than the downside of maybe having to freq feed their children.
3) “…I don’t think inuits have difficulty fasting, their children may, but not adults. And Peter has a theory that it has to do with omega-3 metabolism, which they have a lot in their diet and which the CPT1a evolved to deal with.” Anna, I also haven’t heard of fasting issues in Inuit adults, and would like to learn how they adapt to fasting as Inuit grow older. Given their huge and harsh environment and often subsistence diet, it’s very hard to imagine the Inuit are always snacking all the time. It’s likely there were plenty of times they had to go hours or even days without eating anything. Peter’s comment I will (as usual with him) have to spend more time with it, but these comments jumped out to me: “…while systemic ketones are a useful adjunct, a ketogenic diet is essentially a fatty acid based diet with minimal glucose excursions and maximal beta oxidation. Exactly how important the ketones themselves are is not quite so clear cut…”
4) “Chronic cold exposure depletes glucose/raises FFA, so this mutation is an adaptation to Inuits’ cold surroundings and has to do with using UCP for free heat…” Anna: Yup. Like like my example in 2)
5) “a ketogenic diet is essentially a fatty acid based diet with minimal glucose excursions and maximal beta oxidation. Exactly how important the ketones themselves are is not quite so clear cut.” Anna: Again, yup.
6) “…can we thrive long term on persistent LCHF? Even VLC? Besides possible liver issues …or thyroid issue … are there any other known concerns/issues with VLC dieters who feel well on it? Anna, I haven’t heard of other issues beyond what you list, and would really like to.
7) “I have an issue with medical tests, most of the reference ranges are based on people eating a “normal’ HC diet, not LCHF, so how useful are these tests? Besides, may be there are some things we are not even testing for? …Can we go on how we feel and look…” Anna: Yes, I also have plenty of issues with the current state clinical health measures, as I discuss elsewhere in this forum. We shouldn’t rely much on any single health measure but interpret them in their totality with an eye for mitigating factors. Even a lot of doctors fail to do in this age of push-button medicine, e.g. “Got high LDL? Take this statin.” I agree we have to look at as many factors as feasible–including how we feel and look as you note Anna. Together, tests + qualitative personal observation further our individual health states way more than the vast body of research–even peer-reviewed-“science” out there that people can sling at each other till the cows come home. Best of all is to look at all three things: research, clinical health tests and qualitative personal observations (e.g. “how do I feel?”)
8) “I think fasting insulin so far is one of the best markers that correlate with longevity in population studies. Anna, that is my sense too, and I’m looking forward to when we will develop a home test for serum insulin that’s as cheap easy and reliable as checking blood glucose. There’s plenty of evidence to suggest that chronically elevated insulin can further metabolic syndrome and lead to a host of pathologies, including Alzheimer’s disease. –Bryan
Reblogged this on SENSIBLE PARTICULARS and commented:
I love reading intelligent women. And I love nutritional research. Party party y’all.
Thanks Denise. You are the nerd -brain that I have longed for to help make sense of these different dietary camps and their successes and differencss. I have read about the Natural Hygiene fruit – greens high carb low fat diet, the Esselstyn diet, the anti Arthritis plant based diet, and the Terry Wahls diet and similar ketogenic diet, and various animal food – loving tooth healing diets. I found them all convincing and although I’m currently doing a tooth healing diet high in fat and meat, I mostly have lived in the Swampland (probably still am in it actually), confused by the different camps. I have also thought there must be some special magic on either end of the fat – carb spectrum. Thanks for detailing and elaborating on it in a way that I have no time for and making entertaining to boot! You are on my A-list!!
Guys I finally got my hands on the 1940 Bertelsen report on Inuit CVD that vegans like McDougall and Inuit diet debunkers love to cite. Newsflash: It doesn’t debunk any diet-health hypotheses for ancestrally living Inuit. It doesn’t confirm or debunk anything. It’s a short interesting read. But it’s little more than anecdotal.
I put it up for you in the original Danish and in English from Google Translate. The translation’s kinda rough but gets the points across. Check it out:
http://www.adventuresinnonfiction.com/monographs-on-greenland.html
I wouldn’t try to compare Bertelsen’s 1940 report with Bang and Dyerberg’s more detailed work with ancestrally living Inuit in far Northern Greenland. That’d be like comparing a mystery fruit basket with slightly punky oranges. Interestingly, Bertelsen gives evidence for low CVD in northern Inuit from just a few decades earlier: “…Hastrup express[es in] 1886: “I have not even seen or anywhere found already mentioned cases of heart disease in North Greenland between Greenlanders,” [and] Kiær [in] 1900 declares not to have seen cases of Mb. cordis [mitral heart disease] in Northern Greenland…” It’s likely many of these remote far north Inuit led a more ancestral lifestyle than those down south in settlements.
Page 102 starts the section on heart disease (Endocarditis, Myocarditis, Pericarditis), It makes clear heart disease was essentially unknown there as recently as 1900, but that the modern world, even in the 1930s, had come to many Greenland Inuit. That included an increase in infectious disease, some of which drives heart disease. We learned little about these subject Inuit’s lifestyles and nothing about what they ate.
Bertelsen addresses arteriosclerosis starting on page 104. He based his observations on the Inuit and mixed “Inuit-Aryan” who came to his office for his medical services. His self-selecting “cohort” was sick from the get-go. Bertelsen admits his observations are his opinions, and says at least twice that he did not methodically test for arteriosclerosis. Bertelsen doesn’t say where he examined these people or where any of them come from. He tells us almost nothing about his subjects’ diet and lifestyle, except to suggest they are influenced by modern ways: “…greatly increased connection with the outside world and by the associated higher frequency of imported Infectious diseases are conditions for the genesis of heart disease significantly increased…” That matters because even in the 1930s Inuit living in the many Greenland communities with Danish trade outlets were eating lots of SAD like flour and sugar, and also drinking and smoking. As for the exam, for arteriosclerosis, the only consistent medical measure he discusses is blood pressure. He even discusses how a patient looks to contribute to his largely informal diagnoses. That person looks older than his years–must be sclerosis. Finally Bertelsen cites observations from other researchers, doing their studies at the same time, that contradict his own:
“…Thomas almost simultaneously studied 142 Greenland Eskimos between 40 and 60 years and found blood pressure of these average 129/76 mm with a single maximum Fund of 170/100. He declared then that Hypertension and related complications are extremely rare in Eskimos despite their pronounced meat and fat diet….”
Given near no rigor, why did certain folks latch onto Bertelson’s 1940 disease report like it was a definitive study? For vegan God John McDougall, who pompously calls Dr. Bertelsen “…the father of Greenland epidemiology.” the reason is obvious: Any strike, real or imagined, against the high meat diet is a score for the vegans. For Dr George Fodor, who helmed last year’s meta-study that fueled a backlash against the “Inuit diet” and the Omega-3 fish oil cap “craze,”
““Fishing” for the origins of the “Eskimos and heart disease” story. Facts or wishful thinking? http://ottawa.ctvnews.ca/polopoly_fs/1.1814937!/httpFile/file.pdf
his motivations are less clear. However we can look to Fodor’s long-standing financial ties to Big Pharma for ideas. The more health people find through diet, the less they need to buy statins from Pzifer, Merck, and the like.
I’m guessing some folks didn’t bother to read more than the English summary, which says on page 215: “Arteriosclerosis and myocardial degeneration are common, and heart disease a not uncommon cause of death, specially among the oldest age groups.”
And it’s true that’s pretty much what Bertelsen concludes in his Danish-language summary:
“Arteriosclerosis and myocardial degeneration are common in the Greenlandic population, and Heart disease is not a rare cause of death.” Why does Bertelsen say that? What compelled him to conclude with such apparent sweeping conviction, so clearly beyond his very limited and self-selected biased evidence to ascertain this claim for Inuit across all of Greenland, and which is even at odds with some of his contemporary researchers he cited? Bertelsen made abundantly clear he lacked controls and parameters; that he based this report primarily on him seeing a stream of patients. Again, hard to know why he made this apparent contradiction, but his times may give answers. Bertelsen wrote and his report during wartime Europe when Germany had just invaded (or about to invade) Denmark. It’s not likely Bertelsen got much or any funding from the government. We should look to his private sponsor, the P.Carl Petersen Fund (Udgivet Med Støtte Af P. Carl Petersen’s Fond). P. Carl Petersen was a merchant who became a coffee magnate, so it’s not immediately clear to me what vested interests influenced Bertelsen. Further digging here may turn up clear motivations. It would not be the first time we saw a researcher strike a quasi-Faustian bargain with his benefactor.
Out of all this, I’m most disappointed by Dr Fodor, a well-respected figure in Canadian cardiology. For whatever mysterious reasons, Fodor wasted an opportunity to show the world that ancestrally-living Inuit really *do* appear to have much reduced CVD and that fish oil caps don’t seem to work. Instead, curiously, Fodor stuck to a much more narrow focus: he seemed mainly intent to discredit Bang and Dyerberg’s work. Fodor glaringly omitted obvious trends in his own data that clearly point to significantly lower CAD in Inuit eating ancestrally and not eating SAD, and he practiced inconsistent, even shoddy scholarship. E.g. Fodor criticizes Bang and Dyerberg for relying on death certificates of questionable validity here:
“Bang and Dyerberg’s acceptance of the low incidence of myocardial infarction (MI) relied on the reports of the CMO in Greenland for 1963-1967 and 1973-1976. These reports are based on death certificates and hospital admissions. Concerns over the validity and accuracy of death certificates and mortality statistics in Greenland have been raised…”
Yet Fodor claims Bertelsen’s work “ascertained” prevalent heart disease in Greenland, ignoring that Bertelsen even *admits* to the very kind of uncertain data that weakens his findings! See what Bertelsen says here:
“Partly because of defaulting Reports and partly because of a considerable number of unspecified declared death causes must be stated [that] Numbers increased…”
No question Fodor tapped into the current diet-health zeitgeist. The headline-hungry media splashed Fodor’s results around the world, fostering new doubt and confusion and causing untold numbers of metabolically deranged people to question a high omega-3 fish diet therapy and become discouraged, feeling forced to turn to statins and other prescription drugs. Not only does Fodor passively conflate the effects of a fish diet with that of fish oil caps, he even outright misstates what Bertelsen did, saying “… a number of studies have confirmed what Bertelsen ascertained more than 70 years ago, i.e. that the prevalence of CAD among Eskimos in Greenland and other Inuit populations in Canada and the US is similar or higher compared to that of non Eskimo/Caucasian populations…” Whatever Bertelsen may have “concluded” his discussion proves beyond any doubt that he “ascertained” little or nothing about the Inuit living all over Greenland or even in his own patients. And Bertelsen certainly didn’t discuss Inuit living elsewhere!
It’s a sad irony. Fodor, a well-respected academic researcher, claims to debunk a fish story through a curiously narrow and dubious meta-study that itself turns out to have a strong funk. What’s most rotten here, we may not find in the State of Denmark. –Bryan
The Inuit are irrelevant, they always have been. I hope you feel fulfilled doing all this research into their diet but it was a complete waste of time for two reasons.
One, if they were healthy, which is not proven. Noone could or would recreate their diet and lifestyle. Remember they ate things like seal blubber, polar bear liver, fermented fish heads, etc. Have fun with that! No, cows liver and fatty ground beef is not that same thing.
Two, if they wernt healthy, well, trying to replicate an inuit diet is a complete disaster.
So either way, Inuits and their diets mean absolutely nothing to us modern westerners
When I think about living in an igloo and eating raw baby seals I get a warm fuzzy feeling.
Wow, lots of information: thanks for that! This confirms what I’ve read before about the Inuit.
You’re welcome Morgana!
In my research on research, so often the signs point to vested interests. I don’t know if we can ever overestimate the pernicious effect of corporate money in food and medical research and even on social media. –Bryan
Too bad Keys didn’t travel north of CVD-challenged Finland looking for population groups free of heart disease. He found them in Crete and Italy instead, and settled down there for the rest of his very long life. Would he have done as well in a 1900-style igloo? Perhaps. But leaving Minnesota and moving to Greenland to rough it probably wasn’t high on the family’s list of destinations.
Guys if you can’t get enough of the grains debate and its offshoots, here’s an exceptional back-and-forth on it:
http://www.fathead-movie.com/index.php/2015/08/31/ancient-wheat-was-superfood/
The main ‘tagonists:
– Tom Naughton of that Fathead-movie site, who takes a more ancestral and persistently questioning stance on grains, new and old;
– “Duck Dodgers”–who, based on reading these comments and recent postings in Free The Animal, may be a composite of several individuals–suggests that early grains, esp early wheat, may have been a “superfood,” presenting many of the same arguments we’ve seen here, and;
– Richard Nikoley of the Free The Animal blog in his ranging yet always inimitable way, navigates between the two, though tends toward Duck’s position(s).
For their probing and/or just plain interesting and/or levity-bringing comments, honorable mentions go to Galina, Tatertot, Vincente, Anand, Gollum, and Bob Niland. And to the Frenchman “Egocyte” and his long suffering mistress who misses him during these long grains debates.
In these lively yet very civil exchanges, topics include:
– Dr Davis’ book “Wheat Belly”
– More perspectives on the wheat-eating Hunza diet
– Interesting stuff on microbiome, For health effects, its gene pool? Our genes? What’s their interplay?
– And the intrigue and promise of “tigernuts” (maybe not what you’re thinking).
Enjoy! –Bryan
wbryanh- Wow, that was interesting! So “Duck Dodgers” is really a composite of people? (A sock puppet?) But there is also a “real” Duck Dodgers? Who is Duck Dodgers? I’m confused….
In any case, I read quite a bit of that wheat debate (not all), until it eventually turned into a continuous, unresolved back-and-forth between Tom Naughton and Richard Nokely, so I stopped at that point. Thanks, it was interesting.
This may be the wrong place to post this, but when I was looking for information on the Inuit, I found a lot of stuff written by “Duck Dodgers”. Unfortunately, one can’t always get a balanced view of things from the internet, in my opinion: whatever is there is there. But regarding the Inuit affair, there seemed to be a rather emotional attachment to certain beliefs- (and sometimes a bit of nastiness on the part of certain people when others didn’t accept their opinion). I’m not saying one side is any “better” than the other- (I haven’t really come to anything that I can call an answer at this point, regarding the Inuit). But basically, when I see very strong biases- and when it looks like people are trying to persuade others over to their viewpoint- I immediately become suspicious.
So this is from the blog of Dr. Eades, which I mentioned before- (you can skip the first part if you want to and scroll to the part about the Inuit). There are many links to click onto, there are the comments, and eventually the discussion gets diverted over to the Free the Animal website:
https://proteinpower.com/drmike/2014/04/18/beware-confirmation-bias/
Morgana, it is interesting no? Reflecting on the Duck Dodgers entity, it leads to greater (deeper) questions. I have no idea the identity(ies) that comprise Duck. Who is Duck really? Be it him, her or they, does it really matter? The internet and mass media makes our planet more and more into one vast neural network in which we share ever more ideas concepts ever more in real time. You can argue that each of us is less an individual and more an integral part of the collective human consciousness than ever. In our increasingly Ex Machina world, we might regard “Duck” to be every bit as legitimate and real as a collaborative effort, say from a corporation or group of corporations, as from an individual. That might explain more easily, or plausibly at least, what drives Duck to write about Duck’s passionate causes, which include the possible dangers of wheat fortification and “debunking” Inuit “myths.”
For brevity, I refer to Duck as “he” for this rest of this post.
Here’s a Richard Nikoley explanation on Duck’s emergence:
http://carbsanity.blogspot.com/2015/07/temporarily-closing-comments-on.html#disqus_thread
“… It was originally one guy, as far as I know. I think the couple of posts on tiger nuts were his first contributions. But when we began what became a 17-post series on the Inuit and ketosis, those he drove were originally with his own collaborators I knew nothing of, and it grew into a core group of collaborators that is still in swing. The original Duck is still the chief draftsman of the DD posts, then they get edited and vetted by the team…”
BTW Morgana, this Carb Sanity post gives you a vivid idea how intense the grain/grain-free HCLF/LCHF debates can get. Evelyn’s one of the more strident pro-carb voices out there.
Certainly I get the feeling that our Duck Dodgers here in Rawfoodsos is the same individual, at least within this post’s comments. But I couldn’t say if ours is the original one Nikoley referred to, or some other Duck.
Is ours motivated solely by the personal story he related to us? Who went from toxic refined carbs→ low carb → “healthy carbs/grains” as he explained to us Rawfoodsos’ers?:
“I used to be low carb and bought into the anti-grain propaganda after (processed) carbs made me quite sick. At first I felt great, but after almost a year I got even sicker from low carb dieting. It was horrible. Through my own experimentation I regained my health through the Perfect Health Diet and then made even greater health improvements by slowly incorporating real whole grains and legumes back into my diet. It wasn’t the carbs that made me sick, it was the processed and refined carbs that made me sick. You could say I’m post-low carb now.”
Does a burning desire drive him to debunk CW? If so he applies that desire very selectively. You certainly don’t see it in the gushing paeans to grains from early historical figures that he amply repeated in this forum and elsewhere, claims which perforce lack sufficient science.
Do corporations, like those that comprise Big Agri, influence Duck after all? In that same post above, he responds to my “paid shill” float with this non-reason:
“… A shill for the grain industry would not be against fortification, which is widely supported by the 13 major grain lobbyists.”
That confirms nothing. What stops him from working for folks who produce whole-grain foods? The US doesn’t require these firms to fortify whole-wheat products. http://www.choosemyplate.gov/grains They might well be happy to see people inveigh against supplemental iron, B Vitamins and other fortifications in order to direct more customers away from “enriched” flour to whole wheat flour.
Even Big Agri might be pleased with his efforts. The industry faces one of its biggest market challenges ever in North America as people scale back and abandon grains in record numbers. In the US:
https://www.npd.com/wps/portal/npd/us/news/press-releases/percentage-of-us-adults-trying-to-cut-down-or-avoid-gluten-in-their-diets-reaches-new-high-in-2013-reports-npd/
“…about a third of U.S. adults say they want to cut down or be free of gluten in their diet…”
“…about one in four consumers feel that gluten-free is good for everyone…”
And in Canada:
http://www.cbc.ca/fifth/episodes/2014-2015/the-war-on-wheat
(cue to 8:10) “…over half of Canadians now report say they are cutting down on whole grains like wheat…”
At this stage Morgana why shouldn’t Big Agri condone, even support, to make fortification the bogey-man? To distract people from modern and even heirloom wheat’s other nagging health questions we’ve only recently been able to elucidate, including those raised by gluten, hemagglutinating lectins and phytic acid? In Big Agri’s view, it may be better that people switch from refined to whole grains rather than abandon grains altogether. And to buy time to come up with fortification “fixes.”
Duck’s efforts may even please the huge $26B/year supplement industry. After all, without fortification, maybe you should pop a pill to be sure you’re getting all your vitamins and minerals, right?
In sum, we can find plenty of powerful vested interests that might well be very happy to see the message that Duck calmly, rationally, and copiously delivers on the likely evils of grain fortification. When you couple that with his equally dogged insistence that we should completely ignore the Inuit diet example–thus cutting off by far humankind’s greatest ancestral LCHF success story–and all arrows point to “Grains” albeit “wholehealthyones.” Even if he started out genuinely driven by his personal experience, it’s easy to imagine Big Agri and Big Supps enraptured by his very rich multi-faceted and detailed message and even to offer him handsome compensation to widely propagate his comprehensive story. Especially if its veneer is just thick enough and the rhetorical strategies employed are robust enough to largely hide the arguments’ great many flaws from casual and lay readers. Morgana, at over $200 **billion** per year in crop sales, Big Agri can afford talented media-savvy writers like Duck and many others like him. We underestimate the power and sophistication of Big Agri’s media outreach at our peril. Enormous money is at stake.
http://www.agcensus.usda.gov/Publications/2012/Online_Resources/Highlights/Farm_Economics/
I can post here many fascinating candidates for this social media outreach if you’d like.
Morgana, not gonna lie, I obviously have suspicions here. But to be clear, I truly can’t claim to know what entity(ies) Duck(s) is/are, nor can I claim to know what motivation of mix of motivations drive him. It could be a complex mix of factors, as is so often the case, e.g. grain fortification may genuinely pose health issues. I simply try to offer possible explanations for us to consider. Apart from Duck himself, who can really say who he is and all the factors that drive him? Like the New Yorker cartoon says, “On the internet, nobody knows you’re a dog.”
https://en.wikipedia.org/wiki/On_the_Internet,_nobody_knows_you%27re_a_dog
–Bryan
wbryanh- Yes, that’s all fascinating! Great post you wrote, by the way. Basically, the very strong opinions I kept reading- (mostly when studying the Inuit issue) got me suspicious. It became clear that there was an anti-low carb agenda. Many of them on the Richard Nikoley site seemed to think (including he himself) that low carb is “dangerous”, and were trying to “disseminate” the information that people need to stop following these diets. If anyone had bad experiences on low carb or ketogenic diets, I don’t negate their experience. We all have different problems, and my guess is that most of us adults are damaged in some way after years on a refined food diet. We all have different issues, and for some, a low carb or ketogenic diet might exacerbate, or even cause some issues. As was explained in Dr. Lutz’s book “Life Without Bread”, it seems to be much easier for children to go low carb; some adults might have problems due to years on a high carb, Western diet; the body starts to compensate. Again, I’m not suggesting that everyone *has* to go low carb; but, like you wbryanh, it’s helped me enormously, in very many ways. So whenever someone criticizes it, I will always be there to defend it! (By the way, yes, I’ve read about Carb Sane already, so I know all about her anti-low carb stance).
As for the fortification issue and Duck Dodgers, you make very good points. Also, I’d like to remind you that the USDA guidelines each year are recommending more and more “whole grains”. In fact, whole grains seem to be quite a fad at the moment (along with fruits and vegetables of course), and basically every ” health food” site or nutritionist recommends them. Maybe “the masses” will still eat refined grains (they are addictive, after all); but diverting the upscale, health conscious consumer to whole grains could very well be a ploy to get more people to eat more grains, as you say. In any case, for me the grain issue is already decided, as I am celiac, so wheat and all glutinous grains are out. And I just feel so much better when I don’t eat grains at all.
By the way, awhile back I saw that 5th Estate program you sent a link to. A rather silly show. They tried to use “science” to prove that eating wheat was fine for everyone except celiacs. However, they didn’t really address the issues thoroughly enough, nor did they represent the problems in their entirety. Obviously though, there is quite a bit of media “backlash” to the current anti-grain movements.
Thank you Morgana! Glad you liked my post. I agree with so much of what you say. Very interesting about the USDA guidelines upping whole grains, yet so not a surprise. Apart from the increasingly cozy relationship the leaders have with Big Biz–indeed we see a bigger revolving door between the two–what could the USDA do anyway? They simply can’t come out against grains even if they wanted to. The food system is much too deeply entrenched in grains production. To go against grains would hugely disrupt the system at the least. I can’t see how fundamental food change will happen except in the grass roots, where customers vote with their dollars. Also interesting about Dr Lutz’ book–I’d like to dig more into the details how children can more easily go low carb, though I have plenty of ideas how that works.
About what you say here Morgana: “…most of us adults are damaged in some way after years on a refined food diet…” I add to that so many more things: The dozens of thousands of novel estrogenic chemicals in just about everything we come in contact with in our modern default environments since 1945: hard plastics (BPA) and soft plastics (phthalates), chemicals in body- and hair-care products likes shampoo, soaps, and toothpaste, carpet-bombing antibiotics pills and topicals like triclosan-filled soaps and creams, all of which that may profoundly disrupt our microbiomes, dietary supplements with their hosts of unknowns, and perfumes, colognes, and cosmetics with their even bigger hosts of chemicals unknowns:
http://www.cbsnews.com/news/new-legislation-proposes-greater-fda-oversight-of-chemicals-used-in-beauty-skin-products/
We find more and more novel organic chems are hormone (aka endocrine) disruptors, for which the FDA’s standard dose-dependency straight-line curves don’t apply. We need only vanishingly small amounts of hormones–our bods’ “emails”–to orchestrate our metabolic functions. Oddly, relatively large doses of these endocrine disruptors may cause negligible effects. So the FDA generally stops there and doesn’t test them at lower doses where they may wreak much greater damage though that may change, see here for more details:
http://www.ourstolenfuture.org/newscience/lowdose/lowdose.htm
Then there’s sunblocks that not only sports their own novel toxic brews (e.g. oxybenzone) but keep us from getting enough sunshine Vitamin D, more and more of us working late and graveyard shifts, massively disrupting our circadian rhythms, a cycle as ancient as life itself. Morgana if you feel like you haven’t been depressed enough lately, you can go here for the cure: http://www.ewg.org/skindeep/ and enter the ingredients for any common household products *including* from supposedly “safe” stuff from Seventh Gen. I recently sent this link to a friend, she spent a few hours going through it, then literally grabbed a 45gal garbage bag and went through her house pitching things into it.
Then there’s chronic noise and chronic light…Morgana, the list of our modern novel inputs goes on and on. Of the blogs I regularly read, Mark Sisson seems to cover these the most broadly, though no site is truly comprehensive. Even when I was born (1960) we’d already saturated our environment with pesticides and herbicides prompting Rachel Carson to write Silent Spring which she published only two years later. My folks were still in the “better living through chemistry” age, and many parents didn’t bat an eye at their kids playing in the DDT spray of the passing pesticide truck. These endocrine disruptors can gravely affect the exquisite hormonal choreography required for rapid cell differentiation and blastocyst formation. Who know that I didn’t suffer some deleterious epigenetic changes a week or two in my conception?
Morgana, I suppose my point is this: HCLF, swampland, LCHF, high protein, etc, if a lot of us can steer ourselves back *to a simpler lower-input life* I suspect the macro and even the micro balances will matter less, maybe a LOT less. We’ve evolved very many compensating mechanisms to cleanly cope with episodic nutrient shortfalls and excesses. Like lots of other folks, I was caught up in the details, going down endless rabbit holes looking for additive life-hacks and tweaks, taking a huge quant approach. The “simplify” message dawned on me in the beginning of 2011 when I’d gotten as far as I could with my foodway. Even though I was eating organic/pesticide-free locally produced minimally selectively-bred whole foods like foraged dandelions and wild fish, I was stuck on a BG plateau for some months. Then when I started taking other measures, esp to ditch the complex body- and hair-care products, my BGs more reliably normalized. In my kitchen, I use mainly stainless steel and glass–no plastics, teflon or aluminum. For personal care products I just use Dr Bronner’s hemp soaps, and make my laundry soap from that Dr B’s soap, borax, and washing soda–no chlorine. To clean the house, just vinegar, baking soda, and lemon juice–no bleach. Who can say say if one change was *the* seminal change that durably normalized my BGs, or maybe it was the cumulative effect of the changes? Or maybe it’s that our bods steadily optimize anyway for up to 15 years from the start of recovery, including to fully correct the w6/w3 balance in our cell membranes? (I’m 8.5 years into the journey.) Or a blend of those things? Somewhere in 2011 I evidently dropped my daily chronic toxin exposure below a threshold where the liver, lymph, and other body detoxing agencies could keep up with the daily task. Intermittent fasting also helped hugely in my recovery. My springtime allergy symptoms virtually disappeared.
In the end Morgana for me, “less is more.” I started durably recovering when I stopped permanently to *add* novel things like supplements, RS-loaded potato starch, etc. and to engage in various cleanses (except to fast, the one true cleanse in my view). Rather I started to *remove* stuff, like replacing complex products with those with fewer and simpler ingredients. I even stopped using shampoo, and lo and behold, after six weeks of feeling greasy, my hair suddenly became silky again! My scalp finally got the message it didn’t need to keep cranking out a new sebaceous skin layer every day to replace the one the shampoo stripped away. And other good news–I can eat more carbs now. Though at this point, I like what I eat and generally don’t bother.
Don’t get me wrong–I still love diving into the details! I’m hooked now! E.g. I can’t wait to see us flesh out our microbiota, to learn more how our microbial boarders interact with each other and our bods proper. But the less-is-more approach truly seems to have done the trick for me, at least to give me the final (so far) firm nudge onto the right side of the metabolic divide which now needs only the occasional intermittent fast (18–24h) to “trim” back in place. But no-one advocates the less-is-more approach. It is a lot of work to make all the changes, it requires patience and a years-long view, and it feels less satisfying that taking a pill or doing something to address some symptom. Plus, what can you sell with it? –Bryan
About the Fifth Estate piece, Morgana, yes, it also struck me as a little lightweight. Maybe it’s through nostalgia’s gauze, but I remember the CBC in better days, with more grace and gravitas, when Barbara Frum was our much-loved anchor. Good at least that War on Wheat decently followed the familiar format–interview the “experts” who pooh-pooh people’s concerns, and then interview some people who reject the party line from the “experts.” I credit them with ending the piece highlighting the disconnect between the experts and the legions of Canadians leaving wheat in droves.
I’ve seen plenty worse. Like this clickbaity dross:
http://www.salon.com/2015/05/03/diet_fads_are_destroying_us_paleo_gluten_free_and_the_lies_we_tell_ourselves_partner/
in which the author, a religious scholar, explains the anti-gluten “craze” completely in terms of religious fervor. Schulson seems incredulous and despairing at the facts he cites in the lede, that over one in three Americans are trying to cut down on gluten, throwing over mainstream consensus science.
But Morgana in these two cases and others, I see an intriguing thread. Covering the grains debate, the media, unwittingly or not, highlights and elevates the age-old Aristotelian “Experts vs Wisdom of the Crowd” to a new and exciting level. Both sides are armed as never before. Big Biz bucks back the health and medical research community to deliver the most polished (and/or obfuscating) conclusions money can buy. Meanwhile the internet arms the masses. Does that alter the balance of Aristotle’s adversarial pair? With keyboard/smartphone in hand, is today’s Crowd getting the upper hand? In North America, I don’t recall seeing such broad popular rejection of something as we now apparently see with wheat. What’s the next shibboleth to crumble?
And will this experience cement a broad-based popular rejection against consensus “experts” opinion? As obvious disconnects like the health of wheat compel more of us learn just how deeply that mainstream “science” sit in the pockets of Monsanto and other multinats? Can these researchers ever earn back our trust? Telling, and very ironic, one of the most downloaded research papers of all time:
Why Most Published Research Findings Are False – John P. A. Ioannidis
http://journals.plos.org/plosmedicine/article?id=10.1371/journal.pmed.0020124
What a change from when I was a kid. I grew up with absolute implicit faith in science. I naively believed science, even gov’t science, sat walled off in an isolated rarified place, blissfully free of the influences of politics and Big Biz. I began to doubt that assumption early on, but still it remained visceral for a long time. One of the biggest hurdles I had to clear in my life was to accept that the Dietary Guidelines might actually be not just a little wrong, but profoundly egregiously tragically wrong, made so very wrong by grim realities that went way beyond mere bad science.That grains could indeed harm us esp for those of us already suffering metabolic derangement. That dietary fat might not actually clog our arteries after all. Early on in my journey I understood the biochem that supports those views. But it still took me two years to fully internalize that knowledge. When Schulman talked about the religious fervor of the anti-gluten folks, it made me think of my un-self-acknowledged unquestioning religious belief in what my governement and mainstream “science” told me. –Bryan
wbryanh- I had a look at that link you sent- (the one criticizing gluten free and Paleo diets). Strangely, this man claims that there is no real science to back up gluten free or Paleo diets- he claims it just “sounds like science”- but then he never offers one iota of science to back up his claim that these are just “fad diets”. Instead, he talks only about religious diets and restriction. I would call this a diversion tactic! He’s saying a lot, without really saying anything. He is awfully smug about it though. Do you think people are actually influenced by this sort of thing? I’m not, that’s why I wonder about it…..
On a side note, I’ve decided to try fasting! (Remember when we talked about that?) I’m a little past the 24 hour mark now. We’ll see how long I can keep it up- (3 day would be the maximum).
Sure I remember Morgana, glad you’re fasting! How do you feel at this moment? Did you go through a rough patch where your bod nagged at you to eat? I used to get that typically at 18h into the fast, but sometimes as early as 15h and as late as 21h. You seem to be plunging into it. I eased into fasting–15h then 18h etc, initially going overnights when I was asleep for most of it. I don’t get the rough patch anymore. Morgana if you’ve been keto for a long time, chances are very good it’ll go very smoothly and you’ll feel great at the end. Maybe you’ll keep us updated here?
About Schulson’s piece, what you ask: “…Do you think people are actually influenced by this sort of thing?” Morgana, I’m afraid so!! Its power comes from perceived cred, (People see Salon’s as one of the better Webloids), the sentiment it conveys to feed one’s confirmation bias, and that these pubs count on people reading quickly, to not dig, to absorb only the gloss, the veneer. One of my best friends from university and one of the smartest people I have the honor to know, this piece resonated with her and she had earlier spent a year on grain-free LCHF losing 40 pounds! It amazed me this Yale PhD and actual savvy person didn’t see the glaring disconnects and lack of evidence in this piece and resisted even to discuss it. This journey offers me so many teachable moments! Especially about the power of the acculturation, status quo, and the great money and influence behind preserving it to guide mass and social media to subtly shape our perceptions without us even being conscious of it. If you listen to NPR, the On The Media program does a great job to discuss many points of this phenomenon: http://www.onthemedia.org/ –Bryan
wbryanh- I’m about 30 hours into my fast right now. I will try either 2, or if I can make it, 3 days. I felt a bit rough when I got up this morning; the feeling I get after a long overseas flight and I’m jetlagged, is how I felt! Now it seems to be a bit better. I actually started to feel hungry last night after 12 hours, which was very odd, seeing as I very often do 16 hour overnight fasts; however, I think skipping dinner is harder for me. (Plus, I had to make some bone broth in preparation to break my fast, and it was cooking on the stove last night, so I could smell it…..I think that got my hunger going!) I am used to low carb- (though I’m pretty sure I’m not ketogenic all the time, I think I cycle in and out)- and I’m used to intermittent (long night time) fasts. However, on my long overnight fasts I do allow green tea sometimes in the morning, no breakfast. This fast is very different, partly because it’s longer, but until now I’ve been doing only water. So we’ll see how it goes; I am very thin and I do have low blood pressure, so if I notice any undesirable effects, I will stop. I’ve done pretty long anyway, I think.
Morgana, excellent! Only, in my experience at least, I *always* feel really good throughout. I never feel ill or ratty in the least. Dunno if you take any meds or supps–I take neither–but if you do, they may cause an effect. The hypotension I got back in 2009-2010, I no longer get those symptoms and my BP is still 90/60. Are you going for walks during the fast? Whenever I’m sitting around and start to feel peckish, I go for a walk and that always does the trick. Long as you keep things aerobic, no problem to exercise (like walk) as much as you want. During one 3-day fat, I walked **40 miles** (roughly a third of that each day). About you being thin and having low BP, certainly that’s something to stay aware of. From my reading, healthy BF% readings for men are 10–20%; for women, 15%–25%.
When I fast I let these three things guide me, after the 15–21h window:
– Do I start to feel a strong desire to eat?
– Have my BGs dropped solidly in the 70s? (check with glucometer)
– Have I stopped losing body fat? (Check with home scale. I use Tanita UM-028 which measures total weight and BF%. You can find plenty of scales that give both.)
If I start to feel a strong desire to eat, or even a mild desire to eat that lasts more than 30min, I end the fast. That’s happened exactly twice in 300+ fasts.
If my BGs drop solidly into the 70s and stay there for 8 hours (three BG checks, 4 hours apart.) I end the fast. Usu I get there by 24–40h.
If I ever stopped losing body fat%, I’d end the fast. But after fasting over 300 times, that’s never happened. 🙂 I measure it every morning after I get up and before I eat or drink anything.
Morgana, do you have a glucometer? Even if you’re not diabetic, it’s a very useful tool. Plus a lot of people ride above the 75–95 mg/dL range and their docs still tell them “no prob.” So it never hurts for any of us, diabetic or not, to self-test esp at post-meal. Dunno about in Deutschland but hre in NA it’s getting a lot cheaper to get set up with a kit and 100 strips, as low as $35. –Bryan
wbryanh- I don’t take any medications, and I also don’t take supplements. I’m like you in that regard, I don’t “believe” in supplements, possibly because every time I’ve tried to take them, I’ve felt awful. So I’m not sure why I was feeling terrible; though if you look online, many people talk about feeling awful while fasting. They call it “detoxing”. I never believed in that before, though now after my experience I’m not so sure…..
In any case, this morning when I woke up I felt even worse. I felt very nauseated, and like I was going to be sick. When I stood up I felt like I was about to pass out. I had to lie on the floor for a long time with a cold compress on my head. When I finally stood up and looked in the mirror, I looked very pale. So I decided to “listen to my body”, and I just had a cup of bone broth. I feel markedly better after that! Although I actually had no hunger, I think the other symptoms told me I needed some nutrients. I made it to about 2 days on just water alone. It was my first longer term fast, so I guess that’s admirable. It could be that I’m just not cut out for long term fasting, although I feel great with my 14-16 hour overnight fasts! As I said, I’m skinny and I have low blood pressure. In any case, I might possibly try the 3rd day (now) as a liquid fast, with bone broth, yogurt, tea, etc. But if I feel a strong desire to eat solid food, I will.
I don’t have a glucometer, so I have no idea what my blood glucose was. Last time I measured it was about 2 summers ago, when my fasting blood glucose was 76, as I recall. Maybe I should get one, but I get worried about becoming too obsessed with measuring! I can be quite obsessive about things like that…..so I’m not sure if it’s good for me. I would also be kind of interested in measuring blood ketones- (but I guess those implements are expensive?)
So in any case, I’ve broken the water fast, but I’m still doing a fast of sorts. Oddly enough, after awhile I started to feel like I disliked water. Water seems to give me gas (who’d a thought? I haven’t really noticed that when I ate food; I assumed it was what I was eating). In any case, at the moment I feel a bit opposed to water! Whereas the bone broth went down smoothly…..strange. I might just be an odd person. (In fact, I’ve thought that many times, ha ha).
Morgana, sorry you felt so off when you woke up! You did the right thing to start the broth. I made it a point to end a fast if I felt anything was awry for more than a brief period–say for 30 min. Only, that’s never happened in 300+ fasts. Still I should’ve restated that condition in my last post. Without fail, I always felt better and better as the fast progressed, in time, to the point of sublime. Esp I get a mental acuity and (self-perceived of course) great cognition coupled with a sense of deep calm and well-being. And usu by the second night of fasting (starting at ~28h), I start to have wonderful vivid dreams, at times transporting. I understand how some ancestral cultures, esp some First Peoples here in NA, fast as part of their spiritual quests.
One other thing, during fasts, I drink water, hot and chilled green tea, and decaf drip coffee throughout. I doubt I take in a dozen kcals from that during a fast. But they supply a small but steady stream of minerals (like manganese, potassium) and phytochems like the lauded EGCG (if you believe in the phytos). For whatever reasons, my green tea (specifically Yamamoto’s uji cha loose leaf in 100g bags) does a wonderful job to calm any residual desire to eat and helps me feel very good and calm. Your micro-packed bone broth is excellent–we tend to lose fastest the water-soluble micros like minerals and some vits like most of the Bs. I plan to make broth when/if I decide to fast past three days. At three days, I’ll convert to a broth fast.
What may help explain your bumpy experience, Morgana, I have a few thoughts. Most important, what was the longest you fasted previous to this fast? 16 hours? I can’t emphasize how much I *eased* into longer fasts. I added only an hour or two at a time, and even then stayed on plenty of plateaux. I took months to work up to 2+ day fasts. Also, I was firmly into ketosis for at least a year before I started fasting, eating only 30–40g carbs per day, evenly spaced across several meals–I rarely ate more than 10–12g carbs at a meal. You said “…I’m pretty sure I’m not ketogenic all the time, I think I cycle in and out)…” Sounds like you weren’t getting food desire, but still, recent glycolysis, however intermittent, *may*–I say *may*–be a disruptor for you. I feel mild brief glycolysis shouldn’t pose a problem, but YMMV.
Not sure that weight/body fat/BP per se are necessarily issues. Even as a 6’ 1”/1.85m man who dropped to 168lb/76kg and 10% body fat, I did fine with fasts. But again YMMV.
For me, BGs are the biggie. They are my main fasting guide. Per the C-Peptide endo-insulin proxy biomarker, I have low, even marginal insulin production. Likely due largely to this, I’ve long tended to have slightly elevated BGs. E.g. I stayed into 70s and lower 80s, even as others might drop into the 60s under the same fasting conditions.
About serum ketones, I stopped measuring that in 2008 because they always came up negative on the urine strips. But this was after going keto diet but before I started fasting. Now as combo glucose+ketone meters and supplies get cheaper:
http://www.walmart.com/ip/PRECISION-XTRA-KIT/5379215
maybe I should consider to re-add it. Again Morgana, my conditions almost certainly vary from yours, so maybe a good idea for you to add ketones. I understand your concern about “over-measuring,” only it’s appropriate when we embark on a new thing.
Finally, I always stayed physically active during fasts. Esp I walked, usu a lot. Fasting or not, walking always makes me feel better! About being odd, Morgana, aren’t many (most?) of us a bunch of odd ducks to be here and so passionate about all this? 🙂 Guilty as charged! –Bry
wbryanh- thanks for the tips. As I look back on this whole experience, I think the big problem was that I did just a water fast; mainly because Dr. Thomas Seyfried recommends that. (Have you heard of him? The “Cancer is a Metabolic Disease” guy?) He recommends water-only fasts of 3 days twice per year- or 7 days once per year- to get rid of rogue cells in the body that might turn into cancer. I did it partly for that reason, but for other reasons as well, like the spiritual, sublime feeling. However, I think there was something about the water-only aspect that was a problem for me. When I do my 14-16 hour fasts- (and by the way, I average 14-16 hours; I have done 17 and 18 hours with no problems. And occasionally I only do 13 hours, it depends on convenience, what fits into my schedule). When I do the long overnight fasting, I drink green tea, just like you; and yes, it’s awesome, it makes it so much easier to fast! But I guess the caffeine in green tea can spike insulin in some people, so that’s why it’s not recommended. However, there are loads of fasts that are recommended in books and online; some include tea (and even coffee, so long as it’s 0 calorie) and one of the books I read said lemon water was an option. I opted for water only, and I think that was just too intense for me. I wonder if the water flushed out too many nutrients? Because my symptoms early this morning seemed like an electrolyte problem. What also happened is that after awhile, the water started making me feel sick, until eventually I just didn’t want to drink it anymore. Maybe that was my body telling me it was the wrong thing.
As I’m writing this, I realize that I have done some 16 hour fasts on water only. Hmmmm…..not sure…..maybe it was just too long with water only? If I were to try this again, I think I would use green tea and lemon water.
As for “ketosis”: before I did the fast, I had done my 16 hour fast- (possibly even more)- then i met a friend for lunch at a restaurant. It seemed like a low carb lunch, but I can’t be sure. I had a lamb in yogurt sauce, maybe the yogurt spiked my insulin? I also had some vegetables, but they were minimal. It should have been low carb, but it wasn’t my usual bacon and eggs, so who knows if the body reacts differently. But what could also explain my problems is I might actually by nutrient deficient. (Not sure). I had many health problems for many years, and had malabsorption (due to undiagnosed celiac disease) for a long time. It could be that I need to be eating right now. (?)
In any case, the intermittent fasting seems to work brilliantly for me, so I’ll stick with that for now. And right now I’m craving a nice cup of green tea, so I will have that in a moment! By the way, all day I’ve only had that little bit of bone broth. So it’s still fasting of sorts, I guess……..
I forgot to add in my last long winded post, that I was doing some walking. I had to run some errands both days, so I did a reasonable amount of walking outside (not anywhere near as long as you, I couldn’t have mustered it). So I don’t think that was the problem.
As for sun, there’s zero sun here right now. But I try to eat lots of oily fish and eggs.
Morgana, another thing that works very well–sun. Without sunblock of course–I never use that anyway. 40 min of midday sun (20m each front and back) makes me feel very calm and good, esp during fasts. I realize that’s not much of an winter-time option where you live. Maybe you can find light therapy with uV-B? 20–40 minutes of uV-B converts your dermal pre-cholesterol to Vitamin D (D3), see more about it here:
http://www.cholesterol-and-health.com/Vitamin-D.html
–Bry
wbryanh- Well I broke my fast today; exactly 3 days. Guess what the first solid food I had was? Eggs sunny side up, with runny yolk and crispy white! Very delicious. I also had a few sauteed cherry tomatoes with fresh basil. This first meal tasted so good. What’s amazing is that my digestion feels so good and “clean”; don’t know if that makes any sense.
By the way, the whole 3rd day fasting I felt pretty good too. Many people say it gets easier as you go on, but I’m sure it helped that I was drinking tea, bone broth and having other fluids besides water. I feel like I could do a fast, no problem, with these other liquids, so if I do one again, that’s how I’ll do it. (I also felt today like I could have gone on, but I decided not to; it’s Christmas after all). Apparently a water fast is much more intense than other types of fasting, and people go through a period of “detox”. When I read about these symptoms of detox online, I assumed they were “low carb flu” and that I wouldn’t have these issues; however, now I’m not so sure. If the body really is going through autophagy and getting rid of cellular debris, maybe some of us do feel those effects? The “water only” part might have just been too intense, and too much at once for me. Besides, I’m not a big fan of water. (Never was). Especially not now, since it made me feel sick! Oddly enough, I do notice now it gives me gas. I never would have realized that.
Anyway, now that I’ve broken the fast, I feel even more awesome. Really clean and healthy. I think it was worth it; I learned something, next time I would do it differently for sure.
Morgana, one other thing to think about in the “water only” category is electrolytes. In a book I was looking at about the Rice Diet, it was noted that the low-salt diet could be quite dangerous because of hyponatremia. Drinking water with no salt WILL make people sick and kills some athletes each year. Broth is a really good idea!
heathertwist- I was drinking water with a higher sodium content than what I usually drink (at least for most of the time). So I doubt that was the issue. I had even read that in a short term, 3 day fast that electrolyte imbalance is normally not a problem, though I guess it could have been in my case. Many websites seem to agree though that what I was experiencing were common “detox” symptoms, which happen more often on water-only fasts (as they are more intense than other liquid fasts).
About the broth: it did have salt in it, but there are many other nutrients in broth, so it could have been any number of things. In any case, the broth solved the problem.
Good point Heather. Esp on hot humid days when we lose a lots of NaCl through our pores.
http://www.rice.edu/~jenky/sports/salt.html
I’ve thought about how to add salt to my fasting bevs. Though so far haven’t done it, probably because I live in a very mild and relatively dry climate. –Bryan
Morgana, excellent! I’m tempted to say “all’s well that ends well” though if you want let’s keep examining why you felt off at any time during your fast. Could be the bad patches will simply fade away as you do more long-ish fasts. Again, can’t stress enough, in my six years of over 300 fasts, I almost never suffered issues, except for occasional hypotension-like symptoms in the first year or so, and that I had to end fasts only twice due to a strong persistent (i.e. more than 30min duration) desire to eat.
Wonderful you broke it with those eggs. God they’re yummy! About your digestion feeling “…so good and ‘clean’…” it makes a lot of sense to me. For me *everything* feel good and clean. Everything works a little better and even a lot better. For me, fasting is the one true “cleanse.”
Morgana, the water-only fast never made any sense to me. Why shouldn’t we avail ourselves to a small but steady stream of nutrients from near-no-cal bevs like green tea and coffee if it makes the fasting more healthful and even enjoyable? Why shouldn’t we drink the tea to deeply calm our GIs, to let them quiet like a primeval forest? Even fasting this way, I always get the desired result: nice low BGs and always weight and fat percent loss. And honestly, I can’t imagine a better “drug.” A down-side, I sometimes catch myself thinking that food is a “necessary poison” and have to remind myself that view comes because we usu chronically over-nutriment. The dose makes the poison, and the chronic dose makes the chronic poison. And it’s true what you noted, you can feel even better when you finally break your fast.
As it happens, I’m 41h into a fast now, the first double-overnight fast I’ve done in some months. BG last aft/eve was 83 (at 23h), late this morning 84 (at 37h) so will keep noodling along till I reliably drop into the 70s. That lovely sublime feeling started kicking about an hour ago. I’m gently sipping drip coffee and weak warm green tea and very much feeling like I’m gently centering into the zone. I’m getting that lovely gentle silent thrum all over my bod to the tips of my toes and esp my fingertips. My fingertips now feel exquisitely nimble as they fly across the keyboard and I’m feeling a calm deep contentment, making me wonder why I don’t seek this even more often. –Bryan
wbryanh- This link explains why water fasting can be so intense, and that the autophagy that takes place can cause symptoms (very much like many of my symptoms):
http://www.freedomyou.com/common_physical_reactions_to_fasting_freedomyou.aspx
I must have had many toxins in my body, mostly due, I imagine, to very harsh medical treatments I had in the past. These things can get locked in the cells, and I guess it all came out too quickly. Drinking things like bone broth and green tea would have slowed down the process- (though it still continued to an extent, just more bearable). I think this is what happened. In retrospect, I see there were many bad things in my body, probably more than most! I didn’t realize it would be a problem, since i didn’t believe in the “toxin theory” before I started, but now I do. One reason why I believe in it now is not only that I experienced those bad effects, but I also feel “cleansed” now. It’s amazing how great I feel! Because of that, I would definitely do it again, but this time, as you said, I would drink green tea, maybe lemon water and/or broth. At least for now….I think I need to. Also, if the “toxin/cleansing theory” really is true, maybe the next one would be easier anyway, since I got rid of a lot of toxins already. With the intermittent 16-ish hour daily fasting, that has many benefits too, but it doesn’t actually cause autophagy. So I wasn’t really prepared for that.
wbryanh- First, off Happy Holidays! How is your fast going- did you break it yet?
In any case, I’ve been thinking a lot Post Fast. As I said, I finally got the feeling of deep inner peace, euphoria, happiness, whatever, on the 3rd day of my fast. Many people talk about this during fasting, and accredit it to the fasting state; however, this feeling is still with me even though I’m eating now; if anything, it’s enhanced! (Having it coincide with Christmas is perfect). I have a new theory about that: if fasting really does cleanse the body and get rid of “toxins” (otherwise known as “autophagy), maybe when this process is completed (or even near completion), there is a sense of euphoria because the body has gotten rid of toxic elements that weighed it down? For many people, this may coincide with the fast- (i.e., they got over the “hump”)- whereas I chose to end my fast, as planned. I’m beginning to think this may be the case, and not necessarily the fasting state per se……what do you think?
I posted a link yesterday about some common symptoms during fasting, with an explanation as to what they mean. I had many (though not all) of those symptoms. What’s interesting is that many of the pains I had really did coincide with “problem spots” in my body: old operations, injuries, lower back pain (which was attributed to the intestines), etc. So I’m really beginning to believe more and more that there is something to the “flushing toxin” theory! I’ve been eating healthy for the last years, and since I went low carb I felt massively better than I had done, so I assumed that I had no real “toxins” to come out. However, I read that these things get stored in your cells for long periods pf time, so you don’t necessarily “feel” their effects…..although I guess one day, they could cause problems. And if that’s true, my body would have been really loaded with “stuff” from years ago: chemotherapy, operations, medicines, antibiotics; you name it, I had it! Maybe the water-only part was just too intense for all that. Well happily, I haven’t taken any medicine in years now…..
Anyway, I feel so good now I’ll probably do this again in June (except not water-only).
Happy Holidays Morgana! I’m really delighted you feel more and more positive about your long fast! No question when I end a fast and start to eat, that lovely body-wide gentle lift I get, that’s amazing in itself. It’s at that moment I feel that THAT shows what should be our relationship with food. To eat when the food genuinely physiologically benefits us. Not to use food mainly as some kind of drug, to scratch a vague itch, to eat from a mindless response to chronic low-level stress in our lives, its large amount maybe yet another product of modern life.
One of (many) questions I often self-debate: Is it ancestral for us to always want to eat more than we need? Should we give full weight to the idea that we evolved to deal with chronic food shortages? That’s it’s deep in our genes to eat AMAP at every opportunity?
Reason I ask this, I feel I’ve come very far in my journey, and start five years ago to eat ad libitum, and hover around the same weight and BF%–190–200lb (86–90kg), 18–20%. I eat keto and make sure I get in my food all the micros (as best I understand the levels of those micros we need, using RDIs as *starting* points). And yet, inevitably my BGs slowly start to slide off the rails, increasingly staying stubbornly 100+ fasting, 110+ post-meals. Only fasting corrects this, when I drop back to high 70s/low 80s fasting, high 80s/low 90s post-meal. This cycle keeps lengthening, but I still face it. Would I never have had this issue had I not eaten mostly SAD for my first 46 years? When I meet, and occasionally rent rooms to, older people who come from more ancestrally-connected societies, like country Poles, Nepalese, Tibetans, Ghanaians, several things strike me about them: how thin they are, how fit they appear, how low their BGs are (they usu let me measure them and they usu give 70s mg/dLs), and especially how modest their food portions are. They simply seem to be satisfied with what we may well think are remarkably, even ridiculously, small servings. And they often eat grains/HCLF. What if I had been born and grew up in one of their societies? Would my default birth state still would have been “eat AMAP” but subsistence diet living and early cuisine acculturation modifies and permanently establish in me a healthy food relationship? True, the question, as it relates to my own bod, grows more academic as I continue to heal, even nine years after I embarked on this journey. But I still pose it, it interests me, and the answers may help others of us in the struggle.
As far as fasting to “get rid of toxins” how I understand autophagy, where we see the benefit is intracellular, in our cells’ cytoplasmic fluid. The “toxins” may not so much be heavy metals or other inorganic compounds or even novel toxic organic compunds, but rather something as normally innocent as incompletely digested organic debris. This debris bump around in the cytoplasm, which literally physically interfere with the many metab processes that occur in that fluid. “If our hosts constantly chow food” our bods may ask, “why should we ever bother to break down this junk to scavenge kcals?” And so we lay the groundwork for chronic disease, in which often the *ultimate* driver is our bods’ failure to *properly signal* processes, in which timing, quick action and response are vitally important for long-term health. An example is T2 diabetes, an early condition most often preceded by insulin resistance, in which the cell ignores insulin’s request to let in glucose. Go here and scroll down to the third graphic in the section “Insulin Signal Transduction:”
http://themedicalbiochemistrypage.org/insulin.php
You see that the insulin receptor is located elsewhere in the cell membrane from the GLUT channel that admits glucose. There’s a least a 4-step process that occurs in the cytoplasm to finally tell the GLUT channel “hey, you, let in that glucose!” If the cytoplasm’s gunked up with junk, the GLUT channel gets that memo late. Walk through Times Square at 3am and 9am and you see how fast and slowly you travel. At which hour will you more likely arrive late to a meeting? Meanwhile the beta cells see only that serum BGs keep piling up and decide to dump still more insulin into serum, which in itself promotes inflammation which increases further insulin resistance leading to yet more serum BG buildup. And so you see how we kick off the vicious cycle of more insulin more insulin resistance. This Morgana because we don’t force our cells to clean their cytoplasmic “rooms” every once in a while so all the players there can simply reach each other quickly! That’s the hypothesis anyway.
We live in an utterly unique time in human existence in which record numbers of people, in essence, can and do over-nutriment themselves nonstop. Certainly for all of here in this forum, we rarely if ever lack access to plenty of food. Even for all of my grandparents who grew up in the US, they didn’t face this condition. Norman Borlaug and other achieved an incredible thing, they helped drive down world hunger to record low levels. But the downside is that increasingly, we never have to clean cytoplasmic “house.”
To look at the matter more broadly, we build up cascading mythologies to explain and justify emerging new status quo: “Eat healthy carbs, eat three squares a day, move your bowel every day, avoid dietary fat, long fasts can harm us,” and on. A big part of my journey has been first, to acknowledge that, even in our highly rational and empirical world, we can still promulgate and nurture a bevy of mythologies. And then slowly trace back along that long tortuous trail of modern-day health and nutrition mythologies to expose them. This is where staying current with our growing and evolving understanding of ancestral ways helps me immensely.
Anyway Morgana I hope I answered your questions!
LESS IS MORE!
Btw, I’m still in fast, at 63h (2.5+ days). Last eve/this morn the BGs were both 80, not quite the mid-70s I seek. Weight dropped from 198 to 192+ (90 to 87kg) with the same BF (20%), suggesting some glycogen drawdown. My sluggish BG correction may be because I’ve done less exercise than usual. I walked 12mi/19km during this time, but that’s less than usual for me, and I’ve done no resistance at all. But I feel great and very calm with my steady flow of uji cha and coffee and so far get no other “stop” signals. So on I go! The sublime feeling kicked in yesterday mid-morn and I slept well and long last night. I‘ll go for another walk after I post this to you. It’s crisp and beautiful out. –Bry
wbryanh- Thank you for your long and very interesting post. In my own case though, I’ve almost always eaten “less” food. I had years of malabsorption due to undiagnosed celiac disease and other digestive issues. I ate a mostly vegan diet for many years before getting very ill, and I always had to “watch my weight” (I used to be a professional ballet dancer). I even suffered from anorexia for awhile, which, luckily, was short lived. But I definitely didn’t get sick due to “over nourishment”; however, I did eat the SAD as a child, and I ate high carb for most of my life, which, in my case, meant eating often (though little). So I’m not sure if it’s the “amount”- (apparently, according to some observers some hunter gatherers and other native cultures ate huge amounts of food)- but rather the food quality, and also, *when* we eat. (Conventionally we’ve been told, at least for awhile, that we needed to eat “little and often”, that “breakfast is the most important meal of the day”, etc.) It is true that for many food is available 24/7; well, mainly for those people who can eat candy bars and soda and gluten. These foods are cheap, and in Germany, you can buy them and eat them whenever you want. These foods are lacking in nourishment though, so I wouldn’t call that “overnutrition”, I would call that too much sugar and junk. There are theories out there that many eat too much because after eating nutritionless junk, their bodies are hungry for real nutrients, so they try to get it somehow (by overeating). This makes sense to me; although i still find Duck Dodger’s theory about fortification interesting, but both could be true. Eating fortified nutrients is different from eating whole food, as we’ve discussed.
In any case, about fasting/autophagy; the way I understood it is that any damaged, sick, or diseased tissue tends to get “eaten up” or excreted by the body. How much of this happens is determined by the individual probably and also by the length of the fast; (this is why some people like Dr. Seyfried recommend at least a 3 day fast to get rid of rogue cells that could turn cancerous). Although I think the things you wrote about happen too, it wouldn’t surprise me if some other toxic elements get removed from the body as well. According to what I read online, when we aren’t able to excrete toxins, we either store them in our fat cells, or they lie deep in other tissues or organs in our bodies, to “get them out of the way” where they won’t cause acute harm (at least not right away). I can find links if you want; (if so it may take awhile). Of course, fasting hasn’t been studied much, so much is probably conjecture, but based on my experience I think this may be a possibility.
What is known scientifically is that longer term fasting increases human growth hormone, has an “anti-aging” effect, lowers blood sugar and insulin, raises ketone bodies, is good for brain health, and revs up the immune system. There might be more effects which I have forgotten to write about……
Morgana, many good points you make. Fasting works so well for me for many possible reasons, which include:
– I had no serious diag’ed med issues till my T2D diag in 2007. So more “ancestrally capable?”
– I never took prescription meds, except for short courses like antibiotics. So more “ancestrally capable?”
– I’m near the top end of “healthy BMI” and, at 20%, at the top end for healthy body fat for males. – I look thin, but have plenty of fat to start with.
– I fully keto-adapted more than a year before I started to regularly fast
– I greatly eased into fasting. Over months to gradually nudge up to 2- and 3-day fasts.
– I “intermittent fast (IF)” most every day. I typically eat between noon and six–eight, so do IF 16-18 hours most days.
About chronic overeating, you’re right, I should have said more specifically. We usu eat and absorb too many *calories*. Though not always, like your case. I haven’t heard we can eat too many micros. Except in super rare cases like too much preformed Vitamin A from polar bear liver.
About Duck’s ideas on fortification, I’m very interested too, and indeed, see fortification as (a big) part of the larger problem of supplements and their many attendant concerns which include the sources (e.g from China with all its heavy metals/other toxins?), doses that can vary wildly from stated amounts, and novel formulations that can hugely impact bioavailability and skew our metabs in unknown ways. Supps, which includes fortification, with all their wild cards, is the Wild East of nutrition.
On fasting/autophagy, seems likely many things happen at once. What you say “any damaged, sick, or diseased tissue tends to get ‘eaten up’ or excreted by the body.” could be our fasting autophagic bods do this better because of more timely metabolic processes–proper signaling–like I talked about in my last post. About what you quote from Dr Seyfried: “…fast to get rid of rogue cells that could turn cancerous…“ yes, pre-tumorous and tumorous tissue love glucose, and fasting drops BGs which severely limits their favorite food. And, again, lower cytoplasmic junk allows better more proper signaling, which allows our immune system to more effectively mop up rogue cells. About purging toxins, many organic toxins, like organochlorides and -phosphates, are fat soluble–like you noted they lodge in fat tissue. Fasting forces our adipose tissue to release lipids and presumably the fat-soluble toxins they sequester. Maybe also the case for some heavy metals, e.g. methylmercury in fish adipose tissue. Morgana, no hurry on the links. But when you have time, I’d really like to see them.
Finally, it’s so interesting, I intuit that fasting should reduce HGH because where’s the fuel for all that anabolism? I wonder what was the evol selection for that? Haven’t seen a great def for it, but Jason Fung gives a decent explanation here:
https://intensivedietarymanagement.com/fasting-and-growth-hormone-physiology-part-3
Oh Morgana meant to tell you, I very much liked that list of fasting symptoms you posted Christmas Eve. Some lines stood out like this here, which I only slightly modify:
“…Wonderful freedom comes when our flesh is allowed to dwell in silence, sharpening perception of the greatest sound of all; God’s still small voice…”
I’m not at all a religious person. But as a 55yo who loses more peers and family, most to chronic disease, I think more about the forces and presences beyond our ability to empirically observe.
Speaking of fasts, I’m *still* at it! Now my longest ever fast–87 hours and counting. A little over 3.5 days. I walked 14mi/22km yesterday which brings total fast-walking to 25mi/39km. My BGs finally reliably dropped into the 70s–76 last eve, 77 waking today. I continue to feel very calm and very good, though feel I’ve had enough coffee and ujicha for the moment. I’ll eat in an hour. –Bry
wbryanh- congratulations on your long fast! Sounds like a great way to break it.
I’m sorry: I forgot what links I was supposed to post for you? (My old age, ha ha). I have a system where I can easily see all the posts that you guys write, but I can’t go back and reread my own posts without scrolling up and down the whole comments section of this blog….so I’ve forgotten what I had offered to link to. If you can remind me, I’ll do it when I get a chance (sorry).
By the way, I just read that Jason Fung article earlier today, coincidentally, and sent a link to one of my relatives!
Thanks Morgana! Now if I can only stay awhile on this “lee side of the metabolic divide.”
For those links, from your post with this: “…when we aren’t able to excrete toxins, we either store them in our fat cells, or they lie deep in other tissues or organs in our bodies, to “get them out of the way” where they won’t cause acute harm (at least not right away)…” But no rush. I’m just sitting here relishing the mellow 🙂 –Bry
This is not exactly the link I wanted to post, but it’s interesting nevertheless. I’ll look for one about the storing of damaged cells in organs and tissues- (I know I read about it; it might take me awhile. I’ll have to look tomorrow, as it’s getting late here). But I’ll leave you with this to ponder (you may have seen it already):
http://www.sciencedaily.com/releases/2014/06/140605141507.htm
Thanks Morgana. Pleasant dreams! –Bry
wbryanh- Here is a link describing how toxins get deposited in the body. I know I read several other articles about this that were specifically related to fasting, but I’m having trouble finding them- (it’s hard to type the exact words needed to find them again, as the main articles were about fasting, and the “toxins being hidden in cells and organs” part was just a side note). I’ll keep looking though:
http://drbenkim.com/toxins-cleansing-detoxing.htm
In any case, like with all nutritional/ health aspects, this may not be a proven scientific fact yet, but possibly a hypothesis. (However, many people who fast seem to experience this effect of what they feel is “release of toxins”, or autophagy, whatever you want to call it). As I said earlier, when I first read about these fasting experiences, I attributed them to “low carb flu” and assumed I wouldn’t get all that. However, I’ve experienced “low carb flu” before, and it was nothing like the intense experience I had while water fasting! Aside from the fact that I should be reasonably adapted by now. People who eat low carb, even when not in constant ketosis, still burn mostly fats. As I said, I think I cycle in and out of ketosis- (though I don’t measure, I’m pretty sure I can feel when I am in ketosis; I recognize the signs in my body). Though I feel good being in ketosis, I do tend to get very thin, and when I think I look too underweight, I add some carbs back in.
Anyway, part of the reason I posted that Dr. Longo link yesterday was due to what he said at the end; that (paraphrasing) these health effects in the immune system most probably extend to other organs and systems in the body as well. They are in the process of scientifically testing that at the moment. Fasting research is still in its “infancy”, and I’m sure there will be a lot more interesting information to come!
wbryanh- here is another extensive link- (I think I already sent an excerpt from this before, a small part of it looks familiar):
http://www.falconblanco.com/health/fasting.htm
Again, I don’t know how “scientific” it is, but I am more inclined to believe this sort of thing now, as it really confirms what I experienced. Who’d-a-thunk-it….
One of the references at the end of the link is to a Dr. Shelton, who oversaw many fasts in his clinical practice, and wrote many books on the subject. One of his books- “Fasting for the Renewal of Life”- was recommended by Dr. Thomas Seyfried- (“Cancer as a Metabolic Disease” guy). I wanted to read it, but it was rather expensive. So, I continue to get my information online. In any case, my fasting experience was so interesting, I’d like to read as much about it as I can now.
Hi Morgana, sorry to take so long to answer. Was on a couple of my occasional Ancel Keys and Inuit binges, hah. Thanks for digging up these links. It’s late here, time for shower and bed. I’ll read them tomorrow.
I’m so glad you found fasting so interesting. The last 8.5 years was a marvelous time full of life-changers for me. Fasting ranks near the top of that list. –Bry.
Morgana, 45min ago I broke my personal-record-breaking fast. 88 hours.
Final BG: 73mg/dL/4.0 mmol/L.
Weight and BF% dropped from 198lb/90kg and 20% down to 192lb/87kg and 18%.
I didn’t have much desire to eat. I didn’t want to end the great calm and quiet I felt. I ate a small avo. Then a small bowl of nuts (~12 macs, ~8 cashews, 8 home-sprouted almonds, 3 hazels) on a few TBs of unsweetened coconut flakes, sprinkled with cassia and raw cacao powder, and mixed with maybe 1–2TB each of pastured salted butter and red palm oil.
Very quickly I realized: That’s all I wanted.
Almost immediately, I could feel a kind of gentle coursing of something all throughout my bod.
Ten minutes later I briefly felt wonderful light chills all over my bod, which lasted may a few seconds.
My bod still feels very calm and quiet. –Bry
“– Richard Nikoley of the Free The Animal blog in his ranging yet always inimitable way, navigates between the two, though tends toward Duck’s position(s).”
Ha. That is a comment thread I’m particularly proud of. I go way back with Tom, so I was on my best behavior. Inimitable is apt, since I doubt I could imitate my own performance there. 🙂
Re the mystery with Duck, yes it’s him. I’m just getting to this post and comments last few days. Very much of what Duck has posted here is on FTA in various forms in the 17-ish Inuit posts we did and the comments, and for the fortification, bloodletting, and grain posts too.
The collaboration angle was the result of a kinda joke, really. Somewhere along the way, Duck, I, and a handful of others began discussing everything going on in various comment threads via email, and I, Duck, sometimes Tim Steele and a couple of others would spontaneously end up getting aspects of that collaboration into comments wherever. We’d mildly strategize or try to figure out some interlocutor’s true angle. Etc.
At one point someone asked “who is Duck Dodgers” and the answer was “we are the Duck Dodgers.” …”We are the Borg. Resistance is futile. You will be assimilated.” LOL. The individual Duck still does most of the work, but depending, for new posts, we often discuss back and forth before I publish. I hope it’s resulted in a higher quality product.
He just confirmed to me last week that another one is in the works for FTA. More of a distillation of obesity integrating everything we’ve learned.
In other news, I recently started a Podcast and my first interview is with Angelo Coppola about “Plant Paleo” that overlaps substantially with this post, which was mentioned in the interview.
One thing I’ve seen only touches of here through my watery eyes over the last couple of days and is something Angelo emphasized in our interview is that one reason to go lower fat is that it’s more calorically flexible and nutrient dense since fat has almost nothing in the way of micronutrients. If you are high fat, like at 80%, you better be eating liver and oysters often.
Anyway, I’m on a tablet and don’t want to risk losing my place amongst 1,500 comments, but the podcast is at FreeTheAnimal.com, click the Podcast menu item. It’s #2.
Denise dear: you have an email from me with an invitation to come on soon.
Richard
Morgana, I may have found more on our friend Duck.
I was reading the Wiki on the “Inuit Diet,”
https://en.wikipedia.org/wiki/Inuit_diet
when I started to recognize the author(s) peculiar take on the matter.
I went the the View History to learn who contribbed what to that Wiki:
https://en.wikipedia.org/w/index.php?title=Inuit_diet&action=history
There I saw a “JamesPem” (I’ll assume it’s a him) who appeared to vigorously promote that peculiar view in mid-late December, soon after Duck took his leave of us in Rawfoodsos. JamesPem’s voice reminds me very much of Duck’s voice.
I checked JamesPem’s Wiki contrib history:
https://en.wikipedia.org/wiki/Special:Contributions/JamesPem
Lo and behold, JamesPem appears to have the same specific hobby horses we’ve seen here from Duck and which you can find at other fora he contribbed to, including Free The Animal. These HHs include the Inuit diet, carnitine palmitoyltransferase I (aka CPT1, that gene variant that may inhibit ketosis) ,Vilhjalmur Stefansson, ketosis, food fortification, folic acid, and phytic acid.
JamesPem’s Wiki work is not without controversy. A Wiki editor called him on the carpet for engaging in a edit war on food fortification:
https://en.wikipedia.org/wiki/User_talk:JamesPem#Edit_war_warning
JamesPem seems especially keen on “Urine Therapy” which involves drinking urine for its purported therapeutic effects. JamePem put up a spirited case to include it as a valid therapy.
If indeed Duck Dodgers and JamesPem are the same entity, it makes me think he/she may be an individual after all. And possibly someone with a vested interest in urine therapy, given how passionately he/she promotes it in the Wiki Talk forum. –Bryan
wbryanh- wow, that’s fascinating! Yes, that definitely sounds like Duck Dodgers! In fact, back when he was promoting his view on this blog, I became suspicious when- through my googling- I noticed almost everything I found online about the Inuit and ketosis either was written by him (or someone else from Free The Animal), or sounded strangely *like* it was written by him- (aside from the fact that his posts were so highly opinionated; he wasn’t really interested in listening to any other valid counter points that people were making). Yes, I’m even more suspicious now! That last link, where he was accused of using “pseudo science” was particularly interesting. (Also, I clicked on a link about ketosis, where other editors were accusing him of being incorrect; someone mentioned sarcastically it sounded like it had been written by the USDA). Funny…..
Do you have any links where he promotes urine therapy? I couldn’t find any on the links you provided- (am I missing something?) Sounds….er….um….gross, but I’m interested in what he writes nevertheless. Back when i was doing my fasting experiment, I had read online that some people do “urine fasting”. Ugh……Definitely something that I DON’T want to try!
Here you go Morgana:
https://en.wikipedia.org/wiki/Talk:Urine_therapy
JamesPem writes volumes (*ugh*) about Urine Therapy in an increasingly defensive, even petulant, tone to these Wiki colleagues:
alexbrn: https://en.wikipedia.org/wiki/User:Alexbrn
abcedare: https://en.wikipedia.org/wiki/User:Abecedare
jytdog: https://en.wikipedia.org/wiki/User:Jytdog
who appear to grow increasingly frustrated that JamesPem repeatedly fails to support his case that Wiki should treat Urine Therapy as something more than a Fringe Theory.
They take JamesPem to task for:
1) Synthesis
https://en.wikipedia.org/wiki/Wikipedia:No_original_research#Synthesis_of_published_material
which “includes any analysis or synthesis of published material that serves to reach or imply a conclusion not stated by the sources.”
2) Citing belief as evidence (Abecedare: “…lengthy talk page explanations of why you believe this would work is not helpful either…”)
3) Outdated sources
4) Unreliable sources (Jytdog: “…youtube is not a reliable source for content about health in Wikipedia – please do read WP:MEDRS…”)
5) Unnamed sources (eg “…a prominent University professor and glycobiologist who has a PhD in Molecular, Cellular and Developmental Biology on the subject of (auto)urine therapy…”)
6) Self-published sources
7) Irrelevant sources
8) Unsupportable inferences (Abecedare: “…The problem is when you shift from cancer detection to therapeutics, especially in the form of drinking, rubbing or injecting urine…).
9) Use of questionable clinical evidence (Abecedare: “…the use of the most well-known of these biomarkers is now deprecated…”
10) Failure to acknowledge mistakes (Jytdog: “…you did not acknowledge you that mis-described what the expert apparently said. it adds to your credibility when you acknowledge mistakes and it detracts from your credibility when you pretend they didn’t happen….”)
Hm. Yeah.
–Bryan
Very interesting- thanks! Yes, that sounds like “Duck Dodgers”; using obscure sources, the desire to be “right”, not addressing questions or valid points that others have made. I’m surprised you were able to find all this information!
Morgana, I didn’t have to look hard or long. Just stumbled onto that maktaaq trail and followed it for a bit. Seeing lots of yellow snow along the way 🙂
A person may use different handles in different places. But he still has his interests and causes. His voice. His particular way of pressing his points. –Bry
So here is a simple mechanism whereby an uber low-fat diet might prevent heart disease and diabetes.
1. It is known that one substance can prevent heart disease, high blood pressure, and help with diabetes and other diseases.
2. This substance is found in foods, but if often lacking in some diets.
3. This substance can be synthesized in the body, but possibly only in limited quantities.
4. This substance is used up by the body primarily to digest fats.
So what is the substance?
Taurine! It appears to be key in keeping the heart healthy. The amount ingested in the diet varies wildly, partly because it is destroyed by heat. The Inuit likely get plenty, because they eat lots of raw fish. Japanese eat raw fish too, plus octopus which is even higher in taurine. Maasai and French people get plenty because they do raw dairy. Vegans get little taurine, and Americans in general also get very little because everything is well-cooked. However, if there is enough sulfur in the diet, the body can produce it.
Here is the kicker though. Taurine doesn’t get “used up” much in the body. It acts maybe more like a catalyst? The one place it gets used up though, is where it is used to create bile salts to digest fats. So … your uber-low-fat diet wouldn’t have much taurine in it. But it also would not cause the taurine to get used up, because there is so little fat.
Your high-fat diet … if it contains plenty of undercooked fish, meat, or eggs … would have plenty of taurine.
Your average swampland diet would have plenty of fat using up the taurine, but very little taurine in all that well-cooked food. Also not too much in the way of high-sulfur vegies to help synthesize it.
Here is a map of taurine metabolism:
Click to access 128.pdf
And this contains information about taurine excretion in various countries vs. mortality (shades of Ancel Keys!):
https://www.google.com/url?sa=t&rct=j&q=&esrc=s&source=web&cd=6&cad=rja&uact=8&ved=0ahUKEwi2zqzVqvDJAhVXzGMKHf7sBUYQFgguMAU&url=http%3A%2F%2Fwww.springer.com%2Fcda%2Fcontent%2Fdocument%2Fcda_downloaddocument%2F9780387756806-c2.pdf%3FSGWID%3D0-0-45-722329-p173764225&usg=AFQjCNHKTYjeVqom7LwE6ofYBk6spOeOEA&sig2=IAt6zVdoLT5tOnAPjIrn7A
Moral of the story: if you are on a low-taurine diet, it should also be a low-fat diet. Or eat plenty of sushi and don’t worry about it.
Heather, at first glance, very interesting! Reading more
BTW, you recently made some change to cause your lines to run way long and off the right margin. I have to Zoom out the text a lot. Or do a Value-only copy into a doc to read it properly. You may want to take a look at that… –Bryan
Oh, your lines they look fine in the forum, just way long in the emails, but whatever. Basically please nemmind… –Bryan
OK Heather. We’re waiting for your Grand Unified Theory for Macronutrient-Independent Euphagia! (GUT4ME) 🙂
Taurine: LCHF? You’re getting plenty of taurine for your bile function to plough through all that dietary fat. HFLC? Does it matter? Don’t need the taurine (for bile anyway)
Vitamin C/Glucose: LCHF? Carbs are low enough on a low-plant diet that less Vitamin C in the mainly animal-sourced food can still effectively complete with glucose for the GLUT1 transporters. HCLF? You’re eating more carbs. BUT you’re eating more Vitamin C too to better compete with those carbs for GLUT1.
Choline: LCHF? You’re getting lots of choline so your liver can use it to process fats and package lipids. (http://www.marksdailyapple.com/2-more-common-nutrient-deficiencies-and-what-to-do-about-them) HCLF? Lower choline, but also less fat to process.
Anyway Heather there’s a start! –Bryan
Bryan:
“We’re waiting for your Grand Unified Theory for Macronutrient-Independent Euphagia! (GUT4ME) :-)” “Euphagia”! New word! I love it!
Long email lines: HTML and browsers are still “in work” I think. My browser routinely thinks my emails should be the width of both monitors combined. Then they come out with a new release and it’s fixed. Who knows. Probably analyzing the HTML one could figure it out. My emails to this group look ok though in my email box at the moment …
“Taurine: LCHF? You’re getting plenty of taurine for your bile function to plough through all that dietary fat. HFLC? Does it matter? Don’t need the taurine (for bile anyway)”
I’m thinking for LFHC, you don’t need to use up the taurine making bile. This is a WAG on my part, but because of this blog, I started experimenting with uber low-fat eating. The thing I notice is that my “output” changes color drastically, and starts looking more like baby poop. Babies don’t make bile much, and bile is what gives poop most of it’s color I think (unless you have undigested blood/iron). Which makes total sense when I think of it. Bile is an expensive thing, loaded with minerals, and your body tries to recover as much of it as it can. Why produce it if you don’t need it? You have loads of cells to detect the content of foods, and tweak enzymes as needed.
“Vitamin C/Glucose: LCHF? Carbs are low enough on a low-plant diet that less Vitamin C in the mainly animal-sourced food can still effectively complete with glucose for the GLUT1 transporters. HCLF? You’re eating more carbs. BUT you’re eating more Vitamin C too to better compete with those carbs for GLUT1.”
I DO wonder about Vit C. Here is the thing: for much of history (and still) human beings lived on shorelines, either on lakes or the oceans. It reflects in our biology, like our heavy need for iodine, or the shape of our kidneys which allows us to process salt like a camel. It is really difficult to get enough Vit C though, from fruits, even if you live in the tropics. So our ancestors were probably eating a lot of fish and shellfish, much of it raw, because well, it’s easy to chew and tastes good raw. So maybe, unlike the big apes, we started using taurine to do some of the stuff Vit C does?
I’m not sure it even has a lot to do with carbs, for Vit C. A lot of our Vit C is used up handling ultraviolet light and fighting inflammation. This isn’t an issue much for big apes because they have fur. Your average ape or chimp is eating a diet that is almost all fruit and greens. Your average shoreline human would be eating a whole lot of fish, seaweed, tubers, and whatever else grew there. Plus in some places aurochs or other red meat, but that was a lot harder to get.
Choline: Wow, that’s another one I’ve never looked at yet.
BTW, this is something of a personal quest for me. One of the big mysteries in my life is that sometimes, for some reason, I just start feeling awesomely awesome. The last time this happened I was on a cruise ship. It was a horrid cruise. I was there for work, and there was a lot of stress. Plus, it turned out the cruise didn’t have celiac-friendly food so I had nothing much to eat. So I wound up eating most meals in the “Asian” section and living off Phad Thai, Poke salad (with raw fish) and sushi (with raw fish). I was feeling sorry for myself at the time because my peers were eating gourmet food in the dining room. But I didn’t get glutened, which was good. Gluten makes me very, very sick, and that’s not a good thing when one is with work colleagues.
What happened though … I lost 20 lbs in 2 weeks. That simply cannot be *fat*, so it was water, from somewhere. Also I felt wonderful: happy and light and rested. That lasted for another week after landing, but then the 20 lbs came back which was quite depressing.
Ever since I’ve been trying to figure out WHY. There were lots of variables, but “exercise” and “stress” wouldn’t be it (it was a high stress and low-exercise trip). It wasn’t “no meat” … the Phad Thai had chicken in it, and oil. Oh, also I had bacon and eggs for breakfast each morning, along with some gluten-free Wasa I brought with me. Wheat and dairy … I never eat those anyway, so it wasn’t that. Drinking … it wasn’t that. I drank plenty of wine, again feeling sorry for myself having to put up with that trip! Salt … it was a normally salted diet.
But raw fish? Whoda thunk!
Now I’m trying to replicate that, only using taurine supplements, dried squid, cold-smoked mackerel, etc. So far so good. “That 20 lbs” sort of disappeared. I’ve been experimenting with other supplements etc. though so it is again, hard to pinpoint. I don’t know much about what kinds of fish are safe for eating raw (or taste good), but if I’m right that it is the taurine that is the issue, it’s easy enough to try out.
Thanks Heather. “Euphagia” sounds almost like the title of a piece of Ragtime music. Or a name I could give my daughter, and people would think it’s Victorian retro. –Bry
Heather, I’m now reading your post more closely. Very interesting esp your cruise food experience! About poop, did you see this Wiki: https://en.wikipedia.org/wiki/Human_feces Again Wiki’s not an unimpeachable source, but it’s a start. You’re right, our GIs had loads of cells–specifically neurons–to detect what’s in the GI, which then send the info via the vagus nerve back to the brain and hormone regulatory glands. Bilirubin, derived from red blood cell carcasses, may explain poop’s often red-tinged brownish color. Sometimes poop can have a pale color due to too much dietary fat overwhelming the GI’s ability to break it down. OR the GI deemed it some trigs to be excess and simply let them keep wending to the exit.
About Vitamin C, I find it yet another one of the near-imponderables (or merely ponderable?). Apparently, many or even most mammals can still make it–e.g. go terrify a goat (hypothetically speaking of course) and it’ll instantly generate tens of thousands of IUs of C. But we and some (all?) other primates for some reason lost the last step in the 4-stage conversion of glucose to Vitamin C. Probably because we were getting enough of it exogenously, and Nature hates to waste effort carrying out unneeded metab processes. e.g making lactases to break down sugars in milk, hence much lactose intolerance in adults. But goats also eat lots of plants, so why did they retain endogenous C production? About what you say here ”…It is really difficult to get enough Vit C though, from fruits, even if you live in the tropics…” I do wonder: How much C is enough? And under what conditions? E.g. the ancestrally-living Inuit got maybe 15mg/day (US RDI is 90)–mainly from blubber–and yet no suffered no connective tissue deficiency issues like scurvy. Among other possible factors, these Inuit may have had so little exogenous glucose that it minimized competition for the GLUT1 channels. I totally agree, most of our ancestors lives on shorelines. So many ancient shell middens all over the world, in California and the Middle East to name just two places. What you say here Heather: “So maybe…we started using taurine to do some of the stuff Vit C does?…” it could well be plus other anti-oxes too.
It’s pumpkin time for me now, so I’ll comment tomorrow on your cruise ship experiences. ‘Night Heather. –Bry
Looks like I’m going to have to eat more raw herring! I live in north Germany, so that’s one of the specialties here.
Also: I guess lightly cooked eggs- (sunny side up) would have taurine in them? I eat them almost every day, I actually crave them.
Anyway: thanks for all this information about taurine, it’s been interesting.
About eggs Morgana, lately I pan-fry them olive oil “Spanish-style” per this delicious recipe Mark Sisson gives: http://www.marksdailyapple.com/spanish-fried-eggs
It’s the ONLY thing I fry in anything other than coconut oil. And it’s a quick fry 60sec, 90sec tops. These eggs taste so good, I make the exception.
Anyway, my goal is to enough cook the egg white since undercooked white may be inflammatory. Meanwhile leave the yolk almost raw, to max those nutrients. From what I’ve read Salmonella rarely if ever migrates to the yolk. –Bry
wbryanh- that’s exactly how I cook my eggs, except I use bacon grease instead of olive oil. And it also makes the white nice and crispy around the edges. And of course, I leave the yolk nice and runny. Mmmm, I’m getting hungry just writing this……
Morgana, right, sorry bout that! Will save such talk for after your fast 🙂 –Bry
Hey Heather, back to serve up a few Qs/thoughts on your cruise food experience. Mainly, was it the first time you ate raw seafood, or at least so much of it and over consecutive days? I first ate a steady diet of this when I went to Hawaii and chowed ahi poke salad made with kukui nuts morning noon and night (technically the ahi was “cooked” but just chemically, not with heat. Not sure how that impacts taurine content). And yes I felt awesome, but this was Hawaii after all with all its wonderful healthful inputs, sun, coconut, mac nuts, fantastic vistas and frequent rainbows, lots of hiking and swimming, Aloha spirit, far from my JayOhBee, etc. Do you know what noodles they used in the Pad Thai? They were rice noodles? Did you eat a lot of the noodles? What were your carb sources? Fruit? The poke salad and sashimi fish–excellent, esp if very fresh and low on the trophic scale like uni and salmon. Going with the idea you lost a lot of water weight, do you have a sense if you were eating less carb than usual? Did you normally eat bacon and eggs for b’fast before the cruise? If not, what did they replace? Did you drink more wine than usual? About how much per day? Red? White? Other? The wine should be fine to a point, esp if dry reds, those usu have relatively low carb amts, 2–3g per 3.5oz glass. The alcohol can inhibit the liver from dumping excess glucose into blood.
Heather, all that said/asked, I love raw seafood and eat it every chance I get. Except not always raw oysters–even though these usu give me an immediate lift and yes, a certain charge. Too often these popped my BGs into the 120s which I felt went even beyond an expected response to the glycogen content. Maybe some inflammation-driving agents like trace amts of norovirus? –Bry
I have thought about this cruise a lot over the years! The differences were mainly:
1. No beef, nuts, or peanuts
2. More sugar (lemonade+ice tea was available)
3. Probably about the same on carbs. Phad Thai is rice noodles, and sushi is mainly rice with sugared vinegar on it.
4. Probably about the same on wine.
5. Less exercise. I was there to write and teach, and I didn’t have to do housework. There wasn’t anywhere to go outside (there was a pool on deck, but it was noisy and crowded).
6. Way more fish, esp. raw fish.
7. More lettuce (with added oil). Maybe a little more fruit.
8. I ate plenty and was never hungry.
I’ve had lox, dried squid, and pickled herring most of my life. Not as a staple in my diet though! Most smoked fish is too salty to eat as a meal. Asian dried squid though, is a pretty nice snack.
The “water weight” I get isn’t the usual stuff. Lasix doesn’t do much for me. Going on a diet I lose about 5-10 lbs of glycogen weight. But this is more like lymphodema … my legs and upper arms get big, but it looks like fat, not spongy and puffy like water swelling. About 2 pants sizes worth. And I’ll lose that almost overnight. It’s happened several times, but I never pinpointed why.
I suppose I could make poke if I thought about it. Raw ocean fish is supposed to be safe enough, esp. if it’s been frozen (esp. salmon should be frozen). Ceviche is TOO cooked in my book … I’d guess the taurine content is ok, but the water gets squeezed out of the proteins. The best fish is very lightly cooked. Maybe lightly cooking maintains more of the taurine too.
Heather, thanks for the your cruise/non-cruise food compares, interesting!
Looking at your list, really does seem the raw fish makes the major diet diff.
A few things poked out at me:
About #1, do you normally eat peanuts at home? Are the organic/pesticide-free? Per Diet for a Poisoned Planet (Steinman), peanuts are some of the most toxin-laden plants we can eat, including up to 140+ of them. And some are baddies like highly inflammatory and carcenogenic aflatoxins. Inflammatory foods and substances can promote weight gain. In 2009 I replaced peanuts with home-sprouted almonds.
Adding up 2,3 and 7, it seems you were eating more carbs, maybe signif more carbs (sugar is a carb btw so we include #2 here). For many folks like me, that’d promote weight/fat gain, but evidently not for you.
A final thought–the cruise vs your default environment. Maybe simply being out at sea, getting lots of fresh air, helped. In our usual lives at home and in the office, these can be very toxic environments especially when sealed from the outside air, as offices often are. We’re constantly exposed to endocrine disruptors exuding from many things, furniture, additional clothing, carpets etc.
http://toxtown.nlm.nih.gov/text_version/chemicals.php?id=65
“…You can be exposed to endocrine disruptors by breathing, eating, drinking, or touching them…”
http://www.menshealth.com/health/21-reasons-your-house-makes-you-fat
Not suggesting the cruise environment made a large impact on you Heather, but in this modern world very many novel things impact our metabolic health, some with surprisingly quick results. All that said, I’m grateful for you and Morgana getting me to delve into taurine. Really interesting little compound! –Bryan
I agree, the whole cruise environment is SUCH a confounder. I’ve been thinking on this for years and trying to replicate it. The boat also vibrated constantly, and vibration effects genes. One of the times I “felt great” was on another boat (this one a Spanish freighter ship, not a “cruise” exactly!) which was even more “shaky”. Another biggie is I was drinking huge amounts of jasmine green tea. And yeah, I do tend to eat a fair bit of nuts here, so I was thinking that could be an issue. My carb/fat levels vary all over the place, but it doesn’t seem to affect much. We could have mold in our house. I could have family stress. I could be reacting to ultraviolet. I could have lots of things.
But the “aha!” thing for me right now though is that I seem to have replicated the effects by simply taking a couple of taurine+arginine pills each day. So what I am doing now is WORKING which for me is huge. I feel about 30 years younger (I’m 60) and weigh about 20 lbs less. Pretty good for two pills!
Mind you, I’d rather do this via diet, mainly because I think your brain knows what your body wants but it has to taste the food to figure that out. So I’m trying to figure out the culinary aspects of it too, which is interesting. Also I have to figure out if I’ve changed anything ELSE without thinking about it. The taurine seems to change my appetite levels hugely though, and also which foods taste good, which affects my eating habits.
So I’m kind of working backwards, looking at the times I felt good and the times I didn’t, through the lens of probable taurine ingestion. It’s a bit easier for me because I tend to eat the same thing for months at a time, esp. when I’m busy.
Heather, Merry Christmas, Happy Holidays, whichever better fits!
Never heard about vibrations affecting genes. But indeed Google turns up a few things. What are your top links for this?
On the cruise, would you say you drank lots more green tea than usual? Or specifically “jasmine” green tea?
Heather, about what you said about “We could have mold in our house. I could have family stress. I could be reacting to ultraviolet….” I sense maybe you’re suggesting I was moving into an unponderable zone. That at a certain point, we need to draw a line, because what can we do about it all anyway?
If so, I certainly understand your sentiment! Let me try to be clearer. I focus on mitigating the *novel* inputs in my life. Those things, like BPA, phthalates, PBDEs, PTFEs (e.g. in teflon), the burgeoning list of other organo-chlorides and -phosphates, teflon, most of which simply didn’t exist before WII. My operating assumption is that these *novel inputs* can derange our systems because we’ve had no time to evolve to exist healthfully with them. Things like mold, family stress, ultraviolet, and other “legacy” inputs, yes, I worry about them too, but feel we can better manage them when we *reduce our novel inputs*. For example, I used to burn easily in the sun, and not brown easily. Now, since starting my healing journey in 2007, and starting to take more sun starting in 2009, I can spend hours in the sun–always without sunblock–and only brown and never burn. Why is this? Is it possible I reduced my overall inflammation and systemic toxicity enough–in essence I *healed* enough–so that my bod can once again properly respond to even lots of uV as was often the case with our ancestors. In our bods, things rarely if ever happen in isolation. Just about all of our bods’ processes are interrelated. If we improve ourselves at a fundamentally and thoroughly systemic level, everything gets better, our stress responses grow more robust and healing, or so the hypothesis suggests.
It also helps to view it through that ancestral question–how did Ogg/Grok whoever manage the sun? I don’t recall reading about ancestrally living groups that WAP and other who studied–even the tropical and subtropical ones–developing skin cancers and they weren’t slathering on Banana Boat. Per their Wiki, synthetic high SPF sunscreens are relatively new inventions:
https://en.wikipedia.org/wiki/Sunscreen#History
Even into the 19th cen, did we commonly suffer from skin cancers? Hard to say. We always have the diagnosis/lack thereof confounder. But the symptoms of melanoma at least–irregularly shaped skin moles that grow over time that can later itch and bleed–these are easily identifiable symptoms. Early literature may cover them. But I simply haven’t seen it.
But Heather, none of this detracts from your main point–that taurine+arginine appears to be really doing the trick for you! I’m seriously interested in this. Livestrong cites Bodybuilding.com: “Taurine is the second most-abundant amino acid in human muscle tissue…”
http://www.livestrong.com/article/295726-taurine-and-l-arginine/
And its Wiki says: “Taurine … accounts for up to 0.1% of total human body weight…” which suggests that up to 1/1000th of us is taurine.
Sure, none of these sites are unimpeachable sources and of course have to watch out for the usual internet-enabled “consensus effects.” But to me these add weight to the idea that this little oddball sulfonic acid is very important to us. –Bry
Bryan & Morgana:
“Heather, Merry Christmas, Happy Holidays, whichever better fits!”
Oh gads, we SO MUCH need a better name for this season. One that includes everyone. And also the fact that our earth wobbles and how much that affects our lives (esp. us living in Northern latitudes). Christmas has this long and wonderful history, starting with the Celts and Saturnalia, getting banned by the Church and really banned by the Puritans but then adopted as a way to unite the US. And of course adopted by Dickens as a way of getting us to care for poor people. None of the trappings of “Christmas” actually have to do with Christ, but the ideals of Christ’s birth, having hope, renewal, … those are real things regardless of religion. The Christian movement to deny Christmas (as too commercial, and being based on Celtic symbols) … I disagree with that. But the symbols aren’t really the issue, are they?
For us Christmas is a huge deal for all of the above reasons. Plus the fact that our days are super-short and now they are getting longer. Two of our chickens actually went broody today … they KNOW the days have changed and they are dead set on getting a batch of chicks. And attacking me if I gather eggs. There is a Christmas movie based on “How to Train your Dragon” which gets my vote as the best “Holiday Movie” of the year … way better than “Christmas Story” or “Rudolph the Red-Nosed Reindeer” etc.
————–
So much for Holiday Digression! I hope your celebrations is wonderful also.
————–
“Never heard about vibrations affecting genes. But indeed Google turns up a few things. What are your top links for this?”
Stuff like this: http://www.ncbi.nlm.nih.gov/pubmed/20638490 . It does appear that vibrations trigger bone marrow genes to produce less fat and more bone tissue. Why? Who knows? When it gets to epigenetics … a day that is a bit longer makes a hen go broody. There doesn’t have to be much more reason than that! But I have spent a fair bit of my life on boats or trains (my Dad liked to travel) and I know it changes me somehow. So I think about it.
————–
“On the cruise, would you say you drank lots more green tea than usual? Or specifically “jasmine” green tea?”
Jasmine pearls are just the only green tea I really like, plus they are easy to travel with. I have no idea what if any difference the “Jasmine” makes. But the fact I want THAT tea only probably signifies something. They cost quite a bit more than the other green teas. And yet here I am buying them!
————-
“Heather, about what you said about “We could have mold in our house. I could have family stress. I could be reacting to ultraviolet….” I sense maybe you’re suggesting I was moving into an unponderable zone. That at a certain point, we need to draw a line, because what can we do about it all anyway?”
Not so much “unponderable” as that I DO ponder it. For right now though, just taking taurine seems to do the same thing as whatever happened on the cruise. I DO happen to react to ultraviolet, even if it’s from an ultraviolet light, and our house did get mold, and family always has it’s stresses. I’m not discounting it. I’m just amazed that a couple of pills would fix “whatever is going on”. It either means is is just one incredible placebo, or else it is hitting a core problem.
———–
“It also helps to view it through that ancestral question–how did Ogg/Grok whoever manage the sun? I don’t recall reading about ancestrally living groups that WAP and other who studied–even the tropical and subtropical ones–developing skin cancers and they weren’t slathering on Banana Boat. ”
It’s an interesting question. There was one albino chimp … and it got skin cancer and died. Most of the tribal cultures I’ve seen covered up a lot. The darker persons living in the Savannah with no clothes … covered themselves in ochre. Others wore long flowy robes. Others lived in the jungle. As far as I’ve seen, there is no animal without scales, fur, or feathers that spends much time in the sun. Hippos are closest, but they have special excretions in their sweat to counteract ultraviolet.
Human beings though, use Vit C to handle ultraviolet. It uses up a lot of Vit C. Our ancestors in Northern Europe simply didn’t get much ultraviolet. A lot of us appear to be adapted for living in caves. Like: blue eyes. Blue eyes see better in dim light, and don’t function well in bright light. First showed up in Spain, where people were living in caves for thousands of years during the ice ages. Which is also interesting … the Inuit weren’t living in a low-light situation, and they kept the brown eyes. An ice field is very BRIGHT even though there isn’t much ultraviolet.
In the 19th century … sun exposure was a HUGE deal for the upper classes. I was thinking about this in terms of my Grandma. She lived to 96, never got cancer, melanoma, high blood pressure, diabetes. Nothing. But she, like all good women of her time, covered herself from head to toe every day, inside or out. No tan at all. I was wondering how she didn’t die from lack of Vit D. But she did eat fish and mushrooms. Anyway, only a low-class railway worker would be out stripped to the waist, and those guys didn’t live long. Other people “covered” … lots of clothes, big hats. Slaves with parasols in Asia and the Deep South. Burkas in the Middle East. Mind you that cloth was a huge expense at the time, often cost more than your house.
————
“And its Wiki says: “Taurine … accounts for up to 0.1% of total human body weight…” which suggests that up to 1/1000th of us is taurine.”
Exactly! On the one hand, it suggests you certainly don’t need to add it to your diet. On the other hand … people who don’t get enough of it, seem to get very ill. Maybe it’s a bit like water! We have loads of water in our bodies, but yet we easily get too much or too little of it.
And yes, I’m happy this latest experiment appears to be working! It’s still an experiment though, and likely not the last.
Heather, Morgana, Happy Boxing Day! That’s easier to say 🙂
It’s true we need to sort out this/these holiday’s(s’) names. Yesterday I went for a long walk and met lots of people walking (some staggering) off their meals. Do I say “Merry Christmas” and risk appearing a sectarian bigot? Do I say “Happy Holidays” and risk being seen as a PC coward “watering it down?” Maybe I should just say “Merry Happy!”
Heather, thanks so much for the long response. More great food for thought. I’ve long wanted hens, but not allowed where I live 😦 Anyway no pasture for them. Vibration may yet be another novel effect on us I hadn’t thought much about before. It could be an issue for many modern-world dwellers, those who live near busy autoroutes, train routes, and from other sources, like those listed in here:
http://www.thorlabs.us/tutorials/tables2.cfm
Another rabbit hole to dive down into.
You make good points on uV exposure. For sure many ancestrals covered up, like the Bedouins and those you listed. Still, plenty of tribal cultures, like San, many First Peoples in NA, they dressed sparingly. Amazonian tribes even more sparingly, though the jungle canopy shielded those latter groups. While other creatures have protective fur, scales, etc. like you say, we humans diverged from our primate cuzzes ~ 6mil yo and soon thereafter lost most of our poil. Our skin adapted in novel ways, e.g. we evolved many more sweat pores than most other animals. I long thought this was mainly to allow us to persistence hunt–like a few of the San still do:
But maybe the increased sweat somehow filters the uV? Mini rabbit hole.
About early sunblocks, in addition to ochre like you said, I’ve heard about coconut oil, though haven’t seen solid evidence for this. The sunscreen Wiki
https://en.wikipedia.org/wiki/Sunscreen#cite_note-20
suggests things like olive oil and even zinc oxide, through the links the Wiki author(s) cite actually don’t support that either. So idk.
About 19th cen (and before) conventions, it seems mainly a class issue, not a health issue. Woman wanted pale skin to show they were higher register, they didn’t have to toil all day in the fields. Similar reason for why artists portrayed “well-upholstered” women in some early Roman periods.
http://beautifulwithbrains.com/2010/08/06/beauty-in-the-victorian-age/
https://en.wikipedia.org/wiki/Women_in_ancient_Rome
Like your Grandma, my grandmothers stayed indoors and pale and lived long lives, (94, 89). But Heather you must admit SO many confounders here! Esp that in their developing years, my grandparents didn’t face chronic hypercalorism, chronic exposure to novel toxins that exploded into our environment following WWII, and they were relatively well off so didn’t face many of the harsh stresses of poorer people. Poverty killed people in so very many ways besides increased sun exposure. My Dad’s Dad farmed and then golfed a lot and always had a deep natural tan, and lived to 92 with no cancer of any kind. BUT in this you bring up a fascinating point: How did they get enough Vitamin D? In my nutrient spreadsheeting stage, I found D the hardest to get in our diet–at least according to its RDI. That led me to start to take midday sun. But mainly to suspect even more the RDIs, which appears that gov’ts base on a very low bar–no bar?–of evidence. See here:
https://en.wikipedia.org/wiki/Dietary_Reference_Intake#Standard_of_evidence
“…current Dietary Recommended Intakes (DRI’s) were largely based upon the very lowest rank in the quality of evidence pyramid, that is, opinion, rather than the highest level – randomized controlled clinical trials…”
Finally, about taurine, I wonder if we can get tested for it? This link says yes:
http://bodyecology.com/articles/deficient_in_taurine_part2.php
But I can’t find it in labtestsonline or any other site. I’d like to get tested for it. –Bry
A few things in regard to the sun/skin cancer issue- (if I may): according to Dr. Mercola, as well as other sources I’ve read (in books), outdoor workers get far less skin cancer than the general population. Vitamin D helps against skin cancer, but also, it appears that when people are out in the sun a lot, their skin becomes resistant to burning. There’s far more danger with the people who stay pale year round and then suddenly go on a beach holiday and cram all their sun in. The fact that we spend less time outside, the office environment, etc., might have contributed to the rise in skin cancer. I find that with myself, I’m always sensitive in the beginning of the Spring, but if I tan carefully (not too much at once), once I get a “base tan” I don’t burn anymore. This may explain why many hunter gatherer tribes did not have problems. (Aside from the fact that most southern native groups had darker skin).
Also: animal fats generally contain vitamin D, and vitamin D is a fat soluble vitamin, so back in the days of our grandmothers (who probably ate more fat and weren’t afraid of it), this may have protected them from deficiency. The fat and cholesterol lowering campaigns of recent years surely had an impact on skin cancer (as it also takes cholesterol on the skin to make the conversion to vitamin D). Skin cancer seems to be correlated with high consumption of omega 6 vegetable oils in epidemiological studies; though if the oils are inherently detrimental to skin cancer, or if they just replaced more healthy animal fats containing vitamin D (which protects against cancer), is hard to tell.
Also: from my own personal experience, I can say that coconut oil does seem to prevent sunburn! If you try it don’t go crazy of course, use caution, but it does seem to be helpful. Also, if you happen to get a sunburn, using it on the skin greatly diminishes the harmful effects.
Morgana, Heather, again to chime in with n=1, I eased into the unblocked sun like with just about everything else in this incredible health and nutrition journey. 10min each side front and back, then 15, then 20… Now all day and no problems. I few times I got pink, on which I slathered fluid from actual aloe leaves which instantly eased the warmth. Now I’m simply tanned and a little brown. Will I get melanoma down the line? Guess we’ll see in this ongoing lifelong Grand Experiment I’m on. But I do put a lot of faith in our modern bods’ ability to adjust to ancestral conditions when we give them enough time to adjust and when we heal in enough ways. Our ability to cope with unscreened sun may be yet another example of nature’s profoundly intelligent design (no *not* that Creationist creation), in which we get exquisite checks and balances. As we get more sun and thus more potentially damaging uV, that same uV (uV-B) also enables prod of dermal Vitamin D3 which may well protect us from that cancer risk. –Bry
Heather about water-weight loss, just saw this latest reminder in today’s MDA for reasons that might explain it:
http://www.marksdailyapple.com/8-reasons-why-low-carb-diets-actually-work
“…Carb reduction drastically reduces glycogen. That’s part of the reason we initially lose so much water weight on low-carb diets; water always accompanies glycogen…”
It goes to my question to you about whether or not you (intentionally or not) ate fewer carbs on the cruise ship. –Bry
A bit of an addition here …
1, It turns out there is a bit of a change in attitudes about taurine synthesis these days. Yes, humans can synthesize it. But the amount in foods is very important.
“Humans have a low level of CSAD, and, therefore, obtain most of their taurine from foods (4).”
http://www.ncbi.nlm.nih.gov/pmc/articles/PMC2813349/
2. Heat isn’t the issue with taurine. “Cooking” kills taurine mainly because it washes away when food is boiled. There is a very nice set of values for lots of foods here:
Click to access spitze.pdf
(You’ll need to rotate some of the pages: Chrome does with on the right-click menu).
In general, the usual meat sources Americans eat are low in taurine. Despite the name, there isn’t much taurine in beef, though it depends on how it’s cooked and what part of the animal (tongue is pretty high), No taurine at all to speak of in plant foods. There is a fair amount in turkey and duck and some chicken parts (dark meat). Broth can be high in it too. Fish is high though, even canned fish. Juice from canned salmon is super high. So fish or shellfish cooked in broth is good if you also drink the broth.
I’ve always suggested we should study “cuisine” … cooking methods, spices, the whole cheroot … and not just macronutrients. Taurine is one area where this seem critical.
3. There is pretty much general agreement that lack of taurine causes all kinds of skeletal and heart issues, and blood sugar regulation issues, in both humans and animals. (see two links above).
4. The existence of taurine was discovered in 1960 or so, which explains a lot as to why we haven’t heard much about it.
To me this really does leave a big question for the “healthy vegans”. Obviously they do exist, and they all seem to be on an uber-low-fat diet and getting enough sulfur, which may well be the answer.
However, since taurine is easily available as a supplement, it’s easy enough to experiment with! You don’t need to run out and get some dried squid … just get some taurine caps or order the powder online. Or take 5-hour energy drinks or try Red Bull.
BTW, a couple of comments on dried squid. I’ve started snacking on this again (it was a favorite when I was a kid) and it turns out my kids love it too. The white powder you see on the squid is taurine! You can toss it in to a stir fry or omelet or soup, or just eat it out of the bag. There are a lot of different brands, but “Captain Brook” is one that I like.
This is $2.99 a bag at our local Asian store. One bag lasts me several days.
One odd thing though. I’m not one for “pairing” wine and foods especially. When I had some dried squid though, then took a sip of red wine … the wine tasted horrible! I’ve never actually experienced anything like that before. Given that this is sold as a “bar snack” they must be drinking something else with it.
heathertwist- in the book “Deep Nutrition”, by Catherine Shanahan, she explains that native cultures around the world ate very different diets that all had just the right balance of nutrients. Presumably, this was all due to trial and error and finding out “what works”. She lists the things that these different diets all have in common, and one of the things on the list was that they all ate a certain amount of raw food, both plants *and* animals. So these native cultures would have been getting their taurine! Also on the list was the fact that they all ate offal, both raw and lightly cooked. Somehow, these native people knew how to eat healthy. The chronic problems we have today were pretty much unheard of.
I often wonder if “food science” has screwed things up. People do experiments, they think they know something, and they announce it to the public too soon, even if they happen to be wrong (which often turns out to be the case). So often food scientists have a reductionist way of looking at things: they don’t look at nutrition as a whole, balanced way of eating. “Food science” is just in its infancy really, there is so much we don’t know yet! It was probably really the wrong thing to forget the wisdom of our ancestors.
Morgana, I agree totally about the “reductionism”. That is the issue with the whole macronutrient arguments!
The issue I have with most of the “traditional eating” books is that each author has their own bias and they tend to look at the cultures that support that bias. Some of the ancient cultures were and are amazingly healthy. And some were not. Goiter, skeletal problems, bad eyes, gout … our “modern diseases” … were endemic in some places. Dr. Cate seems to be coming from a low-carb bias, which is the norm these days. But there were and are plenty of healthy peoples eating a high-carb diet.
What I’ve been doing is exploring the various cuisines, esp. of the people who seem to be doing really well even though they are living in a more modern culture. This has been fascinating for me, plus it’s an attainable goal. I probably can’t replicate an Inuit or Maasai diet in any case, and I probably wouldn’t like it much. But I *can* replicate Korean or Japanese food pretty exactly, right down to the fish species and vegetable choices.
My “thing” right now is all about taurine, and that gets interesting in terms of cuisine! The Koreans are very much into broths and soups. However, one of the common ones is not a bone broth based on collagen (the typical one people talk about today, which is high in glycine), but one based on kombu, dried anchovies, and daikon. They boil all those together and then discard the solids (or use the kombu in stir fries). Since taurine dissolves in water, this makes for a high-taurine soup. They also use fish to make “fish sauce” and put whole squid in kimchi. So the “juice” is generally used and saved. As opposed to our usual cooking methods, which involve baking in a pan (and the juices drip away).
The Japanese and Koreans are both also very much into mackerel. Mackerel is a typical Japanese breakfast food. Mackerel is one of the higher-taurine fish. If you cook a mackerel by boiling it lightly in the fish broth, it’s like chugging several cups of coffee in the morning, but without the shakes!
heathertwist- In that book, Cate Shanahan was not particularly biased towards low carb. Some of the native cuisines that she included in her list that were healthy were the Japanese and the French, who do eat a reasonable amount of carbohydrates. What she focused on more was that animal foods and animal fats are healthy, and that all healthy cultures ate these things. The book was more supportive of the Weston Price philosophy (which includes both low carb and higher carb diets). Also, she did focus on those traditional diets that were healthy. I guess I didn’t mention that in my first post. As I now recall, she mentioned briefly that not all of the native cultures that Weston Price observed were healthy, but he focused on the ones that were in good health to try to understand why. She talked more about nutrients and the symbiotic relationship of various food pairings, as opposed to isolating one factor (being reductionist). I did not find it biased at all. Well, to a vegan it may be biased, ha ha…..
Heather, great info! I’m surprised the USDA Nutrient Database doesn’t include taurine in its list. I’ll pitch my contact there on it. At least try to get their current thinking on taurine. Also, for some reason LPI’s Micronut Info Center doesn’t cover it taurine either. http://lpi.oregonstate.edu/mic This could well be another example of large orgs being on the trailing edge, though I’ve thought of LPI being more up-to-date than most.
Absolutely agree about examining cuisines. It’s also important to source ingreds for them AMAP like they did gens ago, e.g. pastured-raised animals. Obviously when looking just at the macros and principal micros, they vary greatly, French, Japanese, Indian, etc. and all the variants within those nation’s cuisine. Which point to factors other than these nutrients.
About taurine in “healthy vegans” this may be yet another example of our bods’ capacity to up-/down-reg, purge, conserve and otherwise exquisitely adapt to dietary conditions, even novel ones like strictly plant-sourced foodways that lack historical precedent. Could be for vegans, their bods recognize the need to synthesize more taurine from S. I’m looking forward to one day see real life- and health-expectancy data roll in on vegans, though we may always see confounders, e.g. vegans typically supplement.
Btw, I love tongue with Russian horseradish sauce (sauce recipe in various eds of Joy of Cooking), and long wondered about its health bennies besides being exceptionally rich in mono fat. And, from cans of the full bone-and-skin red salmon, I always drink the broth–it’s delicious. –Bryan
There are some vegans that seem to be healthy, but it doesn’t work for everyone. It seems the healthy ones are better able to make certain conversions in the body- (for instance, beta carotene into vitamin A), but not everyone has the ability to do these things. Taurine may be another example. I think the people who are not cut out to be vegans often stop after a time (another confounding factor?) I tried a mostly vegan diet- (I wasn’t even 100% vegan)- years ago, but that was the worst thing for me! I had many health problems during that time. It does seem to be the case that a select group of people thrive on a vegan diet- at least, I take their word for it when they say they do- and I’m assuming that their bodes are, for some reason, better able to adjust than a great many of us who aren’t able to.
“And, from cans of the full bone-and-skin red salmon, I always drink the broth–it’s delicious. –Bryan”
Yes! Always trust the taste buds! I tell my kids: you have a VERY EXPENSIVE chemistry set built into your brain, and it KNOWS exactly what you are eating and if you need it or not. Just listen to it. The signals mostly sound like “Yummm!” and “Yeccch!”.
I think the reason the databases don’t include taurine is twofold. One, it was only discovered in 1960. It’s a newbie on the block, like Neu5GC, another issue in the making. Second, there are SO MANY variables in it.
Take salmon. If you take a chunk of salmon, put it in a jar, and pressure-seal it, you’ll get some nice high-taurine canned salmon. But most of the taurine is in the juice, so if you are one of those that don’t eat the juice you are out of luck. If you dry the salmon in the sun, you get most of the taurine. But if you make “smoked salmon” … this process includes some brining, some de-salination, some re-soaking, and then some smoking. I have no idea how much taurine is left at that point.
Ditto for beef. Normally if a person cooks, say, chili … you put some ground beef in a pan. Cook it, drain off the juices. Byebye taurine! Also fat. Now add stuff to make chili. Lots of protein in chili. Not much taurine.
Asian cooking, traditionally, didn’t involve skillets or baking so much. They tended to use ceramic pots on fires, and cooked everything together into a stew or congee, so whatever meat or fish was in the meal, the juice ended up in the food. The “meat” was often dried fish or squid, which has taurine as white powder all over it. They also tend to use eggs, which are cracked right into the food so no taurine is lost there either.
Now with dairy … the amount of taurine depends on the animal. Goats have WAY more than cows. I think it also depends on the variety of cow or goat. And then how the milk is handled.
“About taurine in “healthy vegans” this may be yet another example of our bods’ capacity to up-/down-reg, purge, conserve and otherwise exquisitely adapt to dietary conditions, even novel ones like strictly plant-sourced foodways that lack historical precedent.”
I agree, our bodies adapt rather nicely! It actually makes sense too. The places where the diet is mainly vegan also tends to be rather low fat. There aren’t many fats in nature that are not animal-based, that you can get to without heavy machinery. Nuts and coconuts are the only two I can think of offhand. So if you have fat, you have taurine to some degree, if you prepare your food right!
Except for the studies Denise published here, and the Japanese mountain people, I haven’t found many really healthy long-term vegans. There are some famous failures, such as the founder of Bastyr univerisy. Jack LaLanne is one of my heros … decidedly on the bleeding edge of all this and he was decidedly healthy in old age. But he wasn’t vegan, and his “meat” was fish. I don’t know how he cooked it.
There is probably a genetic component too. I have read that some people can process flax Omega 3, while others require an animal source, and this is purely genetic. Inland peoples probably learned to process the plant-sourced version. It would not surprise me that Japanese mountain people are really good at processing high-sulfur roots into taurine (although they also eat fish, so who knows).
Or that most people can go into “vegan mode” as needed? One of the most informative things I’ve read is the Lewis and Clark journals. They documented the food rather carefully, and mostly the guys got something like 9 POUNDS of meat a day. But then they would get no meat at all and live off roots of some sort from the Indians.
heathertwist- Happy Holidays!
I wanted to say that I totally agree with “trust your tastebuds”. I definitely notice this in myself, that my body knows what it want’s/needs. Which brings me to a question: you mentioned that taurine is pretty high in goat’s milk. Is it high in goat’s cheese too? I notice I crave goat’s cheese a lot; this started when I began my recovery after being very ill, after my vegan days. I’ve been curious, all along, what there might be in goat’s cheese that makes me like it so much….(I also eat goat yogurt, but to a lesser extent).
About the Japanese making everything in a pot, and consuming the juice too: apparently, many traditional cultures did that; made stews out of bones or fish, vegetables, etc. This is meant to be very healthy (for more reasons than one). Not eating these slow, old fashioned highly nutritious foods is probably why so many people are in sub par health these days.
Also, in another recent post you mentioned jasmine tea. I drink lots of jasmine green tea; in fact, it’s one of my favorites! I’m inspired now to look it up and see if I find anything about it online. If I find something interesting, I’ll post a link.
Morgana:
On goat cheese, it is in fact the only dairy I’ve ever craved. The one that does not generally give me migraines too. But yes, it is higher in taurine than most other foods. Something like 20 times more than cow milk.
Click to access 10ADGC_Gupta_Taurine%20Rich_Goats_Milk.pdf
But it also might depend on breed. It is interesting, because my grandpa always claimed “cows are for rich people. Poor people have goats”. It seems like goat cheese was THE main protein they had growing up, besides eggs.
“About the Japanese making everything in a pot, and consuming the juice too: apparently, many traditional cultures did that; made stews out of bones or fish, vegetables, etc. This is meant to be very healthy (for more reasons than one). Not eating these slow, old fashioned highly nutritious foods is probably why so many people are in sub par health these days.”
I agree. I think a lot of other cooking methods changed in the 1950’s and later. For instance, when I was growing up, a bit deal in all the women’s magazines was “casseroles” … you put a bunch of stuff in a ceramic thing and baked. it.. Tuna casserole was HUGE. A can or two of tuna, some noodles, some cheese, some milk: cook. In China, they do about the same thing, except they use rice and cook it on top of the stove in a ceramic thingie, and call it something else. In the North East, it’s “Clam chowder”. Paella is pretty similar though. And Cioppino. Stick everything in a pot, and cook. However you look at it, it’s about saving the juices from some tasty seafood. The juices are where the taurine is.
———–
On Jasmine Tea … I’m interested too. I think something else is going on, but I have no idea what.
heathertwist- okay, maybe this is why I like goat cheese so much! Glad to know this.
Here is a link about jasmine tea:
http://www.doctorshealthpress.com/food-and-nutrition-articles/11-amazing-health-benefits-of-drinking-jasmine-tea
Not sure I believe all that, but who knows. Like with many aspects of nutrition, there may be much we don’t know about it yet; i.e., some (as yet) unstudied compound that incurs health benefits? In any case, I know I like it too.
Heather what you say “Yes! Always trust the taste buds!” I agree, so long as that food, we can also *smell* it, which is the major part of “taste.” And at least for those produced aerobically, which is pretty much the case for all ancestrally produced foods like ferments. You can’t taste anything amiss with food tainted with Botulinum toxin, but Botulinum grows only anaerobically, not so common a problem until modern inventions like tin cans and tupperware. For example, the natives who died from eating meats fermented in unvented containers like tupperware:
http://blogs.discovermagazine.com/bodyhorrors/2011/08/14/this-aint-yo-mommas-muktuk-or-fermented-seal-flipper-botulism-being-cold-other-joys-of-artic-living
“…tried and true Alaskan Native methods of burying meat underground to ferment had been modified by the introduction of Western conveniences. Tupperware containers and sealable plastic bags were now being used to create a meaty, anaerobic environment that C. botulinum was happy to vacation in. Oh plastics, you synthetic polymers, what have you wrought!…”
and this here:
https://learn.uvm.edu/foodsystemsblog/2013/05/21/meet-sandor-katz-king-of-fermentation-and-uvm-food-systems-summit-speaker/
“…fermentation… [is] actually relatively safe. Botulism, the most commonly feared bacteria associated with food preservation, can only thrive in anaerobic (oxygen-free) and otherwise sterile environments. The aerobic process used in fermentation encourages “good” bacteria to thrive, thereby out-competing the “bad” bacteria. The result is both tasty and healthy…”
About aerobic ferments, Katz says in his book(s) that your nose knows. That’s my n=1 too. I started fermenting sauerkraut and kimchi in ~2010, now made dozens of batches of each. I always ate it if it smelled fine, even after it sat in the fridge for many months, even over a year. Only once did a ferment smell off, and I tossed it out.
About the many conditions that affect how much taurine we get, I still don’t get why the USDA Nut Dbase folks leave it out. Per its Wiki at least, we IDed taurine in 1827:
https://en.wikipedia.org/wiki/Taurine#Discovery_and_etymology
And if you go to the dbase and look up basic foods–e.g. eggs–you find loads of diff preps, and they simply list the nutrient levels for each prep. The dbase folks try to cover all the bases they can. But if they can’t cover “it all” right in one shot, that doesn’t stop them from covering what bases they can. Thus why they leave out taurine is still a mystery to me.
Back to “healthy vegans,” about what you say “…There aren’t many fats in nature that are not animal-based, that you can get to without heavy machinery…” I agree. I add avos and olives to the list, and we can render c’nut, red palm, and olive oils using very crude tools, but it’s still a small list. A LCHF vegan diet would be a decidedly narrow one. Not that that automatically disqualifies it. Many Inuit ate a narrow diet, and still appeared to thrive. For me, what does disqualify the vegan diet is that you HAVE to supplement. Even the Vegan Gods like McDougall admit vegans need B12 supp. And that’s the very best case. As you (and Morgana too?) point out, we have other conditionally-essential nutrients we can’t get in a vegan diet, which include Vitamin A and long-chain w3s. LaLanne not only ate fish, he supp’ed like mad. But Heather as you ask “…most people can go into ‘vegan mode’ as needed?” I think so. We can store long-term amounts of B12 and to a lesser extent, animal Vit A, and Susan Allport in her book “Queen of Fats” discusses a medical case in which the patient went for years without ANY w3–not even the 18C ALA–until that patient became very sick. –Bry
There are multiple taurine supplements on the market. Outside of health-aimed supplements, it is also present in sport supplements, bodybuilding supplenents.
Yes! So it’s an easy experiment. I made a mix of taurine, arginine, glycine, konjac, and powdered Vit C, and have been taking it 2-3 times a day. What it’s done so far is give me a whole lot more energy and ability to do physical work (my muscles seem stronger). My previously always-cold hands and feet are now warmer. My circulation seems to be a lot better. My digestion is also better … I seem to be able to eat anything without any grumblings.
My 21-year-old daughter started taking it too, and what she’s noticed is that her feet no longer hurt after she is on her feet all day.
Taking JUST the taurine would be better from an experimental viewpoint, but I figure that when one eats fish there is a lot more in it than just fish. Konjac works like “resistant starch” giving slow energy release and keeping the gut bugs regulated.
Apparently taurine can also lower cholesterol, because it prompts the liver to produce more bile. That could also make it easier to digest fats, for people who have that issue. I found a good writup:
Click to access 39541.pdf
Taurine appears to be able to prevent hypercholesterolemia and hepatic steatosis induced by
high-fat and high-cholesterol diets in most animal models. The major mechanism by which
taurine lowers serum cholesterol levels is by increased utilization of cholesterol for bile acid
synthesis. In mice, rats, and hamsters, dietary intake of taurine cause reduction in diet induced
serum cholesterol accompanied by enhanced mRNA expression and enzymatic
activity of 7a-hydroxylase, the rate-limiting enzyme of bile acid synthesis. In normal diets
taurine does not appear to modify serum and liver cholesterol levels.
Dietary supplementation with taurine is indicated to have cardiovascular benefits. The effect
on atherosclerosis appears to be highly dose- and model-dependent. In animal experiments
using high-fat diets to induce increased levels of lipids, taurine has been demonstrated to
significantly alleviate atherosclerotic lesions. The effects of taurine appear to be related to
increased degradation and excretion of cholesterol as bile in the feces and the most common
feature is that taurine increases expression and activity of cholesterol 7α-hydroxylase. Only
a few studies have evaluated the effects of taurine in human subjects.
——-
So not many human studies, but there are epidemiological studies looking at taurine excretion. If future studies show the same thing, then “saturated fat” becomes an issue mainly in that it uses up taurine, when taurine is limited. And easily-digested saturated fats (like coconut oil) become less of an issue than the ones that require more bile. And the fat wars can finally come to an end!
Random thinking about Ancel Keys positive contributions again….The whole reason for the Nations studies was to understand and reduce CVD mortality. In the US CVD mortality peaked in 1968, and has fallen dramatically ever since. Dixon summarizes this in the following link.
Despite the obesity epidemic, and our massive increases in fat and carb consumption, our hearts have gotten healthier. This is a multifactorial effort, involving better therapies, statins, reduced smoking….and diet. The last was Ancel’s part. Trans fats are more or less wiped out (even in the 50’s Keys hated margarine), and the fast food chains no longer deep fry with lard.
As a result of this group effort CVD mortality has been reduced significantly in the US. We now live on average 5 years longer than we used to, even though we are fatter. Heart attacks in 50-somethings are much less common. That’s what Ancel lived for.
Keys gave us the Mediterranean diet, but he also gave us fat-phobia, the diabesity epidemic and statins which enriched the pharmaceutical companies to the extent that they now essentially control both medical research and medical education. In my copy of the Mediterranean Diet, Keys applauds trans fats because they’re less saturated than saturated fats. His ad hominem attacks on any who questioned his ideas, such as Raymond Reiser, John Yudkin and Jacob Yerushalmy, are so vicious and below the belt as to suggest sychopathology.
Every failed cholesterol trial has been presented as successful, suggesting science fraud is rampant, and moreover de Lorgeril points out that every statin trial since the Vioxx affair has failed which calls into question whether there was science fraud in the earlier, “successful” statin trials. As to Keys longevity, the photo of him at the Scripps Institute at 100 years of age shows an obese man (Keys despised fat people) confined to a wheel chair whose asymmetric face suggests a stroke – hardly what you’d hope for after decades on a diet designed to bulletproof the cardiovascular system.
On the other hand, Linus Pauling suggested plentiful vitamin C would make for strong collagen in the arterial wall, while low levels of vitamin C would cause collagen to “unravel” and present lysyl residues – lipoprotein(a) binds strongly to lysyl residues, patching the damage but initiating atherosclerosis. Pauling believed vitamin C prevents atherosclerosis.
I’ve taken between one and five grams per day since 1983. My calcium score is zero and I have minimal intima-media thickening of the carotid artery, suggesting I have no atherosclerosis whatsoever. This would be remarkable in a 70-year-old man – Dr Joseph Kraft remarked that among the thousands of autopsy’s he performed, he had never found a person free of coronary atherosclerosis over 40 years of age, male or female. But wait, there’s more: I’ve been insulin-dependent for 35 years. Freedom from atherosclerosis in a long-time diabetic is unprecedented and has not been reported.
Dr Kraft believed hyperinsulinism caused atheroscelrosis, and he is himself hyperinsulinemic and atherosclerotic. However, restricting carbohydrates to 6% of calories has kept my HbA1c below 5.5% and minimized my insulin levels.
So I believe that plentiful vitamin C and minimal insulin are key to avoiding atherosclerosis, not lowering cholesterol – further, I believe Keys focus on lowering cholesterol has diverted research from the true cause(s) of atherosclerosis and therefore killed more people than Genghis Khan.
@Jonathan Keys did not give us fat-phobia. I lay that, and diabesity, at the doors of agribusiness and the USDA. Keys moved to Italy to consume copious amounts of his optimal monounsaturate, olive oil, with his pasta and bread. In a sense Keys was the good soldier of nutrition, posting himself to a place he identified with CVD health for the last 50 healthy years of his life. Still writing papers at 97.
I regret Keys association with the politician McGovern. That food pyramid they inflicted on us has nothing to do with the way Keys ate personally. But giving us those heart-healthy symbols on dietary rubbish has affected the way agribusiness is run. Diabesity required politicians and agribusiness lobbyists, who used Keys only as supporting evidence.
Interesting about the Vitamin C. I better start eating more oranges and spruce buds.
Read Eat Well and Stay Well. Also read Ferlinghetti’s Coney Island of the Mind. Julia Child. Living to be 100 is a multifactorial exercise.
Careful what you wish for! Here’s Keys at 100 http://survivediabetes.com/Keys.jpg and here’s a Kitavan who Dr Staffan Lindberg believed to be 100 years of age: http://survivediabetes.com/Kitavan.png
Pauling said you can’t get enough C from dietary sources
Jonathan, here’s a few Ancel obits:
http://rawfoodsos.com/2015/10/06/in-defense-of-low-fat-a-call-for-some-evolution-of-thought-part-1/?replytocom=160419#respond
http://www.theguardian.com/news/2004/dec/08/guardianobituaries1
The NYT obit includes this:
“The Seven Countries study…revealed that the Mediterranean diet…was highly protective against heart disease even though the diet derived more than 35 percent of its calories from fat…”
LOL!! For sure Keys’ own dietary narrative evolved! What a diff a few decades can make, no?
Even Keys appears to acknowledge the change. He admitted this (the Guardian obit cites):
“… shortly before his death at 100, when asked if he attributed his longevity to the diet Keys, ever the scientist, replied: “Very likely, but no proof.”
–Bryan
@bryan that’s one thing a scientist does. There’s no vested narrative that is true for all time. You learn to swallow your words, and after a while you realize that there isn’t any pride at stake. Maybe GT’s narrative will change too now that he’s doing actual research at NuSI. He used to write biographies of famous scientists before he became an armchair nutritionist vested in Atkin’s 1970 fictional narrative of the American low-fat diet. There’s hope for him IMO.
“You learn to swallow your words, and after a while you realize that there isn’t any pride at stake…”
Sure Thhq. Whatever you say!
Thanks for setting the example!!
LOL!!!
Jonathan, sorry. For one of the Ancel obits, I somehow copied a Neisy Rawfoodsos link instead of this:
http://www.washingtonpost.com/wp-dyn/articles/A7213-2004Nov23.html
That obit suggests that a broken hip and some strokes hastened Keys’ death. –Bryan
hagiography
As I told acupunturist Eades (and which he didn’t post on his blog roll on Keys vs Lalanne, in which he calls Keys an old drooler): What will you look like when you’re 100?
Of course Lalanne looks better! But then he was in the exercise business AND eating a diet very similar to Keys. Oh wait…he died when he was 95…maybe leaving the pasta out was his mistake.
We know Keys date of birth and death…perhaps Dr. Lindberg has similar records on that Kitavan?
Seriously, my dad only made 88, so it’s not likely I’ll outlive any of them. Or Colonel Sanders, Ferlinghetti or Julia Child. But I can dream anyway.
You miss my point, which is that Keys’ Med diet was not optimuum for him since he developed obesity and CVD, the sequelae of insulin resistance. The Kitavan diet (also high carb, but w/o grains or dairy) is evidently healthier for this Kitavan, who has none of the stigmata of insulin resistance. According to Dr Reaven, the ratio of triglycerides to HDL-cholesterol is a surrogate measurement of insulin resistance – in Reaven 2003, astonishingly, no one whose TG/HDL-cholesterol ratio was less than 1.5 got sick over the six-year follow-up period, while 36% of those whose ratio exceeded 3 developed diabetes, hypertension, stroke, heart disease or cancer.
Exaggerated claims of age are common everywhere long-lived peoples are found. Dr Lindeberg wrote that “Our age estimates were based on known historical events: (1) The arrival of Cyril Cameron, a white man from Tasmania, who established a coconut farm in 1912 and remained on the island until his death, (2) American and Australian military occupation of the area during World War II from 1942-43, (3) The founding of an elementary school in 1962, and (4) Cameron’s death and burial on the island in 1966. Everyone above 35 years of age could clearly remember one or more of these events, and their personal experience matched information from relatives and friends” (Lindeberg 2010).
For anyone who is interested: about Kitavans and their high carb diet: I have read that Kitavans ate only 1 meal per day, in the evening. In fact, many hunter gatherer tribes did this. Before that, they either fasted, or ate minimally. So they used a form of intermittent fasting and were probably in ketosis for quite a bit of the time. That will also affect, in a positive way, insulin sensitivity regardless of the macronutrient content of the diet. (Maybe this is the secret to hunter gatherers’ good health?)
Interesting Morgana! I’d love to see a link on 1-meal-day Kitavans (yes yet another link, I know I’m so demanding :-)) but certainly seems plausible and makes sense. I generally eat in a window, noon to six. –Bry
wbryanh, Jonathanchristie- I originally read it in a book, sorry! And I borrowed the book from somebody, so I don’t remember what it was called. Interestingly enough, I went online to try to support my claim, but I found conflicting accounts. Some people say the Kitavans eat once per day, some say twice. In the link posted by jonathanchristie an actual Kitavan says twice per day, so I would probably tend to believe that. However, it may not be so black and white. In the book I read, it was claimed that they didn’t fast as such during the day, they just ate small amounts of food- a root here, a coconut there- as they saw fit, depending on hunger. Then in the evening they had their main meal with other people. So, who knows. At the very least, we know they weren’t chowing down on 3 meals per day plus 2 snacks. Anyway, that’s why I ended up not posting a link in the end.
My “link search” was fascinating though! What I found is that loads has been written about the Kitavan diet, but everyone seems to be obsessed with just the macronutrient content. Almost nobody talked about meal frequency or overall caloric content, which I should think makes a big difference. (Some commenters on this blog mentioned that people nowadays are obsessed with macronutrient ratios, and I can confirm that!) To be honest, I got a little sidetracked during my search. In reading about native people with high carb diets, it was mentioned that the Japanese practice caloric restriction; i.e., they leave the table before they are full. In the comment section of (if I remember correctly) Gary Taubes’ blog, a Chinese person wrote in and said that in China he/she ate a high carb diet, but when they moved to the States, they immediately gained 20 pounds. In analyzing their weight gain, they concluded that in China- although the percentage of carbohydrate in the diet was higher than in America- through eating more calories (i.e. more food) in America, the actual carb amount was probably higher than in China, even though it was a lower percentage of the diet. I think so often people don’t take these things into consideration. And if a high carb hunter gatherer tribe is eating only once per day; or even twice per day, but minimally early in the day, with the main meal in the evening- this would all have an effect. Basically, 3 meals per day is a relatively recent phenomenon; throughout history we ate 1 or 2 daily meals. (OK, I’ll go find a link for that now!)
@Morgana – You make a point that I often repeat, but I rarely hear anyone else mention. Percentage of carb is largely irrelevant. What matters is the total carb intake. That is because a higher percentage of carb intake could be a lower total carb intake if the diet is OMAD and/or calorie restricted, combined with regular fasting. That is the case for many traditional societies, including some Blue Zones.
How many meals a day do Kitavans eat?
People on the island eat mostly two meals a day. But nowadays, breakfast is mainly comprised of tubers (yam and sweet potato and greens all cooked in coconut cream and salt) and dinner is the same with the inclusion of fish as protein most often. In between these two meals, lunch is seen as a light refreshment with fruits or young coconut only to mention these two popular ones. In between the morning and the evening, we mostly eat fruits as snack or lunch. Generally speaking, there are only two main meals per day, i.e breakfast and dinner.
http://wholehealthsource.blogspot.com/2010/12/interview-with-kitavan.html
Even a relatively higher carb diet that is OMAD is effectively low carb over the whole day. That is because for most of the day they are eating no carbs at all, as they are eating nothing outside of that one meal. And I bet that one meal is not necessarily large. Keep in mind that higher carb as percentage is still lower total carb intake when the diet is calorie restricted and OMAD would definitely be calorie restricted.
Sorry to have confused the esteemed Florida acupuncturist Eades with the ad hominem protein/fat promoter Eades.
Thhq, you’re wrong. Ancel Keys definitely fed fat-phobia:
Click to access 133.full.pdf
“…The reduction … of fat consumption…with substitution of poly-unsaturated for saturated fats, is recommended as a possible means of preventing atherosclerosis and decreasing the risk of heart attacks and strokes…”
This report fails even to completely align with the results of Keys’ own Seven Countries Study! In which he correlates CVD only with *saturated* fat. –Bryan
Where is reduction the same thing as a phobia? Read Margaret Keys 1959 recipes in Eat Well and Stay Well. The main thing you don’t see is butter. Fat is not left out.
As time went on, Keys got much more selective about the fats that he ate in 1961, and by the time he updated the book to the Med diet in the 1970’s the polyunsaturates had been replaced by olive oil. People change with time…we’re citing materials that are over 50 years old in this jib-jab….
Unfortunately governments are not so nimble. Judging from the USDA estimate for 2005, where 35% of the US dietary calories come just from added fats, if you add 15% for the fats that occur naturally in foods, we’re at 50% total calories from fat. Carb consumption is up a lot since 1970, fat consumption is up more. We’re on a high fat, high carb, low protein diet.
So apparently no one is paying much attention to the food pyramid. I don’t see fast food, donuts and chips anywhere on it despite their prominence in the REAL American diet. Agribusiness has rout all the corn and soybeans somewhere. As with ducks and geese it’s like a force feeding…death by Fritos….
Thhq, not sure it’s even that low in protein. It’s a high-everything diet. Including novel compounds.
We most of us know the US food system and dietary recommendations are profoundly broken. The growing popular awareness of that will, sooner or later, rise to a critical threshold. Then this thing will blow up in a big way. We’ll see more than just an endless stream of news report that challenge the status quo for a day or two.
The question is “when?” –Bryan
I think “when” comes down to individual choices to fix individual outcomes. At least until the surfeit of food ends, like it has many times in history. That will fix it for everyone.
Yes, and the current state forces more of us into those indiv solutions or we suffer the consequences. I may well have do fine on HCLF now if other factors–toxins in food and elsewhere in the enviro, chronic low-level stress, skewed glutenin and/or gliadin protein balances in modern wheat and possibly wheat legacy issues too, poor sleep and other chronic and often gross violations of my circadian rhythm, the ubiquity of super-cheap food-like substances engineered to press all our evol hot-buttons. But all that happened and I found LCHF works great and lets me transition painlessly into the occasional longer intermittent fasts I need to do to tamp my BGs back down and onto the right side of the metabolic divide. –Bry
Thhq, when anyone states that lowering dietary fat may prevent the nation’s leading killer (heart disease) from striking you down…Yeah, he feeds fat-phobia 🙂 –Bryan
If my estimate of 50% fat in the current American diet is correct then Keys didn’t exactly induce national fat-phobia. It appears to me that Atkins created an urban legend about American fat-phobia which was not true in 1970, and is not true today, but it always help sell his and his successors books. Beyond that, it doesn’t appear that the Omega 6 fat people are eating is harmful to their hearts or their longevity.
On what grounds do you aver that w6 oils do not contribute to our almost universal chronic degenerative diseases?
Only CVD @Jonathan, only CVD. Other chronic degenerative diseases of all sorts may be up, but CVD rates have fallen as Americans have gobbled up the vegetable oils.
Good point – but CVD’s an inflammatory condition, w6 contributes to inflammation, could not w6 contribute to the CVD that does take place? CVD may be down because of fewer cigarettes smoked …
** slowly smh **
Thhq, you plop out this absurd correlation–CVD rates and veg oil use. As usual, you fail to support it with even a shred of evidence.
But hey, let’s do dueling correlations shall we? When you look at the data, you see a *positive* correlation between veg oil and CVD. At least for CVD deaths. If you go by your penchant to conjure causation out of mere correlation, then veg oils jacked CVD deaths!
CVD deaths started to increase at the turn of the last century. It’s still three times higher since that time: http://www.ncbi.nlm.nih.gov/books/NBK11767/
“At the beginning of the 20th century, CVD was responsible for less than 10 percent of all deaths worldwide, but by 2001 that figure was 30 percent.”
This coincides with the rise of veg oil use. Commercial corn oil hit the scene in 1889: http://corn.org/about/history/ The next big step up leg up in 1911 when P&G intro’ed Crisco. By the 50s, soybean oil become the most popular oil in America: https://en.wikipedia.org/wiki/Vegetable_oil#History_in_North_America
CVD death rate peaked in the 60s/70s–before gov’t official guidelines to cut sat fat and pump up the polys: http://circ.ahajournals.org/content/102/25/3137.full
But Thhq, guess what *did* start to markedly drop since that time? Cigarette smoking! Since the smoking-cancer link became irrefutable in the 1940s–1950s.
Click to access m8_2.pdf
http://www.ncbi.nlm.nih.gov/pubmed/22345227
As you find discussed elsewhere in this forum, lower smoking rates may have reduced chronic disease, including CVD, more than any other single lifestyle change. –Bryan
Correlation is not causation….but do you dispute a drop in the CVD rates @bryan? Or the increase in longevity?
Yes, reduced smoking and better therapies are no doubt important factors.
But the consumption of vegetable oils has been increasing. It’s therefore positively correlated with the health improvements.
Have you ever constructed a multifactorial experimental study? I’ve done it a lot in my career. It’s a simple data sorting tool to pick out the major vs minor effects. The apparent strong correlation between vegetable oil consumption and longevity in a single factor study might completely fall apart when smoking and therapy terms are added to the multifactorial longevity or CVD model.
I would be surprised if vegetable oil consumption remained as an important term at all, either positive or negative. IT’S PROBABLY NOT SIGNIFICANT. And that’s my point.
The thing is, back in the days when people cooked mostly with lard, tallow and bacon grease, heart disease was very rare; almost unheard of. And traditionally, the Okinawans- some of the healthiest, long lived people in the world, with a very low rate of heart disease- used mostly lard for cooking. (I think that might have changed just recently). So there is no logical reason to think that traditional animal fats would cause CVD. And as hydrogenated vegetable oils and margarine became the norm, heart disease increased. I realize correlation doesn’t equal causation…..but I am very suspicious of vegetable oils, particularly because the only way you can make them is by highly processing them. In any case, there seems to be absolutely no correlation between natural animal fats and heart disease, as we have been using these fats for much of our history, and heart disease has only become a problem relatively recently.
Of course olive oil is different from other types of vegetable oils, as the oil in olives can be pressed easily and therefore made in a natural way.
Hi Morgana, great points, thank you. The main reason we switched to veg oil once it became commercially viable back the turn of the last century is that it became very available and *cheap.* When my Dad’s dad worked on his Dad’s farm as a kid, they slaughtered their hogs each fall and got the lard for the year at that time, which they used to make soap and for cooking. They had to make it last. The original Crisco came from cottonseeds which the cotton ginners were throwing out anyway. (“Crisco,” from “crystallized cottonseed oil.”)
It’s a fascinating story how people started to see this landmark veg oil as “healthier” than the animal fats. In short, P&G’s clever PR!
Per this piece:
http://connection.ebscohost.com/c/articles/1804327/mans-most-important-food-fat-use-persuasive-techniques-procter-gambles-public-relations-campaign-introduce-crisco-1911-1913
“One of the earliest, most ingenious promotional public relations tools P&G used to promote Crisco was the creation of Crisco cookbooks. P&G’s cookbooks were in sync with the times, yet this strategy contained the element of legitimacy…”
“Story of Crisco” is possibly the first “advertorial” cookbook ever foisted onto the world. Here’s that very book in all its haut-gras glory:
https://archive.org/details/storyofcrisco00neil
Click to page 10. Near the bottom starts a section titled: “Man’s Most Important Food, Fat.”
Some excerpts:
“No other food supplies our bodies with the drive, the vigor, which fat gives. No other food has been given so little study in proportion to its importance…”
Then the PR-meisters go on to quote this from Fannie Farmer’s book “Food and Cookery for the Sick and Convalescent:”
Click to access foodcookeryforsi00farm.pdf
“…a deficiency of fat cannot be replaced by an excess of carbohydrate.”
HAH! –Bryan
Fascinating! Crisco was also promoted as being “cleaner” and “more wholesome” than lard; I’m not not sure why, possibly because it was very white and didn’t really have a smell. In the links you sent, they also promote it as being “more modern”. Anyway, I have read before that they really had to strongly promote it in order to persuade people to use it, since most people didn’t really have a reason to switch over from butter or lard. And how much more is this happening today? I’m sure all the time, as one sees with the constant persuasion to eat certain foods that are supposedly “healthy”- (that’s the number 1 selling point at the moment, apparently). I’m sure we’re being lied to constantly- it’s all about money- so I take it all with a grain of salt.
Morgana, what you said “Crisco was also promoted as being ‘cleaner’ and ‘more wholesome’ than lard…” yes, it’s what P&G itself said–over and over–in its Story of Crisco!
P&G may have planted the earliest major seed that spawned the wildly growing 20th-cen notion of the inherent superiority of plant-sourced nutrients over animal-sourced ones. Which vegans and many vegetarians ardently flog.
In the “Story of Crisco” Intro, P&G keeps hammering home that notion:
“…you can buy this rich wholesome cream in sanitary tins…it is made in sparkling bright rooms by cleanly uniformed employees…the (factory) walls are made of white glazed tile which are washed regularly…sterilized machines handle the oil…no hand touches Crisco until in your own kitchen…**there is today a pronounced partiality from a health standpoint to a vegetable fat**… the lardy greasy taste of food resulting from the use of animal fat has never been in such disfavor…Crisco is absolutely *all* vegetable… Crisco is a manufactured fat where quality and purity can be controlled…” And on. Near to the end of its Intro.
P&G’s “clean” and “pure” emphasis tapped straight into an exploding zeitgeist. Turn of the last cen, people were becoming clean freaks. The concept of “asepsis” arrived to hospitals only a few decades earlier in the 1870s:
http://www.cumc.columbia.edu/psjournal/archive/spring_summer_2008/surgery_in_america.html
The passion to “disinfect” really took off after 1908, when a Jersey City official was the first to add chlorine to municipal water to make the water “pure and wholesome.” Which of course it worked spectacularly well. A few folks started Clorox five years later (1913) to bring this wonderful disinfecting power into our homes, and of course became a hugely successful company.
https://en.wikipedia.org/wiki/John_L._Leal
Maybe this surging zeitgeist helps explain why “pure white sugar” and “pure white flour,” which really became affordable and surged after the Great War, held such strong emotional appeal?
My gg- and g’parents murdered every microbe in reach. My step-mother still does, wielding an arsenal of antimicrobial chemicals.
Morgana, this concept may have hit its apotheosis in the 90s and 00s, with Triclosan-laced antibiotic soaps, and even clothes. Antibiotic “everything.” This, until our knowledge of the microbiome started to take off and we began to wrap our minds round the idea that some microbes might not only be benign, but actually vital to our health. –Bryan
Lots of great information there, thanks! Although I was vaguely aware of it, I guess I never quite “put it all together” that at that time in our history, there was an obsession with cleanliness and purity. It explains a lot though. Indeed, how times have changed with the discovery of the microbiome!
You’re welcome Morgana! In the Belle Époque (Industrial Rev to the start of the Great War)–the time all my grandparents were born into–we saw tremendous transformations in society. We urbanized like never before, which compelled and spawned entire new movements and fields, from modernism (eg abstract art) to psychotherapy to public relations. (And the last two have a connection. Edward Bernays, the “father of public relations”–e.g. the Mad Ave guys–was Freud’s nephew.)
https://en.wikipedia.org/wiki/Edward_Bernays
And yes the creation and mass production of novel foodstuffs. Before 1900, “oleomargarine” was the main synthetic food. All my grandparents still called it “oleo.”
It was such a disruptive time, it instilled such a weird blend of excitement for the future and deep existential angst, it’s no wonder people clung to neat and clean and simple shiny white things. Like the perceived snow-white purity of Crisco.
I was lucky to have three of my grandparents until my late 30s. By which time I’d taken an interest in their lives, including what they ate and how they got their food. This gave me a sense of their transition, from where we came and how profoundly different their early years were, not all that long ago. That made me ever more grateful they lived long rich lives. –Bryan
Morgana, sorry, I meant to carry my Belle Époque comment to this point: the subtle yet profound and enduring power of public relations to shape public opinion and conventional wisdom for decades afterwards, including our food views. Which can, in turn, help drive public policy, like the disastrous US food policy that took shape in the 60s and 70s. Many people believed–and many still do–in the reputed superiority of veg fats over animal fats. When and where did that notion start? Could it be P&G’s PR “creative” flaks were the great-grandparents of that enduring CW?
Another example “An apple a day keeps the doctor away.” We all parroted this adage as kids, right? Of course few of us had no idea where it came from. But we assumed it came from “doctors.”
Some say it’s a Welsh phrase from the 1860s:
https://www.washingtonpost.com/lifestyle/wellness/history-behind-an-apple-a-day/2013/09/24/aac3e79c-1f0e-11e3-94a2-6c66b668ea55_story.html
Maybe so. But what gave it such currency, such popularity? In Botany of Desire, Michael Pollan makes the case this adage is another PR coup to bail out desperate apple orchard owners pre-Prohibition:
http://www.pbs.org/thebotanyofdesire/apple-sweetness.php
“…Bitter apples, planted from seed instead of grafted, were used by homesteaders across the young country to produce hard cider—until a national campaign against alcohol threatened Americans’ relationship with the apple. But with the help of early public relations pioneers crafting slogans such as “an apple a day keeps the doctor away,” the plant quickly reinvented itself as a healthy foodstuff.”
But is this immense PR power just a 20th century phenomenon? Now, in the 21st cen, with everywhere interest and lots of CW-debunking tools like Snopes, TruthorFiction, Politicifact, etc, will we see the power of PR peaked and now headed down? Anecdotally I know that, since the ’00s, many of my friends and family have gotten a lot better about fact-checking stuff before forwarding it to me. I guess in time we’ll see the true effect of new developments like these fact-check sites. –Bryan
Well, yeah, there’s that…..maybe it’s not the right place for me to mention this, but I believe there are powers out there using mind control to try to control our behavior…..I think there is an agenda out there! Sure, part of the motivation is for certain groups to make money, but I fear there may be something more sinister going on. I have become highly skeptical of almost everything. I think much if what we humans think we “know” is actually disinformation! (In addition to the fact that we know so little about so many subjects, like nutrition for example, or even how the body works). Much of what has become “fact” is based on old wives tales.
On another subject though, it was interesting to read about the history of apples. It reminded me that nowadays I find apples too sweet for eating. It was mentioned that they used to be sour; in fact, even when I was a child, apples had more tartness. This begs the following question: do more people have fructose malabsorption nowadays due to the unnatural breeding of sweeter fruit? (Fructose is easier to absorb for people with that problem when the fruit has an equal proportion of fructose to glucose). Since fructose is the part that gives it the “sweet” taste, I wonder if creating sweeter fruit has exacerbated the problem? (In a similar way to modern wheat exacerbating the problem of gluten sensitivity and celiac disease?)
Morgana, I’m not sure how much our world tends toward some Matrix-like future. But I agree, if we don’t always always question and dig ever deeper into our research, if we don’t revisit *everything,* then we could end up “knowing” a whole lot of disinfo! As I felt I had up till about age 46. The last nine years have felt like a long process of unpacking and unwinding that load of disinfo along with my metabolic syndrome.
In the first few years (2007– ~2011) of my T2D-unwinding lifestyle and nutrition journey , what struck me first was to discover to how great a degree the multinats like Monsanto, ADM, Cargill, Merck, Pfizer, etc. appear to own the global nutrition and health conversation. There truly seems to be a “consensus science” a kind of at least partially unspoken collusion between these entities to give us and the government consistent “science”-backed messages. When I thought more on this, though, this makes sense, and yes, money plays a huge role, bigger than I first appreciated. So does recognition.
The big problem these days, at least in NA, is that tax-starved governments have greatly cut their funding to research. This left researchers to seek funding from the well-healed multinats. This forced even erstwhile reputable people like Dr George Fodor at Ottawa Heart, who sat on many national cardiac health committees, to seek megacorp largesse to fund their research. Of course he would feel pressure to deliver the results these megacorps want. Maybe the corps don’t outright *say* to the Doctor “give us results X or kiss your bucks bye-bye.” They don’t have to. It’s understood if he doesn’t deliver some minimum of what they want, they dial down the funds.
So how do these researchers, many of whom start their careers with high ideals, come to terms with this grim reality? Perhaps these researchers justify it by telling themselves that they will somehow work in other truly meaningful research that *will* change the world for the better, not just for the worse, and that the hoped-for net positive effect justifies the means, plus they’ll get a shot at the Nobel Prize. Maybe they justify it by telling themselves the smart ones will figure it out anyway, and even carry this idea to a dark extreme, to say to themselves, “hey, the smart ones will see past it anyway so I’m contributing to positive Darwinian natural selection, so that’s all for the good, right?” Morgana, I really couldn’t say what all are the possible motivations and increasingly strained justifications. As usual, there are many such drives, and they vary by the individual. But the level of collusion in the mainstream corp-backed “science” research community–to whatever degree it is spoken and unspoken–well, that collusion appears breathtaking in its depth and unity of purpose. From the huge and growing ream of “consensus science” — e.g. 2000+ “studies” to show GMOs are “fine”–to the phalanx of social media trolls you find on every SM site eg,
https://www.facebook.com/GenMods4Monsanto
and in almost every forum, at least the many fora I visit, to the paid-for GMO- and glyphosate-loving mommy bloggers. All of whom adhere to a remarkably consistent playbook, eg all link anti-GMO people to anti-vaxxers, that they adhere to “evidence-based” research, that they “are deluded by hysterical cranks like the Food Babe, Mike Adams at Natural News, and other controversial figures who make themselves easy targets. You never know who will get drawn over to the dark side, e.g. one thinks of the former anti-GMO activist Brit Mark Lynas.
http://www.theguardian.com/environment/2013/mar/09/mark-lynas-truth-treachery-gm
It’s almost like these very large corps tend toward stateless nations that cover the world, at least the Big Food/Big Pharma complex, with their enormous resources, with capitalizations that exceed some countries GDPs, with enormous ability to pervert and thwart the truth and keep us unhealthy and in their thrall. –Bryan
I grew up cooking with Crisco, and I have to say it DID do a great job. Far easier to use than butter or lard … it was always at the correct consistency. And made a wonderful crispy pie shell. Nice frying oil too. It really is a pity that the hydrogenated oils turned out to be unhealthy.
The science behind hydrogenation is similar to the reasoning behind those that avoid PUFAs. Polyunsaturated fats go rancid easily … saturated fats don’t. And using a mix of oils, you can get exactly the correct consistency and ability to work at various temperatures.
I think we’ve built on those early food sciences though. The more modern margarines use the same idea, but with a different mix of oils (like palm oil, coconut oil). Some of them, like Earth Balance, are quite yummy and good to bake with.
The story of margarine’s invention is pretty interesting! It started in 1813, in France. The original version used beef tallow and milk, and the idea was to give the poor people an affordable substitute for butter. The dairy industry though, fought it:
“They were predictably more than a little irked. Butter was big business, and the notion that a cheaper substitute, even one made in part with milk, might storm the market terrified dairy farmers. They didn’t take the threat lying down, though, and convinced legislators to tax margarine at a rate of two cents per pound—no small sum in the late 19th century. Dairy farmers also successfully lobbied for restrictions that banned the use of yellow dyes to make margarine look more appetizing. By 1900, artificially colored butter was contraband in 30 U.S. states. Several states took even more extreme measures to turn consumers away from margarine—they required the product to be dyed an unappealing pink color.”
http://mentalfloss.com/article/25638/surprisingly-interesting-history-margarine
My Mom said that no one liked the original version because it was white. It was packaged with a little packet of yellow dye though, and they smooshed the dye into the margerine so it looked more like butter.
Crisco, on the other had, came about because in the late 1800’s, there was a shortage on pig fat during the civil war. Proctor and Gamble were looking at alternatives, and originally, came up with coconut and palm oil. Then they invented hydrogenation, so liquid oils could also be used also for making candles and soaps. Crisco was a sideline, but it took off. It was marketed, among other things, as “The Hebrew Race has been waiting 4,000 years for Crisco!” (it’s kosher) and “It’s all vegetable! It’s digestible!”.
Heather, very interesting, thanks! What you quote: “The Hebrew Race has been waiting 4,000 years for Crisco!” (it’s kosher) and “It’s all vegetable! It’s digestible!” – all straight out of the Story of Crisco cookbook. (page 19)
https://archive.org/details/storyofcrisco00neil
My Mom loved using Crisco for the reasons you give, such as its even consistency. And that she could toss the tin back under the sink after dipping into it.
Actually, P&G seemed to want to hydrogenate the cottonseed polys just up to the point of our main dietary monounsaturated fat–oleic acid. Here from page 20:
“To understand something of the Crisco Process, it is necessary first to know that there are three main ingredients in all the best edible oils:
Linoline [Linoleic acid = LA = 18C w6 poly]
Oleine [Oleic acid = 18C w9 mono, our main dietary mono fat]
Stearine [ Stearic acid = 18C sat fat]…
Linoline, which has the lowest percentage of hydrogen, is unstable and tends to turn rancid.
Oleine is stable, has no tendency to turn rancid and is easily digested
Stearine is both hard and indigestible.”
So P&G aimed to make *mono fats* in its Crisco. Except to also make these mono fats *trans* fats instead of nature’s near-default cis configuration, so as to allow Crisco to stay smoothly solid at room temps. (The trans config allows a “straighter” molecule so they pack together more tightly, raising the melting point. See the diagrams here:
http://chemistry.tutorvista.com/biochemistry/trans-fatty-acids.html
(Scroll down to see the trans-oleic and cis-oleic diagrams)
And more info here:
https://en.wikipedia.org/wiki/Trans_fat
But Heather this raises the Q: Is Crisco that bad for us? If so, why? Is it due to these trans-mono fats? Or due to lots of leftover unhydrogenated polys that sit in the Crisco matrix and rancidify, but somehow we can’t detect them?
I’d love to see actual direct clinical evidence to show trans fats are bad for us. I’ve readily believed it, given that nature generates few trans fats, and because that’s the overwhelming CW on it right now (CW can be terrible reason!). And of course we have “loads of epidemiological evidence” to show trans fats are bad for us. But we know the severe limitations of those purely correlative studies. But where’s the actual clinical proof that trans fats are bad for us? I haven’t been able to accept this from a pure biochem viewpoint. Do trans fats need insulin or can we import them to the mitochondria just like cis fats? Can we beta-oxidize trans fats the same way as cis fats, feeding the acetyls into the Krebs Cycle as normal? Can we vet trans fats in our GIs the way we can vet other fats? I’ve never seen any yea or nay on any of this.
About what you say “Crisco, on the other had, came about because in the late 1800’s, there was a shortage on pig fat during the civil war. Proctor and Gamble were looking at alternatives…” Yes, Cincinnati, P&G’s home city, was once known as “Porkopolis” when Cincinnati was the country’s main hog packing center so there was huge local interest to come up with an alternative. –Bryan
I suppose non-natural trans fats *could* prompt an immune response. Which, if we eat these fats regularly enough, could raise the risk of chronic inflammation. Which can foster chronic disease like CVD.
But I’ve heard mainly that our immune systems respond to unfamiliar *proteins.* Like those under the gluten rubric. And, to a lesser degree, the caseins. At least the cow caseins. –Bryan
Morgana, meant to add, olive oil and red palm and avocado oils, these are fruit oils and low in pufa. Coconuts seem harder to classify. This is the one of the better defs I’ve seen:
http://www.loc.gov/rr/scitech/mysteries/coconut.html
“…a coconut is a fibrous one-seeded drupe, also known as a dry drupe. However, when using loose definitions, the coconut can be all three: a fruit, a nut, and a seed.”
The main point: Olive, red palm, avocado, coconut, all these are low in pufa.
When I say “veg oil” I mean nut/seed/legume/grain oil. Which are major w6 pufa bombs. –Bryan
Thhq, you ask: “Have you ever constructed a multifactorial experimental study? I’ve done it a lot in my career…”
The answer is yes. I did this on a regular basis to analyze specific target markets for technology for consumers and small businesses.
Thhq, you talk a good game. And I like some of your cultural observations suggesting a well-traveled person. But you seem neither to understand this topic with much depth nor possess strong analytical skills or even some basic principles of the scientific approach. You routinely commit the rookie researcher fault of not giving your sources. Indeed, you expect people should just *trust* what you say. You get wrapped up in your views of the personalities in the nutrition field like Gary Taubes. You trash GT and his book Good Calories Bad Calories without having ever read it. You talk against the low carb diet as a long-term foodway approach, yet you can’t even define for us what “low carb” means. Until recently, you even confused lipoproteins, lipids, and cholesterol.
Forgive me thhq if somehow I’m not sold on your knowledge of this field or your dispassionate agenda-free analytical skills you regularly suggest to us that you have.
All I see from you is *agenda.*
Which brings us, thhq, to your latest assertion:
“I would be surprised if vegetable oil consumption remained as an important term at all, either positive or negative. IT’S PROBABLY NOT SIGNIFICANT.”
Sure thing thhq. You give us yet another fact-free opinion. A view utterly unencumbered by any evidence you offer, which is–surprise!–zero evidence. And which is completely at odds with our evolving knowledge of basic human biochemistry which finds that yes, high w6 PUFA–for which veg oils are by far the greatest source–*can* actually harm our long-term health.
http://chriskresser.com/how-too-much-omega-6-and-not-enough-omega-3-is-making-us-sick/
“…several clinical studies have shown that decreasing the n-6:n-3 ratio protects against chronic, degenerative diseases. One study showed that replacing corn oil with olive oil and canola oil to reach an n-6:n-3 ratio of 4:1 led to a 70% decrease in total mortality…”
http://www.ncbi.nlm.nih.gov/pmc/articles/PMC4433071/
“Ready-to-use therapeutic foods (RUTFs) are a key component of a life-saving treatment for young children who present with uncomplicated severe acute malnutrition in resource limited settings. Increasing recognition of the role of balanced dietary omega-6 and omega-3 polyunsaturated fatty acids (PUFA) in neurocognitive and immune development led two independent groups to evaluate RUTFs…reduction of RUTF omega-6 linoleic acid … improved DHA status…”
Thhq, at this point, I’m afraid my reflex response to your comments is that they are based on spurious belief and confirmation bias, not actual science.
–Bryan
Thhq, I’ll add that you sometimes fail totally to comprehend what others write.
You ask “…do you dispute a drop in the CVD rates @bryan? Or the increase in longevity?…”
Well yes I do thhq! And I DID explain just that in my last post!
Did you not read any of that? Don’t you remember that?
And this you say: “But the consumption of vegetable oils has been increasing. It’s therefore positively correlated with the health improvements…”
Here you just drone and intone your party line. Even though, thhq, in that post I gave you highly-sourced evidence to the contrary.
Thhq, you are so committed to your agenda you can’t even absorb any dissenting views. Evidently, to you, these views are just a mere confused jumble of pixels on your screen. –Bryan
ahhh the caffeine’s at full effect now @bryan
You have said that your career was as a journalist, much like GT’s. My career was as a scientist. When I talk about multifactorial studies and abstracting I’m talking about tools I used in my trade. I got paid very well to do that. I can understand where Ancel Keys is coming from much more than where journalists come from. While I did not conduct the starvation study or 7 Nations I’m familiar with the methodology. If you want to play, go back 35 years and start over in a hard science. Or start your own NuSI. But don’t belittle my craft using high school debate tactics. I didn’t see you in Cargill’s lab 10 years ago when I was studying the water-repellant characteristics of the fully hydrogenated high melt soy oils, which are used to make french fries glisten. You’re an amateur.
If we talk about monofixations, yours seems to be GT. I had to press you to even check out a cc of Cordain’s Paleo Diet at the library (I’m still ticked about having to type out passages from the book for you, then take your criticism for not typing out the whole book), and you’re in heavy avoidance regarding reading Ancel Keys. Afraid you might be corrupted? Yours is a pretty strict HFLC party line I must say.
I’m in this for understanding longevity, not just CVD rates. Going down the no-Crisco path you’re only covering the same ground Ancel Keys covered in the 1950’s (though he disliked saturated fats of all kinds, not just the ones made by hydrogenating vegetable oils). This is a single factor, and there are more factors in longevity than diet. I’m interested in Keys primarily for his longevity, but I’m just as interested in Jack Lalanne and Lawrence Ferlinghetti. In the ultimate multifactorial model, diet macronutrients may not even be a significant factor. We’ll never see that model, only a string of N=1’s in the cemetary. Having thought and read about this for the last 9 years, I think that high activity (physical and mental), not smoking, and access to modern medical treatment are factors of greater importance than eating a HFLC – or vegan – or Mediterranean – diet.
Since you’re heavily vested in the great man, and I haven’t read his books, how does GT explain the high number of Okinawan centenarians? I typed out Cordain for you. Do me a favor and type out some GT. Keep it on topic.
Sure thhq. Whatever you feel you must say here. Which btw, not all of which I disagree.
I’m not at all surprised to read this from you “…I didn’t see you in Cargill’s lab 10 years ago when I was studying the water-repellant characteristics of the fully hydrogenated high melt soy oils, which are used to make french fries glisten.” This your experience could help explain your bias toward veg/legume oils.
Actually thhq it explains a *lot.* You, a product of corporate science research, do nothing to lessen my already dim view of those folks who, more than ever, generate the best methodologies and do the finest p-hacking to deliver the best results big corporate bucks can buy. To help generate that exploding ream of “consensus science” that Monsanto, Cargill and others depend upon to justify their products that make people unhealthy and kill them sooner.
If we were corresponding 70 years ago, R.J. Reynolds might well have been paying you handsomely to ardently defend cigarettes with “science.”
So sure thhq, promote your CV all you want. I will just let the things you have said here–and have stoutly *refused* to say here–be our guide. –Bryan
Still waiting on those GT quotes @bryan. I want to see him defend sweet potatoes, or pork fat, or something, in the Okinawan diet.
I didn’t intend to get an education on hydrogenated frying fats that day in Minneapolis. I thought I was dealing with an industrial product, until I saw the chef’s head on the sack of yellow flakes. Melt point 160F – makes tallow (which I also had the pleasure of testing elsewhere, in a similar context) look like health food. When people quit buying trans fats like margarine and Crisco, those hydrogenaters went idle a lot of the time. And what else could they be used for? Paraffin replacement maybe…which is where I came in…
So in a day I got a glimpse of what fast food deep fat fryers run on. But not because I planned to.
Thhq, you say: “Still waiting on those GT quotes @bryan. I want to see him defend sweet potatoes, or pork fat, or something, in the Okinawan diet.”
Hm. Why do you ask for these quotes? Why would they be at all relevant here?
Where do I ever say Taubes gave the final word on macronutrient balances? That LCHF is the *only* way? Whatever you understand LCHF to even mean. Because I sure don’t what you mean by “low carb.” Thhq, you don’t even seem to know what you mean by “low-carb.”
If you can quote me saying anything like the above, we can go from there.
But you won’t find that thhq. You *can’t* find that. –Bryan
While you’re at it thhq, why don’t you share with us what you think the “Okinawan Diet” is? With foods, total calories, macronutrient counts and balances, vit and min counts? You know, pesky things like actual measured data points. Things you seem to hate to deal with.
Thhq, only if you want to give that, of course. In case you actually want us to know what it is you’re talking about. Thanks –Bryan
Sigh. @bryan once again I’ve had to answer my own question. You had your chance, but we’ll start with what I can get for free. There’s a lot here for you to like (you’ll love the sugar-bashing), but I’m only trying to answer my longevity-related Okinawan question from the writings of GT without giving him my cash. What he has to say is about Japan, but I’m taking what I can get.
https://proteinpower.com/drmike/2008/11/17/gary-taubes-responds/
First, we see GT acknowledge the importance of brown rice in the Japanese diet prior to 50 years ago:
“In the case of Japan, for instance, the bulk of the population consumed brown rice rather than white until only recently, say the last 50 years.”
Second, we see GT acknowledge that the Japanese traditionally ate a low fat diet:
“Some of these traditional populations ate high-fat diets (the Inuit, plains Indians, pastoralists like the Masai, the Tokelauans); some ate relatively low-fat diets (agriculturalists like the Hunza, the Japanese, etc.)”
So I got my answer. GT has some caveats about eating the right carbs, but he’s at least agreeing on the LFHC diet composition the Japanese were eating during the 7 Nations study, when they had such low CVD rates.
There’s no need for you to reply. GT has spoken.
Thank you thhq, good work!
So how does any of this depart in any way from anything I’ve said before?
Oh and about what you say “we’ll start with [the Taubes info] I can get for free…”
Thhq, just curious. Why wouldn’t you just borrow the book from the library? –Bryan
Now what constitutes this Japanese diet? I found a full text of the Keys and Kimura article on southern Japanese middle aged farmers, though nothing on the other heavily studied Japanese groups (a report on the fishermen would be interesting to see). Also nothing on the specific foods, since they were pulverized for analysis, but a lot on the macros.
https://www.researchgate.net/publication/17752837_Diets_of_middle-aged_farmers_in_Japan
80% carb, 11% protein, 9% fat. There’s also 6% alcohol, but it’s not reported whether this is included in the carbs. About 2400 calories a day for men who weighed about 130-140 lbs and were reportedly very active. This is the best definition of the traditional Japanese LFHC diet I can find. Deeper digging at UMinn would probably turn up the lists of foods eaten.
I’ve found you can get a pretty good idea of what goes into the diet by looking at the contents of the grocery stores too, and/or a knowledge of the typical recipes and history. I expect your numbers are about right. When I “eat Japanese” by following typical meal plans, it comes out mostly carb, with a fair bit of protein, and not much fat. Like here is a typical breakfast:
http://j-simplerecipes.com/mealtype.html
http://japanesefood.about.com/cs/styles/a/breakfast.htm
And then if you watch Japanese movies (we do) then you see what is considered a typical family breakfast, which is pretty much just you see there. So I figure yeah, that is typical and traditional. When every cookbook and movie agrees, it’s probably fairly accurate. Spending time with some families helps too.
But for stuff like taurine … there are so many variables that you can’t really tell how much the person is ingesting. One species of fish is way different from another. And if the fish is processed one way, it is high in taurine, but if processed another way, it is very low. When it comes to longevity, taurine is really key.
Ditto for iron. A meal can be very high in iron, and yet almost no iron goes into that person’s system, depending on the food mix and genetics.
So the way you can test for taurine is how much is excreted in the urine … that reflects how much is in the diet. For iron, you have to test the entire load in the body (which requires an MRI: even ferritin isn’t a good marker).
I don’t know of such a marker for fat though. And the absorption rates for fat varies by the individual’s needs. The body can create fat just fine … except it needs small amounts of “essential” fatty acids … so is there a way to measure what fat comes from the diet, and what is manufactured?
It’s pretty much a standard thought that when Americans eat Japanese food, they lose weight. If Japanese eat American food, they gain weight. But no one has really pinpointed the variables. I’ve been trying to do that by actually *eating* Japanese food and tweaking the variables. The thing I immediately noticed is that I started eating less. Not because of some rule (“eat til you are 80% full”) but because I WAS full, darn it. Try starting the day out with some grilled mackerel and see what it does to your appetite later in the day!
Anyway, the Japanese diet is one of the most documented diets EVER. Easy to experiment with too … cheap and easy to prepare.
Heather, this USDA article discusses how, the higher up the evolutionary tree the primate goes, the more cystine (–> taurine) that primate has and needs. And which it requires esp for brain and eye development and maybe the maintenance of these organs.
Btw, “cystine” appears not to be a misspelling. Each cystine comes from two cysteines, semi-essential amino acids.
https://en.wikipedia.org/wiki/Cystine
Click to access milk0598.pdf
“…why are some amino acids present in different ratios between species? While all primates—humans, chimps, and apes—have very similar milk components, human milk has the highest cystine content, with the great apes coming in second. Cystine is believed to play more of a role in body maintenance than in growth. So Davis and Reeds reasoned that the high cystine levels reflected the fact that human and ape babies take longer to mature than their primate relatives. In fact, the closer any two animal species are on the evolutionary tree, the more likely their milks are to be similar. Enter Miller’s elephant milk: Davis and Reeds wanted to know if elephants, another slow-growing animal, also had high cystine levels. They didn’t. Researchers now speculate that high cystine levels might relate to brain and eye development. That’s because cystine is used to make another compound called taurine, which is highly concentrated in both the brain and eyes. In fact, cystine levels were higher, the further up the primates were on the evolutionary tree…” –Bryan
thhq- (and anyone else who’s interested)- here is a study done after Keys’ time, showing that as cholesterol levels rose in Japanese men, their rate of CHD continued to decline:
http://www.ncbi.nlm.nih.gov/pubmed/26182938
The authors suspect there is a protective element in their diet or lifestyle- (taurine, perhaps?) Of course, the other possibility is that cholesterol is not an accurate marker for heart disease……
Morgana. thanks for this link. Which brings up a terrific point: Lower serum cholesterol could be bad for us! We need to look at actual serum concentrations.
Amazingly, on our blood panel results, we still get no lower limit for serum cholesterol. That implies the lower the better, right? Except that’s ridiculous. Cholesterol’s a key nutrient. If we drove serum cholesterol down to zero mg/dL (zero mmol/L) we’d be very dead creatures.
Like all our other serum measures, we have an optimum level of serum cholesterol. So what is it?
Let’s look at what the MRFIT study found. MRFIT was a major study from the National Institute of Health (NIH):
http://www.epi.umn.edu/cvdepi/study-synopsis/multiple-risk-factor-intervention-trial-mrfit/
Check out that chart. See where the MRFIT study chart puts the sweet spot at right around 200 mg/dL?
This means if you go either direction–higher *OR LOWER*–your chance to die sooner goes up!
http://sphweb.bumc.bu.edu/otlt/MPH-Modules/PH/PH709_Heart/PH709_Heart5.html
Yet that NECP grid you see right afterwards, it says 200 mg/dL is “borderline high!”
LOL! Oh, the cognitive dissonance!
The cognitive dissonance that stems from our disastrous Ancel Keys-driven dietary policy from 1980. Which has since caused untold amounts of official shuck’n’jive.
I will be grateful for the day the US–and by extension the world–finally unshackles itself from those horrible perverting guidelines. –Bryan
wbryanh- In that 2nd link you sent, I found it strange that they claimed that low HDL is a risk factor for Myocardial Infarction, but that they’re convinced it’s not “causal”. The reasoning is that drugs that raise HDL don’t necessarily lower risk of heart disease- (of course, I had read independently that they are unable to make high quality drugs that really raise HDL to a great extent; in other words, “follow the money”! This could be why HDL is considered a non-issue). So they are convinced that low HDL is “not causal”, but only an indication of what else might be going on in the body. So, why do they not consider high LDL in this way? Why are they convinced that high LDL IS causal, and maybe not just an indication of something else going on in the body? (Well, okay, “follow the money”, I got that). But there seems to be evidence that LDL cholesterol is actually a part of our immune system. That’s right; for instance, people with low LDL have a higher risk for cancer- (if you need a link for that, I’ll find one. I’ve read it numerous times, which is why I’m not going to worry about cholesterol!) Some theorize that high LDL might only be an indication that something is not quite right and the immune system is working……whether you are fighting an infection, or have inflammation, or whatever. So, yeah, if this is true, then lowering cholesterol artificially is the worst thing you can do!
In addition to that, there are times when various groups of people can and should have higher cholesterol than the norm- like teenagers for instance, when the sex hormones are developing and changing. Women seem to get higher cholesterol when they go through menopause. This indicates to me that there is a reason for that; that it’s natural and necessary, and that we shouldn’t be messing with it. There is a lot I could say on the subject of cholesterol…..(don’t get me started, ha ha).
Hi Morgana. I posted that Boston U link mainly to show that MRFIT chart showing that the serum cholesterol level for lowest all-cause mortality is 200 mg/dL–much higher than most people would expect. I started to read the rest of that BU link, but soon as I got to that NECP table that says 200 mg/dL is “borderline high!” that was it–I knew I’d strayed into CW land. No need to waste more time there!
I couldn’t quite make out some of your post, the questions about which lipos are purported to be causal or not. But very curious what you want to say, so hope you’re willing to write it again!
Meanwhile Morgana let me give some of the logic behind the lipos, and please forgive me if you already know this stuff. The much-maligned cholesterol molecule is a repair and structural compound which we insert into cell membranes where our bods feel it’s needed. Lipoproteins are like our bods’ “greyhound buses” that ferry lipids including cholesterol around our bods via the blood. The LDLs (Low-Density Lipoproteins) are the “outbound” lipo buses; these take lipids *from* the liver to body tissue that the bod thinks needs repair, eg to injured arterial endothelial lining. Thus, one reason we interpret high LDL as “bad” is because the higher its level is in serum, the more it may be signaling a strong need to repair tissue injury. In this sense, it’s not so much that LDL per se is bad (though it may be–see more below). But rather it’s the *possible* pathology that high LDL levels may suggest.
Looking the other way, HDL (High-Density Lipoproteins), are the “inbound” buses. These take lipids from tissue back *to* the liver for storage and/or demolition. We see these as “good” because they suggest a healthy bod with no need of cholesterol to repair tissue, so cholesterol can be shipped back to the liver for disposal. As with the LDLs, it’s not that the HDLs per se are good. Rather it’s what their high serum levels suggest: a healthy bod with little need for repair.
So Morgana, what you say here about LDL:
“…Some theorize that high LDL might only be an indication that something is not quite right and the immune system is working……whether you are fighting an infection, or have inflammation…if true, then lowering cholesterol artificially is the worst thing you can do!…”
I can’t speak to specifics about lipo/immune cell interactions, but I agree in the main that high LDL, esp when episodic, may be a healthy if unpleasant response, like pain. I heard someone describe LDL as battlefield medics who rush to where they are needed, and statins as the evil self-serving generals who prevent the medics from going where they are needed to convey the impression “there’s no problem–we’re winning!” As with so many other meds, statins reduce the symptoms but don’t resolve the root problem and can even make it worse!
With the above understanding in mind, let’s look at our badly broken lipid measurement system. At least the default system we get when we go for standard blood panels. These tests measure only the levels of *lipids*, those that are free, those in LDL, in HDL, etc. They don’t measure the actual # of lipoproteins which carry the lipids. That matters because it’s the *lipoproteins* that come into contact with your arterial endothelial lining. Whatever your *lipid* numbers, you much rather know how many of those actual *lipos* course through your veins. Do you have many smaller more oxidized lipos which some think are atherogenic? Or do you fewer larger “fluffy” newer, less oxidized lipos, which many consider relatively non-atherogenic? We have no way to tell based on the current default measures. We do have ways to measure directly the lipos, such as vertical auto profile (VAP), gradient gel electrophoresis (GGE), nuclear magnetic resonance (NMR), and tube gel electrophoresis (TGE). But last I checked none are ready for prime time.
And Morgana, I agree with you completely, it’s “follow the money.” Esp when it comes to statins, a huge market that hit $20B a few years ago:
http://www.cardiovascularbusiness.com/topics/healthcare-economics/slides-generics-push-statin-revenues-down-7b
–Bryan
wbryanh- okay, sorry….I realize you posted that link as proof that “high-ish” cholesterol levels protect one from all cause mortality, and I neglected to comment on it, so that might have been a bit confusing. But, yes, I knew that already (I’ve read a lot about cholesterol). And I guess you admitted you didn’t read the whole link, so you might not have known what I was talking about. Basically, in a nutshell, the authors claimed that lowering LDL was “protective” against heart disease, whereas raising HDL was “not protective” (even though they admit that having higher HDL is associated with lower risk for heart disease). Now some people would quibble with this. According to Nina Teicholz, low HDL is a stronger marker for heart disease than high LDL (I don’t have a link because, once again, I read it in her book; but I could probably find one if you want). I have read this elsewhere too (possibly Malcolm Kendrick?) It would make sense, since heart disease is associated with diabetes, and low HDL is also associated with diabetes. And there seems to be evidence that raising HDL is more effective than lowering LDL. But of course there’s no money in it, as they do have effective drugs for lowering LDL (but not so good for raising HDL) Of course, as Nina Teicholz says, one of the best ways to raise HDL is to eat more saturated fat, but of course they’re never going to recommend that!
In any case, it seems more and more unlikely that “high cholesterol” (including high LDL) is really an issue at all. Your graph proves that; if there is less mortality in people with higher cholesterol, then it obviously can’t be harmful; or at least, I don’t think a substance in the body would be both deadly and helpful at the same time, if you know what I mean. Looking at high LDL seems misguided, as there are many different functions of LDL; for instance, the making of the sex hormones (which explains why teenagers, or pregnant women, or women in menopause have higher cholesterol). Also cholesterol is important for the formation of bile, which means for me, it’s a no brainer that people who eat more fat might have higher cholesterol, in order to digest the fat. So looking at “cholesterol” in this one-sided fashion seems awfully reductionist. And I mentioned in my last post that LDL is part of the immune system, so removing it is counter-intuitive. Sort of like saying ” a high white blood cell count is associated with injury, so we need to lower our white blood cell count to reduce injury”. In other words, I don’t believe that LDL is necessarily “predictive”, like the authors of this study claim!
Apparently there are other markers that are far more predictive of heart disease; I’ll try to find some links for those. Give me time, I have a few things to do….
Morning/Evening Morgana!
Thanks for spelling out the high-low HDL-LDL Qs. Yes, I’ve largely exited that entire debate, at least how it relates to n=1s, because we don’t know the actual number of lipoproteins, those particles that most likely drive atherogenesis. That LDL cholesterol, is spread out among fewer larger LD lipos or more smaller LD lipos? Same Q for the HDL cholesterol: is it in fewer and larger lipos or in many and smaller lipos? I read somewhere that even HDL cholesterol above a certain point for certain cohorts can suggest pathology:
https://www.urmc.rochester.edu/news/story/2872/more-good-cholesterol-is-not-always-good-for-your-health.aspx
But of course our typical blood panel results don’t set an upper limit for HDL c’stol. Which suggests to us that if that HDL level shoots into the heavens we’ll have achieved immortality. 😮
What amazes me is that more people don’t call bullsh*t on the standard lipid panel. Sure if I got a TC and/or trigs of 500+ mg/dL, I’d pay attention. At that point you know you have scads of lipos clogging your vessels. But the failings of the default panel are manifest. It doesn’t even directly measure LDL, but merely calcs it from measured levels of total c’stol, HDL c’stol, and trigs. Meanwhile that deeply flawed panel keeps driving the $20B statin market.
Yes Morgana when you have time to poke around for those other links, that’d be great, thanks! –Bryan
Hello wbryanh! Well, this is not the optimal link, sorry; it does state, though, how important HDL cholesterol is, and he *implies* that it’s more important than LDL. As I said, I read about this in Nina Teicholz’s book, “The Big Fat Surprise”; it was well researched and had many sources. I have a hard time often finding links on the internet to support what I’ve read in books; so much of the internet is either very mainstream, or written by complete idiots! I believe there is generally better information in books, but I’ll do the best I can. (You’re gonna “love” this link, ha ha! it’s written by someone who is a consultant for the drug industry. But as that is the case, you’ll see that it’s relatively non-biased, i.e., he’s not simply what some have called a “cholesterol denier”. Just ignore his emphasis on drugs, I certainly don’t agree with that! As I said, it’s only to prove the importance of HDL):
http://circ.ahajournals.org/content/109/15/1809.full
I’ll look for more links….I have to do it one at a time, sorry, I don’t know how to post multiple links, I’m embarrassed to admit.
Thanks Morgana. Yes, I’ve seen the same issue, finding internet links to support what we get in the books. Very interesting to see that limitation in our supposedly “free” and “unfettered” web-o-sphere. Makes me wonder about the underlying forces at work here.
To give credit to this drug industry author, he at least gives “lifestyle modification” as the first-line approach in his flowchart. Of course he doesn’t suggest what those mods should be, surprise!
Dr Toth also says “…Fibrates should be first-line therapy in patients with hypertriglyceridemia, LDL <130 mg/dL, and low HDL…” I need to delve more into fibric acid which I almost never hear about.
One line of Toth’s stood out:
“…There is considerable controversy about whether one HDL subfraction is more antiatherogenic than others…” This suggests he discusses one or more methods for directly measuring lipo content, eg VAP. I’d love to see more details on those observations.
BTW, later today I’ll drop by the library to borrow Big Fat Surprise. Thank you for that reminder! –Bry
Wbyanh, Morgana: Well, here’s a theory for you. Taking bile salts lowers cholesterol. Why? Because it binds to cholesterol in the bile:
“Bile acid resins are substances that bind in the intestines with bile acids that contain cholesterol and are then eliminated in the stool. The major effect of bile acid resins is to lower LDL-cholesterol by about 10 to 20 percent. Small doses of resins can produce useful reductions in LDL-cholesterol.”
http://www.medicinenet.com/script/main/art.asp?articlekey=9494
My understanding is that the liver creates HDL, which delivers cholesterol to heal tissues. The LDL is the “used up” fluffy cholesterol that comes back to the liver. The liver can reuse the LDL, or toss it into the bile and get rid of it.
But then commonly in the US, the LDL in the bile doesn’t LEAVE … it gets re-absorbed. I’m thinking this is an error on the body’s part, caused by lack of bile. Ideally the LDL gets bound up to something else in the bile salts, and it is then excreted. That gives your body a way to “take out the garbage” … heavy metals, damaged proteins, weird chemicals, or whatever.
So of course you can see where I’m going with this! The ability to make bile is limited by the amount of taurine the body can spare to make bile. If you have all this extra taurine around … because, perhaps, you happen to like sushi and dried squid … then you’ll be excreting tons of LDL. Which will allow your body to detoxify itself by getting rid of the “dirty” LDL.
By that theory, high LDL is then a sign that you don’t have enough bile and your body isn’t able to take out the garbage so well. Low LDL (or low HDL) might mean the body has a problem making HDL, which isn’t a good thing either. Or maybe your body is using it up too fast, which means there is inflammation somewhere. In either case, the measurement is like glucose: the glucose is high or low for a reason, and you need to know the reason before you know what to do about it.
I got to thinking about this because since I started my T-experiment, my output has gotten more and more greenish. I’ll be interested to see what this does to my LDL levels next time I get tested.
“Taking bile salts lowers cholesterol…” Interesting idea Heather! And maybe limited avail of methionine/taurine could be a gating factor.
I do wonder though–if bile salts scarf up serum c’stol, will our livers just crank out more? If our bods continue to perceive the need for it?
A big part of this may come down to our bods’ perceptions of our serum c’stol needs. C’stol is a thoroughly organic cmpd. We make it just from Cs Hs and Os. Our livers can churn out unlimited amounts of c’stol. Using materials it scavenges right at hand.
Heather, about what you say here:
“My understanding is that the liver creates HDL, which delivers cholesterol to heal tissues. The LDL is the ‘used up’ fluffy cholesterol that comes back to the liver. The liver can reuse the LDL, or toss it into the bile and get rid of it.”
Actually, it’s the other way round. It’s LDL that ships out lipids like c’stol from liver to tissue the bod perceives is injured or otherwise needs attention. It’s the HDLs that return “unneeded” lipids back to the liver for disposal. What’s “fluffy” is not c’stol itself, but the lipos themselves that carry a full and heavy charge of c’stol and other lipids. Like new and largely unoxidized LDLs. Some say these large fluffy LDLs lack atherogenicity because they are not oxidative. Others say it’s because they are simply physically too large to lodge themselves into small endothelial “nooks” and thus to seed eventual plaque formation. Some folks say both the oxidative potential and size are atherogenic factors.
We could see many causes for LDL that lingers in serum. Loren Cordain claims that certain sat fats–like lauric (12C), myristic (14C) and palmitic (16C)–all down-reg LDL cell receptors, which would lessen cell intake/demo of old small LDL. Meanwhile other folks suggest the thyroid govern LDL receptor expression, so if we suffer some reduced thyroid action–eg from low levels of iodine–then that’s what’s ultimately causes serum LD levels to rise. That last option attracts me. If you don’t eat seafood and sea veg and don’t eat iodized salt, then you could suffer an iodine deficiency. With the salt-phobia we see now, plus the trend away from mainstream salt and toward “artisanal” salt like Himalayan salt, we could now see a return to a broader-based salt deficiency. Anyway, certain MCFAs and LCFAs and low iodine are just a couple of possible causes for insufficient LDL clearance. –Bryan
Yes, hypothyroidism is one of the reasons for high LDL (as well as diabetes). I’ve read that hypothyroidism is rampant these days; probably partly due to salt restriction, as wbryanh mentioned, but another problem in America may be water fluoridation, as that supposedly can disrupt thyroid function. I also wonder about the admonition to eat as many vegetables as possible; there is this fad, for instance, of “green juices”, but some of these juices that people drink are high in goitrogens, which could also disrupt thyroid function in susceptible people. Maybe it’s all three put together…..but, yeah, once again I think much of our “health” advice” has been harmful.
And many people don’t know they have thyroid issues until it become blatant like pronounced hypothyroidism and they have to go on meds. The standard TSH test may not reveal the true story. You need more tests, esp T3 and maybe T4.
http://www.marksdailyapple.com/iodine-deficiency
http://www.marksdailyapple.com/hypothyroid
–Bryan
Bryan:
“And maybe limited avail of methionine/taurine could be a gating factor.
I do wonder though–if bile salts scarf up serum c’stol, will our livers just crank out more? If our bods continue to perceive the need for it?”
I’m kind of thinking that maybe it’s like white blood cells. Your body makes them as needed, and cranks up production if there is an infection. But when they die … they need to be gotten rid of. Bile is something of a garbage truck, and one of the few ways the body can get rid of junk from the liver. The liver and kidneys clean the blood, and the junk goes in pee and poop. Well, some good stuff ends up there too (like vitamin B and K) and the body absorbs or reabsorbs that, or you have animals like rabbits that eat their poop.
But cholesterol is produced all over the body, and when a cell produces it (for self-healing?) then it gets transported to the liver. If all the cells are producing it, then there may not be one central agency for “produce this much c’stol”?
Anyway, T does some gene tweaking that causes the liver to excrete more. And yes, in rats with no extra cholesterol, more cholesterol is created, so the overall levels remain the same. But in the rats with high cholesterol (induced by diet) the cholesterol levels go down:
“The degradation products of cholesterol are bile acids, and the conjugates of bile acids with taurine or glycine contribute in the solubilization and excretion of cholesterol. There is a species difference in the conjugation of bile acids, and in rats, the conjugates with taurine predominate. When rats were fed the HC diet, fecal excretion of cholesterol and bile acids increased significantly compared to those of rats fed the test diet without cholesterol, and taurine further increased the bile acids excretion. We found that, in the HC diet group, the content of hepatic mRNA of CYP7A1 significantly increased, and it was also further elevated by taurine..”
“The addition of taurine to the diet did not reduce serum level of cholesterol in control rats (Table 4 and Fig. 2) (Mochizuki et al. 1998). Even in these rats fed a control diet, CYP7A1 was induced by taurine (Fig. 2). We speculated that the loss of steroid induced caused by taurine would be compensated for by the synthesis of cholesterol. We thought that this would explain why hypocholesterolemic action of taurine observed only in rats fed the HC diet.”
Apparently glycine lowers cholesterol too? Glycine is found in high levels in shellfish too! And in seaweed!
http://jn.nutrition.org/content/129/9/1705.full#sec-14
http://nutritiondata.self.com/foods-000094000000000000000.html
Taurine also lowered triglycerides and prevented gallstones in mice, as well as lowering cholesterol levels:
http://link.springer.com/chapter/10.1007%2F978-0-387-33504-9_27#page-1
But again, if one of the main points of cholesterol is to heal and cleanse the body, then the fact the body makes MORE is a moot point. More garbage might be taken out that way? Like what happens when you drink more water than you need.
The iodine link makes sense too. A large chunk of humanity is low in iodine. Goiter used to be rather endemic. Those “healthy Swiss” Price talked about actually used to have outstandingly high rates of goiter, to the point where it was affecting army enlistments. The Swiss government stepped in and started shipping iodized salt to the mountain people. Maybe that’s one reason heart disease is so prevalent in the slavic countries. It’s hard to separate the effects though, of iodine (seafood), DHA (seafood), taurine (seafood, esp. shellfish), Vit D (oily fish), glycine (shellfish, seaweed and pork), arginine (soy, shellfish). Maybe it’s just safer to eat more seafood …
Heather, @morgana — Heather your post sent me caroming down a cholesterolic rabbit hole. (No not Anichkov’s old experiments!) I’m still rootling round down in there.
I restate my main contention: Our modern lives serve up nearly countless sources that cause a chronic inflammatory response in our bods. Which causes our bods to chronically overproduce cholesterol to “repair” the real and perceived damage from all that novel impingement.
Otherwise, for the moment, I plop out a few thoughts/Q for your rumination. These include:
– What are cholesterol’s fates?
– In which bodily places (liver, elsewhere) do we make our cholesterol and at which relative levels, eg mostly in the liver?
– How do LCHF pegans get enough methionine/taurine?
First, those Fates. Per Lehninger’s Sixth (2013), c’stol goes to:
– bile acids
– biliary cholesterol
– cholesteryl esters (usu c’stol + fatty acids)
http://www.britannica.com/science/cholesterol
also reminds us c’stol “…is the starting material or an intermediate compound from which the body synthesizes …steroid hormones [eg the sex hormones] , and vitamin D…”
My big Q here: do we really have to excrete excess c’stol to get rid of it?! After all, we make our own c’stol, and we need only Cs, Hs and Os to slap it together. Sure we can hugely recycle c’stol even in its largely complete four-HC-ring steriodal form and why not?, it’s easier that way. But still, can’t we just break that steroidal sucker back down to its elemental/near-elemental Cs, Hs and Os? You know, to send those basic building blocks off to make other lipids, glucose, pyruvate, whatevs. Seems totally weird we wouldn’t be able to do that. Anyway.
About meth/taur, my main thought aligns with you–and you too Morgana? That this is yet another example where Nature builds in a way to automatically give us the supp materials we need. The more fat (mainly from animals) we eat, the more taurine we need to form that important bile salt (taurochenodeoxycholic acid). Since we typically get our fat from animals, then we also get more methionine too–our only essential precursor to make taurine.
Ancestrally we would have eaten little plant-sourced fat. Nuts/seeds, olives and coconuts are exceptions. And nuts/seeds are seasonal. Plus we find coconuts and olives in tropical and semi tropical places usually near water. Thus the ancestrals who ate coconuts and olives also ate a lot of meth/taur-rich seafood.
Now today, we see several concurrent movements, paleo and the totally novel vegan approaches, which combine to form the “pegan” movement. Eg what Mark Hyman evidently calls/called himself:
http://drhyman.com/blog/2014/11/07/pegan-paleo-vegan/
Increasingly, to pegan, we add low-carb for the ever-growing numbers of the hyperBG-affliged. Which forces adherents to rely ever more on a relatively narrow supply of plant fats. Which include year-round nuts/seeds, fruit oils like those from coconut, olive, red palm, and avocado, and their whole fruits (olives, avos).
So some Qs. Do these high-fat low-carbing pegans suffer from meth/taur deficiencies and thus develop fat digestion problems? Do they get enough meth/taur? Can they skip methionine and cadge enough S from brassicates/allia/other S-rich plants?
Heather what you say “…But cholesterol is produced all over the body…” I find divergent info on this. At this site:
http://themedicalbiochemistrypage.org/cholesterol.php
“Slightly less than half of the cholesterol in the body derives from biosynthesis de novo. Biosynthesis in the liver accounts for approximately 10%, and in the intestines approximately 15%, of the amount produced each day….”
Yet Lehninger’s Sixth says “Most of the cholesterol synthesis in vertebrates takes place in the liver…”
That above link goes on to say “…Synthesis of cholesterol, like that of most biological lipids, begins from the two-carbon acetate group of acetyl-CoA….” So this suggests like you say Heather, that “…all the cells are producing it, then there may not be one central agency for ‘produce this much c’stol’?…” All cells that have mitochondria anyway (only our RBCs are certifiably mito-less), and thus run the Krebs Cycle, in which acetyl-CoA is a key compound.
Still, I’d like to see some confirmation how much we crank out c’stol from our livers. And how much we make “locally.”
Guys, that’s what I have for the moment. –Bryan
Good thoughts!
I don’t know that the body needs to get rid of cholesterol. I think it uses the cholesterol to get rid of “whatever” it needs to get rid of. Like a garbage truck. That MIGHT be excess or oxidized fat. Or damaged proteins. Or heavy metals. Some damaged tissues can be recycled, but it seems there also needs to be a way to “dump” stuff. Like how uric acid and oxalates and one form of lactic acid is dumped by the kidneys. The kidneys though, can only handle whatever is soluble in water. Bile can handle all the stuff that is solid. Bile is THE only method I can see for the body to GET RID of solids.
In the case of oxidized fats … I guess the fats could be taken apart and de-oxidized? Seems like the body doesn’t handle rancid fats all that well though. If there is a lot of fat in the diet anyway, it would make more sense to dump it?
So T doesn’t actually lower Ch at all, turns out, compared to a normal diet. It has more effect on a high or low cholesterol diet. But it does lower triglycerides and tend to cause weight loss, and reliably prevents CVD.
Click to access 39541.pdf
So as to the fate of Ch … bacterial toxins, for one, have a notable tendency to glom onto Ch.
“Studies such as THIS have shown that LDL cholesterol has the capability of reducing pathogens and infectious bacteria. Endotoxins from gram negative bacteria bind to LDL particles. When bound to LDL, they are inactivated. Additionally, when endotoxins are bound to LDL, the toxins are unable to trigger the production of pro-inflammatory cytokines such as TNF-a. Therefore if there is insignificant cholesterol and LDL, a person may be at an increased risk for infection.”
http://metabolichealing.com/cholesterol-is-among-your-bodys-most-powerful-defenses-against-toxins-free-radicals/
“Microbial toxins that act on animal cells will have
some kind of interaction with membranes containing
cholesterol. The membrane may be the primary target,
as is the case with membrane-damaging toxins, or it
may constitute a barrier on the way to the intracellular
target, to be overcome by endocytosis and/or by some
kind of protein translocation activity built into the toxin
molecule itself.”
http://onlinelibrary.wiley.com/doi/10.1111/j.1574-6968.2004.tb09768.x/pdf
So now you have some cholesterol with something toxic hanging off it. What to do? I say the easiest thing is: dump it. But where? Oh, I have some handy taurine in the liver: I’ll make some bile!
Now, it may be there isn’t enough taurine, so you have to stop dumping it, and now your Ch levels go high AND you have a bunch of toxins laying around. Or maybe there aren’t enough fats around, so you can’t produce enough Ch to even do housekeeping … so your Ch goes low, which is also bad in this case. Otherwise your Ch levels go up or down depending on what your body thinks it needs.
——————-
As for the Paleo/Vegan etc. discussion … I’ve always said you need to look at cuisines, not at food categories. Esp. we need to look at cuisines that have worked for a lot of people for a long time. Like you said, there really have not been many cultures that had a high-fat high-meat diet for a long time. The Neanderthals and some of the Paleo people seem to be exceptions. But I don’t see a lot of evidence that they were very *healthy*. They were “old” at what we would consider a pretty young age (like 50). Lewis and Clark weren’t terribly impressed with the health of the Plains Indians either. And they themselves figured if they made it to 60 that meant they were in good health. And their diet would have been considered ideal by many Paleo fans!
On the other extreme, most vegan cultures weren’t that way voluntarily, and they were malnourished. That’s why the exceptions (like the Yuzus) are important.
However, there are thousands of years and many cultures that did and do fine on a shorelilne diet, which is why I sort of glommed onto that one. Japan and Korea are the best-documented, plus they are now living a more “modern” lifestyle so it’s hard to credit their longevity on the pristine air and easy life. But folks in the British Isles used to eat a shoreline diet, then suddenly switched to an inland diet, and the skeletons show the results.
So the shoreline diet has varying amounts of fat, but fat isn’t rare among sea creatures. And all the other stuff we’ve been discussing is there in spades.
“So some Qs. Do these high-fat low-carbing pegans suffer from meth/taur deficiencies and thus develop fat digestion problems? Do they get enough meth/taur? Can they skip methionine and cadge enough S from brassicates/allia/other S-rich plants?”
Normally I agree with what Denise says in one of her blogs: for the folks who are ethically against eating animals or animal products, eat molluscs! Mussels simply don’t have a brain to speak of, and they are loaded with good stuff. And don’t pollute the ocean (actually they clean the water).
But yeah, heart disease is a big deal in vegans in general. The founder of Bastyr university died of heart disease at a young age, and his son also, at an even younger age. How do the Yuzus do it? I think because it’s a very specific diet, grown on volcanic soil. And has a fair bit of soy in it. And a some fish.
“Dr. William A. Mitchell Jr., naturopathic physician and co-founder of Bastyr University, died Tuesday in Seattle of a heart attack. He was 59.
His death came just hours after his son, Noah, 27, suffered a heart attack and died, according to a release from the university.”
http://www.seattlepi.com/local/article/William-A-Mitchell-1947-2007-Physician-1226634.php
“CONCLUSION:
The low dietary intake of protein and sulfur amino acids by a plant-eating population leads to subclinical protein malnutrition, explaining the origin of hyperhomocysteinemia and the increased vulnerability of these vegetarian subjects to cardiovascular diseases.”
http://www.ncbi.nlm.nih.gov/pubmed/21872435
And most of the people becoming vegan as adults already have a good store of amino acids in their bodies. Some last a few years and then get ill. A lot of them cheat now and then. A lot of them take supplements. Denise has a blog entry about supplements vegans need (taurine is one of them!).
Omega 3’s are an interesting case, because it seems that there is a gene that controls whether or not you can use the plant version of O3. It appears that when people moved inland, they got the ability to use the plant version.
“The fatty acid desaturase (FADS1) gene is responsible for conversion of plant-based oils to EPA and DHA. About 40-50% of Chinese, Japanese and Hispanics carry a FADS gene with lower activity, which limits these conversions. If these people rely solely on plant sources of omega-3, they may suffer from deficiency of EPA and DHA. People of African, Middle Eastern, South Asian or European descent tend to have a higher frequency of the more active form of the FADS gene, which means they can readily convert plant-based omega-3. The genetic difference in the FADS gene might reflect evolutionary selection based on food availability and culinary practices in different regions and ethnic groups through history”
https://www.gbhealthwatch.com/include/newsletter/2014-09-15.html
Mark Hyman seems to have sort of hedged all his bets though, with “pegan”. It’s sort of “uh, if you eat meat make sure it’s grass-fed” and “don’t eat high-mercury fish”. Which is hardly vegan! Actually the diet he recommends isn’t too different from what most of us would do, except some of the hard-core Paleos at one point were sort of “against vegetables” … I think that’s changed. His version of “Pegan” isn’t far off from the traditional Japanese diet, except the Japanese did rice.
Speaking of the Japanese diet: I found a great site for Japanese recipes. Seems to be linked to a store in Kyoto too, which will ship to the US. Ha!
http://kyotofoodie.com/home-cooking-sanma-no-shioyaki-salt-grilled-pacific-saury/
Saury is one of the highest-taurine foods. Also pretty cheap. Canned mackerel is kind of similar, and is also very high in taurine (and sold in US markets). I had saury, rice, and cabbage for breakfast. It was so yummy!
OK, so maybe an analogy. This is what I’m thinking.
There is this place called “New York City”. It makes a lot of garbage, every day. And people are packed together, so there is nowhere to hide the garbage. So they put the garbage in bags, and put the bags in an alley.
Trucks come and pick up the garbage. They take it to a place called Liverpool (joke … or maybe just call it “the dock”). There garbage scows get loaded with garbage bags. The scow goes out into the ocean and sinks itself, where it goes into a Black Hole so it doesn’t pollute the ocean. We dunno where the Black Hole goes! Probably the other side of the universe, so we don’t have to worry about it.
So the garbage bags are cholesterol. You have to have the right building blocks in the diet to make enough garbage bags. If there aren’t enough garbage bags, then the garbage just piles up inside apartments.
The garbage trucks are the HDL (? I think? I get confused by all this too). So you have to have enough garbage trucks too, or the bags pile up.
But what happens if the garbage trucks get to the dock, and there aren’t enough garbage scows? Well, all the full garbage bags just pile up … on the trucks, I imagine, which just keep on driving around. Until there are more scows to sink the full garbage bags. So then you build more garbage trucks and make more garbage bags, until the garbage scow shortage is fixed.
In that story, the cholesterol readings are the number of full and empty garbage trucks, and the number of available garbage bags. Taurine (and glycine maybe?) are the garbage scows.
If you see a lot of full garbage trucks driving around, that means that either a WHOLE LOT of garbage is going out, or else there is a lack of garbage scows. If there are a whole lot of empty garbage trucks, then that means the city planners are either just on the ball or are expecting a lot of garbage.
What do you think?
Heather, @morgana —
Heather you say: “So the garbage bags are cholesterol…”
Q to U: How exactly does Ch bind to, and otherwise envelop and bundle up, the molecular “garbage?”
Do you have a molecular-level schematic to show how it does this?
Or maybe it’s the *lipoprotein* that binds to the endotoxins and other “garbage?”
In that Uffe Ravnskov link you posted earlier…
http://qjmed.oxfordjournals.org/content/96/12/927.full
…it says: “Lipopolysaccharide, or endotoxin, the main pathogenic factor of Gram-negative bacteria, binds rapidly to *lipoproteins*, mainly LDL…”
So Heather even though this articles *title* says:
“High cholesterol may protect against infections and atherosclerosis…”
maybe the endotoxins actually bind to *lipoproteins*? And not directly to cholesterol? Or even at all to Ch?
Could it be that even the editors of these august journals like Oxford Journals confuse “cholesterol” and “lipoproteins?”
If so, stranger things have happened 🙂 –Bryan
“maybe the endotoxins actually bind to *lipoproteins*? And not directly to cholesterol? Or even at all to Ch?”
The article you linked to is indeed unclear. I was thinking of a different one though. When I started looking at “cholesterol” and “toxins”, it appears that cells use cholesterol in the cell walls, and yes, the toxins interact directly with the cholesterol. Which makes the cholesterol look a little bit like cinderblocks outside the wall … when the cinderblocks get damaged, they get carted away but the embassy is still ok!
http://onlinelibrary.wiley.com/doi/10.1111/j.1574-6968.2004.tb09768.x/pdf
“Microbial toxins that act on animal cells will have
some kind of interaction with membranes containing
cholesterol. The membrane may be the primary target,
as is the case with membrane-damaging toxins, or it
may constitute a barrier on the way to the intracellular
target, to be overcome by endocytosis and/or by some
kind of protein translocation activity built into the toxin
molecule itself”
————–
http://qjmed.oxfordjournals.org/content/96/12/927.full
If the lipos clean up endotoxins too, that’s great also! It still leaves the question: what to do with the toxins once you have them sequestered? Seems like they’d have to be dumped. If they can’t be dumped, then maybe they end up being parked by the side of the road, and now they are *toxic* cholesterol/lipos.
————-
And yeah, it sounds more like Ch is a sponge, and the lipo is the garbage bag/truck. (since it does the containing AND the moving). And taurine or glycine is the trash barge … the trucks each get loaded on one and then the whole thing sinks. But then sometimes a big crane comes and drags the garbage back to shore … 🙂
Thanks for the Palmer link Heather. I’m still trying to sort how it fits into your evolving garbage bag/truck/barge/crane analogy. I like it btw. Please keep working on it.
The Q you pose remains:
“…If the lipos clean up endotoxins too, that’s great also! It still leaves the question: what to do with the toxins once you have them sequestered? …”
The Palmer piece you posted:
http://onlinelibrary.wiley.com/doi/10.1111/j.1574-6968.2004.tb09768.x/pdf
talks about how endotoxins bind to cholesterol in *cells*, but not in lipos. In fact Palmer doesn’t mention lipoproteins. Palmer appears to focus on endotoxin pathology initiation. Not endotoxin disposal.
Here you see a diagram how cholesterol embeds into cells’ lipid bilayer. Nicely nestled in both the cytosol-facing and circulation-facing layers of the cell’s membrane:
http://www.nature.com/nature/journal/v438/n7068/box/nature04399_BX2.html
But we don’t find cholesterol molecules embedded into the lipoprotein’s monolayer. This likely because the lipo is *ferrying* the cholesterol through blood, an aqueous solution and thus hostile to the non-polar cholesterol molecule and which might impede the lipos’ travel in the blood. That’s why we likely won’t find Ch or any lipid embedded in that monolayer. But rather firmly tucked inside the lipo’s spherical “cargo hold.” And unavailable to attach to endotoxins.
So how do we respond to endotoxins like lipopolysaccharides? This piece:
http://www.ncbi.nlm.nih.gov/pubmed/12135807
suggests our phagocytes uptake them. And appear to deliver them into bilirubin for excretion:
http://www.vivo.colostate.edu/hbooks/pathphys/digestion/liver/bilirubin.html
BUT… Ch appears to play some kind of role in phagocytosis:
http://www.nature.com/icb/journal/v81/n6/abs/icb200362a.html
So on that note Heather, I’ll toss this back to you! –Bryan
It seems cholesterol is a waxy substance that is used among other things, as the structure of the cell wall. It never floats away on it’s own. So “blood cholesterol” always means cholesterol that is neatly packaged up in lipos. So the lipo is a sort of truck. It trucks in fresh cholesterol, and trucks out the damaged cholesterol.
The lipo is also a sort of bag. So maybe it’s a dump truck, where everything is neatly contained in the back. So instead of garbage bag we’ll say the Cho is blocks on the truck.
White blood cells eat up bacteria. But bacteria also attack cells directly, and glom on to the cholesterol. Bacteria seem to have an affinity for cholesterol. This protects the cell, but the cholesterol gets damaged. It also gets damaged by oxidation … H2O2 in the blood, which kills bacteria but damages cells too. So the cholesterol layer is a sort of protection for the cell. So when it gets damaged, I’m thinking the damaged Cho goes into a lipo-truck, and new Cho gets unloaded from a lipo-truck to repair the cell.
From the previous link, it looks like the bacterial toxin somehow gets glommed onto the Cho. So the Cho does sort of act like a garbage bag too. Oxidation products would be part of the Cho also.
If the cells are getting damaged a lot, then there will be more trucks on the road.
Then the trucks drive to the liver, pick up a ticket (glycine or taurine) and get dumped into the river.
“Bile acids are synthesized from cholesterol in the liver. First, hydroxyl (OH) groups are inserted at several points, shown in the above picture; second, the second ring of cholesterol loses its double-bond; finally, the hydrocarbon tail is shortened by three carbons, and a carboxyl group is added to the end.
The bile salt shown above is called cholic acid, which contains three hydroxyl groups. The other primary bile acid is called chenodeoxycholic acid, which contains only two hydroxyl groups. These are the “primary” bile acids, although there are other “secondary” bile acids synthesized from primary bile acids by intestinal bacteria as well.”
http://www.cholesterol-and-health.com/Bile-Acids.html
So it sounds like the lipo (the truck) is emptied, the Cho broken down and made into bile, and dumped. The question would be: why would the Cho then be recycled? It’s the same question for the red blood cells in bilirubin.
“One of the most important and clinically relevant examples of waste elimination via bile is that of bilirubin. Additionally, the mechanisms involved in elimination of bilirubin are similar to those used for elimination of many drugs and toxins.”
http://www.vivo.colostate.edu/hbooks/pathphys/digestion/liver/bilirubin.html
The only reason I can think of to recycle it is to retrieve some substances the body really needs … taurine and glycine could fit here.
—————–
http://www.jbiomedsci.com/content/17/S1/S6
So, here is an interesting case: There are two populations living in the same area. One group (St. John’s) are living off mainly sheep and some fish, which they did not eat raw. The other group (Guiyang) is living off soy beans and fish. The St. John’s group has higher rates of CVD. They measured the T and Mg levels in the two groups … the Guiyang, unsurprisingly, had much higher levels of T and Mg (they mentioned the water is high-magnesium … I wonder what it is for the Yuzus?). So given that both groups live a pretty good life eating their traditional foods, the question would be … if the St. Johns people DID get more T and Mg, would their CVD rates go down even with a mainly-sheep diet? I.e., is the difference in the type of protein (mammal vs. fish) or the type of fat (saturated vs. fish oil) or is it just a taurine issue? And if so, how much taurine is possible to get out of a sheep?
The chart is pretty amazing:
http://www.jbiomedsci.com/content/17/S1/S6/figure/F9
It raises an interesting question. How many cultures that eat a fair bit of meat, also eat raw fish or squid?
heathertwist- wow, thanks for that extensive post, with all those great links! I especially liked the one from metabolichealing.com; it described very well what had always been my understanding about cholesterol- (and wbryanh, if you’re reading this, it was a much better description of what I was trying to say in my post last night. As I’m not a doctor or biochemist, I am not always able to accurately say what I mean….) He mentions that LDL is not “bad”, and HDL is not “good”; instead, we’ve simplified matters and coined these judgmental terms due to biased (or reductionist) thinking. I think that was a very well written article. In addition, he also mentions there are times that we may need a higher level of cholesterol and it may not necessarily be pathological; for instance, we need cholesterol to make hormones, including the sex hormones. This reminds me also that a cholesterol blood test is just a tiny “window” in time, like a snapshot. Checking your cholesterol a few days later might give an entirely different reading.
About the link where the son died at age 27, and then the father died soon after: was there any indication that these people were vegan? I did not see any mention of veganism in the article; just curious. But it did remind me of another possible cause of heart disease that many don’t think about, and that is stress, extreme sadness, etc. Heart disease often seems to follow difficult events. I saw on a documentary recently that apparently many people who are diagnosed with late stage cancer often die from sudden heart attack; again, I wonder if that’s from the stress of the diagnosis.
About vegans and heart disease: yes, the taurine/sulfur theory is very interesting, and I don’t doubt it. In addition, some vegans might be malnourished, and there are many other reasons why someone who is starving might have a heart attack- (again, something that people tend to “forget”, that very thin people die of heart attack as well). For instance, anorexics often have this problem- (you’ve probably read about very thin models who suddenly die at a young age). On anorexia and heart disease:
http://www.everydayhealth.com/columns/jared-bunch-rhythm-of-life/for-both-men-and-women-anorexia-nervosa-is-increasing-and-the-effects-on-the
Finally, about inland people, Paleo diet and heart disease; although I do believe fish and sea food are important (and I do love to eat them), other explorers have found that inland people eating meat diets (or meat and dairy diets) can be just as healthy, so it depends on whose “word” you want to take. Weston Price, for instance, in his book “Nutrition and Physical Degeneration” noted that inland people on meat diets were very healthy IF they consumed dairy as well; and if they didn’t consume dairy, they had to be eating the offal of the animals in order to be healthy. (Is there more taurine in the offal?) So, yeah, those Paleo people or high fat ketogenic people might have problems down the road I guess if they don’t eat any sea food, dairy products or offal- (though who’s to say, I guess this hasn’t been studied long term).
Lastly, heathertwist, your ideas and analogies (about cholesterol), make a lot of sense to me!
Good morning/evening/weekend Morgana and @heathertwist–
I’m back and now reading your latest posts and mini-oeuvres … –Bry
“About the link where the son died at age 27, and then the father died soon after: was there any indication that these people were vegan?”
Oh, absolutely. This was the *founder* of Bastyr University, and Bastyr is one of the earliest “pushers” of veganism. So their diet was “extremely healthy” by their own standards, which is what makes this so ironic.
I agree, stress pushes people to heart attacks. But generally only if there is an underlying condition (or the person gets hit in the chest with a baseball). Veganism and anorexia have this in common: they can lack what the body needs.
” other explorers have found that inland people eating meat diets (or meat and dairy diets) can be just as healthy, so it depends on whose “word” you want to take. Weston Price, for instance, in his book “Nutrition and Physical Degeneration” noted that inland people on meat diets were very healthy IF they consumed dairy as well; and if they didn’t consume dairy, they had to be eating the offal of the animals in order to be healthy. ”
I’ve heard that too, about how healthy the inland meat eaters were. The problem is, I haven’t found any actual documented examples. First, there are very, very few cultures that eat a LOT of meat. It’s just too difficult to do in most regions. Even Lewis and Clark, with good guns and prime huntsmen and a mostly unpopulated continent, often had a hard time finding game and ended up having to buy tubers from the Indians.
Second, the few who did reliably eat a lot of meat, don’t appear to have been all that healthy. Yes, they got taller (beef makes “beefy” people!). And the young warriors were tough and healthy. But they aged relatively quickly and were prone to gout and arthritis.
The people who eat dairy are basically pastoralists, and they tend to eat more dairy than meat. You don’t kill a cow while she is producing. They’d eat the extra (male) calves and older cows, generally on feast days. The diary-drinkers do seem to do well. And yes, milk has taurine. Also loads of other good stuff!
Good point about the offal though. Yes, the offal has more taurine in it than the meat does. Also the hooves and skin have glycine, which is important.
Price looked mainly at teeth and bone health, which is important. He doesn’t say much about longevity, and actually, at that time a lot of people didn’t even know how old they were, esp. in the tribal areas. The explorers were generally from places like London, where people had pretty serious growth and teeth problems, living off a diet that was mainly wheat and barley probably.
So they’d go to these tribal people and just be amazed that they had strong skeletons and straight teeth … and a meat diet can do that. But for some reason it also seems to promote arthritis. I’m the only member of my family that is NOT popping Advil all day. But if I eat beef two days in a row, my joints will start having “lumps” in them, where the collagen starts swelling (which my siblings and Mom always have). Further, I’ve seen the same thing in the older folks that are big meat eaters … while the egg/fish/chicken eaters don’t seem to have that. I’m thinking it has to do with neu5gc. Anyway, I’m 60 now and my hands look and work about like they did when I was in my 20’s. But when I was in my 40’s I started getting arthritic, about when I was eating a lot of grass-fed beef.
Anyway, if someone comes up with some examples of long-lived people who live primarily off land mammals, I’d love to see a documented example.
heathertwist- thanks for answering the question about the vegan father and son who died. Wow…very interesting.
Then- when you talk about inland people eating meat based diets, do you mean people who eat *only* meat? Because most healthy inland hunter gatherers that I’ve read about do eat plant foods too; as well as nuts, tubers, eggs and birds. Many eat insects as well. Basically, hunter gatherers have extremely varied diets- (well, at least they used to, before they were relegated to less than optimal land). According to what I’ve read, there were a very high amount of centenarians among the Sioux Indians- (I’ll try to find a link in a moment). The way of telling someone’s age is if they remembered certain things happening (i.e., they were alive when certain events took place)- so it would have been just estimation at best. Still, that’s something. The reason they “looked old and wrinkled” was because they *were* old!- and they were out in the sun a lot. Most hunter gatherers age more naturally than we do; they don’t stay out of the sun, put creams on their faces, etc. As just a personal observation (so you can take it pretty lightly), most people who look haggard and wrinkled to me nowadays are the ones who eat plant based diets; I haven’t noticed that with heavy meat eaters. So I personally doubt that it’s the meat, per se, that makes people look wrinkled; there are many other factors involved, including genetics.
In any case, here is a link describing American Indian eating habits, as well as their overall (not just teeth and bone) health. It is an article written for a different purpose- (fat intake of early hunter gatherer groups), but I include it here because there is a lot written about diet and overall health (including arthritis). You will note that absolutely *all* of the animal is eaten, which I’m sure makes a big difference!
http://www.westonaprice.org/health-topics/guts-and-grease-the-diet-of-native-americans/
As per arthritis, I never heard of a link between meat and arthritis before (that doesn’t mean it doesn’t exist). I have read about a link between gluten and arthritis though, which may partly explain why it’s rampant among Westerners. Keep in mind that when Lewis and Clarke made their observations many of those Indians may have already had contact with the white man and were eating other foods.
There were also other healthy inland meat eating groups, like the Australian Aborigines who weren’t on the coast- (I have read that they were in excellent health, before much contact with the white man; sadly, all these groups go downhill fast when they start eating Western foods). I’m sure there are others. But, again, though they were eating a reasonable amount of meat, their diet was very varied as well. And we need to also keep in mind that many of these early hunter gatherers traded with each other as well, so some of them may have even gotten fish and sea foods of various sorts.
The information about aging in mainly-meat-eaters is partly from skeletons. There are ways to figure out the actual age of the person that died (using something like the tree rings on trees), and an “old man” in Paleo times was about 50. At that age they started losing teeth, bone mass, etc. That’s been documented in other tribal cultures too. Centenarians that are ALSO in good health are rather rare, so it’s good to look at what the differences are! Getting good documentation is hard to do. Also it’s hard to know what the true diet was of some of the peoples. It is common for tribal cultures to brag a lot about all the meat they got … but like you say, their actual diet was pretty varied. This is changing as some studies are now using bone isotopes to figure out the actual diet.
My guess is that one of the issues is neu5gc … it is found in mammal meat, but not in birds or fish. It is absolutely known to be inflammatory, and it builds up in the body. Another issue is iron … high-heme foods will age a person faster than low-heme foods. Wheat of course is absolutely on my bad list, and these days the wheat-eaters and the mammal-eaters more or less overlap, which does make it hard to know. The paleo guys didn’t get much wheat though, and neither do the folks in Africa and South America. A lot of those folks are fish-eaters, but others live on “bush meat” so one could study them. Most of the tribal folks DO eat the whole animal too, so it makes a good contrast with the typical Westerner!
Right now what I’m looking at has to do with amino acids, esp. some of the oddballs like taurine. Taurine, though named for a bull, is not found so much in most mammals. It is common in molluscs and oddly, turkeys (so maybe in other land birds?). Glycine is also key to longevity, and is found mainly in seafood and in hooves/skin/cartilage … which is where your bone broths come in. How many mainly-meat-eaters get enough taurine and glycine? I don’t know. Probably depends how hard they work at making broths and headcheese etc. Ditto for vegans. Seafood-eaters get plenty without working at it. Seafood eaters that also eat mammal meat probably get plenty too … which is where Spain, France, Crete, and Greece come in! There is this odd lack of overlap … you don’t see a lot of peoples that eat a lot of meat and also a lot of fish. In ancient Britain the people went from an all-seafood diet to an all-land-based diet in a period of 50 years or so.
I’ve also noted that among the new-paleos, there is more of a movement toward more fish and vegies:
“I had the following: a chopped salad, tuna tartare, a 12 oz filet; and we split an order of sautéed onions, brussels sprouts, and a bowl of berries.”
http://eatingacademy.com/personal/actually-eat-part-iii-circa-q1-2014
That’s Peter Attia, who has been a big fan of meat.
“And I noticed I was eating less meat. Not at all by “design,” but somehow by seemingly craving less. It seemed an average week would have maybe 2 servings of red meat. When a great steak is placed in front of me, believe me, I enjoy every bite, but I found I just wanted it less. I also started craving a bit more fruit, especially berries and even apples, the former I consumed in modest amounts in ketosis, the latter I did not at all. (Because I know someone will ask – do I think red meat is harmful? – the answer is no, I do not believe so. Certainly not based on evidence I’ve seen to date, including the recent story about protein. ”
I’ve noticed the same in myself. More fish and eggs and vegies, less meat … not originally because of any study, just that it tasted better. Then I noticed I feel better on eggs and fish, and started looking at it in larger populations.
There needs to be a ton more studies obviously. Those are just my observations of patterns and of what works in my life.
Here is the one I found interesting:
“The toothless skull of an early human ancestor discovered in the Caucasus may attest to evolution’s oldest known example of compassion for the elderly and handicapped, scientists report today.
Other experts agreed that the discovery was significant, but cautioned that it might be a stretch to interpret the fossil as evidence of compassion.
The well-preserved skull, found in Georgia, belonged to a male Homo erectus about 40 years old. All his teeth, except the left canine, were missing. Regrowth of bone indicated that the man had been toothless for at least two years before he died at what was then an old age. (The discoverers call him the “old man.”)”
So for these paleo skeletons, a 40-year-old man is rare, and this one had lost his teeth a couple of years ago. Oetzi was considered old too, and he was 46 when he died, and had arthritis. (He ate mainly meat and also wheat, which confuses things).
There probably are simple cultures that have centenarians, but then you are looking at people like the Yuzu and Okinawans.
Kennewick man, OTOH, was 40-55 years old, had “minimal arthritis”, a full set of teeth. And ate almost nothing but seafood.
https://www.mnh.si.edu/arctic/html/kennewick_man.html
“The skeleton is nearly complete, missing only the sternum and a few small bones of hands and feet. All teeth were present at the time of death. This was a male of late middle age (40-55 years), and tall (170 to 176 cm ), slender build. He had suffered numerous injuries, the most severe of which were compound fractures of at least 6 ribs and apparent damage to his left shoulder musculature, atrophy of the left humerus due to the muscle damage, and the healing projectile wound in his right pelvis. The lack of head flattening from cradle board use, minimal arthritis in weight-bearing bones, and the unusually light wear on his teeth distinguish the behavior and diet of Kennewick Man from that of more recent peoples in the region. A fragment of the fifth left metacarpal analyzed by AMS has an isotopically-corrected age of 8410 +/- 60 B.P. (UCR 3476) (ca 7300 to 7600 B.C.). Amino acids and stable isotopes indicate heavy dependence on anadromous fish. DNA was intact, but two partially-completed extractions were inconclusive.
The man lacks definitive characteristics of the classic mongoloid stock to which modern Native Americans belong. The skull is dolichocranic (cranial index 73.8) rather than brachycranic, the face narrow and prognathous rather than broad and flat. Cheek bones recede slightly and lack an inferior zygomatic projection; the lower rim of the orbit is even with the upper. Other features are a long, broad nose that projects markedly from the face and high, round orbits. The mandible is v-shaped,with a pronounced, deep chin. Many of these characteristics are definitive of modern-day caucasoid peoples, while others, such as the orbits are typical of neither race. Dental characteristics fit Turner’s (1983) Sundadont pattern, indicating possible relationship to south Asian peoples. ”
I’d love to see a comparison of the skeletons, the diets, and the health issues, of various ancient peoples!
heathertwist- I’m so sorry, I couldn’t find a link for “Sioux Indians and Centenarians”. I must have read about that in books. However, I’m sure I did read it numerous times. I have the problem that I often get so much of my information from books that it can be difficult to find the same information on the internet. The internet does not contain an exhaustive supply of information on every subject.
I did, however, find a link about gout, which supports what I have read, namely that fructose (and insulin resistance) is probably the main cause of gout. wbryanh might be interested in reading this too!- it contains a short chapter written by Gary Taubes about gout; this is a “missing chapter” from Good Calories, Bad Calories:
http://fourhourworkweek.com/2009/10/05/gout/
Hi Heather, @morgana –
Heather just a quick cautionary note on attributing pathology to N-Glycolylneuraminic acid (Neu5Gc). I too have heard lots of buzz about it. But like so much else, the evidence is just epi data on it, purely correlative. Futhermore, the studies afaik, don’t distinguish between the red meats, eg industrial vs small farm, grain- vs grass-fed, diff meat cuts, etc.
http://www.pnas.org/content/112/2/542.short
“…A well known, epidemiologically reproducible risk factor for human carcinomas is the long-term consumption of “red meat” of mammalian origin. Although multiple theories have attempted to explain this human-specific association, none have been conclusively proven…”
And then it goes on to discuss lab evidence, but in mice, which favor grains, fruits and seeds (think: Anichkov’s utterly flawed dietary cholesterol tests in rabbits). And even here the study’s not mechanistic. All it says is:
“Interactions of this (Neu5Gc) antigen with circulating anti-Neu5Gc antibodies could potentially incite inflammation…”
Bear in mind this protein, likely much unlike the glutenin and gliadin proteins in wheat, *was* in us way back when, and other primates still make their own Neu5Gc. So I’m not yet sold on Neu5Gc’s its inflammatory potential in us.
Eg we don’t what *other* change in the mice chow they made when they ramped up Neu5Gc.
Anyway, Heather, loads of caveats on purported Neu5Gc pathology, all I’m sayin’ … –Bryan
wbryanh, heathertwist- how strange, but my last post appeared in the wrong place in Denise’s comment section…..I’m not sure how that happened! But I hope you guys got it in your e-mail? (I wrote more about meat-based diets).
wbryanh- I had another look, and the only other comment I wanted to make was that you made very good points about longevity! I totally agree that lack of stress, family oriented society, relaxed pace, acceptance of old people, etc., all make a difference in that respect; it’s not just diet alone.
heathertwist- I finally had time to look it up online, and yes you’re right, there are a lot of n=1 cases of people who claim to have problems with arthritis when they eat red meat. (I had never heard of this before; as I said, I knew about a connection between sugar and arthritis, as well as wheat and arthritis). I’m not convinced though that this is a problem for everyone, most particularly for hunter gatherers or people on native diets. I have a theory that it may possibly be due to gut bacteria and digestion; I’m wondering if food that is not properly digested might cause other problems in the body? Especially in the case of autoimmune problems, which i guess arthritis would be. I have also just read online that many people have trouble with inflammation on high fat diets. Again, I find it hard to believe that fats inevitably cause inflammation in everyone, but maybe those who have trouble digesting them properly (i.e. impaired bile function) may experience problems, including inflammation? In any case, in our modern day life digestive issues and food intolerance seem to be rampant, due to various reasons.
Another theory I have in regards to the meat/arthritis link is the eating of mostly muscle meats, which is what we tend to do these days. When you had trouble while eating grass fed beef, do you remember, were you eating mostly muscle meat, or was it all parts of the animal? I’m just curious.
My last theory has to do with lack of variety in the diet. I’ve noticed- and mention this often- that in our society, we tend to eat the same 3 red meats only- (and some people eat only 1 or 2 types)- whereas in hunter gatherer cultures, they ate anything that moved; i.e., many different foods with many different nutrient profiles! We have more varieties of plant foods than we do red meat (now). Even in the Mediterranean, they seem to have a wider variety of animal foods in general than, say, in the U.S.
I totally agree about the variety of meats. When they look at coprolite samples (fossilized human poop! Yes, there is such a thing!) then they can analyze what meals were eaten. The old thought was that humans ate lots of large mammals, because those are the bones that were found. But it turns out our ancestors were often eating a whole lot of things like fish, insects, and lizards, where the bones didn’t survive time.
And I agree that our ancestors were way into the ‘variety’ meats. Actually you can just look at the Lewis and Clark journals. If they were hungry, they might just kill an animal and just eat the tongue. And if the Indians came around, they would grab … and eat … the intestines first (raw!). Gelatin … and/or glycine in general … turns out to be super super important.
For me though, I was way into the whole traditional eating thing, so I was boiling hooves, learning to make tripe, etc. We bought a whole cow and I took the parts that the butcher wouldn’t take, including lungs and spleen. It was a really good learning experience! If you want to REALLY learn biology, go watch a cow taken apart.
Anyway, I totally overdid it, as usual. We ate beef daily, 2 or 3 times a day. Super good beef too! Lots of good thick broth. Also I started making molasses beer, and cooking in iron pans.
What happened is that I got gout. My big toe joint swelled up and my knees got all red and big. My ferritin levels went way up too.
Now, I could control the ferritin with IP6 and donating blood, and drinking tea. But my joints still started swelling when I ate beef. Oddly, this didn’t happen with other high-uric-acid foods, like certain fish.
So when I was on the infamous cruise trip, I ate zero beef and ate mostly raw fish. Bingo! No joint pain.
Now WHY that happened I can only speculate (and I’m continuing to speculate). But later I heard that the farmer I had bought the cow from was giving up ranching, because his joint problems were so bad he could barely walk. And I started actively looking for some HEALTHY older people who lived mostly off beef. I couldn’t find any, either in modern or ancient times. I’d love to see one.
They did eat a huge amount of beef in the 1800’s, but their health was pretty bad. Not heart disease necessarily, or diabetes, but loads of joint problems. And yes, they also ate a lot of wheat. So you have to look at ancient bones to find people who ate lots of large ruminants and also didn’t eat wheat, and there aren’t many of those. But the ones I’ve found aren’t very healthy either. So I’m still looking for my n=1 for heavy meat eaters.
But the thing I could not … and still can not … get my head around is the neu5gc thing. The non-vegan blog writers are mostly punting at this point: “There isn’t enough evidence yet”. Which is true, it’s a new discovery. But it’s very worrying. Sialic acid is a basic part of the immune system, and if human beings incorporate beef-style sialic acid instead of human-style sialic acid, that changes the entire immune system. And I can’t think of any “cure” for it. The body attacks neu5gc so it absolutely is inflammatory. But could it be digested if one’s gut was healthy?
The whole theory behind traditional or paleo eating is that we look at what worked in the past and then replicate it. But what if what was done in the past did NOT work as well as we may have thought? Not all traditional or paleo peoples were equally healthy.
The sialic (neu5gc) acid issue is a completely different thing than the gelatin (glycine) issue or the iron issue or the taurine issue. I think we’ll be hearing a lot more about all 4 of those in the coming years!
heathertwist- thanks for your reply. So it looks like you were eating mainly just beef, so I’m wondering if maybe the problem wasn’t “red meat” in general, but “beef” in particular? I’m also wondering if this is mainly a problem for people who tend to store iron, which is not everybody. The link below explains that joint pain is a symptom of haemochromatosis:
http://patient.info/health/haemochromatosis-leaflet
Apropos gout: I was under the impression that beer was one of the main causes of gout, so can you be sure that it wasn’t the beer you were drinking that caused it? And I agree, wheat is definitely a confounder! Unfortunately, there aren’t too many groups of people nowadays who eat beef without eating wheat….(but I’ll keep looking!) It’s a shame I can’t get any information about the health of the Brazilian gouchos. I was under the impression that they were very healthy, but I don’t know for sure. Dang…..and I only have access to the internet, so I’m limited here…..
I was not under the impression that the beef eating people in the 1800’s were unhealthy, or had gout or joint problems…..but I’ll have to look this up. As I’ve said, I know people who eat quite a lot of red meat (and have done all their lives) that have no problems, so maybe only a minority of the population are sensitive to these things?
Finally, I’m not too worried about neu5gc. Everything I’ve looked at on the subject looks like very dodgy science to me; therefore, I agree, we don’t have enough evidence yet. At least I’m not going to stop eating red meat because of it. I feel great eating meat, and felt rotten all those many years that I didn’t eat it, so that’s my n=1.
” I’m also wondering if this is mainly a problem for people who tend to store iron, which is not everybody. The link below explains that joint pain is a symptom of haemochromatosis:”
Certainly that can be an issue too. And beer, yes! We’ll certainly see in coming years … lots of people doing lots of experiments, which is kind of cool. You and others are doing the “lots of meat” experiment. I’m interested to see the results of all those n=1’s over the years!
“I was not under the impression that the beef eating people in the 1800’s were unhealthy, or had gout or joint problems”
Reading journals and novels written in the period helps. Think about the fact that George Washington had no teeth … most people lost their teeth at a rather young age. Hair too, which is why they were into wigs and headcloths alot. Ben Franklin had horrid gout, and needed glasses (hence he invented bifocals). “Old age” was 60 … and people actually aged faster than they do these days (i.e. getting wrinkly, losing bone mass etc.).
But not everywhere … in some areas people were taller and healthier and aged slower. Northern Europe … England in particular … was one of the worst. The Mediterranean was one of the best, and still is. But England ate mostly sheep, while the Med. countries ate mainly fish.
They tended to be shocked at the lively health and height of the peoples they met while exploring the world. Also their amazing teeth. Which was the whole impetus for Price to go photographing the world.
“Everything I’ve looked at on the subject looks like very dodgy science to me; ”
Dodgy in what ways? I kind of hope they are wrong too, but I can’t find a hole in their science is the problem. Anyway, to answer another question you asked, there are high levels of neu5gc in most land mammals. There is less in pork, and none in guinea pigs. None in birds or fish. Less in milk than there is in meat. I don’t know if it ferments away … I think it might though.
heathertwist- I’m still trying to find evidence that meat eating people were unhealthy, or at least had arthritis and similar ailments, but still can’t find any evidence. I did find the following link though, which confirms everything I’ve read:
http://researchnews.osu.edu/archive/tallind.htm
About the health of Americans in the 1800’s; unfortunately, once again, there are a lot of confounders. Weren’t they eating a lot of wheat (and other grains) at this time? I believe that was actually what Duck Dodgers had said (it was also around the time of Reverend Graham and the introduction of cereal). In addition, I was also under the impression that in those times people drank relatively a lot of alcohol. And the English were already eating a pretty high sugar diet. So, I’m not surprised by some of these health problems you mentiomed, and I’m not convinced it’s because of the meat.
Also, you mentioned that the Mediterraneans, who ate lots of fish and vegetables, were healthier than the English who ate lots of lamb. But in many parts of the Mediterranean they also eat lamb! (Think Greece, Turkey, etc.) So I’m not sure…..And of course, the French have traditionally eaten pretty high meat diets, and they have been quite healthy.
Actually, apropos English health, the author of “The Meat Fix” claims that English people in times past were healthy. I think in both America and England, poor people and people who were crowded in cities might have had quite a few health problems, and living conditions- as well as the food supply- were not always sanitary.
About the “dodgy science” of neu5gc; wbraynh did a great post on that (he beat me to it). I might add a few things, but tomorrow- (it’s late here, and I had a hard day!)
Well, my challenge was to find a HEALTHY group of people that ate mainly meat. I mean, it’s easy to find excuses why this or that culture is UNHEALTHY … stress, wheat, etc. I posted examples of skeletons of meat-eaters that were less than long-lived and healthy, and we have plenty of examples today of unhealthy meat-eaters.
I also have posted examples of HEALTHY peoples who are mainly fish eaters, today and in the past. They all had stresses too, and some also ate wheat (the Mediterranean peoples, for one).
But I can’t find an example of HEALTHY mainly-meat eaters.
This doesn’t disprove the idea: “It’s possible to eat mainly meat and be healthy”. It sounds like you are trying to defend that idea, and basically I’m not trying to attack it. People are experimenting and if someone can do it, they will, and then we will know.
I’m not doing more experiments on myself though, because this one fails on ME, and it hurts when it does. I like lack of pain!
heathertwist- Well, I agree that if meat makes you feel bad, then by all means, don’t eat it! I wasn’t trying to suggest that you *should* eat more of it, by the way- (just so we get that clear). I guess I feel frustrated, because I’ve read a lot about so-called healthy meat eaters in the past- (who, by the way, were eating no, or minimal grain and sugar)- but I just can’t prove it with the internet. That’s my problem…..it’s just frustrating. I guess in the end a lot of it is hearsay, and it depends on who you decide is probably trustworthy in terms of what to believe.
And of course, another caveat is that most of the healthy meat eaters I know of were eating very varied diets, as I’ve mentioned, not just 1 or 2 different types of animals. That’s why I wonder about the health of the Brazilian gauchos (who were eating mainly beef). Because that information would be important. Even the buffalo the Plains Indians ate would have been very different to domestic beef. I really like bison, and it seems like a whole different meat from beef.
Speaking of which, about my “n=1”: although I eat red meat, I don’t eat much beef at all. I’m not that crazy about it these days. Since eating game meat, I just prefer it (same is true of chicken). When I eat meat, it’s usually venison, emu, or when I’m in America, bison. I eat some goat too. I eat offal regularly, which is considered a “red meat” (even if it comes from bird)- presumably due to the nutritional profile.
” I guess I feel frustrated, because I’ve read a lot about so-called healthy meat eaters in the past- (who, by the way, were eating no, or minimal grain and sugar)- but I just can’t prove it with the internet. ”
Well, when I brought it up, it wasn’t to prove anything. My theory is that the “seafood diet” is healthier than the “inland diet” … and in general, that appears to be the case. Most humans for most of history lived on the coast. But my caveats were … and are … that there are so many confounders that it’s hard to figure out WHY. And I mentioned a number of the confounders:
1. Shoreline: Seafood, chicken, sometimes pork. It has loads iodine, Omega 3, taurine, fish oil (Vit D and A). Tends to be based on rice. Tends to have loads of vegies, and seaweed. In Asia, tends to have a fair bit of soy and fermented food. Maybe they fermented more because they had easy access to salt …
2. Inland: Mammal meat, chicken, pork. Tends to be based on wheat and potatoes, high iron levels, low urinary taurine levels (I’m still not sure how much is in the diet), higher neu5gc levels, the pros and cons of milk. Tends to have fewer vegies. Tends to feature fermented milk (or cheese).
3. Vegan: This is a new thing! But the modern version tends to be based on 1, for whatever reason, except without the fish and shellfish. The Yuzus are mostly in 1 (they eat some amount of fish and a fair bit of fermented soy).
So there are two very very different diets that large groups of people follow. I grew up on 2. Now I switched to mostly 1. There are lots of differences between the two diets. I theorize, but exactly WHY they work differently is hard to pinpoint.
I haven’t seen a whole lot though, about people comparing shoreline to inland diets. The Paleo and WAPF folks mostly talk about inland diets, which is, after all, the history of most of us English-speaking folks. The other big group are Vegans, who are anti anything of animal origin. So there aren’t many people speaking up for the shoreline diet! Some people are moving from 3 to 2, or 2 to 3. Not many moving from 1 to 2 or vice versa.
It’s coming though … you’ll see more comparisons and then the picture will get clearer. Meanwhile if you are doing well, kudos! You are way better off than back when we lived off Taco Bell!
Plains Indians: I agree the meat-eaters are taller. There is something about beef that makes people “beefy”. Which is likely not surprising … big ruminants are BIG and likely they have enzymes etc. to support that. But you see it in the Japanese too: they are hardly starving, but they tend to be short. Dairy eaters tend to be even taller. Milk makes baby cows grow big fast!
However, the idea that being tall means you are healthier is pure faith. If you live in a meat-eating country and you are shorter than your fellows, then yes, you aren’t eating much food. But the average short Japanese is quite healthy.
The levels of arthritis … you have to look at the bones. Lewis found the Indians had high levels of joint problems, and that was at a time where the Indians were doing well. But really it would be better to have some documentation from skeletons.
“Also, you mentioned that the Mediterraneans, who ate lots of fish and vegetables, were healthier than the English who ate lots of lamb.”
No, the English ate a lot of mutton … full-grown sheep. Part of the difference is that you only get lamb once a year or so. But likely more of it is that the English ate very little fish, for some reason (given that England is surrounded by water … ). Maybe it’s just easier to go fishing in the Mediterranean. In the taurine studies, they measured the taurine urinary excretion rate. England was on the very low side, Japan was on the highest side. The Med. countries were smack in the middle. So the Med. people are smack in the middle for heart disease, between Japan and England. The Japanese are the highest in eating fish and eggs, the English the lowest, and the Med. folks in the middle.
Might be total coincidence. Or it might have something to do with qty of fish in the diet.
“Actually, apropos English health, the author of “The Meat Fix” claims that English people in times past were healthy. ”
They were! They also ate a diet that was mostly fish. Then suddenly they switched to farming and stopped eating fish almost totally … and their health crashed. It’s the weirdest thing.
http://news.nationalgeographic.com/news/2003/09/0924_030924_neolithicdiet.html
They find that the shift was rapid and complete at the onset of the Neolithic. “Marine foods, for whatever reason, seem to have been comprehensively abandoned,” the researchers conclude in the September 25 issue of the journal Nature.
…
“The previous hunting-fishing-gathering way of life was extremely successful for humans—it is the main way we have obtained food for most of our existence—so it seems strange that we would give this up so readily to start farming and stock-keeping within a generation or two,” said Richards.
According to Copley, this research highlights how advantageous the Neolithic diet of farm animals, dairy products, and cereals must have been. For example, he said, it allowed populations to boom and larger, more complex societies to emerge.
“Of course, it poses more questions,” he said. “For example, are marine foods still consumed during the Neolithic but in much lower abundances? And why is there this very quick shift in diets?
http://www.beyondveg.com/nicholson-w/angel-1984/angel-1984-1a.shtml
Here we present a summary of a classic paper on the health and longevity of late Paleolithic (pre-agricultural) and Neolithic (early agricultural) people. [Source: Angel, Lawrence J. (1984) “Health as a crucial factor in the changes from hunting to developed farming in the eastern Mediterranean.” In: Cohen, Mark N.; Armelagos, George J. (eds.) (1984) Paleopathology at the Origins of Agriculture (proceedings of a conference held in 1982). Orlando: Academic Press. (pp. 51-73)]
Note that these figures come from studies in the field of “paleopathology” (investigation of health, disease, and death from archaeological study of skeletons) of remains in the eastern Mediterranean (defined in Angel’s paper to also include Greece and western Turkey), an area where a more continuous data sample is available from ancient times. Due to the unavoidable spottiness of the archaeological record in general, however, samples from the Balkans, the Ukraine, North Africa, and Israel were included for the earliest (Paleolithic and Mesolithic) periods. While the populations in the region were not always directly descended from one another, focusing the study within the eastern Mediterranean minimizes bias in the data due to genetic change over time.
heathertwist- I’m going to answer your post kind of quickly, since I’m getting quite busy now, so I may miss a few points.
First off, I agree that “height” and “health” are not exactly one and the same; that link was probably a bit lame, but as I said, the internet is really limited. All of what I’ve read about the health of Plains Indians was in books, and I can’t replicate that. The Plains Indians were tall though, but not “beefy”; in fact, they were tall and thin. They were not eating any beef whatsoever, they were eating mostly buffalo; a very different meat with a very different nutrient profile! About Lewis and Clarke claiming they had joint problems and rheumatism; I’ve never seen this confirmed, I’ve only read it from you. It may be true; however, I’ve also read that there were many centenarians among them, and these types of problems- arthritis, rheumatism, etc.- do tend to happen to older people, especially if they are living in the damp and cold. Are you sure that all the centenarians among your Japanese Mountain people are totally free of all aches and pains, or other small problems? I think the more important point though is that all these people weren’t/aren’t getting cancer and heart disease! Of course I don’t know which people Lewis and Clarke claimed were riddled with joint problems; young people? children? I doubt it; the Indians were fierce hunters and warriors, so they must have been in pretty good shape.
About heart disease and fish eating: yes, fish does seem to be protective. I think that’s been pretty well proven. Although the people that John Nicholsen said were healthy- (in England)- were his grandparents, so they were already eating a meat, not a fish diet. He said they ate meat, dairy, butter, and lots of vegetables, and not excessive carbohydrates or sugars; and of course it wasn’t processed food. Apropos heart disease; you say Japan was on one end, England on the other, and the Mediterranean in the middle. But what about the French? Most particularly, the region of Gascony (which has the lowest heart disease rate in France)- where they eat lots of liver, goose pate, and cook in duck and goose fat? Although I agree that fish seems to be protective, I’m not sure that it’s the only thing…..I don’t think it’s that simple.
Moraga, @heathertwist — Morgana, you’re right, a lot of arthritis comes from auto-immune response. But I caution against relying much on the n=1 cases of people who claim to have problems with arthritis when they eat red meat. The potential confounders are legion. What cuts of meat did they eat? From which species? How were they raised – grain- or grass-raised? Was the meat processed or fresh? If fresh, whole meat (like steak) or ground, the latter which is much more prone to collect and harbor pathogenic E.coli? What else did the respondents eat with their meal? And on.
Heather, sorry, I know you have your eye on red meat and Neu5Gc, but I have to be more reserved about this matter for the moment! For reasons posted earlier, I’d have to see a lot more on Neu5Gc to consider to indict it. It’s quite possible red meat–and the things that purport to help explain it, eg Neu5Gc–get demonized through anecdotal and the wholly correlative epi studies, without researchers getting actual proof. Like what happened to cholesterol, salt, sat fat and MSG. –Bryan
“Neu5Gc–get demonized through anecdotal and the wholly correlative epi studies, without researchers getting actual proof.”
To be clear: I’m not saying neu5gc causes arthritis. I do know FOR ME beef gives me swollen joints. Neu5gc might be one cause. Or some other thing that hasn’t been discovered yet. It does seem to be fairly common. If your joints don’t get swollen … kudos! My sisters are living off Advil. Would perfect grass-fed beef help? I don’t know … it didn’t help me though.
However, the stuff about “neu5gc” isn’t anecdotal. It’s fairly simple lab testing: it is a sialic acid that for some reason, gets incorporated into human tissue. It does get attacked by the immune system. The “opinion” part is: “How much of an issue is this anyway?”. Good question. For me it’s kind of a moot point. I eat steak when I feel like it, and put up with the swollen joints for a couple of days.
If someone asks though, “Why might a VLF diet help a person?” or “Why do some people feel better on a vegetarian diet?” I have to say that “sometimes not eating beef makes some people feel better”. And “I have more examples of healthy fish-eaters than I do of healthy meat-eaters”.
Maybe to be a healthy meat-eater, you also have to be eating only grass-fed beef and also be low-carb and also eat lots of organ meats. I didn’t do the “low carb” part of that, and really, I’d rather not if I can help it.
Heather, @morgana —
Heather, what you say here: “ [Neu5Gc] does get attacked by the immune system…”
Thank you for this ticket to ride a great thought train!
You appear quite right to say we make antibodies for Neu5Gc:
http://journals.plos.org/plosone/article?id=10.1371/journal.pone.0058443
A Simple Method for Assessment of Human Anti-Neu5Gc Antibodies Applied to Kawasaki Disease
But we find this within:
“…In cancer, [these antibodies] have dualistic and opposing roles, either stimulating or repressing disease, as a function of their dose…]
What?! Way I read this Heather, to eat red meat at a certain level may–I say *may*–actually help us *avoid* cancer!
Of course we also need to consider our other Neu5Gc sources and their amounts.
In general, it provokes this question: Can Neu5Gc, and the antibodies it invokes, make us less healthy or *more* healthy? Ie via our hormetic response to it? Similar to the hormetic response we may experience against some or even many of the 5000 phytochems we eat from plants?
http://www.sciencedirect.com/science/article/pii/S0925443911002523
Cellular stress responses, hormetic phytochemicals and vitagenes in aging and longevity
This idea challenges the conventional notion that antigens serve solely to promote chronic inflammation and disease. And it certainly reconciles with the ancestral idea that we consistently ate at least some red meat since we split from the chimps ~ 6mya. Chimps, who btw, produce Neu5Gc and they do occasionally hunt down and eat red meat, esp red colubus monkeys.
For us, Neu5Gc is like Vitamin C in one respect–we advanced vertebrates lost our ability to produce it somewhere along the line. For whatever reason. Maybe because we started to get enough of it in our food?
I’d like to know why we evolved to favor the closely-related Neu5Ac variant. Which seems to serve a similar dual role as its close cousin Neu5Gc both to prevent and (hormetically?) enable disease:
https://en.wikipedia.org/wiki/N-Acetylneuraminic_acid
“… Along with involvement in preventing infections (mucus associated with mucous membranes — mouth, nose, GI, respiratory tract), Neu5Ac acts as a receptor for influenza viruses…”
Btw, here’s an intriguing survey of various vertebrates and how they lost endo Vit C through the ages:
http://www.ncbi.nlm.nih.gov/pmc/articles/PMC3145266/
The Genetics of Vitamin C Loss in Vertebrates
Finally, Chris Kresser offers one of the more clear explanations I’ve read on Neu5Gc and why and in what ways we should care about it:
http://chriskresser.com/heart-attacks-and-red-meat-correlation-or-causation/
“…[Neu5Gc is]…a monosaccharide—that’s a single sugar—that acts as a type of signaling molecule in mammalian cells. One of its functions is to help the immune system distinguish between self and foreign cells. Humans actually lost the ability to produce this Neu5Gc millions of years ago through a genetic mutation, although we still produce a compound that’s closely related called Neu5Ac. But humans are unique in this respect, because most other mammals still do produce Neu5Gc, which is why that compound is found in mammalian meat that humans eat. When we consume red meat and milk products, we incorporate this compound, at least some of it, into our own tissues, especially tissues that grow at a fast pace: a developing fetus, epithelial and endothelial tissues, and tumors, either benign or malignant tumors.
The concern is that most of us have anti-Neu5Gc antibodies circulating in our blood. Some researchers have suggested that these antibodies react with the Neu5Gc in our tissues to create chronic inflammation, leading to chronic diseases like cancer. Essentially, we’re having almost like an autoimmune reaction against the meat. And through molecular mimicry, because we have the Neu5Gc in our tissues, then in a similar way to gluten intolerance, we’re getting attacked against our own tissues, not just the Neu5Gc in the meat itself. The problem with this hypothesis is that researchers are nowhere near proving it. It’s a theory; certainly an interesting theory, but the research is at the very early stages. We need studies to confirm or refute these hypotheses. Most of the studies that have been done, if you actually read the full text of the paper, acknowledge that. They say, “At this point, these results are preliminary. We need lots more research. It would be irresponsible to draw conclusions from this.” But of course, the media does not pick up on that nuance. The media does not like nuance…”
–Bryan
“When we consume red meat and milk products, we incorporate this compound, at least some of it, into our own tissues, especially tissues that grow at a fast pace: a developing fetus, epithelial and endothelial tissues, and tumors, either benign or malignant tumors.”
I basically agree with Chris on that one. I agree it’s not proven either. What I found though is interesting. The animals that have only the AC variant … fish and birds … don’t age in the same way as the animals that have mainly the GC variant. So with fish, for instance, they just keep getting older and older, but they don’t get grey and decrepit. Except, oddly enough, ONE particular fish: salmon. And they age suddenly, as they head upstream to spawn and die. Other fish don’t do that. Birds don’t do it either … you can have this really old albatross (64) leading an incredibly stressful life, and still breeding every year.
https://www.washingtonpost.com/news/speaking-of-science/wp/2015/11/30/at-the-ripe-age-of-64-wisdom-the-albatross-is-doing-the-unthinkable-preparing-to-lay-another-egg/
In mammals that have both GC and AC, the GC is associated with fast-turnover cells. The AC is associated with long-lived cells, like brain cells.
Over and over, the species I found with mainly GC are short-lived and have “old age”, while the AC ones are longer-lived and die mainly from illness and accident. This is true for mammals too … there are only a few mammals that are mainly AC. Guinea pigs for one, which live quite a bit longer than their cousins, the rats. (Rats are old at 2 years old, while GP’s can reach 15).
And humans live longer than our cousins, the chimps. Which is why I started looking: is it possible that eating mammal meat is associated with human aging? Are there long-lived people (like the Yuzus) that are mainly meat eaters?
I didn’t find any. There ARE long-lived dairy eaters, but then mammal milk has more AC than the meat does, and it may ferment out.
Usually when I bring this up on groups I get answers like: “Oh yeah, there was this group that so-and-so said lived a long time” or “we can’t possibly know how long people lived in the past because they died in childhood a lot”. Or, “They only got ill because of something else … “. And basically, the lack of a thing doesn’t prove it doesn’t exist. We don’t KNOW Nessie doesn’t exist, and likely never will.
Anyway, the excuses about why ELSE the meat eaters might be unhealthy or why it’s impossible to “know for sure” … isn’t an interesting question for me. Someone else will do the plodding science that is needed for certainty. I’m more apt to just do the experiment and see what happens!
In the meantime, there are loads of cultures that don’t eat mammals and are doing better than the average American, so I can’t see any pressing reason to eat more. I do think they are part of our farming and grassland ecosystem, and I have two goats myself, which shear and fertilize my lawn nicely! And if I could drink their milk I would (goat milk is high in taurine!).
Heather, @morgana, good morn/aft to you. And Happy Groundhog Day…Happy Groundhog Day…Happy Groundhog Day… (yanks alarm clock out of wall socket)
Heather, your stuff on Neu5Gc/Ac here, it is seriously interesting!
What you say here:
“In mammals that have both GC and AC, the GC is associated with fast-turnover cells. The AC is associated with long-lived cells, like brain cells…”
I’m busy googling away for links on that and post here a Jaminet link that may relate to it.
Meanwhile if you have any (more), please post them!
This Wiki suggests the two sialic acids enable cell-binding points for diff pathogens:
https://en.wikipedia.org/wiki/N-Glycolylneuraminic_acid
“…Humans should have been less susceptible to Neu5Gc-binding pathogens and more susceptible to Neu5Ac-binding pathogens. It is suggested that human ancestors survived a then-prevailing malaria by eliminating their Neu5Gc production. However, with the rise of Plasmodium falciparum, the parasite that causes malaria today, humans were once again endangered as this new strain of the malaria had a binding preference to the Neu5Ac-rich erythrocytes in humans…”
So this Wiki (fwiw) suggests maybe Neu5Ac doesn’t somehow confer some fundamental and immutable longevity benefit over Neu5Gc. But that, in the ever-shifting pathogen environment, maybe Ac ended up for the moment being “the good guy.” Or at least “the better guy” than Gc.
The Jaminets offer some intriguing backdrop and discussion on Neu5Gc’s role, starting here:
http://perfecthealthdiet.com/2015/01/neu5gc-red-meat-human-disease-part/
When I have time I will try to vet the Jaminets’ sources and what they say here. I try to do that AMAP as a general rule. And when I poked into a few of their past posts, I found the Jaminets certainly don’t merit an exception to that rule. Though they are generally better than many, maybe even most of the major diet/lifestyle/health bloggers.
Anyway guys, a few Jaminet giblets–or should I say sashimi tidbits?–that stand out:
“…this [Neu5Gc to Ac] mutation by itself may have led to a speciation event, after which our ancestors could no longer mate with other apes. From that point on, Neu5gc-less females had difficulty producing children with males who retained the Neu5gc gene, because they would form antibodies against Neu5gc-coated sperm, making fertilization unlikely…”
“…The human brain is extraordinarly rich in sialic acids: neural membranes have 20 times more sialic acids than membranes of other human cell types. Animal brains are also enriched in sialic acids relative to their other tissues, but not as much as in humans; the human brain has 2-4 times more sialic acids the brains of other mammals…Curiously, though, Neu5gc is rare in the brains of all animals. Neu5gc is strongly suppressed, by about 98%, in the brains of all vertebrates…”
BUT, Heather, the Jaminets give this too, which does not resoundingly support the no-low-Neu5Gc/longevity idea:
“… Neu5Gc has been lost independently in some other mammals as well – ferrets and new world monkeys. New world monkeys such as capuchins and spider monkeys also experienced a brain expansion, and ferrets are notably smart, so either explanation might be relevant to these cases of ‘convergent evolution.’…”
https://en.wikipedia.org/wiki/New_World_monkey
I haven’t been able to confirm that New world monkeys make Neu5Ac, only that they no longer make the Gc variant:
http://www.ncbi.nlm.nih.gov/pubmed/25124893
Capuchins live 15–25y in the wild, up to 45y in captivity
https://en.wikipedia.org/wiki/Capuchin_monkey
Spiders live to ~ 22y in the wild:
http://animals.nationalgeographic.com/animals/mammals/spider-monkey/
Howlers live to 15–20y in the wild:
http://animals.nationalgeographic.com/animals/mammals/howler-monkey/
And ferrets live 7–10 years:
http://www.ferret-universe.com/
And which do endo-make only Neu5Ac:
http://www.nature.com/ncomms/2014/141217/ncomms6750/abs/ncomms6750.html
Heather, I’m not saying these monkeys and ferrets invalidate your Neu5Ac/longevity idea. Maybe they suffer mitigating factors that shorten lifespan. But we need to include their stories.
I also just learned our very own Neisy discusses something similar in this very post. (Her post is so l-o-n-g-g-g, I’m sure I’ll discover things in it for years.) Neisy suggests the purported pathogenicity of sat fat could be a red herring to Neu5Gc:
“… We produce a similar molecule called Neu5Ac, but lost the ability to make Neu5Gc after splitting from our last common ancestor with the great apes. … Other primates (and almost all mammals) can still synthesize Neu5Gc just fine! …Here’s why it matters: even though we can’t make Neu5Gc on our own, we can incorporate it into our tissues when we ingest it from food. And the prime sources of Neu5Gc happen to be red meat and dairy, the same food-vehicles that deliver most of our saturated fat. Because Neu5Gc looks like a foreign substance to our paranoid human innards, we’re capable of producing antibodies against it (although levels of those antibodies vary widely from person to person), which, in turn, can stir up all sorts of trouble. So far, we’ve got theories about a potential role for anti-Neu5Gc’s antibodies in systemic inflammation, cancer, heart disease, hypothyroidism, and also… WAIT FOR IT… multiple sclerosis … I waffled over whether to even include this speculation here, since Neu5Gc research is just a wobbly-kneed babe in the woods right now, and we’d need a lot more data before we could definitively link it to any disease. But, considering that 1) humans are the only primate that develops multiple sclerosis, 2) humans are the only mammal that can’t make Neu5Gc (and that produce antibodies against it), 3) multiple sclerosis tends to cluster around areas with a higher intake of Neu5Gc-containing foods (land meat and dairy), and 4) there’s a plausible mechanism linking Neu5Gc with the development of multiple sclerosis (through the effects of antibodies on the blood-brain barrier and axon-myelin unit)… well, all I’m sayin’ is it seems quite intriguing!…”
BUT Heather, all that said,on longevity and animal-sourced foods, maybe we can explain the matter more simply?
It’s my sense that the “Blue Zone” and other very long-lived folks, they tend to limit *all* animal-sourced foods. Not just red meat, but poultry and fish too. Eg the Okinawans’ seafood-centered foodway, though they eat pork too. The Seventh Day Adventists in Loma Linda some of whom are vegan, others who avoid all animal flesh but eat eggs and/or dairy, while some others actually eat red meat:
http://www.seventhdayadventistdiet.com/
So maybe it’s not so much the presence or absence of specific compound(s) like Neu5Gc, but maybe the chronic protein load?
Or even simpler–a persistent cal “restriction” eg the Okinawans’ 80% rule? Maybe that, with the emphasis on plant-sourced foods, with their high amounts of micros and fiber, that simply allows the person to eat fewer overall calories and still be happy and energetic?
This makes me think of my fasting experiences. I’ve fasted hundreds of times since 2009. *Without fail* fasting makes me feel better, more energetic, calmer, my bod much more *in synch* with itself. I perceive my cognition to soar during my fasts. It goes back to what I discussed earlier here, that fasting promotes autophagy, that our bods begin to clean out the molecular detritus from our cells’ cytoplasm so the very many metab processes within all happen much more efficiently.
Btw, to fast is to “eat” the ultimate VLC-VHF foodway. It’s a near 100% fat diet! All endo fat 🙂
–Bryan
wbryanh, heathertwist- Here is part 2 of that Jaminet link:
http://perfecthealthdiet.com/2015/02/neu5gc-autoimmunity-hashimotos-hypothyroidism/
Interestingly, in the comment section below he claims that Neu5gc is only a problem for people who have certain gut bacteria, i.e., it’s only a potential problem for some of the population who are sensitive. This makes more sense to me. We’ve evolved to eat meat (and fish too, I’m not disputing that); it’s illogical to believe that the food we’re meant to eat would be killing us at the same time. Although it’s certainly fashionable for the media to condemn meat at the moment! (I believe there is an agenda out there to persuade us to stop eating meat, for whatever reason!- but that’s another conversation….)
wbryanh- I thought your idea about neu5gc and “hormesis” was extremely interesting! Just like plant foods, which are also high in “toxins” and “poisons”, which we’re told all the time are good for us. They may well be good for us healthy people because they make us stronger; not so for certain people with sensitivities. My brother has problems with oxalate in foods. Many people have problems with nightshade vegetables; in fact, nightshades have also been linked to body aches and joint pains. It may not be the “meat”, per se, but just whatever substance your particular body is sensitive to! I, myself, seem to have more sensitivities to various plant foods, though interestingly enough, ever since my fasting experiment, that seems to be much better.
Lastly, in the part 1 of this Jaminet link- (the one you posted, wbryanh)- Paul Jaminet mentions that the experiment was done under artificial conditions- (i.e. mice were artificially made to be “like us”). I agree! This was exactly my problem with the whole thing in the first place. They have no way of really knowing how neu5gc reacts in the human body; we’re not germ free mice who’ve been given a shot of neu5gc + antibodies. So often, things work so differently in the human body than how we think. I have nothing against science, that’s how we learn, but nutrition science is just in its “infancy”, and people tend to jump to conclusions too soon and get it all wrong. After listening to others and having major health problems, I’ve finally decided to go with how *I* feel….nothing else. I’m interested in the discussion maybe, but my body is the “experiment” that I ultimately listen to. Oh yeah…..in the first paper I read on neu5gc, the heading was “We Know That Red Meat is Bad for Us; Now We Might Finally Know the Reason Why”. Whoa! Major bias there. That was a big red flag for me.
Hi Morgana, @heathertwist —
Morgana, very good points on the phytochems that are fine for some us but which other people react badly to, like oxalates.
How different is Neu5Gc really from some other compounds we routinely eat? From both plant and animal sources?
We routinely eat compounds from both animals and plants that causes our bods to make antibodies against them.
Lectins are a huge class of antibody-inciting compounds. These are carb-binding proteins we eat from animals and plants. Just like Neu5Gc, they can incorporate into our tissues. For at least some lectins, we produce antibodies:
https://en.wikipedia.org/wiki/Lectin
http://www.precisionnutrition.com/all-about-lectins
http://www.ncbi.nlm.nih.gov/pubmed/7683052
Of course the biggest example of potentially problematic phytochems: some gliadin proteins in gluten. Like for Neu5Gc, our bods generate antibodies to these potentially offending proteins, and most providers offer blood tests for that–IgA, IgG, and IgE. Yet it *appears* many people are unaffected by these glutenous proteins, and may even experience a healthful hormetic effect when they eat glutenous grains like wheat at or below threshold amounts. Though certainly many of us should avoid these gliadin proteins completely!
https://en.wikipedia.org/wiki/Anti-gliadin_antibodies
With so much, often “the dose makes the poison.” –Bryan
1. The theory about neu5gc and binding pathogens … yes, that is the main theory as I understand it. What that doesn’t say though, is why the AC version is used in brain cells and other “slow growth” cells.
2. I don’t know why some animals have only AC and some don’t. In the case of guinea pigs, it may well have been human breeding. Guinea pigs are very much an artificial animal: they can’t survive in the wild. And perhaps while AC HELPS animals live longer, there still needs to be other changes for the animal to actually survive longer.
There is a knockout mouse that only makes AC … I haven’t read anything that it lives longer. So there must be more to it than that? One question might be: are any of the “non-aging” animals (like fish and birds are) based on GC? Are there differences in their brains or aging patterns? Ferrets and monkeys are among the most intelligent animals, for starters.
It just seems that there is more to it than just bacterial/virus issues. It has a lot to do with cellular aging within the body.
3. Jaminets: I like them a lot. And the bit about breast milk is important: esp. if you are going to have a baby! No one though, has explained why birds and fish don’t age. I mean, they study aging in worms and flies and mice and chimps … but not the lack of aging in birds and fish. Actually dolphins too … they don’t age in the same way other mammals do.
Dophins, I think, do have the GC version also. BUT … their diet is about all fish, which is pure AC. Ditto for the long-lived albatross. All it eats is fish.
4. In this blog article: Yes, I noticed that! It’s a fair question. Denise has a good summary of the issue there. Yes, there isn’t much info on it yet.
5. “t’s my sense that the “Blue Zone” and other very long-lived folks, they tend to limit *all* animal-sourced foods. Not just red meat, but poultry and fish too. ”
Do they? When I go to a Korean or Japanese store, they don’t seem to skimp on protein in general. I was there today, and there was a good 15 feet of shelf-space JUST for squid. And more for fin fish, plus stuff like crab, crayfish, oysters, mussels. A little fair bit (4 feet) for hooves (cow and pigs) and heads (mostly fish) and innards. A little bit for beef (thinly cut rib meat) and pork belly (maybe another 4 feet). And a whole section for several kinds of eggs (including fermented and balut).
Mind you the vegie section was way bigger. But compared to the average American store, there was WAY more space for protein foods.
Shelf space is a pretty good way to figure out how much is actually sold. Most grocery stores these days work on computer algorithms that “reward” shelf space according to how much sells. It’s very exactingly calculated. There are a few “loss leaders” for foods that attract customers even though not much is sold, but mostly, if there is a lot of shelf space, people are buying it.
Now this might not reflect people in Japan or Korea, but I suspect it’s close. The “traditional” folks here look and act much like the people I see in their home countries. The ones that have adopted our lifestyle … tend to look like it.
Anyway, I haven’t seen that “protein” in general is an issue. Maybe the balance of it is, with glycine. But the thing is: in a shoreline diet, there is a “stop” limit on the protein. I can be really really really hungry, and sit down to a meal of mackerel and rice and vegies … but I can’t eat all that much. Maybe 3 oz squid and half a cup of rice, and a cup of vegies. Squid is worse. One piece and I’m full and happy. But I went to PF Chang’s for lunch today, and downed half a big bowel of egg drop soup, a whole order of street noodles (GF) and some beef and green onions and a bowl of rice. My stomach hasn’t shrunk at all. PF Chang’s food just doesn’t fill it up.
Even weirder: the same thing happens to my old cat! She was driving us crazy, because she cried for food ALL DAY LONG. Loudly. But if we fed her all she wanted, she threw up. We kept a timer to feed her on a schedule because it was such an issue. I started adding the taurine and now she laps up her food … and then goes to sleep for 3 hours or so. (BTW she treats the taurine bottle a lot like a catnip bottle. Makes her go nuts.).
So is eating less protein keeping her healthy? Or does eating the CORRECT protein make her eat less? Based on my personal experience I suspect the latter.
6. Fasting: “It goes back to what I discussed earlier here, that fasting promotes autophagy, that our bods begin to clean out the molecular detritus from our cells’ cytoplasm so the very many metab processes within all happen much more efficiently.”
There is a lot to that. I did Fast-5 for years, until I got into issues with medications that can’t be taken on an empty stomach. It worked.
Heather, @morgana, good day gentlefolk–
Heather, about aging, do you know about the Hayflick Limit?
https://en.wikipedia.org/wiki/Hayflick_limit
This suggests each species has an evidently genetically determined limit on how many times a cell can divide before its chromosomes’ telomeres shorten so much it prevents further division.
https://www.tasciences.com/what-is-a-telomere/
The Hayflick Limit may go a long way to determine inherent longevity and senescence rates for each species. Our human cells (on average? or for the cells with the lowest limit, so thus give the “gating” factor in our senescence rate?) have a Hayflick limit of 40 to 60 divisions. Galapagos tortoises have a Hayflick Limit of 110 divisions.
Of course you can adjust your environment (which includes diet) to extend the cell life *between* the divisions. Eg by preserving the telomeres which act like protective caps on the ends of our chromosomes similar to the way shoelace caps keep shoelace ends from fraying. The sialic acids may play a role in extending or shortening inter-division cell time.
A quick Google didn’t turn up any connection between Neu5Gc/Ac and the Hayflick Limit. But maybe you’ll find one?
Btw, here’s a Wiki fwiw on species that apparently enjoy biological immortality, whose cells lack a clear Hayflick Limit, eg because their tissue is so rich in telomeres, such as in lobsters. Maybe there’s a monster Godzilla-sized lobster clomping around the sea floor in the North Atlantic. (if it solved the big-lobbie moult problem):
https://en.wikipedia.org/wiki/Biological_immortality
This senescence researcher suggests that species that evolved to sexual reproduction also started to age, suggesting the two may be related:
http://www.senescence.info/aging_animals.html
Hm. Reminds me of a Woody Allen quote (from Sleeper?) 🙂
Heather about your example that you quickly fill up on squid but can’t fill up at PF Chang (I’ll guess PF Chang doesn’t mind that). I suspect that, like most things in our diet and elsewhere in our environment, it’s super multifactorial, it goes way beyond “correct” and “incorrect” protein. I do think protein quality matters, that the more correct balance of AAs we get to replace those we typically use up and excrete, the less overall protein we need to eat. We even see attempts to quantify these AA balances, eg the PDCAAS rating system:
https://en.wikipedia.org/wiki/Protein_Digestibility_Corrected_Amino_Acid_Score
though this is far from exact as you can imagine and may not be any more useful than the Glycemic Index charts. Nevertheless, it’s one of the (many) reasons I eat at least two eggs most every day. Besides being an eminently ancestral food, eggs score near the top for PDCAAS.
Our bods need the proteins and other calories of course but also the micros (vits and mins) and other nutrients, which may include the trace minerals that govt’s haven’t yet listed, like chromium, vanadium, and molybdenum. You may continue to get the hunger signals even if you eat enough calories but still fall short on the micros. I have heard our bods can send us specific and legitimate signals–eg when I’ve worked hard on a hot and humid day, I can crave salt and immediately feel better when I eat some. It’s the kind of hard-wired impulse that leads Mountain Gorillas to chew on rotting wood even though they get no calories from it–but they get salt which is very hard to find in their habitat.
http://rsbl.royalsocietypublishing.org/content/2/3/321
But I also feel that often our bods can’t tell us specifically what it needs and so simply tell us to “eat.” –Bryan
1. Telomeres
“Our human cells (on average? or for the cells with the lowest limit, so thus give the “gating” factor in our senescence rate?) have a Hayflick limit of 40 to 60 divisions. Galapagos tortoises have a Hayflick Limit of 110 divisions.”
Except when it comes to the non-aging animals:
“Telomere length in blood cells declines between the chick stage and adulthood in both species. However, among adults, telomere length is not related to age. This is consistent with reports of most telomere loss occurring early in life in other vertebrates. Thus, caution must be used in estimating annual rates of telomere loss, as these are probably not constant with age”
http://www.ncbi.nlm.nih.gov/pubmed/15306302
I’m thinking it is something like in plants … some plants are annuals or bi-annuals, and have a set “death date”. Some plants are perennials, and will just keep going and going (and can be propagated by cloning too!). So the perennials have immortal cells, even though most of them also have sexual reproduction. Perennial plants do age, sort of, but they don’t have a set death date.
I kind of think it’s related to population control. Some species are just very very “portable”, and if they overpopulate in one area they just spread to another … like fish and birds. Others are very local and populate very quickly … like mice and rabbits. So the mice and rabbits just die at a certain age, unless a predator eats them first. If long-lived mice in history showed up, they probably died out. Seabirds though, have a near-infinite supply of food.
In plants, there is a “switch” such that the same species can be bred to be perennial. They are breeding perennial corn and rice now … it wouldn’t have to be replanted every year and the roots would be way deep so it would be more drought-proof.
Hmmm. Yes sialic acid is related somehow to telomere activity? Seems like it’s still being figured out.
“http://www.kocatepetipdergisi.aku.edu.tr/PDF/Mayis%202007/04%20_19-24_%20Didem%20Cosan.pdf”
In mammals the AC sialic acid tends to be used in the low-turnover cells, like brain cells. Gut cells turn over very quickly and use the GC version. Cancer cells grow and replicate quickly, but I think they also don’t die? (the cancer cell lines are immortal?). Cancer cells seem to hoard the GC in the body.
2. Satiety: “You may continue to get the hunger signals even if you eat enough calories but still fall short on the micros. ”
Yes! That has been studied a lot in farm animals, esp. the ones they want to have grow quickly, like chickens. In chickens methionine is the appetite regulator. If there is too much methionine in chicken feed, the chickens grow up healthy and not fat, but slowly. If there is too little met then they grow quicker but get fat. “Just enough” met and they grow fast but not fat.
Anyway, eggs are high in met, so they make good diet food. Squid are high in met too. But the squid is even more appetite-suppressing than eggs, so I think it’s the other amino acids … which we tend to be short in.
Very slowly digested foods also affect appetite a lot. I keep track by meal: some meals keep me full a long time, while others just make me hungry quickly. I used to get hungry ALL THE TIME and could never fill up. The taurine drink though, seems to stop that regardless of other food in my diet, which makes me think that the tau/gly/arg mix affects appetite rather a lot. Although the mix also has konjac and C and xylitol, so there is that! Probably would need more experimenting … konjac has the nice property that it helps prevent ulcers and reflux, which is an issue for me if I go for a long time without food (which is why I gave up intermittent eating).
Heather, @morgana —
OK Heather. More devil’s avocado for you!
Do you have more links on “ageless” animals? In addition to the Wash Post piece on the 64yo still-breeding albatross?
What you say here: “…non-aging animals…” Maybe better to say “slow-aging” animals? After all, which animals experience no senescence at all?
I made an earlier post that talks about “ageless” lobsters. Maybe I jumped the gun? This Smithsonian link seeks to debunk it:
http://www.smithsonianmag.com/science-nature/dont-listen-to-the-buzz-lobsters-arent-actually-immortal-88450872/?no-ist
“…older crustaceans stop shedding their exoskeletons altogether—a clue that they’re near the end of their lifespans. They run out of metabolic energy to molt, and their worn-and-torn shells contract bacterial infections that weaken them…”
Even the grey-headed albatross suffers senescence:
http://rspb.royalsocietypublishing.org/content/273/1594/1625
“…extremely long-lived individuals usually experience some degree of general physical deterioration, leading to reduced foraging and breeding performance…”
Plus the slow-aging species may enjoy anti-aging advantages apart from their sialic acid status.
For cold-blooded animals like fish, this piece proposes that a cold environment can increase longevity by signalling the DAF-16/FOXO gene, a gene apparently associated with longevity.
http://timesofindia.indiatimes.com/home/science/Revealed-Why-cold-blooded-animals-live-longer-in-cool-environments/articleshow/18527300.cms
Lobsters and ocean (arctic?) quahogs live in cold water, even sub-Arctic water.
http://sciencenordic.com/new-record-world%E2%80%99s-oldest-animal-507-years-old
Birds are warm-blooded. But this link proposes possible reasons for their longevity which may or may not relate to their Neu5Ac/Gc endo/exo status:
http://everythingbirdsonline.com/care-feeding/why-do-birds-live-so-long/
One thing we know: birds engage in very healthy frequent bursty “resistance” training–they flap their wings vigorously to fly! Regular brief resistance spurts through the day like Jack LaLanne who always scooped up the dumbbells for a few curls through the day. Most of us humans don’t do that kind of exercise all day long.
The above link also gives a list that shows that birds actually do age and physically decline.
Here’s a fun list of super-long-lived creatures. Won’t guarantee its accuracy!:
http://twistedsifter.com/2012/09/animals-that-lived-longer-than-the-oldest-known-human/
What’d be great to see: A chart of species that shows Hayflick Limits, telomere lengths at different ages, endo Neu5Gc/Neu5Ac status, balance of Gc and Ac in diet, the amounts and types of energy expenditures, warm- or cold-blooded, typical ambient temps, average BGs, on and on endlessly … 🙂
About what you say here: “I … think it’s related to population control. Some species are just very very “portable”, and if they overpopulate in one area they just spread to another … like fish and birds. Others are very local and populate very quickly … like mice and rabbits.”
Very interesting idea. I’d love to see some natural selection mechanisms spelled out for that.
And Heather I’ll definitely look more into what you say here:
“In plants, there is a ‘switch’ such that the same species can be bred to be perennial…”
Now *that’s* interesting. Do you know if an SNP governs the annual/perennial switch?
About meals, what works great for me, I always start with two fave high-fat high-fiber foods: an avocado and some fresh coconut, and make sure to hydrate to give the fiber some liquid to glom on to and expand. Then I nibble on a 1/2–3/4 oz piece of lightly cooked then frozen chicken liver. Just those three foods seriously blunt whatever appetite I started out with. I’m super grateful for that! Up to age 46, my desire to eat was out of control along with my BGs. –Bryan
wbryanh- Have you ever read the book “The Dorito Effect”? The author explains that when we have strong desires for certain foods, it means that our bodies *need* the nutrients in those foods. (Granted, many people’s taste buds are “hijacked” by processed food, so in many case nowadays the signals of what people really need are lost; hence, the random overeating, as you mentioned). But when people- and animals- are eating a whole foods diet, their bodies know intuitively what they need. They did experiments on babies back in the 60’s (I think?)- where they weren’t told what to eat; they were offered a smorgasbord of foods and chose, themselves, what they wanted. But they were only offered whole foods, and no sugar except fruit. Interestingly, they found that the babies were intuitively very good at eating a balanced diet of all the nutrients they needed. In addition, if they had particular problems, they *knew* what they needed to eat to rectify the problem- (for instance, 1 child had a vitamin D deficiency. That child willingly ate cod liver oil, wanted it in fact; but then the desire for cod liver oil went away when he was no longer deficient). I think it’s quite fascinating! Oh, I forgot to find a link to that study, but if you want one I’ll find it.
Morgana, The Dorito Effect, just ordered it, thank you!
Fascinating how the babies knew what to eat–including cod liver oil! –Bryan
Hello wbryanh and heathertwist!
Heathertwist: I agree with you that protein probably isn’t really an issue. The Jaminets (Perfect Health Diet) say that humans tend to eat the amount of protein that “feels right”: i.e., it’s difficult to overeat protein; we start to feel bad if we do. I find this is definitely true of myself. I know many of our current “diet gurus” would disagree with this- (some claim that we “eat too much protein”)- but I question this, and wonder if it really is true. Weston Price noted that healthy hunter gatherers and people on native diets tended to eat more fat and protein than Westerners of his time- (who were eating more processed food, mainly in the form of low quality carbohydrates). I also notice that protein helps to curb the appetite- (as does fat, but fat doesn’t work for me alone); it’s very satisfying, and enables one to go a long time without food. I guess protein can be a problem for people with blood sugar issues, or people who want to stay ketogenic. And I guess I’m not really sure that I advocate “fake” protein, i.e. processed stuff in the form of shakes that some athletes might be consuming. It’s possible that people who are eating extra protein in processed, fake foods might not be getting the signals to stop when they’ve had enough- (in the same way that people who overeat processed, crappy carbohydrates might not get the signals to stop eating). I don’t know for sure if that’s true; it’s a theory of mine though.
Morgana, @heathertwist —
Morgana, what you say here:
“I guess protein can be a problem for people with blood sugar issues, or people who want to stay ketogenic…”
Maybe not even that? Check out this link which you posted on December 17th:
http://www.ketotic.org/2012/08/if-you-eat-excess-protein-does-it-turn.html
and my Jan 5th response post to you which includes this:
“…your (Morgana’s) link which suggests GNG output–even in the presence of excess AAs–remains more or less constant…other GNG processes might be going on at the same time, which the bod dials down as AA-driven GNG ramps up, all to maintain the same net output. Those other GNG sources include glucose from glycerol, the backbone compound for triglycerides. And now, apparently, glucose from acetone…”
Morgana what this suggests in short: Our bods appear to make glucose from several sources at the same time. When excess protein forces our bods to GNG it, they simply dial down the other glucose sources. –Bryan
Morgana, @heathertwist — Morgana, yes, I agree, we see loads of reductionist thinking with serum lipids’n’lipos!
What you say here: “Finally, about inland people, Paleo diet and heart disease; although I do believe fish and sea food are important (and I do love to eat them), other explorers have found that inland people eating meat diets (or meat and dairy diets) can be just as healthy…”
The only truly inland people I can think of that WAP studied are the those (Romanisch?) Swiss of Loetschental Valley, those who lived deep in alpine valleys and ate lots of dairy and some rye-based foods.
http://gutenberg.net.au/ebooks02/0200251h.html#ch3
But even these mountain people, can we say they never ate fish? Switzerland has many lakes and rivers. Otherwise where did they get their w-3s? It’s possible they ate animal brain, the one rich source of terrestrial long-chain w-3.
Btw, on taurine, the meat they ate should have had plenty of it. –Bryan
Heather, I have to go out for now. One of my errands is to go pick up the two Huxtable taurine tomes from the library! I breezed through your long and very interesting post and will focus on it more tonight/tomorrow. –Bry
Heather, @morgana —
Wow Heather, what a work, thanks for all your thoughts!
I’ll have to address what all you said in a multiple posts.
What you say: “…Like how uric acid and oxalates and one form of lactic acid is dumped by the kidneys. The kidneys though, can only handle whatever is soluble in water. Bile can handle all the stuff that is solid. Bile is THE only method I can see for the body to GET RID of solids…”
Yes, that’s generally how I see it too. Only I add that non-fat (ie. polar) solid waste, eg proteinous waste, can exist free in chyme and feces, no bile needed. Our bods don’t need to bundle up that non-fat waste into bile micelles.
Btw, bile salts and lipoproteins perform the same basic task! They carry fats through aqueous environments.
Both entities present a highly polar “outer” face to the aqueous environment they travel in and a non-polar inner space for their lipid cargos. Lipos do this in order to be able to tote around lipids in our blood. If you pour olive oil (a pure fat) in water you see they don’t mix. Same thing with free lipids (ie fats) in blood (which is mostly water)–they don’t mix. Thus we can’t easily transport free lipids in blood. That’s where lipos come in. They have very polar phosphate heads that face the blood surface, making the lipo very soluble in blood. Meanwhile the inside chamber is non-polar so we can easily stuff the lipids, like cholesterol and triglycerides, into that spherical chamber.
Similar deal with bile. The bile salts present a polar surface making them more soluble in chyme, that thin slurry of digested food in our GIs that’s mostly water. Meanwhile the bile-salt particle auto-arrange around lipid micelles to take those tiny drops where they need to go. Scroll down in the Bile Wiki to see the yellow and green diagram of bile salts auto-arranging around the lipid micelle.
https://en.wikipedia.org/wiki/Chyme
https://en.wikipedia.org/wiki/Bile
Here you ask: “…the fats could be taken apart and de-oxidized?…”
Could be. I’m trying to find if our mitos beta-oxidize even rancid fatty acids. Not that we want to do a lot of that. But I expect we also, and maybe primarily, excrete rancid FAs.
You say: “So T …does lower triglycerides… and tend to cause weight loss, and reliably prevents CVD.”
About “reliably prevent CVD,” see Attia multi-parter I posted to Morgana and you. I’m not sure we can really say for sure *what* are all the proximate and ultimate drivers of CVD. Except to take what steps we can to minimize or eliminate our chronic inflammation, as measured by the C-Reactive Protein test and other such blood biomarkers. When we minimize this inflammation, we can keep our macrophages down to a dull roar. Macrophages are those little eager WBC hoovers that Peter Attia says are a critical agent to seed CVD.
http://www.marksdailyapple.com/the-straight-dope-on-cholesterol-10-things-you-need-to-know-part-1/
“The sine qua non of atherosclerosis is the presence of sterols (cholesterol or phytosterol) in arterial wall macrophages.”
Heather about what you say here:
“…So as to the fate of Ch … bacterial toxins, for one, have a notable tendency to glom onto Ch…”
This idea of cholesterol, or cholesterol-containing compounds like lipoproteins, that bind microbial toxins, that’s very interesting. I need to read more on this. Btw the authors of that Oxford Journals piece is the well-known researcher Uffe Ravnskov, a big debunker of the Lipid Hypothesis who’s published such books like “The Cholesterol Myths: Exposing the Fallacy that Cholesterol and Saturated Fat Cause Heart Disease”
https://en.wikipedia.org/wiki/Uffe_Ravnskov
http://qjmed.oxfordjournals.org/content/96/12/927.full
I have to stop here for now. More later. –Bryan
“Yes, that’s generally how I see it too. Only I add that non-fat (ie. polar) solid waste, eg proteinous waste, can exist free in chyme and feces, no bile needed. Our bods don’t need to bundle up that non-fat waste into bile micelles.”
The thing is, I can’t see any other portal from the blood to anything solid, except via the liver! The entire gut can *absorb* nutrients, but is there anywhere that it exits waste? I know enzymes get delivered, so maybe some waste goes into that. And some goes out via sweat (like excess iron: which then feeds pimple bacteria!). Water-soluble waste can go out via the kidneys. But other than bile, what does the liver excrete into the gut?
I really appreciated your links and explanations of “cholesterol”. Yes, it’s misnamed obviously! My “garbage bag” would be the lipos, which actually DO look like a sack! But the cholesterol itself (the “stuff inside the sack”) also has two states: new, and used? The “used” cholesterol gets oxidized or stores toxins from bacteria or wherever. The “new” cholesterol gets delivered to cells for many different uses. Sounds like.
“Could be. I’m trying to find if our mitos beta-oxidize even rancid fatty acids. Not that we want to do a lot of that. But I expect we also, and maybe primarily, excrete rancid FAs.”
This is again, what intrigues me. Some “anti-cholesterol” medications work by preventing re-absorption of bile, according to the producers. But what determines when bile is re-absorbed? It seems to me that one of the big points of bile is to get rid of used cholesterol. So perhaps it gets re-absorbed when the body is short of the bile ingredients … taurine and glycine … which in our diets at least, tend to be in short supply. And often the precursors to making them are ALSO in short supply. But by reusing bile, that puts the more toxic stuff back in circulation?
“You say: “So T …does lower triglycerides… and tend to cause weight loss, and reliably prevents CVD.””
Yes, I was referring to the studies on Taurine. High T diets feature less CVD, and adding T to the diet seems to help CVD.
“So if methionine above a certain level *is* truly toxic to us (I’m not convinced btw, but that’s another convo.)–”
Methionine is absolutely toxic, as in “it has killed people”. It is more toxic to animals than people though it seems. But it’s only toxic if it is given without the balancing amino acids. All the food sources I know of have a range of amino acids.
http://www.ncbi.nlm.nih.gov/pubmed/12067919
” I haven’t yet seen a mechanistic explanation for how exactly glycine is supposed to counteract the supposed pathogenic effects of methionine.”
http://jn.nutrition.org/content/136/6/1722S.full
“Methionine is an indispensable amino acid for humans, but there is evidence that if given in excess, it can interfere with the utilization of nitrogen from dispensable amino acids. In studies of nitrogen balance in subjects receiving low-protein diets, nitrogen balance was improved in subjects receiving low protein plus urea or low protein plus glycine, but not with diets containing low protein plus methionine or low protein plus both methionine and urea (23). Also, the urinary excretion of 5-L-oxoproline, a marker of glycine availability, was significantly lower when the diets contained low protein plus urea or low protein plus urea and methionine. There was a significant correlation between the excretion of 5-L-oxoproline and excretion of sulfate. The interpretation was that glycine was consumed to detoxify the excess methionine, with the result that the availability of glycine for other metabolic processes became limiting (23).”
Maybe it’s just based on experience? When I first read about it, it was about growing chickens. The chickens will limit their eating if there is too much methionine in the chicken feed, which (the article said) makes sense because otherwise the chickens would die from methionine overdose.
Hm though. If glycine is “used up” to detoxify excess methionine, then there is another reason there isn’t enough glycine!
“Why pick these particular compounds?”
Interestingly, some animals use glycine, others use taurine, to make bile. Humans use both! I’m guessing it has to do with being an omnivore. Taurine is mainly found in an animal-based diet, glycine is found in plants.
Heather, @morgana — Heather, back to your long post…
What you say here: “The Neanderthals and some of the Paleo people seem to be exceptions. But I don’t see a lot of evidence that they were very *healthy*. They were “old” at what we would consider a pretty young age (like 50). Lewis and Clark weren’t terribly impressed with the health of the Plains Indians either. And they themselves figured if they made it to 60 that meant they were in good health. And their diet would have been considered ideal by many Paleo fans!”
We need to remember these guys faced lots of other stressors, like infectious diseases and frequent traumas. We can’t really attribute “x” amount of their short and often brutal lives to diet. It could be they died young *despite* their healthier diets. Eg, we’ve found that our meat-chowing grain-free low-carb ancestors had better dentition than us:
http://news.discovery.com/human/evolution/ancestors-had-much-better-teeth-130219.htm
Another excellent series that found the same is the one Alan Alda narrated last decade:
http://www.pbs.org/wnet/humanspark/episodes/program-one-becoming-us
About what you say: “…there are thousands of years and many cultures that did and do fine on a shorelilne diet, which is why I sort of glommed onto that one. Japan and Korea are the best-documented…
I can’t argue against it. Again, we find giant ancient shell middens all over the world. Shellfish/shoreline is a reliable source of some of the most nutritious food on the planet. Why some of those shoreline groups seem to live a little longer than others–eg Okinawans longer than Japanese, Japanese longer than Koreans, we’d have to look at additional factors. Okinawans are exceptionally family oriented and slow paced. I was married to an ethnic Okinawan and experienced all this up close. All four of her grandparents who migrated to Hawaii at the turn of the last century to fish and work in the pineapple and sugarcane fields, they all lived well into their 90s. She had an auntie in Okinawan who still lived on her own at age 102 and still tended her garden. Her father fished off of the pre-industrial Kakaako section of Honolulu, deep diving for seafood, and sport a moray eel bite scar on his arm, though lived only into his 80s on the mainland. (RIP Shangy.) Okinawans regularly eat goya (bitter melon) which is exceptionally good hypoglycemic food. They grew up in a very pleasant and pristine environment, the “Hawaii” of Japan, that encouraged lots of outside life and was largely isolated from the ravages of continental life till the last century with WWII. Okinawans revere their elders. So many factors. It is remarkable though how so many of them lived so long even after the terrible traumas the Japanese soldiers visited on them in WWII. They must have suffered PTSD from this harrowing time. Were their exceptionally powerful family and societal ties the “therapy” they needed? I’d love to see some research on this.
So sad about Bastyr’s co-founder father and his son! I wonder, did the coroners do complete autopsies on them? Did William have any CVD? This may be a case of a father literally dying of a broken heart 😦 But that these vegans (was the son Noah vegan?) may have suffered nutrient deficiencies like meth/taur, I can’t argue against that either.
You say: “And most of the people becoming vegan as adults already have a good store of amino acids in their bodies. Some last a few years and then get ill. A lot of them cheat now and then. A lot of them take supplements. Denise has a blog entry about supplements vegans need (taurine is one of them!).
Yup, except Heather we can’t “store” AAs per se. AAs (except our oddball taurine and other non-proteinogenic AAs) have to be part of polypeptides and proteins which we need for all kinds of things, like to build muscle tissue, collagen, and hormones. BUT if we eat excess protein, we have to pretty much immediately deanimate its AAs (ie strip off the amine aka -NH3 groups), send the -NH3 off to excrete in urine, and convert the rest of the AA into either glucose or a fatty acid. So for exceptionally dietary AA deprived people like I imagine some vegans to be, they have to catabolize eg muscle tissue to cadge those AAs.
About the FADs gene that governs how much ALA we convert to the longer chain w-3s like EPA and DHA, it’d be interesting to see research on that. I’d especially like to see studies done on ancestrals that lived far from seafood. Did of them live far enough from seafood that they truly could not get enough of at least minimal EPA and DHA? Very hard to imagine it! Even our very earliest ancestors that split from the chimps, Heather as you pointed out, they lived near riverine enviros and so could gather shell-/finfish. Per the case study of the young Indiana woman cited in “The Queen of Fats” we can survive for years without any form of w-3, be it ALA, EPA, or DHA.
Finally Heather, thanks for the Kyotofoodie link!
*Whew* What did I forget here? 🙂 –Bryan
“We need to remember these guys faced lots of other stressors, like infectious diseases and frequent traumas. We can’t really attribute “x” amount of their short and often brutal lives to diet.”
I hear that a lot. However, the people living by the shore had the same lack of infectious diseases and trauma. Compare skeletons from Kennewick to one from Paleo Europe. We can determine diet now, from bone isotopes. So far as I’ve found examples, the fish-eaters are healthier than the meat eaters. Wheat eaters are the worst. But tuber and millet eaters are sometimes surprisingly healthy (like the Yuzus).
I should say that my Mom is an example of a healthy meat-eater. She’s 90, and she’s always been way into meat. Lots of steak! But she is also into liver, gizzards, headcheese. And cooked fish once or twice a week. So now, at 90, she is pretty much the same as she was at 70, and certainly doesn’t look her age. Has all her teeth. So yes, I know it’s possible and works for a lot of people.
BUT … she ended up with loads of deposited iron, and her joints are a mess. And that’s about the pattern I’ve seen in the cultures I’ve looked at. You CAN eat meat and be healthy. But it’s more common to find healthy centenarians among fish-eaters (all the “blue zone” countries are vegetable or fish-based). The people I know who eat a lot of meat locally happen to be farmers and their meat is mostly home-grown … organic and grass-fed … and so far all the ones I know that are over 40 have loads of joint problems. So it might be the neu5gc, might be something else. But I got tired of having sore joints! And I don’t want to end up looking like my Mom!
” Okinawans are exceptionally family oriented and slow paced. I was married to an ethnic Okinawan and experienced all this up close.”
Cool! Did you learn some good recipes? My thoughts are that when people are healthy, they tend to be happier and have better family lives. But like I said, I’ve been looking for good documented examples of healthy “mainly beef” eaters. I still haven’t found any. If it was truly a sustainable and doable life, there should be at least one example? Mongolia maybe comes close, though they basically drink a whole lot of milk which comes close to making up for lack of fish.
Anyway, instead of continuing hypothesizing, my experiment is to just swap my dietary habits and see what happens with loads of fish and shellfish. So far it’s made an amazing difference. Seems to be working on my family too.
“Per the case study of the young Indiana woman cited in “The Queen of Fats” we can survive for years without any form of w-3, be it ALA, EPA, or DHA.”
Oddly enough, there seems to be a gene that allows some people to process O3 from plant sources rather than animal sources. So there was some sort of adaptation there! There is some O3 in animals too, esp. in the brain and marrow. But in general, the more fish the mother eats, the smarter the kid is. So probably what you see in general is dumber people inland.
http://www.regaltribune.com/mothers-high-fish-intake-linked-to-babys-intelligence/25037/
Omega-3’s are produced by microbes though … so there is some in cow meat. Also some in fermented foods? And insects, I think? (our ancestors did eat insects).
Plus yeah … where in the world could our ancestors live where there are NO fish? If you didn’t live near a river, then you lived near a lake. Otherwise you died of thirst.
Re my long posts … yeah, I do rattle on. Feel free to just ignore whatever you want to ignore.
Heather and @Morgana —
Heather about long posts, no worries! I read them as several shorter posts.
About grains vs red meat vs seafood diets, I’d love to see Jared Diamond weigh in more on all this. He doesn’t delve deeply into nutrition. But he takes a great geo-anthropological view, which includes looking at macro migration patterns of early humans and that includes what they ate. Of his books, I’ve read Guns, Germs and Steel, and The Third Chimpanzee.
GRAINS: Here in this Discover Mag piece, Diamond gives us his unambiguous view on grains:
http://www.ditext.com/diamond/mistake.html
The Worst Mistake in the History of the Human Race
RED MEAT: Diamond talks about (in GG&S?), that out of the hundreds of species out of all the terrestrial megafauna ( I think > 50kg), we domesticated only five: cows, horses, sheep, goats and pigs. And that we appeared to do this around the same time as the Ag Rev, ie only 10–12k years ago. This suggests that, except for when our ancestors migrated to new lands, like to Australia and NA and spent a relatively brief ~1k year eagerly decimating the Pleistocene megafauna they found there like mammoths and giant sloths, that humankind has only a recent history to eat large amounts of red meat.
SEAFOOD: I don’t recall what Diamond says nutritionally about seafood, but gives startling examples of societies that refused it, possibly for superstitious reasons, even if it meant they starved to death. eg like a Norse settlement Greenland he cites here:
http://www.americanscientist.org/bookshelf/pub/jared-diamond
Heather you mention insects, and in fact we could make a case to include or at least ally them with seafood, since many species in both categories are closely related and offer similar nutritional profiles (e.g. lots of protein, w-3, minerals in shellfish and insects).:
https://en.wikipedia.org/wiki/Shellfish
“…Many varieties of shellfish (crustaceans in particular) are actually closely related to insects and arachnids, making up one of the main classes of the phylum Arthropoda. Cephalopods (squid, octopus, cuttlefish) and bivalves (clams, oysters) are molluscs, as are snails and slugs…”
Yes slugs apparently *are* edible! Learned that just now.
http://www.motherearthnews.com/real-food/edible-insects-zebz1305znsp.aspx
NA and most of Europe shunned insectovory until very recently. But most of the world still eats insects. This includes highly developed nations like Japan:
http://travel.usnews.com/features/Countries_That_Eat_Bugs/
Even the FAO now advocates insectovory:
Click to access i3253e.pdf
About Okinawan recipes, I’m sorry Heather, I don’t have any. We went our separate ways in 2005, before I started my lifestyle/nutrition/health journey. But her parents grew up in Hawaii where spam (!) became a huge part of the diet. They often served up east-west blends like spam musubi, mass-produced mochi, that kind of thing. Not super healthy.
https://en.wikipedia.org/wiki/Spam_musubi
Her parents moved to the mainland decades ago, in the ’60s I think, and that heavily influenced their menus too. It’s interesting all her grandparents–all immigrants from Okinawa to Hawaii–all lived well into their 90s, but her parents lived only into their early-mid 80s, and suffered various chronic diseases including cancer and COPD. It wasn’t due to lack of community. They had four children, most of whom lived nearby and everyone was close, good relations. We had frequent family get-togethers, and they had a large circle of friends. Her Mom never worked more than part-time. Her Dad retired early and appeared in great health and stayed very active even after he retired.
About what you say about the w-3 starved Indiana woman:
:”…there seems to be a gene that allows some people to process O3 from plant sources rather than animal sources…”
The remarkable thing is, Shawna Strobel didn’t get w-3 in *any* form. That’s what made her the first documented case of w-3 deficiency to ever be recorded in the scientific lit. During those ~ 18 months when she became symptomatic, her only food during that time was a formula she received intravenously. Not even the plant-sourced w-3, which is ALA (the 18C parent w-3). So even if she had the ability to synthesize longer chain w-3, she had no ALA from which to build them. The formula gave loads of w-6 (the 18C LA) but no w-3 of any form.
Heather what you say here: “Omega-3’s are produced by microbes though…”
Do you mean in our gut flora? My understanding is that w-3 is essential, meaning we have to consume it.
OK, back to youse guys … –Bryan
Heather, @morgana —
Here’s that w-3 deprivation case study in mentioned in the last post.
Her name is Shawna Renee Strobel:
https://books.google.com/books?id=TdQhZFWOU_MC&pg=PA80&lpg=PA80&dq=shawna+renee+strobel&source=bl&ots=bwXGG3MzlI&sig=EeeZ3SLHsl_VPAn9M067JtLBnMM&hl=en&sa=X&ved=0ahUKEwjl8urY5MXKAhVDoJQKHerpB_kQ6AEIIjAB#v=onepage&q=shawna%20renee%20strobel&f=false
Shawna went 18 months totally sans w-3 before she started to show symptoms. —Bryan
Heather I wrote in the last post: “…we could now see a return to a broader-based salt deficiency…” I meant to say “…**iodine** deficiency…” –Bry
Heathertwist- yes, wbryanh is right; it’s the LDL cholesterol that nourishes cells and heals damaged tissues, and the HDL that carries the cholesterol back to the liver. I know it seems like it *should* be the other way around, given that LDL is so maligned in our culture!- but the fact is that it is a very important molecule. One of the reasons some people think of HDL as being the “good” cholesterol is that it carries the cholesterol away from the heart, and back to the liver. Silly……in my opinion, they are overly concerned with heart disease only, at the expense of everything else. Low LDL cholesterol, for example, is a risk factor for cancer (as well as all-cause mortality). So, there are many reasons why it is very important to us. Basically, it’s an oversimplification to call one cholesterol “bad” and the other “good”.
In addition to that, it is completely normal for a healthy body to recycle cholesterol. In fact, there are many substances that the body recycles; nothing ever gets wasted! Although some cholesterol might leave the body through the bile, this is most likely either excess cholesterol that the body no longer needs, or damaged cholesterol. (My guess is that a healthy body eliminates damaged cholesterol. When that doesn’t happen, there’s probably an imbalance somewhere within). I think our bodies “know” how much cholesterol we need at any given time. This is why I don’t believe in messing with the process. Of course, it may happen sometime that our cholesterol is too high due to an imbalance of some sort, in which case it’s important to find the root of the problem and rectify the imbalance.
Morgana, @heathertwist, iirc, the LDL/HDL logic is that the lower the LDL, the healthier your bod must be because the liver sees less need to ship cholesterol from liver to tissue. Same idea for HDL. The healthier the bod–the more cholesterol the bod can remove from tissue to take back to the liver for storage/demolition. –Bryan
Morgana, what you say here: “I don’t think a substance in the body would be both deadly and helpful at the same time…”
This brings up an interesting Q. I think some of our vital compounds may be harmful too. Glucose the classic example. We have to maintain a certain blood concentration of glucose to feed our RBCs and maybe a few other cell types. But glucose is highly oxidative and wants to glycate other compounds like proteins, like those muscle proteins in the endothelial linings of our arteries. There are very few very old people, ancestrals or in the developed world, that don’t exhibit some level of CVD however minor. it seems we haven’t yet evolved to some perfect adaptation to our environment and maybe never will. –Bryan
wbryanh- here is a talk given by Malcolm Kendrick. In it, he explains what the key risk factors for heart disease are; as you can see, cholesterol- both HDL and LDL- are pretty low on the list. There are some surprises here- it’s very interesting. I watched it awhile ago, but if I remember correctly, the biggest risk factor for heart attack was blood with a high clotting factor. Many of the elements on the list are not even tested regularly at the doctor’s office:
Morgana, do you have that Kendrick link? –Bry
wbryanh- Did you not get the link I posted? It’s a talk on You Tube. Here, I’ll try again:
If you don’t get it let me know, and I’ll at least tell you where to find it.
And, I think you’ll enjoy “Big Fat Surprise”!
Morgana, how weird! The Kendrick link appears on the site, but not in my emails. OK, I’ll watch it now… –Bryan
Morgana just watched the Kendrick clip, it’s very good, thank you! Kendrick gives sources for what he discusses and I’ll follow up on those. If all pans out, this is yet another powerful indictment against serum cholesterol as a CHD predictor. Except maybe for *lower* CHD!
Interesting he says “diabetes” is a CHD predictor, but blood sugars per se are not. I’d like to know what diabetes elements he looks at besides high BGs. How he distinguishes between diabetes and mere high BGs. –Bryan
wbryanh- Okay yes, good point about the glucose. I guess there is an optimal level for certain elements in the body. However, on the other hand, I see glucose as being quite different from cholesterol:
1) we need to maintain a very tight range of glucose level in the blood, so the body has hormones and regulating factors that work to keep this range in check. Interestingly enough we have only one hormone for lowering glucose, but quite a few- (is it 5?) for raising glucose. Leading me to believe that in our history, raising glucose levels was more necessary or “important”- (i.e., we probably didn’t have access to huge amounts of dietary glucose). As far as I know, the body has no such mechanism for lowering cholesterol. Our liver makes what we need. Sure, the levels can get higher when there is a problem in the body; however, it’s not always clear that the problem is always a heart problem- (i.e. inflammation in that area of the body). So it’s silly to assume that the body is “making more cholesterol in order to kill us off”- (as some mainstream health officials seem to believe).
2) You say that as people age, they get more arteriosclerosis. Yes, this is true. However, arteriosclerosis isn’t the same as myocardial infarction. The plaques have to become unstable and “break off”. Gary Taubes writes about this in “Good Calories, Bad Calories”, not sure if you remember? They looked at populations of people where heart disease is practically unheard of, and the people did have plaque…..just not the dangerous kind that breaks off and chokes off the blood supply. Nina Teicholz writes about this in her book too. (It could be that Malcolm Kendrick mentions this in his talk that I gave the link to; I can’t remember).
Morgana, you may be right. I made the more general point that we shouldn’t assume any compound, which includes c’stol, to have only positive and no negative impacts on us. Seems like many things in the Game of Life pose a trade-off, and we evolve to find the best trade-off. Some argue that the sheer increased presence of c’stol in serum means it’s more available to become part of developing atheromas, that the lower the c’stol concentration the more slowly the atheromas develop or maybe don’t develop at all. You can say the same thing about serum triglycerides and calcium, the latter which helps form the hard plaque in the atheroma. But we don’t know. Even if true, of course ymmv.
https://en.wikipedia.org/wiki/Atherosclerosis
But what you say: “…we have only one [way] to lower glucose, but five ways to raise glucose…” I agree. And it makes sense. Humankind spent much of its existence trying to find enough to eat and usually didn’t find lots of non-fiber carbs, and these carbs were often scarce, even mostly absent.
As for what you say “…As far as I know, the body has no such mechanism for lowering cholesterol…” actually yes it does – the HDLs! HDLs scavenge the c’stol from tissue and take it back to the liver for storage and demolition.
I agree with what you say here: “it’s silly to assume that the body is “making more cholesterol in order to kill us off…” The bod’s making the amount of c’stol it makes for a reason–in our modern life cases, often due to chronic inflammation that accelerates tissue damage. And even if we were genetically disposed to high cholesterol–eg familial hypercholesterolemia (FH)–one of the studies that Kendrick discussed in that clip you posted shows no association between FH and CHD.
About atherosclerosis vs MI, yes, I agree the atheromas can take a very long time to develop into anything life-threatening and we die of other things first. Like prostate cancer, which often grows so slowly, something else kills the sufferer first. –Bryan
wbryanh- I don’t think of HDL as a mechanism to lower cholesterol; it is, after all, a type of cholesterol itself. Unlike with insulin- (a hormone we secrete in reaction to dietary glucose), claiming that the purpose of HDL is to “lower LDL” is looking at it with this biased view that LDL is inherently dangerous and “needs to be gotten rid of”. I am highly skeptical of this. (Remember, we’ve been thoroughly brainwashed on this issue). Each molecule has its own purpose in the internal choreography of our bodies, and HDL is only serving its role as part of the whole cholesterol cycle. It scavenges the LDL once it has served its purpose. As far as I know, we have no special hormones that kick in and “remove” cholesterol if it gets “high”, and that’s what I meant. (Although we can remove the waste products in our bile, as with other processes of the body; that’s something different). But cholesterol is so important to our bodies that we make it, and we make more if we don’t get enough from diet; and we recycle it as well. Comparing it to glucose, yes, we can make glucose too, but when we do- (outside of when we ingest it through diet)- we make only the amount we need. This is why, I say it again, I think it’s counter-intuitive to lower cholesterol artificially. That’s managing the symptom, but not finding out the root cause.
I think I said this before, but there are numerous reasons why someone’s cholesterol may be high (possibly temporarily so), which don’t all have to do with heart disease. So this fear of this substance in our bodies just seems silly. 75% of cases of myocardial infarction occurs in people with low to normal cholesterol.
Morgana, I agree with your main message. Only sorry dear, I need to make some correx in your last post!
You say “…HDL .. is …a type of cholesterol itself…”
HDL’s definitely not a cholesterol. It not even a lipid. It’s a lipoprotein. Which carries all kinds of lipids through the blood–eg cholesterol and trigylcerides. Unlike lipids which have little polarity, lipoprotein are very polar. Which is what allows it to travel through the blood.
“… claiming that the purpose of HDL is to “lower LDL” …” Whoever claims that would be silly. HDL and LDL are just two diff kinds of lipoproteins. However, HDL definitely clears systemic *cholesterol* into the liver. Which is what we were talking about, what you said in your post yesterday: “…the body has no such mechanism for lowering cholesterol.” HDL definitely does lower systemic cholesterol. And LDL raises systemic cholesterol. And that’s all perfectly fine.
What you say “…[HDL] scavenges the LDL once it has served its purpose…” No, again, HDL doesn’t scavenge LDL. Our our cells ingest and demolish has-been LDLs. Our cells have LDL receptors, which, when the cell detects the LDL is enough depleted of its lipid cargo, the cell ingests the remnant LDL and breaks it down.
Also, you say “Unlike with insulin- (a hormone we secrete in reaction to dietary glucose)…” Actually we secrete insulin in response to *all* glucose, from diet and also any that our bods make (aka endogenous glucose).
But Morgana, your main message, yes I do agree, we shouldn’t artificially lower cholesterol! And yes, the correlations between serum cholesterol and CVD are dubious at best. –Bryan
OK, correction, it is technically a lipoprotein, of course. I just tend to think of it all as “cholesterol” because that’s the colloquial; (most people call it “cholesterol”, even doctors, though that’s inaccurate). I never really thought HDL actually lowered systemic cholesterol, I just thought it was part of the whole cholesterol cycle- (but I guess you know more than I do, as you’ve studied this; I’ve read about it, but not studied it in detail). So what do you make of very high cholesterol but “good ratios”; in other words, both high LDL and HDL? Based on your description, it would seem that the ratio would be far more important than the actual number of LDL? I’m curious about this, as there seems to be a difference of opinion in the literature. In fact, the more I read about cholesterol and heart disease, the more I think that nobody really knows much of anything; at least, there certainly doesn’t seem to be much consensus on anything! Which makes it hard for me to take much seriously. I do like a lot of what Malcolm Kendrick says though, as he seems to be very logical- (at least, what he says makes sense to me).
Hi Morgana, @heathertwist. Morgana you ask “…what do you make of very high cholesterol but “good ratios” in other words, both high LDL and HDL?…” It’s a really good Q.
Many factors affect serum cholesterol levels. And these factors may *separately* affect LDL and HDL levels. For example, how our cells’ lipo receptors express (or not) affect how those cells bind and intake the lipos:
HDL receptors (like in hepatocytes, adrenals etc):
http://www.jlr.org/content/40/2/187.full
LDL cell receptors:
https://en.wikipedia.org/wiki/LDL_receptor
SO guys … Eg lipopolysaccharides may down-reg HDL receptors. Allowing an accumulation a “back-up” of HDL particles in serum:
http://www.ncbi.nlm.nih.gov/pubmed/12010990
For LDLs, Eg a thyroid T3 deficiency can down-reg LDL receptor function:
http://www.ncbi.nlm.nih.gov/pmc/articles/PMC3109527/
again leading to a “back-up” and aging of LDLs in serum. Thus high serum LDL. Which likely includes lots of small oxidized atherogenic LDL particles.
The longer the lipo hangs around in serum, the more oxidized it gets.
So how do you “oxidize” a lipo? Simple. Go to this link and scroll down to Fig 2, a diag of a generic lipo particle:
http://www.intechopen.com/books/lipoproteins-role-in-health-and-diseases/pathophysiology-of-lipoprotein-oxidation
Those blue and pink-headed particles inside the lipo are triglycerides and (esterified) cholesterol. But see those green-headed particles? Those are the phospholipids that form the “wall” of that lipo “lipid cargo” chamber. The green heads are the phosphate groups and the rest of the compound is the lipid tail. To me, that spherical cargo chamber always reminds of the deep-space spaceship in 2001 A Space Odyssey speeding noiselessly into the unknown!
Anyway, the point I make here, those lipid tails on those green-headed phospholipids, many, even most of these of these fatty acid tails are *unsaturated* and thus prone to oxidation. As the lipo courses through our blood, nearby oxygen and other oxidants attack those unsat tails.
Here’s another diag of a phospholipid (scroll down to first diag):
https://www.boundless.com/biology/textbooks/boundless-biology-textbook/biological-macromolecules-3/lipids-55/phospholipids-300-11433/
Again, the longer the lipo hangs around in serum, the more oxidized it gets. In general, we want to quickly clear the lipid cargo out of serum lipos and recycle those lipos.
Back to the many and varied factors that affect serum lipid and lipo levels, as you suggest, Morgana, there’s so very much we DON’T know. –Bry
OK, more for me to read up on! I’ll comment when I catch up!
I found out something else important though, about my garbage scows. If there aren’t enough scows, then bile can’t be manufactured. Which, I think, means that damaged cholesterol (full garbage bags) can’t be dumped. So maybe you end up with these garbage trucks just driving around and around. Or maybe they offload their cholesterol at the side of the road, like in a New York garbage strike. Except the side of the road is your artery.
But … some animals use taurine to make bile. Others use glycine. It seems humans USE BOTH.
Click to access 19375.full.pdf
So your famed bone broths might work as well for making bile as the taurine does? The body is in competition for both taurine and glycine. Taurine is also used in the heart, and in handling glucose. Glycine helps make collagen, and also handles methionine. If a diet is high in methionine without glycine, the methionine is somewhat toxic and is associated with a shorter lifespan (low methionine animals live longer). Both taurine and glycine can be produced in humans, but having more in the diet has a big effect, so maybe we don’t quite make enough.
Getting enough glycine isn’t really an issue if a “whole animal” is eaten … most animals have both. But with, say, meat, the glycine is in the offal, so eating JUST the meat isn’t a good idea.
For the vegans though … there is a fair bit of glycine in seaweed. Also in some greens. So the Yuzus wouldn’t need a whole lot of bile in any case, to digest fats, because there aren’t many fats. And they could use glycine instead of taurine to make bile. There wouldn’t be so much competition for the glycine to handle methionine either, because they don’t eat much methionine-rich foods.
Heather, @morgana — Heather, just to quickly say, a few things jump out at me. What you say:
“The body is in competition for both taurine and glycine. Taurine is also used in the heart, and in handling glucose. Glycine helps make collagen, and also handles methionine. If a diet is high in methionine without glycine, the methionine is somewhat toxic and is associated with a shorter lifespan (low methionine animals live longer).”
Yes Heather and methionine is THE only essential precursor our bods use to make taurine. It can cadge everything else endogenously.
So if methionine above a certain level *is* truly toxic to us (I’m not convinced btw, but that’s another convo.)–that it goes off to convert into reams of the dreaded homocysteine – what makes our bods decide to make homocysteine rather than taurine? Maybe the high fat diet, which calls on more bile and thus more taurine to make that bile salt, will force more methionine conversation to taurine rather than to homocysteine? That is, when you eat high fat but still relatively low protein, so you don’t get lots of methionine to begin with?
Btw, while loads of people including Chris Masterjohn, Mark Sisson, ever our own dear Neisy have been all over the glycine-methionine connection like Grok’s animal hide suit, I haven’t yet seen a mechanistic explanation for how exactly glycine is supposed to counteract the supposed pathogenic effects of methionine.
http://www.westonaprice.org/health-topics/abcs-of-nutrition/beyond-good-and-evil/ http://www.marksdailyapple.com/is-a-high-protein-diet-really-as-bad-for-you-as-smoking
http://rawfoodsos.com/2014/03/09/new-animal-protein-study/
BUT–interestingly–our main bile salts derive roughly in equal measures from glycine and taurine (= methionine!). So there you see a bile salt rationale for balancing glycine with methionine!
https://en.wikipedia.org/wiki/Bile_acid
It intrigues me that, out of all the many different lipid (ie non-polar) tails and many polar heads our bods could choose, they somehow select cholesterol-derived cholic acids for the tails and two amino acids (glycine, meth/taur) for the heads. Why pick these particular compounds? Why not go with straight-up fatty acid tails and phosphate heads just like we get in lipoproteins and the outer layer of our cells’ lipid bilayer? OK, maybe those fat micelles are comparatively larger and so require the bigger more rigid sterol-based cholic acid tails. Maybe that explains the cholic acid choice. But I still can’t guess why bile salts seem to need mainly those two particular AA residues, glycine and meth-taur. Why don’t bile salt seem to work using polar heads from any of the other 20 (21?) proteinogenic AAs? Or from any of the slew of other ~ 480 non-proteinogenic AAs? Why can’t it use phosphates for the heads? This enquiring mind etc. –Bryan
wbraynh, heathertwist- First off, thanks for that Weston Price link, that was really interesting! Wbryanh- I was under the impression that the glycine/methionine connection was simply one of correct balance of nutrients; i.e., that you need enough B vitamins to make the proper conversions? And muscle meat is relatively low in the needed vitamins- (according to them. I don’t study vitamins thoroughly enough, so I don’t know). But the argument is that traditionally we evolved to eat the whole animal, not just the muscle meat, so when we eat everything, we get the proper balance of nutrients. (Both skin and liver have been demonized, skin due to its “high fat” content, and liver I guess because it’s thought of as a “red meat”…..actually, not sure why liver is demonized). In any case, yeah…..
As per this talk about bile: am I to understand that people without a well functioning gall bladder, or even people who’ve had their gall bladders removed- are at risk for heart disease? (Or other diseases?)
Morgana, @heathertwist — Morgana, you’re welcome and all good Qs/comments. When I read Chris’ WAPF piece again:
“…methionine must be balanced with B vitamins, choline…” and didn’t spell them out more.
I see he didn’t really give us their context.
I’m not sure we need to worry about getting enough of these B vitamins. Except possibly for B9 (folate) and B12. Most of them the water soluble ones, like Bs 1–3, 5 and 6 (thiamine, riboflavin, niacin, pantothenic acid, pyroxidine) these are by far are the easiest vitamins for us to get. You find them in just about everything we eat. That is if you believe the RDIs! (I have serious doubts about RDIs–but that’s another convo.) When I spreadsheet-tracked my meals in 2007–2010, I never had trouble to meet these RDIs.
What you say: “…But the argument is that traditionally we evolved to eat the whole animal, not just the muscle meat, so when we eat everything, we get the proper balance of nutrients…”
I agree Morgana, and so glad to see, and be part of, the “nose to tail movement.” In fact, our forebears before they evolved their hunting tools, they likely fed more often on carcasses left over from kills. They used rocks to crack open bones and skulls to get the fat- and nutrient-rich marrow and brain tissue. Most muscle-meat is relatively nutrient-poor compared to organ meats and marrow–at least poor with respect to how much of them we apparently need. I see it as yet another element of Nature’s wonderful evolutionary genius. The highly carnivorous big felids like lions, tigers, etc. caught the animal and chowed mainly the muscle meat. Then we come along later to scavenge the more fat- and nutrient rich parts to nourish more our evolved neural system like our bigger keener brains. Could be too, with the SAD’s focus on quick-cook muscle meat, we don’t get enough glycine either, which along with proline are the main AAs in collagen, an important part in skin that helps give it its elasticity. If you have to eat muscle meat, better to stick to the collagen-rich skin and the “harder-working” areas of muscle meat like shanks, and shoulder/chuck, those cuts that come from the front of the beast which bear most of the weight and do most of the propulsion, which also have lots of collagen. Chuck and shanks are richer in minerals too like zinc.
About demonizing liver, maybe I haven’t heard this so much as you, but a lot of people seem to dislike its metallic earthy taste, at least in the non-poultry livers. Also some people mistakenly think even healthy livers must bristle with toxins because they are the “bod’s waste filter, right?” They don’t understand it’s the *bile* the liver issues and which first enters the GI that packages up fat-soluble waste, and that the water-soluble toxins don’t even need the bile but simply wend down through the GI and carry the toxins to the exit. I don’t know any ancestral cuisine that put chyme on the menu.
Morgana, about what you ask: “am I to understand that people without a well functioning gall bladder, or even people who’ve had their gall bladders removed- are at risk for heart disease?..”
Great Q! It’s yet another one of the CW assumptions that we can do just ducky without our gallbladders, likely based on the default SAD diet that makes the carb the primary calorie. But do we really do so well without them? Mind you we still produce bile–the gallbladder is just its overflow reservoir–but we may not be able to make enough bile “on the fly” to properly digest all the needed fat in a high-fat diet. Again, all our modern dietary the CW evolved from the high-carb SAD. The authorities don’t allow for anyone–like me– who eats a HF-moderate protein-LC diet. –Bryan
Morgana, @heathertwist, on lipids/lipos/CVD, you might enjoy this multi-parter from Dr. Peter Attia:
http://www.marksdailyapple.com/the-straight-dope-on-cholesterol-10-things-you-need-to-know-part-1
http://www.marksdailyapple.com/the-straight-dope-on-cholesterol-10-things-you-need-to-know-part-2
http://eatingacademy.com/nutrition/the-straight-dope-on-cholesterol-part-i
It’s a thick read in places. You may need to take time to key into it. But it’s very clarifying.
Please AMA on it!
Summary of summary per Attia: The baddies are sterol-laden macrophages (foam cells). Esp *phytosterols.* IE those sterols found only in plants! NOT the endlessly demonized cholesteroll!
Possible bad news for LCHF pegans doing loads of plant fat, e.g. “tree lard” like red palm oil!
Some highlights (some may be obvious I know…):
– Cholesterol is vital for life; no cholesterol = no life.
– The cholesterol we eat has little to do with the cholesterol we measure in our bloodstream.
we don’t actually absorb much, if any, exogenous cholesterol (i.e., cholesterol in food).
– ** A biggie guys → Think of your veins, arteries, and capillaries as the “waterways” or rivers of your body. Cholesterol is precious “cargo” that needs to move around, but it needs a “boat” to carry it. The proteins that traffic collections of lipids are called apoproteins. Once bound to lipids they are called apolipoproteins, and the protein wrapped “vehicle” that transports the lipids are called lipoproteins…lipids go nowhere in the human body unless they are a passenger inside a protein wrapped vehicle called a lipoprotein. ** see Attia’s excellent diag of a lipoprotein.
– The only way sterols end up in artery walls – the one place we don’t want them to be – is if the sterols are carried there by an apoB-containing lipoprotein particle.
– The sine qua non of atherosclerosis is the presence of sterols (cholesterol or phytosterol) in arterial wall macrophages. Sterols are delivered to the arterial wall by the penetration of the endothelium by an apoB-containing lipoprotein, which transport the sterols.”
– The cholesterol we eat has little to do with the cholesterol we measure in our bloodstream.
the body works very hard (and very “smart”) to ensure cellular cholesterol levels are within a pretty narrow band (the overall process is called cholesterol homeostasis).
– Plasma cholesterol levels (which is what clinicians measure with standard cholesterol tests) often have little to do with cellular cholesterol, especially artery cholesterol, which is what we really care about. For example, when cholesterol intake is decreased, the body will synthesize more cholesterol and/or absorb (i.e., recycle) more cholesterol from our gut. The way our body absorbs and regulates cholesterol is really amazing, so I want to spend a bit of time discussing it.
– Inflammation makes it worse, but the inciting event is **the LDL particle getting past the endothelium**.
– LDL particles (LDL-P), not LDL cholesterol content (LDL-C), is what drives sterols into artery walls. Don’t confuse the “boats” (lipos) and the “cargo.” (lipids)
– ** The greatest way to reduce your risk of atherosclerosis is to make sure your boats are carrying the right cargo – that way you’ll need fewer of them.
Morgana, Heather, I’m sure we have new info since Attia wrote this in 2012. But it’s some excellent stuff to build on. –Bry
Very interesting read, thanks wbryanh!
morgana, @heathertwist–
Morgana, you’re welcome! And I’m sorry I’ve delayed to answer. House stuff ties me up at this time. Now, just as things start to get interesting here! –Bryan
OK, so I’m thinking that cho is more like the the tiles on the outside of the space shuttle. They can be used as building materials too, so the image fails there. But like the space shuttle, you NEED the tiles and they cover our cells, protecting the layer below. Then when they get damaged, they get carted off and new tiles get carted in (by the lipos).
Taurine and glycine help get rid of the damaged cholesterol, methinks. The official take is:
“The taurine content is high in oyster meat 243 mg/100 g (Table 6) which is significantly higher than that of fish 40–85 mg/100 g (Divakaran, 2006). The ratio of taurine to cholesterol is an important index in foods and higher ratio is beneficial to the consumer (Choi et al., 2006). Taurine:cholesterol ratio is 2.3 in oyster (Table 6). Among taurine’s many natural functions in living systems, is its hypocholesterolemic effect (Rijssenbeek et al., 2006). Taurine acts by conjugating bile acids that are formed from cholesterol synthesised in the liver and excreting them through bile. To replenish the excreted bile acids more endogenous cholesterol is converted to bile acids which results in lowering of cholesterol in the body. Thus taurine exhibits a hypolipidemic effect by stimulating hepatic bile acid synthesis from endogenous stores of cholesterol (Ogawa, 1996).”
http://www.sciencedirect.com/science/article/pii/S168742851400020X
Which seriously doesn’t make sense. Why would you want to get rid of any ol’ cho? Seems like you’d want to get rid of only the damaged stuff.
————
Now, you get into how to get enough taurine. If you compare St. John’s vs. Guiyang, you see the St. John’s folks have rather low Tau output, while in Guiyang it is rather high.
http://www.jbiomedsci.com/content/17/S1/S6
The highest is in Japan, at about 2000 mg per day. This got me to thinking. How much meat would you need to get 2000 mg per day of Tau? Lamb is pretty high in Tau, at 110mg per 100g. So you would need 2000 g of lamb per day, or 4.4 lbs. With beef it would be more, something like 5.5 lbs per day. Somehow the 9 lbs a day that Lewis and Clark allotted seems more reasonable then.
Fish though, isn’t much better. Many of the fish are about the same as beef, around 80 mg/100mg. 5.5 lbs of fish a day is too much for most people!
So how would the Japanese (or the Guiyang) get so much per day?
The situation gets worse when your realize that cooking leaches taurine easily. Plus, if you got your Tau from lamb, the saturated fat would use up a lot of the Tau just to handle the fat. So the Japanese start with an advantage: they tend to eat their fish quite raw or barely cooked. And there isn’t much fat that needs bile for digestion.
The real answer though, might come from molluscs. Oysters sit at 243 mg/100 g. Octopus is even greater: 520 mg/100 g. And squid at 350 mg/100 g. And also … these are commonly eaten in dried form, as a snack. It’s pretty easy to eat a lot of dried squid! Esp. as a bar snack!
——————
Another answer might come from milk. The Tau content of milk varies greatly, depending on the animal. Goat milk can have 10 times more Tau than cow’s milk, and it depends on the breed of the goat.
http://www.sciencedirect.com/science/article/pii/S0921448898000959
Cheese tends to have more than Tau than milk, esp. cottage cheese. Pork and wild game has more than beef. Eggs are pretty high, as is turkey. And oatmeal, oddly!
http://suppversity.blogspot.com/2010/08/taurine-from-foods-can-i-be-taurine.html
This is interesting in that body builders have glommed onto oatmeal, cottage cheese (and whey in general), and turkey for a long time.
—————–
The point is: you can get a high Tau on fish, and it will probably be a low-fat diet. For some reason I can’t fathom, most fish-heavy diets are low in fat. Plus less Tau is used to digest fats in a fish-diet (fish can have fat, but it is easier to digest. Coconut oil is easy to digest too, it’s almost water soluble).
If you have a land-based diet though, it takes a LOT of meat or dairy products to get a decent amount of Tau. Which means a high fat diet. Maybe that is the magic of the “high fat diet” … loads of cheese and meat.
Oddly some sources list oatmeal as high in taurine, and others as having no taurine at all. But I have heard from reliable sources of people raising cats on oatmeal ONLY, which could only happen if the oats had taurine in them. If that is true it’s an amazing thing, esp. for vegans.
Heather, maybe c’stol is the material *within* the tiles of the Space Shuttle? Because it is firmly embedded inside the lipid bilayer of the cell membrane? In the sense to keep undesirable elements out (eg too much reentry heat.)
That may work well. C’stol, due to the rigidity of its four interlinked rings, serves to stiffen the cell membrane, for many reasons, generally summed up here:
http://www.cholesterol-and-health.com/Cholesterol-Cell-Membrane.html
“Without cholesterol, cell membranes would be too fluid, not firm enough, and too permeable to some molecules. In other words, it keeps the membrane from turning to mush.”
About what you say: “Taurine and glycine help get rid of the damaged cholesterol…” I’d like to know more about this. How do we “damage” c’stol? (One often thinks first of oxidation.) If we do damage c’stol, to what degree can we repair it? I ask this, because if we routinely make c’stol de novo, why would we not be able to repair it?
What you say here:
“Taurine acts by conjugating bile acids that are formed from cholesterol synthesised in the liver and excreting them through bile. To replenish the excreted bile acids more endogenous cholesterol is converted to bile acids which results in lowering of cholesterol in the body…”
I’ll point out we quite efficiently recycle those taurine- and glycine-headed bile salts via enterohepatic circulation, thus we suffer minimal loss of c’stol via bile salt action on lipids. Point is, even if we eat a high-fat diet, we may not excrete much c’stol-taurine.
https://en.wikipedia.org/wiki/Enterohepatic_circulation
What you say “The highest [Tau excretion] is in Japan, at about 2000 mg per day, perhaps this is due to such a high Tau intake (from the high-Tau seafood) coupled with such a low fat diet, that the Japanese vent off lots of extra unneeded Tau. Which suggests that Tau, like other AAs, we can’t retain but have to excrete.
Heather you did the math to find that the sheer amounts of excreted Tau seems to go way beyond what the cohorts would eat, and that’s very interesting. I’ll guess some of that Tau comes from de novo synthesis from excess methionine. That their/our bods convert methionine to taurine for excretion rather than to allow it to go off to form potentially harmful homocysteine. This idea gives weight to the idea we very easily convert cysteine + methionine to taurine. Btw, the Japanese traditionally were not big dairy consumers, though could be they were consuming more dairy by the time the researchers found “The highest is in Japan, at about 2000 mg per day.”
What you say here: “For some reason I can’t fathom, most fish-heavy diets are low in fat…”
I’ve wondered this why most fish seem so high on protein and low on fat. However, I’m not sure the fish eaters necessarily heavily favor the protein over the fat, at least those who eat traditionally/ancestrally. Bluefin tuna fat is highly prized in Japan. The shoreline Inuit prefer maktaaq above all else. Ancestrals eat the whole fish, including the fat-rich skin and heads. Yes, shellfish diets per force are low fat, but how much do they make up the total calories of the daily diet? Maybe the other calories come from carbs instead of fat, but still not from protein. Also, if they do eat lots of shellfish, and thus lots of extra protein, remember that at least a quarter, maybe lots more, of that excess protein goes off to make fat.
“Goat milk can have 10 times more Tau than cow’s milk, and it depends on the breed of the goat.” Fascinating! So often cheesemongers told me that customers who react to cow milk and cheese do just fine on goat milk/cheese. Maybe it‘s more than just the presence of the potentially inflammatory and even T1 diabetogenic casein called A1 beta casein? Maybe the whopping extra load of Tau in goat’s milk also gives a calming and salubrious effect?
http://www.motherjones.com/environment/2014/03/a1-milk-a2-milk-america
It seems what you say here is the crux of your post:
“If you have a land-based diet though, it takes a LOT of meat or dairy products to get a decent amount of Tau…”
My Q: How much is enough? Heavy excretion of Tau may mean just heavy excretion of excess Tau. That alone doesn’t necessarily confirm better Tau-driven health. I might worry if people excreted no Tau at all. But what about folks with low Tau excretion? Maybe they get enough Tau, only they just don’t have much left over hence the small overflow?
The Tau or from oatmeal, super interesting! I’d love to hear more about that.
Btw, minor point , but I use c’stol or Ch because “cho” can mean carbohydrate:
http://www.cpmc.org/learning/documents/cho.html
Finally, the tenor of this discussion reminds of a favorite book: The Tao of Pooh.
Or is it: The Tau of Poo? –Bryan
“I’ve wondered this why most fish seem so high on protein and low on fat. However, I’m not sure the fish eaters necessarily heavily favor the protein over the fat, at least those who eat traditionally/ancestrally.”
Right. Everyone loves fat. And the most popular edible fish in Japan are quite fatty. But they don’t use a lot of extra fat, and the fat in fish is rather soluble. In Okinawa though, they use pork fat also. Pork is also a high-tau food, plus you have all that glycine in the skin. Still, the Okinawan diet is characterized as “low fat”.
“’ll point out we quite efficiently recycle those taurine- and glycine-headed bile salts via enterohepatic circulation, thus we suffer minimal loss of c’stol via bile salt action on lipids. Point is, even if we eat a high-fat diet, we may not excrete much c’stol-taurine”
That’s exactly my point. We may be *recycling* the cholesterol. I think we should not be doing that! The damaged Ch needs to go away. It’s toxic, very toxic. Mercola talks about what happens when you eat it (I don’t usually quote Mercola, but this one is good):
“”There is an excellent research on animals where they fed animals plenty of cholesterol in their diet and they did just fine. But when they gave them even small amounts of tainted cholesterol, meaning oxidized cholesterol, within weeks it showed up in fatty streaks in their arteries,” Dr. Rowen says.
“We know why now. There are receptors in the endothelial cells that are the lining of your arteries. There are receptors there for oxidized cholesterol. It picks it up, and it goes into the endothelial cells. The problem is that oxidized cholesterol does not look native to your macrophages, your immune system. It actually looks like bacteria. The macrophages move in to try and clean up what it thinks is bacteria, which is nothing more than oxidized cholesterol, and it creates a whole bunch of inflammation inside your arterial wall. The real culprit is oxidized cholesterol.”
http://articles.mercola.com/sites/articles/archive/2012/05/05/dr-mercola-interviews-dr-robert-rowen-part-2-cholesterol.aspx
So where does “oxidized cholesterol” in the body come from? From cells! The cells get oxidized by free radicals, and the Ch gets shed. (You can eat oxidized Ch too, which is a bad thing).
So if you look at the structure of a cell membrane, the Ch is sitting there helping hold the membrane together:
http://study.com/academy/lesson/cell-membrane-functions-role-structure.html
http://www.cholesterol-and-health.com/Cholesterol-Cell-Membrane.html
“Cholesterol is an amphipathic molecule, meaning, like phospholipids, it contains a hydrophilic and a hydrophobic portion. Cholesterol’s hydroxyl (OH) group aligns with the phosphate heads of the phospholipids. The remaining portion of it tucks into the fatty acid portion of the membrane.
Because of the way cholesterol is shaped, part of the steroid ring (the four hydrocarbon rings in between the hydroxyl group and the hydrocarbon “tail”) is closely attracted to part of the fatty acid chain on the nearest phospholipid. This helps slightly immobilize the outer surface of the membrane and make it less soluble to very small water-soluble molecules that could otherwise pass through more easily.4
Without cholesterol, cell membranes would be too fluid, not firm enough, and too permeable to some molecules. In other words, it keeps the membrane from turning to mush.”
But the cho is also protecting the phospholipids:
Cholesterol protects the phospholipid bilayer from oxidative damage.
“We claim that (1) cholesterol protects bilayers from disruption caused by lipid oxidation by sequestering conical shaped oxidized lipid species such as 1-palmitoyl-2-azelaoyl-sn-glycero-3-phosphocholine (PZPC) away from phospholipid, because cholesterol and the oxidized lipid have complementary shapes and (2) mixtures of cholesterol and oxidized lipids can self-assemble into bilayers much like lysolipid–cholesterol mixtures. ”
http://www.ncbi.nlm.nih.gov/pubmed/24795978
———————–
“My Q: How much is enough? Heavy excretion of Tau may mean just heavy excretion of excess Tau. That alone doesn’t necessarily confirm better Tau-driven health. I might worry if people excreted no Tau at all. But what about folks with low Tau excretion? Maybe they get enough Tau, only they just don’t have much left over hence the small overflow?”
Excreting extra seems like it shouldn’t be a big deal, I agree. Except … that the level of Tau excretion seems to be a reliable predictor of longevity and health. No explanation for that, just that’s what happens. Could be a coincidence, except that adding Tau to the diet as a supplement is incredibly healing.
I agree that on a low-Tau diet, the Tau can get recycled. In fact I think that’s EXACTLY what happens, and likely damaged Ch gets back into the system as a result. It’s like water maybe … you CAN live off not much water, but in the long run, you’ll not do as well. Water helps keep the body flushed out. Damaged Ch kills your arteries. Damaged Ch needs to go away … far, far away … Tau helps flush out the damaged Ch …
How much is “enough”? It’s a really good question. Why do they test excretion? Probably it’s like water … when you drink water a lot of it is “used up” by sweat or rehydrating, so the only way to tell if there is “enough” is to see how often you pee. And the amount of Tau excreted reflects directly on longevity. Remember this chart (about one page down):
Click to access 7(14)161-166.pdf
Diets for Healthy Longevity Proven by Global Studies
-Lessons from Australian Aboriginals-
—————–
“Btw, minor point , but I use c’stol or Ch because “cho” can mean carbohydrate:”
Ch works. I’m allergic to apostrophes.
—————-
“Or is it: The Tau of Poo? –Bryan”
Running away screaming …
heathertwist, wbryanh- wow, lots of interesting stuff written by you two! I don’t have much to add, and I have kind of a stressful rest of the week ahead, so this is just to let you know that I’m still reading, even if I don’t comment much.
One thing: though fish is often relatively low in fat- (though I don’t know; I find things like salmon and saibling to be quite filling, so I think there is rather a lot of fat there; though I eat the skin, it’s the best part)- some cultures who eat fish eat quite a reasonable amount of fat in their diet. The Kitavans eat a high fat diet, mostly saturated fat from coconut. Most of the Mediterranean countries I’ve visited eat fat in the form of lots of olive oil drizzled all over everything, and sometimes cheese and meats. In northern countries where fish is consumed, they also tend to eat a lot of fat, often in the form of cheese, butter and other dairy products- (think Norway, Finland, Sweden, Denmark, etc.) Herring is often served in a very creamy sauce. So, I don’t think all fish eating groups eat low fat. Generally, Northerners seem to eat pretty high fat diets, and people living in the South might eat lower fat diets (but then again, they might not). But traditionally Southerners had access to more varied plant foods, so some of them did eat more carbs. In any case, I eat quite a lot of fish, but also quite a lot of fat, so hopefully there’s nothing wrong in that….
wbryanh- about you being in ketosis- it may feel like an “experiment” now, especially since most people in our current culture eat so many carbs! (And of course, there’s the “fat fear” too). But I still don’t think we really know what earlier humans, like Paleo man (or even hunter gatherers before our time) ate. Oh, I’m sure people all spread throughout the globe probably ate quite different diets, as they do now; but I’m not convinced that “nobody” ate mostly ketogenic. I think it’s highly plausible that groups of people ate high fat, ketogenic diets, though I have no way to “prove” this- (but then again, nobody can prove that it didn’t happen either). You may remember that Gary Taubes questioned if maybe ketosis wasn’t our natural state, and maybe glucose burning is a “backup” state? One reason I wonder about this is that the ketogenic diet seems to be so therapeutic for so many modern health problems, like diabetes, cancer, Alzheimers, epilepsy and other brain disorders; it makes one wonder if maybe a big issue is that we haven’t been in ketosis *enough*?! So who knows really…..I say, don’t let people tell you that ketosis is unhealthy- (because many people seem to want to believe this). If you feel healthy, I think that’s saying a whole lot! There are so many people our age (I’m about the same age as you) who are in terrible health. So, enjoy it…..
Hi Heather, @morgana —
Heather, sorry for the delay to answer. And thank you so much for the interesting points and ideas! I’m glad we delve ever more down into the lower-level biochem and mechanistic possibilities. As complex as all that is, because evolution has a many-million year leap on us 🙂
In general, the emerging consensus I see from researchers is that *chronic inflammation* ultimately drives a lot of pathology–maybe the bulk of chronic pathology–not just CVD. And that abundant oxidized products are often present in that case, and may also be drivers.
And, most important–the sources of chronic inflammation may well be *very many and varied.*
Heather, it’s certainly plausible to me that oxidized Ch is one such source. But if so it’s one of very many. I contend we’ve seen such a slew of novel inputs in our world since 1945–eg over 100k new chemicals that never existed before WWII–that we may never be able to fully resolve out what environmental factors drive which pathological effects. We truly need to take a (w)holistic approach, to *remove* from our systems AMAP, not *add* to them.
Two recent such people I’ve heard/read to weigh in on this:
Dr Peter Attia–the cofounder of Nusi with Gary Taubes–wrote a series of excellent and richly-detailed posts on cholesterol and how it relates to CVD. So far it’s a nine-parter, “part-i” through “part-ix” and starts here:
http://eatingacademy.com/nutrition/the-straight-dope-on-cholesterol-part-i
And I listened and read that Mercola interview with Dr Rowan you posted:
Click to access InterviewDrRowenCholesterol2.pdf
I’ll say right off, about Rowan, he may well be right about oxidized cholesterol being a contributing factor, but I have real troubles with him. To draw his conclusion–that oxidized oils drive our CVD–he takes an overly simplistic, crudely correlative, and thinly supported approach that lacks sufficient granularity. He also fails to completely flesh out some keys mechanisms, eg what he asserts here at 12:45: “…because heat is damaging the oils, which in turn is going to damage the cholesterol and lead to vascular disease problem…” How specifically does the oil damage the Ch?
I riff more on Rowan further down, but let’s go back to Attia for the moment:
Attia gets into the problem the Ch and CVD in earnest here in Part IV:
http://eatingacademy.com/nutrition/the-straight-dope-on-cholesterol-part-iv
“…[the biggest single predictor] of heart disease [are] the number of apoB *particles* in your plasma…90-95% of apoB particles are LDLs…” This is the measure of the actual number of LDL particles in our blood, which we need to get a special lipid tests called LDL-P to measure this actual lipo actual count. Not the default LDL-C tests we most of get which don’t even directly measure anything.
Attia puts it another way here:
“…The sine qua non of atherosclerosis is the presence of sterols in arterial wall macrophages. Sterols are delivered to the arterial wall by the penetration of the endothelium by an apoB-containing lipoprotein, which transport the sterols. In other words, unless an apoB-containing lipoprotein particle violates the border created by an endothelial cell and the layer it protects, the media layer, there is no way atherogenesis occurs…”
But Attia stresses we don’t fully understand what foundational factors drive atherosclerosis and the factors are hugely complex. We have a *proximate* cause–sterols in macrophages that permanently embed under the endothelium–but not the ultimate cause(s):
“Does having a low level of LDL-C matter? Not if LDL-P (or apoB) are high… But why? As with the previous topics in this series, this question is sufficiently complex to justify several textbooks – and it’s still not completely understood.
Btw, Heather, unlike Rowan, Attia seems not to distinguish between the offending sterols, be they “normal” or “tainted” Ch, “normal” or “tainted” phytosterols, eg beta-sitosterol, etc.
Back to Rowan:
At 4:00 he says “…The cholesterol that is in plaque is modified cholesterol. It’s oxidized cholesterol. There is an excellent research on animals where they fed animals plenty of cholesterol in their diet and they did just fine. But when they gave them even small amounts of tainted cholesterol, meaning oxidized cholesterol, within weeks it showed up in fatty streaks in their arteries…”
Does Rowan claim the Ch in *human* arterial plaque is modified Ch? Or does he say that based on just that animal research he refers to? I’d love to see it. What forms of the oxidized Ch do we get, eg alpha-exopycholesterol? We have to remember animals can respond much differently to cholesterol and other compounds than humans (think Anichkov’s Ch’ed up rabbits.)
Rowan continues:
“We know why now. There are receptors in the endothelial cells that are the lining of your arteries. There are receptors there for oxidized cholesterol. It picks it up, and it goes into the endothelial cells. The problem there is that oxidized cholesterol does not look native to your macrophages, your immune system. It actually looks like bacteria. The macrophages move in to try and clean up what it thinks is bacteria, which is nothing more than oxidized cholesterol, and it creates a whole bunch of inflammation inside your arterial wall. The real culprit is oxidized cholesterol…”
Again, I’ve love to get Rowan’s biochem-mechanistic level evidence that spells out this process. Who’s done the work to show that macrophages attack “non-native” cholesterol? Again, Attia doesn’t distinguish between the sterols and their healthy and oxidized states. Surely someone’s done a detailed analysis of atheroma contents? But I googled for this and found nothing that examines down to the balances of healthy vs corrupted levels of lipids, like sterols, tucked away in the atheroma’s foam cells.
Throughout the interview, Rowan blanket-condemns “oil,” only once briefly distinguishing between sat and unsat oils. He doesn’t make at all clear that sat oils like coconut and ghee (clarified butter) are much safer because it’s very hard to oxidize a fat whose carbon backbone is already fully fleshed out with Hs.
And then there’s this from Rowan, which sent up beet-red flags for me:
“…India has an absolute epidemic of vascular disease…They are as slender as you and me. Your viewers can see our body morphology. These people are actually skinnier. They’re working very hard in the fields, and yet they’re losing limbs in their 30s from vascular disease and diabetes. I’m scratching my head thinking that these people are vegetarian and they’re eating food that they grow, and yet they are losing their limbs from vascular disease and getting heart attacks in their 30s. What it all boils down to is that in India, they cook their food to oblivion in oil…”
What?! He makes it sound like the source of all of India’s vascular disease ills are because “they cook their food to oblivion?” Where do I start with this?
I immediately bridle when someone uses this kind of “n = not a whole lot” to justify sweeping statements like “[The cause of their skyrocketing rates of vascular diseases], what it all boils down to is that in India, they cook their food to oblivion in oil…”
To back this up, instead of stats from WHO or other research bodies, Rowan gives us this:
“At this charitable hospital [where I volunteered], there are a lot of poor people who are peasants. They are as slender as you and me…They’re working very hard in the fields, and yet they’re losing limbs in their 30s from vascular disease and diabetes…”
Well, YES–they’re poor! The world’s modern poor suffer from a raft of chronic and heavy insults to their systems–daily exposure to pesticides and herbicides, exhaust from farm and road vehicles, tainted low-quality food in general, oil or otherwise. If these peasants live in the north like around Delhi or in Bihar State, they suffer from some of the worst pollution on earth which wafts SE across northern Indian from Delhi. The poorer Indians often burn their garbage in their homes, often poorly ventilated. Maybe this was less of a problem a hundred years ago, when there was few highly synthetic disposables to burn. But nowadays we have all kinds of chemicals hidden in our modern garbage, the fumes of which they inhale when they burn it. Finally, because they are vegetarian, they get a lot of their calories from carbohydrates, like dahl, which will be very bad for them if they suffer metabolic compromises from the time they are born.
I’ll also point out Indians have cooked oilseeds for centuries. And they started to cook in groundnut oil (aka peanut oil) well before India’s current explosion of CVD:
Click to access indiaproduction.pdf
http://www.newworldencyclopedia.org/entry/Indian_cuisine
Heather, please I hope you’ll pardon my Rowan rant here. I know that in a near 50 min interview in which people say many interesting and provocative things, it’s easy for something like this to slip by the radar. Again, I’m not saying Rowan’s NOT right. Esp since we have this:
http://www.newworldencyclopedia.org/entry/Indian_cuisine
“…In recent decades, sunflower oil and soybean oil have gained popularity all over India. Hydrogenated vegetable oil, known as Vanaspati ghee, is also a popular cooking medium that replaces Desi ghee (clarified butter)…”
But to blame all of modern India’s vascular ills just on these oils based on the highly correlative and small sample he gives us is irresponsible in the extreme. When don’t even know where this hospital is and when he volunteered there.
Finally, what you say here Heather in response to my previous post:
Bryan: “I’ll point out we quite efficiently recycle those taurine- and glycine-headed bile salts via enterohepatic circulation, thus we suffer minimal loss of c’stol via bile salt action on lipids. Point is, even if we eat a high-fat diet, we may not excrete much c’stol-taurine”
Heather: “That’s exactly my point. We may be *recycling* the cholesterol. I think we should not be doing that!”
Heather maybe you strongly feel “we shouldn’t be doing that!” But …it’s what our bodies evolved to do.
If recycling Ch was potentially so harmful to us, might we have evolved to aggressively recycle it? And the Tau too? I believe Rowan asserts we need to take steps to minimize ingesting “damaged lipids.” Maybe so. But throughout humankind’s existence, we routinely survived on scavenged oxidized rancidified and rotting meat, and may even have routinely eaten it as part of ancestral cuisine, eg traditional meat fermentations with the Inuit and the Icelandic people:
https://en.wikipedia.org/wiki/Rancidification#Oxidative_rancidity
But yes, Heather, this may all support the idea to eat more Tau. The Inuit and the Icelandic people eat very high-Tau foodways. I’d like to see a study of the meat-fermenting ancestrals and how much Tau they eat.
It could be we evolved an efficient system to cull out the corrupted Ch (using Tau?) that minimized the inflammatory process and thus the macrophage and/or high ApoB/LDL response. And why shouldn’t our bods immediately chuck it out? Our bods can easily make all the cholesterol it needs from the readily available Cs, Hs and Os at hand everywhere.
And perhaps that system normally worked very well, even when our forebears ingested oxidized lipids, like those in rotting meat. So long as they didn’t suffer all the additional insults and impingements that our modern world gives us. We may well have chronically exceeded some chronic exposure toxin threshold.
I continue to find Tau very interesting, especially if it turns out we can’t always automatically make all we need via cysteine + methionine. Alas, the two Huxtable books are interesting in places–esp the transcripts of the free-form discussion the taurine summit researchers engage in–but they sadly lack any good summary comments on our oddball AA. These books are by avid taurine researchers for avid taurine researchers who love to dive deep into the weeds. –Bryan
wbryanh- (and heathertwist)- I agree that the Peter Attia series all about cholesterol is excellent and highly detailed- (I also like the fact that he admits what it is we don’t know yet; how many people do that?! It’s refreshing to get the truth). A also agree with you that it’s too reductionist to blame all problems (for instance, in India) on oils. Actually, I’ve seen it mentioned over and over again in documentaries, and through my reading, that India’s sugar intake has soared in recent years. I guess traditionally they always liked a certain amount of sweet foods, but with the addition of Western foods like soda, tea with sugar and pastry, etc., apparently their consumption is very high at the moment which is what most of their health problems have been linked to:
http://www.ncbi.nlm.nih.gov/pmc/articles/PMC4277009/
This problem apparently even includes poor people (I can get a link if you need it; I can only post 1 at a time).
Apropos oils: although I don’t think that polyunsaturated omega-6 oils are necessarily “good”, it is a bit unclear how bad cooking with more traditional oils really is. For instance, in the Mediterranean and other parts of Europe, people often cook with oils at very high temperatures. In parts of the Mediterranean (like Spain) they fry fish in olive oil- (no link because I’ve been there and seen it). In Germany, they cook with rapeseed oil because they believe it to be healthy. And these people don’t seem to be dying right and left, in fact, they seem all in all pretty healthy. So who knows…..some people say olive oil is okay, but only meant to be eaten cold. Well, I roast some vegetables occasionally in olive oil (especially the Mediterranean ones) because it tastes so good. My theory is that processed food- which is often cooked at incredibly high temperatures- is probably more worrisome than home cooking.
“For instance, in the Mediterranean and other parts of Europe, people often cook with oils at very high temperatures. In parts of the Mediterranean (like Spain) they fry fish in olive oil- (no link because I’ve been there and seen it). ”
The “high temp” thing is harder to quantify. Ch deteriorates at 100 C, which is, say, 210 F. But if you are doing sous vide eggs, say, you will see that an egg yolk is cooked at 130 F or so. Yet when you fry an egg … the pan might be at 300 F, and yet the egg you serve is barely cooked and with a runny yolk.If you cook the same egg to 300 F throughout the egg … it’ll be one really lousy egg. (for starters it won’t reach over 200 until all the water is gone).
Also oxidation depends on how much oxygen is available.
Anyway, in my experience the “oxidized oils” usually happen because they are kept in an oxygen-rich environment too long (like potato chips that go stale, or fish that gets freezer burn) or deep fry fats that are re-used for a long time. Oxidized fats and cholesterol taste rancid. I guess people get used to them, who eat fast food a lot, but my kids take one smell and go “yuck, that smells rancid!”.
So you CAN fry fish in olive oil and have a great fish, is what I’m saying. Olive oil is pretty stable, and the fish isn’t cooked very long usually. Canola and other oils … they do tend to go rancid unless they are hydrogenized, which then turns them into trans fats. But if you use a spoonful of fresh canola to stir-fry something, it likely won’t go bad between the time you pour it and the time the vegies are fried.
Heather, @morgana, yes, I agree here in the main.
Remember too that olive oil is mainly a mono fat, so it doesn’t oxidize nearly as easily as the polys. And like you say Heather, we often keep the actual food temps very low during frying. The only thing I fry in olive oil are eggs to make Spanish Eggs because *these are so awesomely YUMMM.* And I fry them for a minute or less, which barely warms the yolk. Everything else, I fry in coconut oil. And I don’t do much of that. –Bryan
Hi Morgana, @heathertwist. Will try to catch up with you guys. So I may be (relatively) brief in my next few posts:
In India, soaring sugar consumption was a huge problem even a decade ago:
Click to access NYT%20-%20diabetes%20-%20Modern%20Ways%20Open%20India’s%20Door%20to%20Diabetes%20%202006-09-13%20text.pdf
In part because of genetic predisposition:
“…because Indians have such a pronounced genetic vulnerability to the disease, they tend to contract it 10 years earlier than people in developed countries. It is because India is so youthful — half the population is under 25 — that the future of diabetes here is so chilling….”
Indians develop vascular diseases much sooner and more profoundly when faced with chronic calorie surplus. From all effects, which likely includes heated oxidized unsat oils. But I wouldn’t be surprised if their vastly increased sugar intake was a huge, even dominant factor. Morgana, like you link suggests. By the way, I like the sugar history in that link. Like this:
“…The word sugar is a derivative of “sarkara”, meaning gravel in Sanskrit. Sugar became known to the world when the army of Alexander the Great came to India in 327 BC. Interestingly, they were surprised to see another alternative to honey to sweeten food, and described it as a ‘reed that gives honey without bees’…”
Finally, you say: “… In Germany, they cook with rapeseed oil because they believe it to be healthy. And these people don’t seem to be dying right and left, in fact, they seem all in all pretty healthy…” Actually rapeseed oil– aka “canola” oil–*is* a poly oil. But again, we need to *try* to look at the totality of inputs, even though in our modern novel-chemical-filled world we have so many of them to consider 😦 For life and health expectancy, Germany ranks high like you’d expect for a developed nation. But far from the best, 26th in both categories: http://apps.who.int/gho/data/node.main.688 –Bryan
Good detailed stuff! I’ll get into it in the next couple of days.
I agree there are tons of reasons for “inflammation”. I’ve mentioned a couple of my favorites: iron and neu5gc. Leaky gut is right up there too, and lots of people think it has to do with sugar. But right now I’m focusing on fat digestion as per the Super Low Fat diet theory. What effects might a super low fat diet have? And the big thing that jumped out at me is Tau. Whatever the “flammatories” are, Tau is an effective anti-inflammatory, and also required for proper handling of glucose. I also think it’s central to heart disease (not just atherosclerosis, but arrythmia etc. too) because diseased hearts are short on Tau, and tend to get better if Tau is added to the diet.
So now I’ve found a couple of interesting things. One is that the reuse of cholesterol is one of the really important factors. In fact, it turns out to be the critical factor in “Pottenger’s cats”. The cooked cat food actually had the SAME Tau content as the frozen cat food, when cat food companies were trying to develop healthy canned food for cats. BUT … the canned food caused Tau deficiency. The original thought was “cooking destroys the Tau”, but no, it doesn’t.
Now, the Tau-deficient cats had the same amount of Tau in their diet, but it wasn’t excreted by their kidneys, so it looked like they were very low in Tau. But really, it was used in bile and not taken up again. The differences in the *protein* content apparently caused the bile acids to conjugate differently! And therefore instead of being reused they were processed by bacteria in the colon.
So this gets right back to the “raw foodist” theories! Or my cruise ship where I was eating mainly raw fish, for that matter.
And we don’t know, for humans, which proteins digest in which way, in terms of bile salts. Or what effect the type of fat has on the reuse of bile salts and levels of taurine excretion. Or how to get rid of damaged Ch if the bile salts are always reused. In cats and rats, soy protein and casein protein have very different effects on reabsorption of bile salts, which may be why casein has a bad rap in rat studies on heart disease.
But it might explain why Tau excretion corresponds with heart issues better than the theoretical amount of Tau in the diet. We can say for sure that “in this country, the Tau/Mg excretion rate is N on average” and we can look at the same measurement in individuals in another country. How this relates to their cuisine and diet … we then have to figure out! If it continues to relate to heart disease (which it does in rats and cats and apparently in people) then there is a whole new avenue for studying heart disease. Way better than measuring “cholesterol” in my book.
All this is also affected by which bacteria are in the colon! Which sure reflects the results of some of the newer studies. It’s in an older book though. Pretty long read but super interesting.
https://books.google.com/books?id=SkfuBwAAQBAJ&pg=PA46&lpg=PA46&dq=effects+of+konjac+on+bile+salts&source=bl&ots=wkJT4vZ86b&sig=S0qbXL7BvN6Uk6xF-ocZwK2m23Y&hl=en&sa=X&ved=0ahUKEwiLt4etsdDKAhVH5GMKHXWzD9QQ6AEIQjAG#v=onepage&q=effects%20of%20konjac%20on%20bile%20salts&f=false
Taurine: Nutritional Value and Mechanisms of Action
edited by John B. Lombardini, Stephen W. Schaffer, Junichi Azuma
(Is this the one you got from the library?)
Hi Heather, @morgana —
Heather you say “…Leaky gut is right up there too, and lots of people think it has to do with sugar…”
I’ve often heard gluten may be a major driver of leaky gut. Mark Sisson made some interesting comments on it in a 2014 post:
http://www.marksdailyapple.com/leaky-gut/
About this “…What effects might a super low fat diet have?…” Petro at Hyperlipid offers and intriguing–and *only*–substrate-level mechanism to explain VLF’s putative positive effects:
http://high-fat-nutrition.blogspot.com/2015/10/protons-and-ultra-low-fat-once-more.html
In fact Petro wrote it in response to Neisy’s 6 Oct post we’ve all been endlessly commenting on here.
Your ideas on the recycled Ch, very interesting. When you say:
“…The differences in the *protein* content apparently caused the bile acids to conjugate differently! And therefore instead of being reused they were processed by bacteria in the colon…”
do you suggest the extra–or maybe diff–protein somehow compels the cats’ bods’ to ferment the bile acids instead of recycling them?
About this Heather:
“…And we don’t know, for humans, which proteins digest in which way…”
I haven’t heard that we digest diff proteins differently. Our proteases digest these proteins in the duodenum. While we have over 100k proteins in our bods, all proteins are made of some mix of the same 22 AAs. When we eat and digest them, we put them all through the same enterogastric denaturation process to unfold them from their quat, tert, and secondary configs so as to let the proteases have at all those yummy peptide bonds. Plus, enterohepatic circulation initiates in the ileum, “downstream” from the duodenum. So I wouldn’t immediately expect the protein mix to make an effect on bile acid recycling. I know that doesn’t accord with what you say here:
“In cats and rats, soy protein and casein protein have very different effects on reabsorption of bile salts, which may be why casein has a bad rap in rat studies on heart disease…”
but I don’t know how these animals’ small intestines are configured. Where you got this Heather, does that source suggest mechanistically how soy and casein proteins exert diff effects on bile salt reuptake?
About this: “…Way better than measuring “cholesterol” in my book…” I totally agree. We make most of our Ch for a whole raft of reasons. We have no way I know of the resolve out all the diff drivers and their relative effects.
Taurine: Nutritional Value and Mechanisms of Action – just ordered the book Heather, thank you! — Bryan
“I’ve often heard gluten may be a major driver of leaky gut. Mark Sisson made some interesting comments on it in a 2014 post:”
Yes! It’s not even a theory at this point: the mechanism is pretty well studied. With gluten the only question is HOW leaky it gets … in celiacs the openings stay open a lot longer than non-celiacs. He mentions some good “other causes” though. I kind of wonder if the other causes are so active in non-gluten eaters. The non-wheat-eating countries seem to have way way less gut issues, even when there is a lot of stress (like say, wars and famine!).
“but I don’t know how these animals’ small intestines are configured. Where you got this Heather, does that source suggest mechanistically how soy and casein proteins exert diff effects on bile salt reuptake?”
That’s EXACTLY what they found in the cat study. The bile conjugates differently depending on the protein structure in that particular meal. With cooked meat, this meant that the bile wasn’t absorbed in the upper intestine, and went to the lower intestine, where it got eaten by bacteria. With raw meat, the bile got re-absorbed. I don’t know what this does to the PROTEIN digestion, but it was a huge deal for taurine usage in cats, and therefore the cooked food ruined the cat’s health. Casein and soy have similar reabsorption differences. One style food: lots of urinary taurine. Another style food … same taurine content … no urinary taurine output, and sick cats.
Does this happen in humans? I have no idea. But since there is this HUGE gap in taurine urinary excretion between countries, it’s a fair guess. Like I wrote earlier, there actually is a fair bit of taurine in other meat sources compared to fish. The only REALLY big sources of taurine are shellfish and, say, tongue. The big difference in diet between the Japanese and say, Norwegians, is that the Japanese often eat their fish raw. And the Japanese tend to eat a lot of squid, but I’m not sure ALL Japanese eat that much squid.
And it may explain the health differences in the folks that actually don’t eat much taurine at all, like the VLF dieters. If the existing taurine can be recycled correctly … if there isn’t any protein that conjugates the bile incorrectly … then there may be enough that the heart and glucose systems can work well.
————
Mark’s ideas seem to be basically about carb levels, and ketosis vs. carbosis. It could be, but like I said before, I think the carbs are a red herring (so to speak!). Totally balancing carbs vs. fats is next to impossible inside a real body, because your body is taking those carbs and making fats out of them as needed. And such careful dieting hasn’t been necessary for most of history, to avoid heart disease or diabetes. People just did not GET either disease much. Even though they ate a large variety of fats/carbs/proteins. There has to be something way simpler and way more basic. Answer the question “Why are Japanese thin?” and you probably answer the question “Why did Americans get fat suddenly?”.
So there is this:
“The effect of taurine on obese-induced diabetic models
The Otsuka Long-Evans Tokushima Fatty (OLETF) rat is a model of non-insulin dependent diabetes, which exhibits hyperglycemia and insulin resistance and has accumulated abdominal fat as compared to the normal rats. It has been demonstrated that taurine supplementation improved hyperglycemia and insulin resistance in OLETF rats (Harada et al. 2004; Nakaya et al. 2000). Taurine also suppressed the increase in serum triglyceride and cholesterol, but not body weight and abdominal fat mass. ”
http://www.ncbi.nlm.nih.gov/pmc/articles/PMC3325402/
—————–
No balancing carbs and fats at all!
Heather, the stuff on on the interactions of proteins (or AGE pdts or ?) with bile salts in the cats’ GIs – that’s all in that Lombardini book on taurine I just ordered right? –Bryan
The extract I read didn’t go into the chemical reasons, mostly just that “this happened”:
Rats and rabbits fed diets containing casein excrete less bile salts in their feces, absorb greater amounts of dietary cholesterol and have higher plasma cholesterol than animals fed soy protein diets. The mechanism responsible for these effects appears to be multifaceted, but a major factor appears to be enhanced intestinal binding of bile salts and increased fecal bile salt loss in animals fed soy compared to casein diets. A peptide formed by the in vitro digestion of soy protein with peptidases has been isolated and found to bind bile salts. When this peptide is fed to rats it causes an even greater lowering of plasma cholesterol and greater fecal excretion of acidic and neutral steroids than diets with isonitrogenous amounts of soy protein.
…
“Water-soluble fibers such as pectin, guar-gum and konjac mannan are viscous polysaccarides that do not bind bile salts but act by entrapping bile salts in the intestine and increasing the total amount of bile salt present in the aqueous intestinal contents as compared to fiber-free diets or diets containing water-insoluble fibers. Rats fed diets containing water-soluable fibers have increased hepatic bile salt secretion, increased fecal bile salt excretion, increased activity of cholesterol 7 a-hydroxylase and decreased hepatic taurine concentration.
… Anyway, you can look at the link I sent, and see the same thing. Here it is again for convenience …
https://books.google.com/books?id=SkfuBwAAQBAJ&pg=PA46&lpg=PA46&dq=effects+of+konjac+on+bile+salts&source=bl&ots=wkJT4vZ86b&sig=S0qbXL7BvN6Uk6xF-ocZwK2m23Y&hl=en&sa=X&ved=0ahUKEwiLt4etsdDKAhVH5GMKHXWzD9QQ6AEIQjAG#v=onepage&q=effects%20of%20konjac%20on%20bile%20salts&f=false
Thank you Heather! It’s interesting to see the diffs between caseins and soy prots–at least their downstream metabolites–in binding tau and generally affecting bile salt re-uptake.
I wonder if they used fermented or unfermented soy? And that that’d affect reuptake? This may matter, according to a WAPF viewpoint which suggests that, at least for tradition-following Japanese, they don’t eat a lot of soy and most of that is fermented:
http://www.westonaprice.org/health-topics/inside-japan-surprising-facts-about-japanese-foodways/
“…it would be a mistake to call soy a “staple” in the Japanese diet, in the way that fish and rice are staples. Dietary surveys indicate that the Japanese consume an average of about 1/4 cup of soy products per day, including the ubiquitous soy sauce. Other soy foods include tofu, a precipitated product, and fermented soy foods such as miso, tempeh and natto. Until recently, these foods were produced at home or by artisans.
The Google preview lacks pages, so will wait for the book before continuing this convo. –Bryan
Heather, a diff between cats, rats and people: We learned to cook our food as long as 1.8 million years ago, according to Richard Wrangham in Catching Fire:
If it truly comes down to raw vs cooked, that might have allowed us enough time to better adapt to conserve tau/bile salts in cooked meat.
I wish these researchers would test the effects of innovations since WWII. Not since Homo Erectus!
http://www.slate.com/articles/health_and_science/human_evolution/2012/10/who_invented_fire_when_did_people_start_cooking_.html
–Bryan
Sorry H, meant to say “…allowed us enough time to better adapt to conserve tau/bile salts *when we eat* cooked meat…”
Heather, @morgana, Heather maybe I should have answered all points in one post, post-for-post like I normally do. Anyway…
I had to laugh at this from you:”The non-wheat-eating countries..” Which ones are left?! I’ll move there! But seriously Heather, I know what you mean 🙂
About what you say on Mark Sisson and macro bals: “Mark’s ideas seem to be basically about carb levels, and ketosis vs. carbosis. It could be, but like I said before, I think the carbs are a red herring (so to speak!). Totally balancing carbs vs. fats is next to impossible inside a real body, because your body is taking those carbs and making fats out of them as needed. And such careful dieting hasn’t been necessary for most of history, to avoid heart disease or diabetes…”
It’s true Sisson often casts things in terms of those macro balances. He does a good job to describe the inherent health advantages of the HFLC foodway and ketosis. Like, ketosis keeps you off the insulin/BG rollercoaster, and fat gives you more than twice the energy for only a third of the Os, so you have much less risk of rogue Os to attack and oxidize fragile mitochondrial membrane like cristae during Krebs Cycling.
Still, a big part of what Sisson does is promote an ancestral ketotic (“carbotic?”) foodway that’s both therapeutic AND appears to be just fine for the long term–among the oodles of other facets of ancestral life he discusses. But I agree your point that macro bals shouldn’t matter. If you do regular physical work, eat a near subsistence diet of real and whole foods, have good community, live and work in healthy environments, get good sleep and sun, and you should be able to swing from VLF to VLC and be just fine. I agree with you that macro balances shouldn’t matter for people who eat real foods–and don’t suffer metabolisms at some stage of brokenness. Alas, hundreds of millions of people in the world suffer that now. It may already be the case for over half of North America. In the past ten years, I’ve checked the BGs of over a hundred people. The normal range **at all times**–fasting, during meal, post-meal–is 75–95 mg/dL (4.2–5.2 mmol/L). Two thirds of them got BGs above that range, 100-200+ Under ten percent of those people checked in at 83 or below. And these were mostly younger people, 18 to 40.
There seems something inherently fragile about glucose metabolism. I’m not surprised we don’t hear much about disorders that stem from a low-carb diet that a high-carb diet magically cures. But I find that diff interesting. Compared to fat metab, glucose metab seems more involved and easier to derail and lead to chronic disease, in this case diabetes.
But Heather what you ask: “There has to be something way simpler and way more basic…”
My concern is that there may NOT be a simple answer. So very much has changed in our world since WWII. We are dealing with many thousands of novel inputs. What I said to Anna in a 4 Dec post:
“Since WWII, chem companies have invented over 100k new chemicals and flooded our environment with them, almost all of which still undetermined long-term biological effects on us. Their cumulative presence may now be persistently overwhelming our toxin filters. So many of the thousands of humble quotidien products we use are mute monuments to extraordinarily complex engineering, containing up to thousands of compounds, again many of them novel, existing only since 1945. We encounter them everywhere, in our homes, like in carpet and drywall, in our cars, in our kitchenware (plastic, teflon, aluminum), in our workplaces, and yes, in the formulations and coatings of our supps. Once I appreciated this fact, I went into full mitigation mode, to reduce as many potential toxins in my life as possible.”
BUT, Heather, all that said, I’d still love to see some good well-designed clinical studies of the effects of ramping up dietary taurine on people! –Bryan
“There seems something inherently fragile about glucose metabolism. I’m not surprised we don’t hear much about disorders that stem from a low-carb diet that a high-carb diet magically cures.”
Is it so very fragile? I mean diabetes was quite rare for a very long time and over a large geography and a large variety of diets. If our blood glucose was so fragile I’d expect it to pop up throughout history whenever oh, there was a war or everyone had nothing to eat but bread or white rice. I’d expect people going diabetic in refugee camps when they eat nothing but sorghum and Tang for years.
I don’t think there is any doubt that low-carb helps a lot of people, and THAT has been studied for years now. It’s not as interesting to me as an answer though, because it doesn’t explain why the “normal” eating habits prior to the 1970’s worked fairly well.
“My concern is that there may NOT be a simple answer. So very much has changed in our world since WWII. We are dealing with many thousands of novel inputs.”
And the huge amount of changes makes it hard to pinpoint what is really going on! The Japanese and Chinese in cities though, have the same novel inputs, and probably more pollution. The ones that get diabetes though, are the ones that eat a “Western diet”. And they tend to get better if they switch back to their traditional diet. Further, Westerners who go on a traditional Japanese diet get better too (like me on my cruise: but there are plenty of others who write the same thing).
To me that points pretty clearly to “diet”, since one person going back and forth between Asian and Western diets isn’t changing their exercise or family or stress levels or pollution levels. Pinpointing WHAT in the diet is harder.
I’d love to see better taurine studies too. They are coming I think. Meanwhile I can experiment on me! And my family. Seems to be working in those cases.
As for conserving bile salts … sure, we are adapted to cooking. The cat studies do show that food drastically effects bile re-absorption, which is the point. I’m not clear even how much we should be re-absorbing vs. what should be flushed out of the system. Or how the body knows the difference between dirty-Ch and clean-Ch. But it may be something super-simple that is totally un-anticipated (like cooked vs. raw for cats). My personal experience might make me think that a diet that contains raw leafy greens plus raw fish does a kind of magic for me, but I’m not sure why it would have the effect it does.
Heather, @morgana, good morn and aft to you —
Heather what you ask here: “Is [glucose metab] so very fragile? I mean diabetes was quite rare for a very long time and over a large geography and a large variety of diets…”
It’s a fair guess we had fewer cases of diabetes earlier on in recorded history, though we IDed the symptoms as early as 3500yo:
http://www.everydayhealth.com/diabetes/understanding/diabetes-mellitus-through-time.aspx
Again I expect T1D and T2D rates in those early days to be more like you sugg–quite rare. But we have no way to compare the rates for grain vs non-grain eaters going back earlier into recorded history. Could be, even way back then, lots of grain-eaters people developed metab syndrome and other complications early on in their lives. But other things killed them first.
My main point is that, with the onslaught of novel impingements on us esp from WWII, they seem to preferentially disturb glucose metab over fat metab. Intuitively that makes sense. We need more concomitant processes to manage glucose metab versus fat metab. Eg, we need insulin to mediate glucose ingress–but not fat ingress–into our cells to send the nutrients to our mitos for Krebs Cycle. Excess BG we have to convert to fat first (mainly the 16C sat fat palmitic acid) before we store it. Fats are already fats, already set to store in our adipose tissue.
Also, fat metab is our default metab state. We store only 2000 kcals of glucose on our bods but unlimited fat. Whenever we enter a fasting state–like when we sleep–we go into fat-burning mode.
What you say here “…it doesn’t explain why the ‘normal’ eating habits prior to the 1970’s worked fairly well…”
Again Heather we don’t really know. I’m not sure what you mean by “normal.” But if it’s the SAD or proto-SAD that NAers ate before the 70s, Weston Price did find major diffs. During his travels and observations of the health of ancestrals and modernized peoples in the 30s, he consistently observed that the ancestrals, most of whom ate little or no glutenous grains, were consistently healthier found that the modernized SAD-like diet folks.
What you say here:
“…And the huge amount of changes makes it hard to pinpoint what is really going on! The Japanese and Chinese in cities though, have the same novel inputs, and probably more pollution. The ones that get diabetes though, are the ones that eat a “Western diet.” And they tend to get better if they switch back to their traditional diet…”
Heather you may be right, though I haven’t see any data on that, plus it is very hard to get reliable data out of China. And even if we could rely in their figs, they’d just about perforce lack vital granularity. Eg how do you separate those country folks who really do eat a truly traditional diet growing org/pesicide-free veg and traditionally milled rice vs the city folks that eat the ersatz “traditional diet” of chemical-laden veg and fruit and industrially milled rice into which the processing intro’ed a lot of hormone-disrupting chems like BPA? It’s much too burdensome to try to resolve all that out in surveys, even for the Japanese who keep such records as you rightly pointed out.
What you say here:
“…To me that points pretty clearly to “diet”, since one person going back and forth between Asian and Western diets isn’t changing their exercise or family or stress levels or pollution levels…”
I suspect diet matters a lot for most people. It sure did for me. I believe it’s the single biggest change I made, and which lead to most if not nearly all of my improvements. But a big part of that was to go to persistent LCHF, some might even call it VLC-VHF (80% fat, 15% prot, 5% carb). BUT, once in metabolic syndrome, many people need to stick to a similar macro balance to manage their BGs, body weight, and other measures. Again, it’s the glucose metab that got corrupted, not the fat metab. At the cell-nutriet-ingress and mito level, I’ve never heard of this problem to exist the other way round–people with corrupted fat metab but healthy glucose metab. –Bryan
“Could be, even way back then, lots of grain-eaters people developed metab syndrome and other complications early on in their lives. But other things killed them first.”
We have pretty good numbers on traditional Japanese, Chinese, and folks in the Middle East … there were places where people tended to live a long healthy life. T2D was just rare. It WAS described as an illness, and T1. And there were fat people (mostly the very wealthy). Just not very many, usually. There were more fat people in some places, like Egypt and Rome.
“Eg how do you separate those country folks who really do eat a truly traditional diet growing org/pesicide-free veg and traditionally milled rice vs the city folks that eat the ersatz “traditional diet” of chemical-laden veg and fruit and industrially milled rice into which the processing intro’ed a lot of hormone-disrupting chems like BPA?”
That was a bit point in the China Study. The country people really do live in the country and grow their own food. And the Yuzus (at least now) still grow their own food. You can see how they live and talk to people who have lived there. They very likely all get some toxins from rain and the air. But the ones getting diabetes are the ones “eating Western food”, it seems.
There was a guy that put some Hawaiians … which have epidemic rates of diabetes … on the traditional Hawaiian diet. So same environment, but just Hawaiian food. And their diabetes got quite a bit better, and they lost weight. But the diet he used was largely fruit based, which goes against the idea that fruit is bad for diabetics!
I don’t know why either. The two obvious targets for experimentation are wheat, beef, and dairy … just because those are the foods mostly associated with “The Western Diet” that are typically lacking from most other diets. (Milk in other countries is different than beef milk in several ways, so I’m not sure they can be compared easily).
Heather, @morgana —
Heather on this you say:
“We have pretty good numbers on traditional Japanese, Chinese, and folks in the Middle East … there were places where people tended to live a long healthy life…”
I respectfully yet resoundingly disagree!
We woefully lacked anything remotely approaching “good diabetes numbers”–esp for the much more prevalent T2D–on *any* population anywhere on Earth until well into the 1980s when home glucose testers became ubiquitous, and even then mainly in the developed world:
http://www.mendosa.com/history.htm
https://en.wikipedia.org/wiki/Glucose_meter
By which time the SAD and its variants had pretty much spread round the globe, along with most of the 100k+ novel chemicals that Dow, Monsanto, invented and ramped up their production.
Iow, Heather, by the time we could start to get any kind of grip on the true levels of T2D around the world, the confounders were already pretty much in place round that same orb of ours.
It’s true that strips that measure glucose in urine have been commercially available since the ‘50s:
https://en.wikipedia.org/wiki/Urine_test_strip
But they only test positive for excess glucose when blood glucose rises to ~180 mg (10 mmol/L) at which point the sugar starts to pass through the kidneys and spill into the urine. Normal BG levels are 75–95 mg/dL (4.2–5.2 mmol/L) and the fasting level considered to be diabetic is 126 mg/dL (7 mmol/L). This means we had millions of T2Ds walking the Earth unaware of their disease.
And we still do! And may still, alas, for decades to come 😦 –Bryan
1. “We woefully lacked anything remotely approaching “good diabetes numbers”–esp for the much more prevalent T2D–on *any* population anywhere on Earth until well into the 1980s when home glucose testers became ubiquitous,”
Maybe not exact numbers … no one was concerned much with diabetes until recently. But you CAN see how many “fat people” there are. The thing about T2 diabetes is that it typically shows up in body type. Less so in Asians … they go diabetic even when they are less-fat. But you can tell their fattiness generally from their pictures.
Go to the old Nat’l Geos. Look at the pics of the old mine workers, tribal people, Mongolians. You can get a pretty good take on their tooth health, skeletal health, rate of aging, fattiness. JUST from the pictures. Then go out to your town and look at people walking around.
But then Japan has government health care, so if someone is diabetic they tend to know it? Anyway, it didn’t come up as an issue in either the US or Japan until it suddenly exploded. Why? Mostly I’ve heard nothing but guesses (“We stopped exercising” … mind you a lot of fat people I know are in jobs like farming and janitorial, which requires lots of movement … ).
Anyway, when I see a 3X person, it doesn’t take a glucometer to tell me “something is wrong”. I see a lot of 3X persons these days!
2. ” Are you sure that all the centenarians among your Japanese Mountain people are totally free of all aches and pains, or other small problems? ”
No, I don’t know. It does say that the 100-year-olds still go out in the garden and harvest their own food. They aren’t in old-age homes. Their skin looks wonderful. Which is better than me at 30, when I started going wrinkly and arthritic!
The articles I’ve seeon on the Yuzus are totally guesses, that I’ve seen. I tried copying their diets. Didn’t last long. But I did come up with my Taurine theory which I’m trying out. I can say my hands look GREAT now … the skin is very supple and not dry. My joints work a whole lot better. I first tried avoiding fats, eating mainly taro etc. Which didn’t do much except my stools went yellow. Then I tried adding taurine/glycine/arginine/mag. And squid, some fish. And suddenly felt very different.
I do still get aches and pains, but I can go up and down stairs now without “puffing”. My blood circulation in general is better. We’ll see what happens over the next months …
3. “Of course the biggest example of potentially problematic phytochems: some gliadin proteins in gluten. Like for Neu5Gc, our bods generate antibodies to these potentially offending proteins, and most providers offer blood tests for that–IgA, IgG, and IgE. Yet it *appears* many people are unaffected by these glutenous proteins, and may even experience a healthful hormetic effect when they eat glutenous grains like wheat at or below threshold amounts. Though certainly many of us should avoid these gliadin proteins completely!”
Well, that’s been one of my soapboxes for years and years now! To the point I was dubbed “The Glutenator” in one group I was in. Anyway, I can’t be very unbiased about gluten because if I DO eat it I feel like someone made me swallow hot coals. For me the stuff is evil incarnate.
My standard answer though, is that I have yet to see an example of a “healthy culture” (say, a “blue zone”) that eats mainly wheat. (ooh, sounds like beef, huh? But wow, they tend to go together, I like I said. the inland diet!). Anyway, there are early early wheat-based cultures, like Egypt and Rome. And they accomplished a lot. And were also a bit crazy. And and loads of health issues.
My own (very personal) take is that wheat promotes a kind of high-functioning autism that also promotes great cultural progress. And also makes for major health problems. Biology is like that a lot. Many of the “super healthy” cultures also did nada in terms of inventions. It’s the “tortured geniuses” that did the inventing. Just sayin’
In terms of this blog though … the majority of the “VLF” diets are also rice-based. A few “allow” wheat, but mainly in the whole-wheat form. I do believe (again, based on personal experience) that the wheat husk interferes somehow with the IgA reaction in the gut. Almost all the “healthy” diets I’ve tried, somehow limit wheat, though they don’t say so outright.
Also, it should be said that celiacs get their symptoms not from the *gliadin* but from the *TTG* … which is a whole different molecule. TTG comes from yeast basically, but is also an additive for high-rise bread these days.
Heather, @morgana —
Heather, this jumps out at me the most:
“…My own (very personal) take is that wheat promotes a kind of high-functioning autism that also promotes great cultural progress. And also makes for major health problems. Biology is like that a lot. Many of the “super healthy” cultures also did nada in terms of inventions. It’s the “tortured geniuses” that did the inventing. Just sayin’…”
YUP!! Can’t say specifically about wheat driving high-functioning autism, but it’s an intriguing idea! In general, you’re right on about the idea that civilizing can impose health penalties, that such advancements often fail to bring unmitigated good. I’ve posted Jared Diamond’s view of wheat several times in this forum. But here it is again:
http://www.ditext.com/diamond/mistake.html
The Worst Mistake in the History of the Human Race
which he wrote way back in 1987.
About what you say here: “…Maybe not exact numbers … no one was concerned much with diabetes until recently…”
Heather, again, I have to at least partly differ with you here. At least for T2D. We simply can’t say what level of problem T2D was through the centuries and millennia, going back to the Ag Revs. For all we know, since people started eating wheat and other glutenous grains, and even rice, T2D rates popped significantly as we formed our first civilizations. The Egyptians may have identified the problem as early as 1550BC, over 3500yo:
http://www.healthline.com/health-slideshow/history-type-2-diabetes#1
But of course we have no way to know how severe the problem was till ~12k years after the Ag Revs, with the advent of home BG testing and rapidly spreading preventative health care.
We truly we don’t know the depth of the T2D problem even now. T2D affects us so thoroughly systemically–high BGs glycates and thus corrupts vascular endothelial linings in every millimeter of our ~70,000 *kilometers* of vessels, that T2D in essence is a disease that accelerates overall aging. From atherosclerosis to the glycating and cross-linking of parallel long-strand proteins in collagen causing them to “lock up” hence tendon stiffness, to retinal degeneration to impotence, just to name a few of its very many effects. Until very recently, we attributed these effects to a multitude of other causes. We usu summed up all these causes as “aging” and “life.”
In the last 100–150 years, the more we sussed out diabetes, the more people we discovered to suffer from it. By the turn of the last century, diabetes awareness had risen enough to prompt Dr Joslin to started his diabetes clinic in Boston. This was before Banting and Best developed insulin therapy in 1922.
At first we focused on the acute form of the disease, the so-called Type 1 diabetes in which the beta cells stop producing insulin, requiring insulin injections. Indeed only in the ‘30s did we identify T2D as a separate condition from T1D:
http://www.healthline.com/health-slideshow/history-type-2-diabetes#5
We only now get a real idea of how ubiquitous T2D is, and perhaps *was* for all those years earlier before the advent of the worldwide SAD likely greatly exacerbated the problem. Since ~2005 the world has more overweight people and too-thin and calorically malnourished people. But as you alluded to Heather, esp in Asians, we find millions thin T2Ds who look perfectly fit.
My point: diabetes–esp T2D–likely existed in people worldwide **at non-negligible levels** since the Ag Revs.
About this you say “…it should be said that celiacs get their symptoms not from the *gliadin* but from the *TTG* … which is a whole different molecule…”
Heather this suggests that gliadin epitopes *do* in fact directly contribute to coeliac lesions:
http://www.ncbi.nlm.nih.gov/pmc/articles/PMC1808891/
“…The intestinal lesions of coeliac disease (CD) are caused, in genetically susceptible individuals, by a T-cell response to epitopes of wheat dietary gliadin…”
BTW, “gliadin” refers to not just a single protein but a group of them:
https://en.wikipedia.org/wiki/Gliadin
–Bryan
Hmmmm, wheat and high functioning autism? Well, there is a current theory that autism is caused by certain gut flora- (or lack thereof?)- which is an intriguing theory (by no means proven though). I don’t think it’s limited to wheat though, but probably to whatever substance that individual is sensitive to. Some autistic people have trouble with eggs, soy, or even rice. Again, it’s not only one substance, or a “1-size-fits-all”. Although I’m a celiac, I’m not convinced that wheat is detrimental to everyone; it may be, I’m just not sure.
I do believe that grains probably did affect our brains in some way. It may sound strange, but I wonder if grains gave people “delusions of grandeur”. It seems that those societies who started eating lots of grains tended to want to go out and conquer the world! I’ve even wondered if some of the ideas of “supremacy” came about through wheat and civilization. It might make people a bit “crazy”. I don’t think the inventions that came about were due to autism; (some might have been); but more likely that through civilization, people became more specialized- i.e., they didn’t need to spend all their time worrying about the day-to-day hunting and gathering of food, so they could use their time and creativity elsewhere.
I also highly doubt that “everyone has high functioning autism”. Trust me, for people who really do have autism or Asperger’s, the civilized world is a *very* difficult place to live in! People who are “neurotypical” have a certain way of being, and the autistic person struggles like mad just to get by in this world. It causes a huge amount of stress. Most people are highly social, and autism is, first and foremost, a problem with social interaction. Although I believe some of our greatest thinkers, inventors and artists were probably autistic- (certainly not all) I can definitely say that the general population is *not* autistic!
1. Crazy: “I do believe that grains probably did affect our brains in some way. It may sound strange, but I wonder if grains gave people “delusions of grandeur”. It seems that those societies who started eating lots of grains tended to want to go out and conquer the world! I’ve even wondered if some of the ideas of “supremacy” came about through wheat and civilization. It might make people a bit “crazy””
Oddly enough, the only civilizations that actually went out to *take over* other lands were wheat-eating ones … Middle East, Rome, Mongolia. Oddly enough, schizophrenia is found mainly in wheat-eating countries. So yeah, literally, it seems to make people crazy.
2. Autism and invention: ” I don’t think the inventions that came about were due to autism; (some might have been); but more likely that through civilization, people became more specialized-”
““What would happen if the autism gene was eliminated from the gene pool?
You would have a bunch of people standing around in a cave, chatting and socializing and not getting anything done.”” (Temple Grandin).
A number of people have theorized that Aspies did much of the inventing in the world. The smart people who are NOT Aspies tend to go into politics I think! At any rate, most “normal” people just don’t sit alone in a room day in and day out not talking to anyone, working with test tubes or electronics or a math problem.
3. Autism and wheat: A number of Aspies have commented on this one … that when they drop wheat, their thinking changes. It certainly did for me, to the point that I had to re-learn how to do my job without the easy “fugue state” I need to do intense software development or math. I did get better at being able to follow conversations or to see expressions in faces. But worse at figuring out difficult abstract problems. Then I’d go eat a piece of bread … and I could concentrate better! (but get sick for few days too).
For me it’s decidedly a drug effect. That maybe isn’t too surprising … zonulin makes the brain-blood barrier permeable, and for celiacs, the MRI scans change after they eat wheat.
And yes, it’s difficult to live in “normal” society if you have Asperger’s. Which is probably why it’s been pretty rare even in wheat-eating countries. Also the fact that if you react to wheat you are very likely to die in childhood (most celiacs didn’t survive before antibiotics were invented). I lived off antibiotics until I changed my diet!
Oddly they can mimic Asperger’s by using a strong magnet to disable part of the “social brain”. If the social brain is disabled, then the “math brain” gets smarter.
Heather, @morgana — Heather very interesting this you say:
“…when [the Aspies] drop wheat, their thinking changes. It certainly did for me, to the point that I had to re-learn how to do my job without the easy ‘fugue state’ I need to do intense software development or math. I did get better at being able to follow conversations or to see expressions in faces. But worse at figuring out difficult abstract problems. Then I’d go eat a piece of bread…and I could concentrate better! (but get sick for few days too)…”
I’ve wondered that in myself too, though don’t go as deep as the fugue state. Yet when I fast and esp when I walk and fast, my mind thrums along in a weirdly calm way, almost like it moves in a fast synchronized lope. And it makes scads of wonderful connections.
BTW, I don’t think Mongolia had much wheat back in Genghis Khan’s time:
https://en.wikipedia.org/wiki/Agriculture_in_Mongolia#History_and_growth_of_production
In those early glory days of Mongolian Eurasian domination, yes it *was* lamb/mutton morning, noon and night.
And this from you:
“…Oddly they can mimic Asperger’s by using a strong magnet to disable part of the “social brain”. If the social brain is disabled, then the “math brain” gets smarter…”
I’ve heard of using magnets to activate the emotion-sensitive brain
https://www.psychologytoday.com/blog/my-life-aspergers/201002/how-science-is-using-magnetic-energy-rewire-our-brains
but not to disable it. I’d like to learn more about that. –Bryan
1. Khan’s armies: In Marco Polo, wheat was mentioned quite a bit. And in history:
https://books.google.com/books?id=A8Y9B5uHQcAC&pg=PA177&lpg=PA177&dq=genghis+khan+wheat&source=bl&ots=Cb92rJe1i0&sig=3m_kwc_P7dahao0ZrwTMiuGWGiA&hl=en&sa=X&ved=0ahUKEwioyM2N1N3KAhUNzmMKHdifA7sQ6AEIPjAF#v=onepage&q=genghis%20khan%20wheat&f=false
Page 172, one of the Khan kids travelled with wheat. So they did farm it. Probably still ate mostly meat: apparently they still do.
2. Asperger’s and magnets: Interesting they can use it as a treatment now! The study was something like this one:
http://www.popsci.com/science/article/2013-05/electrical-brain-stimulation-improves-math-learning-study-finds
Except they also talked about how it mimicked Aspergers.
3: Wheat and fructose: “Btw, wheat is fructose-free. Wheat has two starches–amylose and amylopectin. Both glucose-only polymers.”
“Fructans are chains of fructose molecules which end in a glucose molecule and they can cause the same problems to a fructose malabsorber as fructose itself.
Fructans are found in many grains and vegetables including:
• wheat, spelt, kamut and brown rice
• many members of the onion family, artichokes, asparagus, green beans and tomato paste.
However, you will be relieved to hear that the following grains are fine:
• rye, oats, buckwheat and white rice
• ‘alternative grains’ such as amaranth, teff, millet, corn, tapioca etc.
But, be warned, the glucose/dextrose trick does not work with fructans.”
http://www.foodsmatter.com/allergy_intolerance/fructose_intolerance/articles/fructose_good_bad_malabsorbed.html
“But the gastroenterologists around the world who’ve been trying understand the gluten puzzle say they’re increasingly convinced of two key things: One is that the number of people who are truly non-celiac gluten sensitive is probably very small. Second, they say that the people who say they feel better on a gluten-free diet are more likely sensitive to a specific kind of carbohydrate in the wheat — not the gluten protein.
That carbohydrate, called fructan, is a member of a group of carbs that gastroenterologists say is irritating the guts of a lot of people, causing gas, diarrhea, distention and other uncomfortable symptoms. Altogether, these carbs are called fermentable oligo-di-monosaccharides and polyols, or the cumbersome acronym FODMAPs.”
http://www.npr.org/sections/thesalt/2014/05/22/314287321/sensitive-to-gluten-a-carb-in-wheat-may-be-the-real-culprit
Fructans are a big issue with wheat. And they break down into fructose. Given that in some cultures wheat is the majority of the diet, that would have an effect I think.
4. “Thin as a stick diabetics”: First I’ve heard of that. But there are still cultures living their traditional neolithic diet (like the Yuzus). Are they borderline diabetic, even though they live 100 years? And if they are a healthy 100 years old, are their blood sugar numbers really an issue? It seems in studies the general trend is that the yam eaters are the healthiest, followed by the rice eaters, followed by the wheat eaters.
Yams were probably the first starchy foods that homids ate a lot. A lot of the old hominin bones are found near naked mole rat places … probably because the hominins relied on yams as at least emergency food.
http://cogweb.ucla.edu/Abstracts/Pennisi_99.html
http://www.nature.com/news/2007/070430/full/news070430-5.html
There are only a handful of cultures that do NOT have a “staple starch”, now or in the past, so I guess if you don’t count weight issues, there is no way to tell if the pure meat/fish eaters were healthier than the starch eaters in general.
“Nor do modern tropical hunter-gatherers rely heavily on meat. Among modern tropical African tribes, “there is no case of [people] eating more meat than plant food,” Wrangham points out. For example, anthropologists James O’Connell and Kristen Hawkes of the University of Utah, Salt Lake City, found that although a hunter belonging to the Hadza tribe of Tanzania on average might catch one large animal per month, often weeks would go by with no kills. The Hadza hunt with bows and arrows, technology far more advanced than that of any early humans, yet even for these modern hunters, “this is no way to feed the kids,” says Hawkes.”
There are tribes that can use fruit as their staple, rather than starch. Like say, bananas or breadfruit. And some that can live mainly on nuts. Has anyone checked their BG levels?
Ooooh … I found one!
“‘Im going to start with an extreme example. In the 1960s, when it was fashionable to study non-industrial cultures, researchers investigated the diet and health of a culture in Tukisenta, in the highlands of Papua New Guinea. The eat practically nothing but sweet potatoes, and their typical daily fare is 94.6 percent carbohydrate. Whether or not you believe that exact number, their diet was clearly extraordinarily high in carbohydrate. They administered 100g OGTTs and measured blood glucose at one hour, which is a very stringent OGTT. They compared the results to those obtained in the 1965 Tecumseh study (US) obtained by the same method. Here’s what they found (1):”
http://wholehealthsource.blogspot.com/2010/11/glucose-tolerance-in-non-industrial.html
There’s way more. So one COULD research how various pre-industrial societies handled blood glucose.
Heather, a few minutes ago I posted a response to your post, talking about Mongolians and wheat. Do you see it? I don’t see it from my end. But when I tried to repost it, Neisy’s site gave me the “duplicate post” message. If you would check and let me know. Thanks. –Bryan
Heather, @morgana, Top o’ the Morn/Aft —
Heather, you say “…one of the Khan kids travelled with wheat. So they did farm it….”
This keys off what you posted yesterday:
“…Oddly enough, the only civilizations that actually went out to *take over* other lands were wheat-eating ones … Middle East, Rome, Mongolia…
Which in turn riffs off what you said earlier that day:
“…My own take is that wheat promotes a kind of high-functioning autism that also promotes great cultural progress. And also makes for major health problems. Biology is like that a lot. Many of the ‘super healthy’ cultures also did nada in terms of inventions. It’s the “tortured geniuses” that did the inventing…”
Your comments took me straight to related Qs I’ve mulled a lot the last few years. Can going grain-free low-carb make one less competitive? Less successful in a material way? Less willing to fight for things, like promotions? In bref, can it impose a trade-off between physical and physio-mental health and career and material success?
I look at my n=1. Over most of a decade, I’ve lived no-grain low-carb. My body and mind calmed way WAY down after I went grain-free low-carb. My health is apparently terrific. My med cabinet is bare. I routinely walk and run 10 or more miles. In 2014 I had an open-incision inguinal hernia repair. I walked out of post-op and walked (albeit very slowly!!) four miles! (My surgeon encouraged me to walk AMAP ASAP.) I took not a single post-op med, not even an NSAID. My only ache is mild lower back pain that creeps back if I skip my daily core exercises for a while. I write and edit for a living and sit a lot.
BUT Heather …I’m definitely not the go-getter I was 15 years ago. I have a shade of the wealth I used to have. I don’t scrap like I used to. Obviously I have to consider mitigating factors–the economy, life events like divorce and loss of my Mom, I’m getting older (now 55). I now lose more and more family and friends to chronic disease. This impels me to seek better health, but also to think more what exists beyond our mortal coils.
So, for these core Qs (even for the after*this*life – I look at Tibetan Buddhism, which Altan Khan adopted), I’m so glad we discuss the early Mongols. They are an intriguing anomaly in world history and a terrific example how essentially grain-free low-carb people can show tremendous, even unparalleled, ambition.
Few people enjoyed “career” success like Genghis Khan. GK and his heirs, these fast-traveling warrior horsemen who built the largest contiguous land empire in world. Yet Genghis Khan and his descendants are the only empire-builders who traditionally ate few if any grains! Until they occupied their newly conquered lands, the Mongols ate almost exclusively meat and dairy.
https://en.wikipedia.org/wiki/Mongol_Empire
https://en.wikipedia.org/wiki/Society_of_the_Mongol_Empire#Food_in_the_Mongol_Empire
In the book you linked, “Genghis Khan and the Making of the Modern World” by Weatherford, the “Khan kid” you refer to is Hulegu, Genghis Khan’s grandson, who conquered Persia (now Iran) and much of the rest of Western Asia.
https://en.wikipedia.org/wiki/Ilkhanate
So yes, in Hulegu’s new Ilkhanate, they farmed and ate wheat. But again, back in their high-steppe homeland, the vast arid windswept stretches that helped craft and inform the natures and impulses of these early Mongolians that led them to storm over and conquer so much of Eurasia, they practiced very little if any agriculture until the Soviets imposed it on these much-humbled people in the last century. Now modern Mongolians–at least the urban Mongolians like those who live in Ulaanbaatar which is home to nearly half the country’s population–eat more like their fellow urbanites around the world. The modern diet for most Mongolians includes plenty of grains such as guriltai shol (wheat noodle soup) and the now staple wheat-based pastry called bordzig. For info on that, start on page 43 in “The Changing World of Mongolia’s Nomads” By Melvyn C. Goldstein and Cynthia M. Beall. –Bryan
1. Success and wheat: ” Can going grain-free low-carb make one less competitive? Less successful in a material way? Less willing to fight for things, like promotions? In bref, can it impose a trade-off between physical and physio-mental health and career and material success?”
It’s a really, really good question. I have an old encyclopedia, circa 1909. The author has a really long article on grains. He was questioning why Britain and the other European countries took over the world, rather than vice versa. He didn’t say we are smarter or graced by God or whatever … his take was that our staple grain … wheat … “gives more energy” and motivation than rice and yams do. That eating rice makes one complacent.
The Romans had a similar idea … they fed the slaves barley, but the masters got wheat. Well, barley was cheaper, but also … it didn’t promote rebellion. (Or so I’ve read: I have no idea how true it was). In Ireland the peasants weren’t allowed to eat the wheat they planted … the peasants ate potatoes and the rich folks got the wheat. My granddad said the same thing from Germany. “Rich people eat wheat. Poor people eat oats.”.
So wheat gets this outsized status. Like a drug, not like a food.
Now, I had pretty bad depression and anxiety for 30 years or so. It stopped cold when I stopped eating wheat. It was like being on Prozac I think (not that I ever tried Prozac!). But I just COULD NOT worry like I used to, even when some pretty bad stuff was going on. And without the worry, I stopped writing poetry or keeping journals or going on long rants about the injustice of life. OK, I still do long rants, but they are about stuff like this!
So I have two kids now, and we talk about this. They are decidedly Aspie, but they don’t have the meltdowns and anger fits that Aspie kids are prone to. And oddly, they are also quite social and popular. My daughter worried for a long time though, that she wouldn’t be a “real” Aspie because of the lack of wheat. And it is true, she is not as good at math and engineering as I probably was at her age. But she IS successful, and more so in that she handles people a whole lot better.
As far as material success though … look at Manoz, the founder of the 5-hour-energy drinks. He’s rich as anything now, but he spent 10 years as a monk, meditating. He has a movie on Netflix, called “Billions in Change”, which talks about what he’s doing. His attitude is amazing. Of course he does seem to eat wheat I think (it wasn’t mentioned).
2. Mongols and wheat: Pretty much everything I know about the Khan’s time is from Marco Polo on Netflix! It does seem to have been well-researched though. So how much wheat they ate vs. meat and milk … someone else can do the research! Thing is though, in terms of Asperger’s, dairy is the other food that seems to set people off (I’m dairy-free too). So they had a LOT of dairy. Anyway, there was something about them that made them motivated to take over the world. Most cultures just don’t DO that.
Also they did seem to have an issue with obesity, if you look at the old pics, and gout. So at least one level of society wasn’t low-carb. And does alcohol count as a carb? They were noted for drinking a lot.
And in some places at least, their diet is still meat, meat, and more meat. It does not appear to make them live longer:
“Mongolians are known to have relatively short life expectancy. In order to examine the role of dietary habits in the early aging of Mongolians, the food intake inquiry, anthropometric measurements and blood clinical tests were performed for 365 healthy inhabitants in Murun, a northern Mongolia city, and compared to those of Japanese. Murun inhibitants were found to have a characteristic dietary habit of taking large amounts of meat, milk, dairy products and wheat flour products, in contrast little vegetables, fruits and fishes.”
http://www.ncbi.nlm.nih.gov/pubmed/20021377
Heather, @morgana —
OK, here’s on fructose and wheat.
Heather, our thread goes back to what you posted yesterday:
“…the Japanese and Chinese are both more prone to getting diabetes NOW, but weren’t on their traditional diets. It does seem to be related to fructose (but not raw fruit)… Which makes sense. Wheat starch is half fructose, half glucose, while rice is glucose-glucose…”
First off, what you say “…Wheat starch is half fructose, half glucose…,” Heather, truly, it isn’t. Wheat starch (amylose + amylopectin) is all glucose baby.
But sure, why don’t we look at the *entire* wheat product? As you shifted to in your last post?
For the purposes of fructose’s effect on blood sugar–which is, after all, the focus of your above post, right?–then it’s as I said: Wheat is fructose-free. We appear to realize little if any free fructose when we process wheat in our GIs, and then only in our colons.
In wheat bread, the starches (amylose + amylopectin) are the dominant nutrients. They total nearly almost half the total content of that food by weight:
http://ndb.nal.usda.gov/ndb/foods/show/5611
Meanwhile that same USDA link shows the fiber content comes to only four percent. Of which fructan represents only a part.
This link corroborates that USDA link, showing a very minor fructan content in wheat, <1–3% (scroll down to the table “Fructan content of various foods”):
https://en.wikipedia.org/wiki/Fructan
You can see Heather, this fructose-glucose ratio falls far below your “…half fructose, half glucose…” assertion. Which assertion btw *is* correct for many fructose-containing foods, including many fruits, honey, maple sugar, and table sugar. Those foods that have some balance of sucrose (a disaccharide with one molecule each of glucose and fructose) and their free dissociated glucose and fructose simple sugars.
Furthermore Heather, as you noted, wheat’s fructose is bound up in fructan, a polysaccharide fiber. Inulins are fructans:
https://en.wikipedia.org/wiki/Inulin
We can’t enzymatically digest fructans. They must pass down into our colons where our gut bugs ferment them. Our flora ferments them into various products which include short-chain fatty acids like butyrate. Gases too, as many of us know only too well:
http://www.ncbi.nlm.nih.gov/pubmed/17381985
http://aem.asm.org/content/75/18/5884.full
Heather if you can find where we ferment fructans into actual fructose, I'd love to see it. I've never heard of it.
Again, when we speak of fructose’s effect on BG, wheat is fructose-free. –Bryan
Heather, @morgana, here’s on thin diabetics:
http://www.phlaunt.com/diabetes/14046739.php
“… one out of five people diagnosed with diabetes are thin or normal weight…”
How many diabetics are that? Let’s run the numbers.
In 2014, the world had 7.1 billion people:
http://www.usnews.com/opinion/blogs/robert-schlesinger/2013/12/31/us-population-2014-317-million-and-71-billion-in-the-world
This WHO reports estimates:
http://www.who.int/mediacentre/factsheets/fs312/en/
that in the same year, 9% of adults 18 years and older had diabetes.
9% of 7.1 billion people = 639 million diabetics worldwide. As of two years ago.
That same WHO report claims 90% of those diabetics are Type 2:
639 million diabetics worldwide x 90% = 575 million T2Ds worldwide
Bear in mind that, unlike T1D, where we quickly see dramatic symptoms, T2Ds *can wander the planet for years with no overt clue of their disorder*
If one in five of these T2D are thin, then:
575 million T2Ds worldwide x 20% = 115 million *thin* T2Ds worldwide.
The vast majority of them will be the “thrifty gene” Asians.
More links for you:
http://chriskresser.com/think-skinny-people-dont-get-type-2-diabetes-think-again/
“…Studies of lean, Asian Indian men have found that they have a 3- to 4-fold higher incidence of insulin resistance than their caucasian counterparts. They also have a much higher prevalence of non-alcoholic fatty liver disease (NAFLD) and hepatic (liver) insulin resistance…NAFLD is an independent predictor of type 2 diabetes. Cross-sectional studies have shown that fatty liver and metabolic abnormalities occur together…fatty liver is not just a result, but also a cause of insulin resistance and type 2 diabetes…these Asian Indian men … were lean, and in some cases, even underweight…”
http://content.time.com/time/world/article/0,8599,1902100,00.html
Study: Diabetics in Asia Are Younger, Thinner
“…Asia’s growing number of diabetics are relatively young and well under weights traditionally matched with the disease…”
“…doctors in Vietnam say the spike in diabetes has not been fully explained. ‘Our patients are not obese. Some are very thin,’ said Dr. Khanh…Ms. Mui, who was born in the provinces but works as a dental assistant in Ho Chi Minh City, is rail thin with a 27-inch waist.”
http://www.medscape.com/viewarticle/779072
Thin Asians at Risk for Diabetes Due to Hidden Body Fat
http://desinutritionauthority.com/2015/06/why-young-slim-vegetarian-non-smoking-indians-are-struggling-with-cardiac-blockages-heart-attacks-and-diabetes/
Why Young, Slim, Even Vegetarian, Non-Smoking South Asians/Indians Are Struggling With Coronary Artery Disease, Heart Attacks, And Diabetes
Lemme know if you need/want more. –Bryan
Well, I’ll leave the diabetes speculation up to you. Most of what I’ve read says that diabetes is related to iron levels in the body, which is affected by a whole mess of factors, including stuff like leaky gut, which IS wheat related (also sometimes milk). In which case the huge increase lately may well have to do with iron fortification. And a lot of other people believe it has to do with fructose. And I think it may have to do with taurine too, since taurine actually does the glucose-shuttling.
Anyway, my BG is ok now so I’m not experimenting with it at the moment. Too many other rabbit holes to fall into!
wbryanh, heathertwist- Apropos diabetes in traditional cultures: there are parts of Africa where they have force fed women, making them fat, to attract a husband, as fat is considered beautiful. (Gary Taubes writes about this in Good Calories, Bad Calories). I wonder how many of these women of the past suffered from diabetes?
http://news.bbc.co.uk/2/hi/programmes/crossing_continents/6591835.stm
Heather, @morgana —
Heather, about the “ancestral-ity” of yams and other tubers, I’d love to learn more! Esp if we learned how to “produce” them in the pre Ag days. The CW is that we learned to plant and grow food only during the Ag Revs. But why wouldn’t we have learned how to cultivate root veg and tubers well before then? Doesn’t seem like such a stretch to figure out how to do that.
*If* we never learned to cultivate roots/tubers in the pre Ag days, than we likely ate a lower percentage of carbs than in the post Ag period. I read somewhere that ancestrals preferred meat to roots/tubers and ate the latter mainly in lean times. I’ll try to find that link.
Here’s a few links on a recent report, titled The Importance of Dietary Carbohydrate in Human Evolution, Karen Hardy et al:
http://www.jstor.org/stable/10.1086/682587?seq=1#page_scan_tab_contents
Click to access Press_release_QRB.pdf
Hardy’s full report used to be freely available, but now seems stuck behind a paywall. But diligent googling may turn up the full report.
My sense is that cooking in general–both tubers and meat–is what super-sized our brains. Our brains run on either glucose or ketones. For both tubers and meat, cooking them makes their kcals way more bioavailable to us.
Bear in mind Heather, my recent remarks about people possibly underestimating pre-SAD T2D rates, I confine them to people living in Ag systems in the post Ag period, after which people started to eat loads of wheat and rice with their attendant unique nutrients/anti-nutrients. You give examples of pre Ag folks who lived/live ancestrally and not in large communities, like the early hominins and to extant/very recent groups like the Hadzas and the Papua-New Guinea highlanders. –Bryan
“*If* we never learned to cultivate roots/tubers in the pre Ag days, than we likely ate a lower percentage of carbs than in the post Ag period. I read somewhere that ancestrals preferred meat to roots/tubers and ate the latter mainly in lean times. I’ll try to find that link.”
It’s not really a question … eating tubers was ubiquitous everywhere that I’ve heard of. They weren’t necessarily “planted” … they grew everywhere, and maybe some industrious people took out the competing plants. Lewis and Clark described the bushels of tubers that the Indians collected, which they bought and used to feed their men. Some native tubers are HUGE … taro for one, which was a staple all over. So unlike grains, you can just leave them in the ground to get bigger and bigger, until you want to eat them. Tiger nuts too … they are high in protein and easy to harvest. I think chimps go for tubers too, albeit they are easier to eat if you can cook them.
“My sense is that cooking in general–both tubers and meat–is what super-sized our brains. Our brains run on either glucose or ketones. For both tubers and meat, cooking them makes their kcals way more bioavailable to us.”
I keep sensing this bias towards “meat”. Why? Shoreline food is way easier to get. You can eat mussels and fish without cooking just fine (tubers do need cooking!). Shoreline food has way more “brain” ingredients. Humans mostly lived on the coast of the ocean or a lake or in swamps, from hominin times. To be smart, humans need DHA, iodine, and taurine, at least.
I also keep sensing an anti-carb bias. Again, why? The assumption that “carbs cause diabetes” is purely that … assumption. The logic seems to be “Carbs cause diabetes. Therefore our ancestors who ate carbs must have been diabetic”.
And yet the tests done in the ’60s didn’t show diabetes in tribal cultures eating carbs.
I have heard that Asians get diabetes at much thinner weights, so that is a point. But they aren’t getting diabetes as they eat “more carbs” … in fact they are eating FEWER carbs as they eat more “Western” foods. But in any case, it’s testable, and has been tested. And I just don’t see anything that says a “high carb diet” in general is associated with diabetes.
Which was the whole point of Denise’s post about the Rice diet and VLF diets! A super super low fat diet may not have cured diabetes, but it helped the majority. I kind of think the carb/fat ratio for humans is a bit of a red herring, and the real culprit will end up being something like iron or taurine. But all the people experimenting will get us to the answer faster!
wbryanh, heatertwist- Wow, there’s been a flurry of activity between you 2! So many posts, I just can’t keep up, since my work schedule has gotten busier. So I’m going to use just this one post to comment on the points that “jump out at me”:
First off, wbryanh: yes I remember I posted a link about protein and how it doesn’t always turn into glucose. That seems to be how it works with me; I seem to be able to eat quite a bit of protein and still stay in ketosis, whereas carbs will bring me out of it. I just added that caveat in my post because I have read that protein *can* be an issue for some people with stubborn weight loss, or high blood glucose levels. I can’t say that it’s 100% true, since it doesn’t seem to work that way for me, but I have read about it online, which is why I included it.
About wheat/Asperger’s: heathertwist:-wow, so stopping wheat made things different for you, and your children? In my own case, it definitely helped my physical issues. But aside from that, I’m still just as bad socially as I ever was. Sensory issues aren’t any better, and can be a huge source of stress when I go out into the world. I definitely, generally do feel “calmer”, but it’s hard to say if that’s due to stopping wheat, or if it’s due to the fact that I live alone now and have time in my schedule to be at home alone for certain periods of the day, between work. This helps absolutely more than any dietary change! So, yeah….I don’t notice my thinking being any different than before. But I never really particularly noticed a “foggy thinking” problem with wheat, which some people have commented on.
Oddly enough, I do notice one difference not due to wheat, but to going low carb in general- (I stopped eating wheat about 10 years ago, but remained high carb, and still eating non-glutinous grains for awhile). Back when I still ate “high carb”, my “self” would become very internalized. If people in public or in the workplace tried to make conversation with me, or eye contact or something, being the experienced adult that I now am I was aware of how I was “supposed” to react; I knew I had to smile, or what text was expected of me, but I felt like it was hard for me to come out of my internal world. It seemed like such effort, like *I* was buried deep inside myself, and I had to try to go down into the depths of my very being to “bring myself up”. It’s hard for me to explain, but it was really quite difficult. Since going low carb, I feel like I’m more “accessible”, and like it’s easier for me to at least associate with the outside world. I’m not any better at social situations, but faking it is certainly easier, ha ha!
Re/Type 2 Diabetes: thin people can most definitely get it! In fact, those so-called “professionals” that claim that being fat causes diabetes are wrong. It is now believed that storing fat is a protective mechanism, and it’s actually a way of staving off diabetes. So it’s a symptom rather than the cause. But there are quite a few overweight people in the world who are metabolically healthy too. I’m pretty sure I’ve read that diabetes has been documented in ancient Egypt and Greece- (not sure if it was just type 1, but I think it was both types). Sorry, no links tonight because I’m just too tired, but if you ask for some I’ll try to look tomorrow.
My own personal theory- (and that of some professionals) is that it is mostly caused by sugar (namely the fructose part, although the mix of both fructose and glucose might be even worse). I’m NOT talking about the small amount of natural fructose in whole foods. So what would be implicated is the high sugar foods and high fructose corn syrup, fizzy drinks, and all those fake sugars that are ubiquitous in modern diets. Also, like with Pottenger’s cats, I think it’s a problem that accumulates with generations, so the tendency is for it to get worse by generation; fetuses are affected by what the mothers eat, and so forth. So I personally believe that the native people eating high carb, whole food diets were healthy. Of course, once you get diabetes, then even those natural sugars and carbs might be a problem, but I don’t think they cause the problem in the first place (this is just my theory, I don’t know it for sure). It does seem to be true that yams and sweet potato seem to be staples around the world, and the people who eat them seem to be very healthy. I’ve become interested in sweet potatoes lately, and- even though I’m mostly “low carb”- just recently started eating them again sometimes. I started craving them.
Lastly: I do think there is a link between wheat eating cultures and the desire to overtake the world. Maybe not in every case- (like with Genghis Khan?). There may be other reasons why people may want to conquer others as well, but the wheat link seems to be pretty strong in any case. But that is absolutely *not* a trait of autism or Asperger’s! It’s very Neurotypical to see the world in a hierarchy, and want to “rule” over others. The Aspie is not interested in “ruling” anyone; they would rather have the quiet life on the side. The reason they seem ambitious (i.e. scientists, artists or inventors) is that they want nothing more than to spend all their time on their special interests! So it’s not the notoriety they’re interested in. It could be maybe that wheat affects autistic and non-autistic people in different ways? Anyway, I think this discussion about wheat and the brain is fascinating! I wish more people wrote books on this subject.
1. Aspies rule the world!: “The Aspie is not interested in “ruling” anyone; they would rather have the quiet life on the side. ”
I totally agree. The “wheat effect” … whatever it is … works differently in different people. However, I think it’s pretty clear that say, the Romans and Egyptians, had some Aspies working for them figuring out how to do roads and pyramids etc. Clever war tools and strategies let them win. Someone I know who works in Las Vegas commented that they have more geeks per square mile than anywhere else on Earth … figuring out how to make those shows work.
Do you think the US could have warplanes and satellites if there were no geeks?
2. Carbs and diabetes: “It does seem to be true that yams and sweet potato seem to be staples around the world, and the people who eat them seem to be very healthy. ”
There is an interesting blog that gets into some of the actual evidence for some of this. Unfortunately he doesn’t actually get into information on fish much. But he does point to some sources for actual pre-industrial health information.
a. Sweet potatoes: The Papua New Guineans traditionally subsisted on a plant based diet, of which a number of varieties of sweet potatoes typically supplied over 90% of dietary intake. They also grew a number of other crops including corn, as well as sugar cane which was consumed as a delicacy.
…
In 1973, Sinnett and Whyte published findings from a survey of 779 highlanders using electrocardiograms among other methods, and found little probable evidence of coronary heart disease, and no clinical evidence of diabetes, gout, Parkinson’s disease, or any previous incidence of stroke.16
b. Stefansson: In 1928, Stefansson and his colleague Karsten Anderson participated in a monitored experiment partly funded by the meat industry in which they consumed a flesh exclusive diet for the period of one year. Although the researchers concluded that these two men were in good health throughout the experiment, Anderson experienced a severe elevation in blood cholesterol, with measurements as high as 800 mg/dl on one occasion, which returned to pre-experiment levels after resuming a higher carbohydrate diet.2 A glucose tolerance test carried out immediately after the termination of the meat based experiment showed a marked rise in blood sugar in both men compared to a subsequent test carried out after resuming a higher carbohydrate diet. Glucose was detected in the urine of Anderson in the test following the meat based experiment, a marker of untreated diabetes. This abnormality was not detected in the subsequent test after resuming a higher carbohydrate diet.3
c. Inuit: Contrary to claims of the traditional living Inuit being immune from cardiovascular disease, evidence of severe atherosclerosis has been identified in several frozen mummies of Alaskan Inuit dating back to 400 CE and 1520 CE, both instances predating European contact.7 8 Atherosclerosis has also previously been identified in several artificially prepared mummies of Aleut-Unangan hunter gatherers who lived in the 18th century in the Aleutian Islands in Alaska.9 10 Recently the HORUS study, which examined an additional five recovered mummies of Unangan hunter gatherers who lived in the mid and late 19th century found definite evidence of atherosclerosis in several major arteries in all three who were over the age of 25.11
d: Okinawans and Japanese (with more details on their diets): In 1946, Steiner examined autopsies of 150 Okinawans, of which 40 were between the age of 50 and 95. Steiner noted only seven cases of slight aortic atherosclerosis, all of which were found in those over the age of 66, and only one case of calcification in the coronary arteries. In 1946 Benjamin reported similar findings from a study of 200 autopsies on Okinawans.12
e: Mongols: He confirms they did not eat wheat much. And a study of similar people (1920s): These findings suggest that the diet of these nomadic pastoralists of the Central Asian Steppes was almost exclusively animal based, virtually devoid of grains, legumes and refined carbohydrates. This should make these populations also suitable to study the hypothesis that naturally raised animal foods protect against cardiovascular disease. However, not only did Kuczynski observe that these nomadic pastoralists suffered from high rates of obesity and gout similar to the Mongols of the 13th century, Kuczynski’s observations further extended to the diagnosis of cardiovascular disease and other dietary related disorders. Kuczynski asserted:
They get arteriosclerosis in an intense degree and often at an early age as shown by cardiac symptoms, nervous disorders, typical changes of the peripheral vessels, nephrosclerosis and, finally, apoplectic attacks. Even in men thirty-two years old I frequently observed arcus senilis.32
f: Javanese (1916). Note these are described as “vegetarian” but at the time, that commonly meant what we call now “ovo lacto vegetarians”: Pursuing this clinical impression, he reviewed 10 years of admissions charts and found only 5 cases of acute gallbladder disease among many thousands of patients passing through the medical wards and only 1 case on the surgery service among 70,000 admissions surveyed.
Following these observations, de Langen stated in regards to the rarity of vascular disease among the Javanese that:6
thrombosis and emboli, so serious in Europe, are most exceptional here. This is not only true of internal medicine, but also on surgery, where the surgeon needs take no thought of these dreaded possibilities among his native patients. Out of 160 major laparotomies and 5,578 deliveries in the wards, not a single case of thrombosis or embolism was seen.
http://healthylongevity.blogspot.com/2013/10/Cardiovascular-Disease-in-Ancient-Civilizations.html
http://healthylongevity.blogspot.com/2012/11/traditional-diets-in-asia-pacific-and.html
——————-
So anyway, Bryan and Morgana, you may be right: a number of diabetics might have been pretty high all along. Still no particular connection with carbs though. He doesn’t get into the fact that *vegan* diets can also cause heart disease, or that fish is rather amazing, so there is a bias there. But he seems to have some good pre-modern sources for dietary and disease details.
heathertwist- Well yes, those links you posted I found incredibly biased. It was obviously a “plant based person” with an agenda, so I’m afraid I couldn’t take them seriously. And much of the information went against other things I’ve read, so yeah….I take it with a grain of salt, sorry.
The “impaired glucose response” that Steffansen (I always forget how to spell his name) and Karsten experienced was a temporary Physiological Insulin Resistance, which is different to diabetes. It’s what I always say, “use it or lose it”. If your body is not used to eating carbs, it ramps down its insulin production. But a few days of eating mixed meals will change that back again. The body tends to get accustomed to whatever it is you normally do. I don’t think it was a sign of illness; the doctors observing them concluded they were healthy.
Last thing: I think you may be confusing “Aspies” with “Geeks”? Someone can be a geek without being an Aspie. There are highly intelligent people out there who are also good inventors, scientists, architects, artisits, etc., who aren’t necessarily Aspie They may even be introverts and prefer solitude, or might even be eccentric, but that doesn’t make them Aspie. There is a certain criteria for diagnosing someone with Asperger’s syndrome based on social impairments, repetitive behavior, along with several other factors. I think it’s a bit confusing because many people have speculated on which historical or famous people “might have had Asperger’s”; however, we don’t really know about that. Of course, there may have been Aspies in ancient Egypt for all we know, but I don’t think every inventor or architect was an Aspie! It could be that there were Aspies in hunter gatherer cultures too, who knows? It may not even have anything to do with wheat- (or: another theory: what if in some susceptible people, wheat causes an “autistic like” state that dissipates with the cessation of wheat eating? This may be different from someone who really is autistic. This is just pure speculation on my part). I think, like with so many other things, we don’t know enough about it yet.
“Well yes, those links you posted I found incredibly biased. It was obviously a “plant based person” with an agenda, so I’m afraid I couldn’t take them seriously. ”
HE is biased, but the sources he is quoting are wonderful! The HORUS study looks at mummies, which is about the best and non-biased info you can get. The authors of HORUS didn’t actually make any conclusions at all, except that “heart disease has been around forever”.
Anyway, if we start tossing out info that doesn’t agree with our worldview, then we are just as biased as we claim everyone else is. A person’s motivations aren’t important if the information is accurate.
“But a few days of eating mixed meals will change that back again. The body tends to get accustomed to whatever it is you normally do. I don’t think it was a sign of illness; the doctors observing them concluded they were healthy.”
I agree. And I think the reverse is true too: the cultures that ate, say, lots of sweet potatoes were probably adapted to them, and there isn’t a reason to think they must be diabetic from all the sweet potatoes. Some of the high-protein type writers who thought they couldn’t handle carbs … are deciding that resistant starch works just fine for them. So maybe people are lightening up a bit!
” I think you may be confusing “Aspies” with “Geeks”?” — I’m thinking in the sense of the book, “Geeks, Freaks, and Weirdos”. There is a certain conflating of geeks and Aspies. I actually prefer the term geek, because “Asperger’s” is technically a *diagnosis* … it’s saying there is something wrong with the person. I don’t think it’s a “wrong” … I think it’s a brain type. The geek brain is built more like a race car, with close tolerances and the ability to go very fast. But it’s not as rugged as say, a pickup truck.
I tell this to my kids. Muck that a pickup truck can handle, will ruin the sports car. Loud noises, stress, etc. are harder on geeks. And problematic foods … notably wheat … can cause a total meltdown in a geek where an NT just plows right through. I think wheat affects NTs too though … it causes maybe more anxiety and anger, which might be why the non-wheat-eating cultures come across sometimes as more “laid back”.
I’m also not clear that geeks are less “social” in general. When I go to a programmer’s group, everyone has a whole lot of fun and we socialize like mad … even though a lot of the individuals have a reputation for being unsocial at work. It’s just that socializing with NT people is stressful. “Gorilla Nation” is a wonderful book about that. The person could not manage to socialize with people, but she made friends easily with the gorillas, and eventually became a PhD and gorilla expert, having learned from the gorillas how to handle humans.
heathertwist- I had a closer look at the link by the vegan guy. The problem is, he writes a lot of stuff and “quotes” information, but doesn’t provide links, which I find suspicious. There was no link to the Horus study (that I saw)- so I looked it up. This study is only on Egyptian mummies- (duh: I should have figured it out since it’s called the Horus study, ha!). The huge confounding factor is that the Egyptians ate a high carb diet. It’s true that the nobility ate more meat than the poor people, but they also lived longer- (atherosclerosis is a process of aging; more on that later). In addition, they probably also ate more sugar (in the form of honey, fruit, dates, etc.). I might hasten to add that they also probably ate more fish. There is no mention of any other skeletons, so we’re only talking about Egyptians here.
In addition, it looks like atherosclerosis is probably a natural part of aging. Both Nina Teicholz and Gary Taubes talk about this in their books. We actually had this discussion somewhere on this comment section already. Not everyone with atherosclerosis has a myocardial infarction and dies; the lesions have to become unstable and “break off” essentially, causing a blockage. So it’s unclear anyway that these people were dying of heart attacks. Also, the mummies and skeletons with “more” athersclerosis could have been older skeletons, and in some of the other groups of people (like the Inuit) I don’t believe the ages were mentioned.
I don’t think I’m disregarding evidence that doesn’t fit with my world view. The problem is, I need strong scientific evidence to convince me, and I just haven’t seen that. In fact, many of the low carb promoters use the Horus study as evidence that a high carb diet is unhealthy! I would not go so far as to say that either, but it’s clear that there’s not enough evidence to implicate meat *or* low carb.
Heck, “they” don’t even know exactly what causes heart disease yet, or how exactly it happens. So we can’t really jump to conclusions before having the proper information.
Morgana, @heathertwist — Sorry to not post recently, but I’ve been attending to a matter of the (metaphorical) heart. But I’m here and reading everything you put up. –Bryan
“Also, like with Pottenger’s cats, I think it’s a problem that accumulates with generations, so the tendency is for it to get worse by generation; fetuses are affected by what the mothers eat, and so forth.”
Yes! And the interesting thing about the cats is that they HAVE figured it out, and it has to do with taurine. Which gets depleted when the cat is fed cooked meat. *Cooked* meat gloms onto the taurine in a way that it doesn’t get re-absorbed. I don’t know if cooked fish does the same thing! But for cats, they need either raw meat or extra taurine in their diet. Otherwise, the poor cats get the “diseases of modern civilization”. Heart disease, diabetes etc … for cats, they get it simply by lacking taurine.
It seems the mama can passes on taurine to the kittens in the milk, and en utero? So by the third generation it’s gone totally?
If the answer for humans turns out to be taurine, that is GOOD NEWS because it’s an easy thing to add to one’s diet.
heathertwist- when I mentioned “Pottenger’s Cats”, what I meant was “how does that relate to humans”? So I was talking about glucose control as a generational concept. For instance, I think it’s pretty well established that mothers with insulin resistance, who eat a high sugar diet while pregnant, will tend to have children with metabolic problems. This is one of my theories about the soaring diabetes rates today, and oddly enough, nobody really seems to be looking much at the generational aspect! Of course, your theory about taurine might also be the key, or one of the keys to the puzzle- (as possibly magnesium and vitamin D as well). Unfortunately, the trend is to look at diabetes as isolated cases, and to blame the individual.
“I definitely, generally do feel “calmer”, but it’s hard to say if that’s due to stopping wheat, or if it’s due to the fact that I live alone now and have time in my schedule to be at home alone for certain periods of the day, between work.”
Yes, I think that makes a huge difference too. And being able to take naps when I feel like it. I felt the best when I was eating mainly salads and fish … there is something about fresh greens and vinegar that is sort of magic. I guess my salads were low-carb-ish, but I had rye crackers with them too (it was pre GF). Also on the cruise ship: I was eating plenty of rice and rice noodles, but felt great.
I had to stop dairy too though, before my thinking really cleared up. Dairy does something weird too. It does seem to cause leaky gut in some people.
heathertwist- I already did go through a long phase of eating both gluten and dairy free- (my mostly vegan phase). I actually had to stop dairy for a time, due to damaged villi from celiac disease; my body wasn’t making lactase, so I couldn’t digest it for awhile. I was still eating a high carb diet at that point- (actually, very high carb! Mostly carbs). I never had the problem that my thinking “wasn’t clear”; I’ve heard people claiming to have “fuzzy thinking”, but I’ve never had that- (I’m not sure what it is exactly. Is it like being drugged?) The problem I had was a social problem, a problem of being “inaccessible”. I felt like I was buried inside myself, and it was terribly hard for me to feel any desire at all to relate to people. Actually, I felt fine within myself, it was just very hard to go out into the world; it was like I was in my own little box. Once I lowered my carb intake, it became much easier for me to relate to other people. Actually, what might have helped too was eating more fat; hard to say if it was fewer carbs or more fat, but I think it was both! When I eat too many carbs again, I start feeling not so good, both mentally and physically. I do eat dairy again now (fermented sheep and goat) and feel fine (mentally as well), so I don’t think dairy is the issue, with me at least.
” Actually, I felt fine within myself, it was just very hard to go out into the world; it was like I was in my own little box. Once I lowered my carb intake, it became much easier for me to relate to other people. Actually, what might have helped too was eating more fat; hard to say if it was fewer carbs or more fat, but I think it was both! ”
Sure. And you also know that for some reason your body doesn’t handle glucose well (hence the diabetes). My belief is that if a person is healthy, they can handle glucose just fine. And they can handle cholesterol just fine. And fat just fine. But if their body lacks whatever it takes to process those foods, then they end up with fatty arteries or fat bellies or diabetes or whatever.
It’s also true though that starches tend to turn up the serotonin levels, which makes people calmer (or sleepier!).
“The carbohydrate-serotonin connection has a direct impact on our emotional state, too. Drugs that increase serotonin activity have been used for several decades as a therapy for mood disorders. However, our studies showed that natural changes in serotonin could have a profound impact on daily fluctuations in mood, energy levels and attention.”
https://www.psychologytoday.com/blog/the-antidepressant-diet/201008/serotonin-what-it-is-and-why-its-important-weight-loss
For handling cholesterol, taurine might just be the key. Could be for diabetes too. Or at least that’s the experiment I’m doing right now. I can say that my thinking has gotten a lot more clearer since I started taking the taurine. I can see why they added it to the energy drinks!
Some specific foods might muck up the works … like cooked meat keeps cats from processing taurine correctly. That’s one reason I’m looking at the mummy info. If cooked meat (or the type of fat in meat) leaches taurine from the system for humans in the same way it does for cats, then that would explain a lot! And also be a solvable problem.
heathertwist- I think you have me confused with someone else! I don’t have diabetes at all. As far as I know, I don’t have any blood sugar issues either. My body does not handle carbs well for other reasons. I had loads of health problems on a high carb diet, most notably stomach/digestive issues. But many other little niggling health problems cleared up as soon as I went low carb. I’m sure wbryanh would tell you the same thing. A high carb diet is not for everybody, just like a high fat diet is not for everybody. I am also a person who does NOT do well on a vegan diet; some people may thrive on that diet, not me. I definitely need to eat enough fat. More information on individual diets later…..
Sorry, my error! I did probably get the emails mixed up.
BTW, the HORUS study is available online. It does talk about the probable diets of the four populations they studied (as mummies). It’s very interesting!
Click to access finch1.pdf
I hope we get more hard information like this, rather than a lot of speculation.
heathertwist- thanks for the Horus study link; I wasn’t able to find that online, but just a shorter version, where they only mentioned Egyptian mummies. There was also no mention of diet in the link that I was able to find, so this was helpful.
I’m assuming you’ve read the whole thing; which means you must have seen the very last sentence, the conclusion they came to: “the presence of atherosclerosis in premodern human beings suggests that the disease is an inherent component of human aging and not characteristic of any particular diet or lifestyle”. So, like I said, this vegan guy was biased. I rest my case.
heathertwist, wbryanh- below is a link that I thought was interesting, mainly because it says that the diet that’s best for you may be your own ancestral diet; i.e., what your great great great grandparents ate (before processed food). This might partly explain why we have evolved to eat different diets, depending on where we’re from: why some people can handle carbs better (or worse), or meat, etc. (The part about the people from Crete and olive oil is very interesting). I don’t agree with absolutely everything in this article- (they interview different people), but I like the general gist explaining why some diets might work better for some people, and other diets for others:
http://www.macleans.ca/society/health/eat-like-your-grandma-why-you-should-skip-the-kale-salad/
“The problem is, he writes a lot of stuff and “quotes” information, but doesn’t provide links, which I find suspicious. ”
??? He has links all over the place. They are the numbers interspersed with the words.
——————–
“This might partly explain why we have evolved to eat different diets, depending on where we’re from: why some people can handle carbs better (or worse), or meat, etc.”
I’d largely agree with this … there is a huge genetic component. However there’s no guarantee that your great-great-grandmother was actually in good health. Some populations did way better than others. And that is still true.
I think this is part of our “people were healthier in the old days” bias. We have zero evidence for that. In some times and places, people living the traditional life live younger … like the Yuzus. In other places, they didn’t, and lost their teeth etc. at an early age. Oetzi wasn’t in great shape for his age, albeit he was probably eating his ancestral diet.
———————
“In addition, it looks like atherosclerosis is probably a natural part of aging. Both Nina Teicholz and Gary Taubes talk about this in their books.”
And yet, some populations get more heart disease than others. That’s what interests me. The Mongolians get it at a very early age: the Japanese didn’t. Why? The Japanese are quite motivated to figure that out, because I’d imagine they don’t want to start aging like everyone else.
In their case, it’s NOT genetic … when they live elsewhere and eat the local food they start getting problems.
“Among Japanese, men living in California had the highest age-adjusted prevalence of CHD, with 10.8 cases per 1000, followed by Japan (5.3) and Hawaii (5.2). Californian Japanese also had the highest prevalence of angina pectoris (25.3 per 1000 men) and possible infarction (31.4 per 1000 men). [3]”
http://www.epi.umn.edu/cvdepi/study-synopsis/nihonsan-study/
——————-
“In addition, they probably also ate more sugar (in the form of honey, fruit, dates, etc.). I might hasten to add that they also probably ate more fish. There is no mention of any other skeletons, so we’re only talking about Egyptians here.”
Yes, they mention the other skeletons. The picture of the Unangan woman is especially interesting … she was 25-29 years old but her teeth were a mess. I do wish they showed more of the skeletons. Some of them had perfect teeth and really great bones: others did not.
———————–
Oddly enough, the Egyptians (the mummies anyway) appeared to not have eaten much fish:
“The real mystery is the fish. Most people would probably expect the ancient Egyptians living along the Nile to have eaten loads of fish. However, despite considerable cultural evidence, there seems to have been little fish in their diet.
“There is abundant evidence for fishing in Egyptian wall reliefs and models (both spear and net fishing), and fish shows up in offering lists. There is also a lot of archeological evidence for fish consumption from sites such as Gaza and Amama,” said Spence, who added that some texts indicated that a few fish species were not consumed due to religious associations. “All this makes it a bit surprising that the isotopes should suggest that fish was not widely consumed.””
https://www.insidescience.org/content/what-did-ancient-egyptians-really-eat/1630
Oddly a similar thing happens in Britain. Despite living not far from water, the Britons gave up eating fish when they started farming. And among the paleo/low carbers/WAPF groups, there don’t appear to be many fish eaters either. Why?
———————–
I haven’t found any ancient studies on fish-eaters yet. There are some from the 60’s and 70’s.
heathertweist- I saw the numbers on the post written by that vegan guy, but when I tried to click on them nothing happened. Usually the number takes you to the link- (unless he listed them at the bottom, but I don’t remember seeing them. Maybe I looked at it too fast). In any case, I don’t really trust his conclusions, sorry.
As for studies of ancient diets and fish eaters: in that Horus study you sent me, where they listed the diets, according to them all of the groups of people with atherosclerosis were fish eaters, including the Egyptians. (The recent link you sent me about the Egyptians being vegetarians seems to have come from another study? There were 45 mummies in that study, but they don’t say- at least I didn’t see it- whether they were nobles or peasants. My point was that the nobles probably ate more fish than the peasants; the peasants might very well have been vegetarian! I don’t think we can conclude from 45 mummies that absolutely all Egyptians were vegetarians; it seems unlikely, especially since there is other evidence that they ate fish). In any case, the Horus study does mention fish in their diet, along with other animal food. And the Unangans (the hunter gatherer group they studied, but only 5 skeletons)- ate a mostly marine based diet, including fish and shellfish.
“As for studies of ancient diets and fish eaters: in that Horus study you sent me, where they listed the diets, according to them all of the groups of people with atherosclerosis were fish eaters, including the Egyptians. (The recent link you sent me about the Egyptians being vegetarians seems to have come from another study?”
I haven’t seen any serious studies about ancient Egyptians being vegetarian. Some people believe the poorer people were, but it sounds speculative. The richer people certainly weren’t.
None of the HORUS populations were vegetarians that I could see. The Peruvians might have been the closest (lots of corn and beans). But they also didn’t have a fish-based diet … the Inuit did a lot of sea-mammal meat plus some fish.
Anyway, I’m still looking for examples of a verifiably healthy long-lived mammal-meat-based culture, and so far I haven’t found any. With or without grains. We do have some examples of tuber or grain-based long-lived healthy people, and some of grain/fish-based people.
““the presence of atherosclerosis in premodern human beings suggests that the disease is an inherent component of human aging and not characteristic of any particular diet or lifestyle”.”
I don’t think the HORUS people were vegan, though for sure it’s getting quoted by vegan people! But I don’t agree with the study’s conclusions either. We already KNOW that some diets produce less heart disease.
Again, maybe we are all doomed to get heart disease eventually. But the point of these really super-low-fat vegan diets recently is that they appear to get rid of artery fat … and if they do, then we should figure out WHY. I for one would rather not go super-low-fat. But since the ones doing the research on VLF tend to be vegans for political/emotional reasons, they aren’t doing the research to think of other reasons why it might be having the results they are getting (or what the side effects might be).
heathertwist- I’m a bit confused as to why you sent me that link in the first place…..in your own link, it was claimed that “Egyptians were Vegetarians”. I don’t think that was speculation, I think they analyzed the skeletons? (Unless there were shortcomings to their analysis, always possible). My own quip was that they didn’t look at enough mummies to make the assumption that *all* Egyptians were vegetarian- (or, for that matter, that *no* Egyptians ate fish).
As to the Horus study: no, I strongly doubt that the authors of the study were vegan. However, they were quite scientific in analyzing their data, which was what I liked. If you looked at their data, it was absolutely clear that the older skeletons had more atherosclerosis, and the younger skeletons had less (or no) atherosclerosis, so I would definitely agree that age seems to be a pretty strong factor! And as they all ate different diets, I would also agree that diet doesn’t seem to be a factor- (as far as we can tell). So, I would agree with their conclusion. It’s only certain vegans who would extrapolate from that that the “vegan diet is better”, but this is unscientific, and frankly, why I had problems with that original vegan link you posted. I preferred the actual study itself.
I haven’t seen enough proof that a vegan or vegetarian, or low meat diet “prevents” heart disease, as vegans and vegetarians seem to be getting the same- (or sometimes, more)- heart disease as other populations (just one example here):
http://naturalsociety.com/new-study-suggests-vegetarians-less-healthy-meat-eaters/
As for the very low fat diets that Denise wrote about: some people on this blog already made the point that those diets either severely limit, or omit completely, vegetable oils, margarine, and fake fats. It could be that it’s not “fat” that causes the problem, but certain types of (processed) fats. So, yeah…..a low fat diet would help in that sense. I’m not convinced that it’s necessary to eliminate all fats, and in my own case, that causes health problems: I already know, because I’ve done it!
Another point I’d like to make is that there may very well be factors related to heart disease other than diet. For instance, stress! Maybe some of the populations who have less heart disease experience less stressful lives. In the case of Genghis Khan’s armies, I would imagine that that would have been a high stress life. Another point, which the authors of the Horus study mentioned, was infection.
In any case, I’m going to leave this particular discussion. I’m going to be busy this coming week and I don’t have time anymore to keep quibbling about this. I thought we already mentioned some traditional meat eating cultures who are/were healthy- (the French, the Swiss, the Spanish, the Plains Indians, the Australian aborigines)- so I’ll leave it at that.
“Anyway, using Otzi as an example of a “native diet” is not really apt; Otzi was an example of what the switch to farming and grain eating did to the human body. In fact, many proponents of the Paleo diet use him as an example of what the wrong diet can do to you! ”
The article said it was best to eat whatever your great-grandma ate. Otzi’s grandma likely ate the same diet he did, and even further back than that. Ditto for the Egyptians. And the Mongolians. They’d been eating the same diet for hundreds or even thousands of years. So the question is: “How long does it take to adapt”? If no one has really adapted to a farmed grain diet YET, then the “eat like your great-grandmother” theory doesn’t wash.
Well, maybe we’ll all be adapted in ANOTHER 10,000 years?
Also by that logic, there should be SOME mainly-meat-eating culture that has adapted and should be healthy. I agree that there is a lot of adaption … the Sardinians for example, and the Japanese are adapted for seaweed. But most people get healthier on a Japanese or Sardinian diet anyway, even if they aren’t particularly adapted. Therefore, while paying attention to what you ancestors ate is certainly useful, it’s not an absolute, unless your great-grandparents tended to be centenarians and were in great health.
And yes, with heart disease it definitely shows up in later age, though in the mummies some of it showed up in the 30’s, which is pretty young. Point is there are places where it does NOT show up much at all, and where people routinely live past 55 … even in the distant past. HORUS only mainly mammal-based foods though … I’d like to see one on a fish-based culture, esp. one featuring shellfish. For instance, the Chinese building the railroads were notably healthier than the Irish, and there were a number of good habits the Chinese had. But one thing might be that one of their main proteins was dried oysters
http://web.stanford.edu/group/chineserailroad/cgi-bin/wordpress/faqs/
“in your own link, it was claimed that “Egyptians were Vegetarians”. I don’t think that was speculation, I think they analyzed the skeletons? ”
You mean this one:
https://www.insidescience.org/content/what-did-ancient-egyptians-really-eat/1630
You are right, it does talk about vegetarian diets. Which is a bit misleading because “vegetarian” and “vegan” are technically different, and they didn’t specify. Mostly what I’ve read about that study in the past was that it notably didn’t include FISH, which is what you had mentioned: you said they were probably eating a lot of fish. But anyway, I think we both agree the ancient Egyptians weren’t HEALTHY, even though they ate the same diet for a rather long time.
“I haven’t seen enough proof that a vegan or vegetarian, or low meat diet “prevents” heart disease, as vegans and vegetarians seem to be getting the same- (or sometimes, more)- heart disease as other populations (just one example here):
http://naturalsociety.com/new-study-suggests-vegetarians-less-healthy-meat-eaters/”
Well yes, I agree, which is where this thread started out. Mainly for me, because the vegan diet lacks taurine (and B12) for starters. So how do people like the Yuzuharians even survive? I’m not promoting their diet as a cure, because yes, it is very difficult to make veganism even work. But when it does work, it’s worth figuring out what is going on.
“I thought we already mentioned some traditional meat eating cultures who are/were healthy- (the French, the Swiss, the Spanish, the Plains Indians, the Australian aborigines)- so I’ll leave it at that.”
Yes, it is a bit of a time sink. But no, I still haven’t found any actual science that supports “healthy meat-based diets”. The French and Spanish eat a lot of seafood, including shellfish. The Swiss eat a lot of dairy. The aboriginese traditionally ate a lot of fish too, plus stuff like molluscs and insects. To me it’s looking like taurine/arg/gly (and maybe Vit C, as Jonathan suggests) are going to turn out to be the keys to the puzzle.
I agree the “eat like your grandma” theory doesn’t wash. There is a basic flaw to this line of thinking, namely, most people are not pure “whatever strain your grandma was”. Even before the industrial age made humans more mobile, there were mixtures, as folks are finding when they get genetic testing done. So, does my friend eat like his great-great granny, a slave whose parents were from West African AND central African stock (originally eating different diets)? Or like his great-great grand-daddy (his ggm’s master), who was of Anglo-Irish stock? Next, the child of this union, his great grandmother, now a free young woman of West African-central African-British-Irish stock, marries a Native American man, whose father was Plains Lakota and whose mother was coastal Narragansett. Their daughter (his grandmother) eventually migrates to the Bay area of CA and marries a man of Chinese-Vietnamese descent. Their daughter (his mother), now West African-central African-British-Irish-Plains Native Am- Coastal Native Am-Chinese-Vietnamese, gets a scholarship to University of Hawaii at Hilo, starts getting interested in her Native American roots, joins an activist indigenous student group, where she meets and marries a Native Hawaiian. Now, their son (my friend) has to decide which “ancestral” diet to follow. He could end up like the proverbial centipede that lost the ability to walk when he “lay pondering, in a ditch, which leg came after which”. As another commenter said, food gets broken down into relatively simple components in the body. Some traditional diets are better at supplying some components than others. But, still, whatever food you eat has to get broken down into those components to digest and contribute to your well-being. Thinking about this has made me hungry. I think I’ll call my friend and see if we can get some West African-central African-British-Irish-Plains Native Am- Coastal Native Am-Chinese-Vietnamese-Hawaiian-American take out for dinner. Organic and locally-sourced, of course.
” As another commenter said, food gets broken down into relatively simple components in the body. ”
Yes! Some people have created the “broken down” version for people to pinpoint allergies etc. (Alpha nutrition) or to simplify life (Soylent) or to feed people in a coma. Probably none of them are really “complete” yet, but they are getting better and better. And so people in a coma or unable to “eat” can remain alive for decades. By the time the food is digested, it’s ideally something really simple: like amino acids, glucose, and lipids, and some vitamins and minerals. A lot of the genetic changes have to do with how to digest foods into their simpler version.
“I think I’ll call my friend and see if we can get some West African-central African-British-Irish-Plains Native Am- Coastal Native Am-Chinese-Vietnamese-Hawaiian-American take out for dinner. Organic and locally-sourced, of course.”
🙂 Maybe someday you’ll just register your gene print and the restaurant will know that your pizza should be gluten-free, cheese-free, and heavy on the fermented fish paste, with a side of poi and a dish of roasted peanuts!
heathertwist- the whole point of that article I posted was that the diet that you’re genetically adapted to would be the best diet for you; in other words, copying the diet of some other long lived folks halfway across the globe might not have the same effect. This point was made in the article in the example of Northerners trying to copy the Crete diet; their bodies were not genetically adapted to process all that olive oil. Your link of Japanese men who had worse health after moving to the U.S. just proves that point! Of course, one might also argue that the Americans weren’t healthy either, but have we really fully adapted to our modern diet of processed food, vegetable oil, soy, white flour, and other foods that are ubiquitous now, but not in the past?
On the same vein: one of the theories out there as to why the Mediterraneans are healthier is that they’ve had a longer time to adapt to that diet- (the “fertile crescent”, which is the place where grain eating began). Some say- and I think this is an interesting concept- that, through years of grain eating, they’ve slowly made adaptations (as well as the possibility that the people who couldn’t tolerate it eventually died out) to be able to thrive on that diet. Maybe they already had all the diabetes, obesity, heart disease, etc., that we’re experiencing now (that study with the Egyptian mummies seems to confirm this point). Since grain was introduced to Northern countries later, maybe this is why many of us are struggling now. (This also would explain why many native cultures, like the Inuit, Plains Indians and Aborigines- who traditionally ate mainly non-grain foods- are even worse off). Of course, our modern day high sugar usage is another factor in all this.
Anyway, using Otzi as an example of a “native diet” is not really apt; Otzi was an example of what the switch to farming and grain eating did to the human body. In fact, many proponents of the Paleo diet use him as an example of what the wrong diet can do to you! I’ve read it’s pretty much of an established fact that the switch to farming caused huge health problems and worse life expectancy- (which eventually improved, actually). And this from Paleontologists, not from nutritionists who might be biased or have an “agenda”.
“atherosclerosis is probably a natural part of aging”
I really doubt that http://www.ncbi.nlm.nih.gov/pmc/articles/PMC55170/pdf/pnas01048-0325.pdf – atherosclerosis did not occur in guineau pigs (who like us cannot make vitamin C) when adequate vitamin C was given.
People too maybe: “We studied 55 patients with various degrees of coronary heart disease. Changes in the size of the coronary artery calcifications in each patient were measured over an average period of one year without vitamin supplementation, followed by one year with … the fast growth of coronary artery deposits was slowed during the first six months and essentially stopped during the second six months” http://www4.dr-rath-foundation.org/pdf-files/why-book/whybook_02_sep2003.pdf
Being insulin-dependent for 35 years, my doc expected rampant atherosclerosis – C and glucose are very similar and rely on the same transporter to enter the cell, so diabetics with their high glucose levels have lower intracellular C – yet I have a zero calcium score and therefore zero atherosclerosis. The only thing I did different was to take copious C …
“I really doubt that http://www.ncbi.nlm.nih.gov/pmc/articles/PMC55170/pdf/pnas01048-0325.pdf – atherosclerosis did not occur in guineau pigs (who like us cannot make vitamin C) when adequate vitamin C was given.”
Oooooh, and get this:
“Normally our bodies manufacture taurine rather than obtain it from our diet. It is produced by a combination of cysteine, methionine and vitamin C, but low amounts of these substances can in turn lead to taurine deficiency.”
http://www.smart-publications.com/articles/taurine-protects-heart-eyes-and-improves-glucose-tolerance
So guinea pigs use glycine for bile, and don’t get any taurine in their diets I think, they must manufacture it. In theory humans can produce it also, but it appears in real life humans don’t produce it very well and in many countries people are short on Tau. And damaged hearts tend to be low in Tau (and get better with Tau added to the diet).
And that might be what worked in the Rice diet too! They ate mainly rice, but they also ate fruit, so they’d be getting a fair bit of Vit C I think (and sulfur, from dried fruit, probably). Ditto for the other VLF folks … they tend to be diets high in Vit C, and low in taurine usage (taurine tends to get used up digesting fats or combining with cooked meats?).
Vitamin C also helps produce other ‘-ines’ that keep hearts and collagen healthy:
https://www.drlam.com/blog/vitamin-c-therapy-in-cardiovascular-disease/803/
Jonathan Christie- interesting links! Of course, when I made my comment about age and atherosclerosis, I was referring to old mummies and skeletons of the past, who did not have access to vitamin C pills- (I’m not sure if you saw the whole conversation). And it’s hard to know exactly how much C they were getting in the diet. But, the fact that you’ve found a solution that seems to be working for you is great! I’ll remember this information in case I need it someday.
I see this as also a (possible) confirmation that atherosclerotic plaques may have more to do with sugar than with fat- (as “experts” disagree on what exactly causes it).
1. T2D: “We simply can’t say what level of problem T2D was through the centuries and millennia, going back to the Ag Revs.”
??? Why not? We can tell from a skeleton how much weight the person carried, and we know that where there is obesity there is probably T2. For instance, they can tell now that monks brewing beer were fat, while monks brewing brandy were not.
http://www.theguardian.com/uk/2004/jul/15/highereducation.artsandhumanities
I haven’t read about obesity during the Ad Revs, but it certainly was a problem for the Romans and Egyptians. Wheat does seem to be associated with obesity. I haven’t seen anything like that for millet or rice though. The Chinese do appear to be MORE sensitive to T2 when they start eating certain foods though, so they aren’t esp. adapted to “carbs” in general. Ditto for the Japanese, and their health tracking system is darn good.
It seems that the Japanese and Chinese are both more prone to getting diabetes NOW, but weren’t on their traditional diets. It does seem to be related to fructose (but not raw fruit):
http://www.cbsnews.com/news/rising-type-2-diabetes-rates-linked-to-increases-in-high-fructose-corn-syrup-consumption/
Which makes sense. Wheat starch is half fructose, half glucose, while rice is glucose-glucose.
Or that wheat and barley are used to make beer a lot!
2. Farming: I like Jared Diamond a lot! And mostly I agree, esp. in situations where people have ONLY grain to eat or they over-populate (which was a big problem in the Americas). The rice or yam based cultures in Asia and the Pacific did really well though, in terms of health, esp. for the upper class. The wheat-based cultures didn’t do well though, even for the wealthy, and you have folks like Queen Victoria and Henry 8 that were quite ill and very fat. Gengis Khan too … and he certainly got enough exercise. Fat Japanese? That is soooo rare these days, and in history. Except the sumos, but they got a special diet (which, BTW, features more beer and beef …).
3. T2: “From atherosclerosis to the glycating and cross-linking of parallel long-strand proteins in collagen causing them to “lock up” hence tendon stiffness, to retinal degeneration to impotence, just to name a few of its very many effects. Until very recently, we attributed these effects to a multitude of other causes. We usu summed up all these causes as “aging” and “life.””
All of which, oddly enough, are the symptoms of Tau deficiency in cats! Cats eating a pure meat diet even, if the meat is cooked.
4. Celiac: “Heather this suggests that gliadin epitopes *do* in fact directly contribute to coeliac lesions”
I agree, and that’s probably one reason why there ends up being an anti-TTG issue. But in the definition of “celiac”, the anti-TTG reaction is the one they usually go by. A lot of people that are considered “non-celiac” do have anti-gliadin IgA antibodies, but that doesn’t count for some reason. My understanding is that the gliadin gloms onto the villi in everybody, and for some reason that’s not considered a problem. Even if your body mounts an immune response. It’s only a “problem” if it actually causes lesions and you also have the anti-TTG thing. Maybe that is changing. The last gastro I had said that if you have celiac genes, and stopping wheat makes you feel better, then you are celiac by definition (his definition anyway).
And I agree that the nomenclature is just really slack. There are certain peptides that are considered the “problem” with gliadin, and those are found in barley and rye too, but then there are peptides in other grains that cause issues for celiacs and other people too. I think maybe the only really safe grains are the ones without much protein at all (white rice! Yay!).
Heather, @morgana, allo again…
Heather you ask:
“??? Why not? We can tell from a skeleton how much weight the person carried, and we know that where there is obesity there is probably T2…”
That’s just it, we can’t assume it’s only “diabesity.” Far from it. Look at the scads of Indians and Chinese, thin as rails and losing limbs to deep T2D. You mention Romans and Egyptians but I’d be very surprised if we found much obesity at all among the plebes way back when, and they represented 99++% of society. Yet does that mean they were T2D free? Or did they suffer a lot of T2D anyway? We can’t say for sure. I know of no skeletal or dentition or any markers to verify the presence/absence of T2D, except maybe in the few mummies, and they were almost always remains of elites which likely did have some level of the metabolic disorder.
We *know* a global T2D pandemic rages today. Trouble is, we assume it wasn’t a problem before. I always hear “T2D practically didn’t exist until the SAD.” I’m not so sure! Since the Ag Revs, T2D may have been considerably worse and more prevalent than we commonly assume. But only now are we able to even begin to take the true measure of it.
I suspect as you say Heather, it was worse for the wheat eaters as they had to contend with, in addition to carbs, additional confirmed and conditionally inflammatory agents such as gluten, hemoagglutenating lectins, and phytic acid. But it wouldn’t surprise me at all if BG levels went up everywhere in the civilized world after the Ag Revs, maybe considerably even pathologically so for Asians with their “thrifty” genes.
The Ag Revs preceded writing systems by almost 7000 years. Ag was widespread by the time the Sumerians started to stab their styli into clay tablets. We have little history of peoples who traditionally eat VLC-VHF–the shoreline Inuits the great exception. With my 80% fat, 15% protein, 5% carb foodway, I still do feel like an explorer heading ever deeper–8.5 years and counting–into barely charted territory. And maybe back through the mists to the pre Ag Rev time. “2007: A Foodway Odyssey.”
Heather, what you say here:
“It seems that the Japanese and Chinese are both more prone to getting diabetes NOW, but weren’t on their traditional diets. It does seem to be related to fructose (but not raw fruit)…”
I’ll place bets that their highly industrialized toxic environments, esp in China, the most polluted place on Earth, play large, even major, roles here. Of course we find many other possible factors which include, like you suggested, a huge pop in fructose like in HFCS and yes, the trite but not entirely untrue “more food, less exercise” trope.
Btw, wheat is fructose-free. Wheat has two starches–amylose and amylopectin. Both glucose-only polymers.
If someone forced me to eat a grain, I’d choose rice over wheat every time. And I’d always choose sweet potatoes over either of them. –Bryan
“I’ll say right off, about Rowan, he may well be right about oxidized cholesterol being a contributing factor, but I have real troubles with him. To draw his conclusion–that oxidized oils drive our CVD–he takes an overly simplistic, crudely correlative, and thinly supported approach that lacks sufficient granularity.”
1. — Diet isn’t the only way to get oxidized Ch —
Yes, he seems to be all about diet. I’m not as concerned about HOW the oxidized Ch gets there … I quoted him because he brings out the point that the UN-oxidized Ch is not only harmless, it’s required by the body
As far as eating rancid oils or Ch goes, oxidized gross. Think burnt egg yolk. I’m going to assume that we here aren’t eating a lot of it. But there are about 10 other usual ways Ch gets oxidized. Plus it picks up toxins in the blood. Ch goes bad just keeping us alive. My interest is: how does the body GET RID of it?
2. — Now, it seems that only the LDL containing ox-Ch will attack the artery walls: —
“The initial association between cholesterol and cardiovascular disease was born out of the detection of lipid and cholesterol deposits in atherosclerotic lesions during the progression of atherosclerosis.14 Subsequently, studies have elucidated a role of LDLs in cardiovascular disease development, particularly the role of oxidized LDL (ox-LDL; LDL particles that contain oxidized fatty acids) in infiltrating and damaging arterial walls, and leading to development of lesions and arterial plaques.15,16”
http://www.lifeextension.com/protocols/heart-circulatory/cholesterol-management/Page-01
So you end up with the same question: why does LDL that is full of ox-Ch, going to the liver and then leaving again, going into a holding pattern and not getting rid of the ox-Ch?
3. — The liver gets saturated with LDL and sends it back out into the bloodstream.—
“HDL-D is converted to HDL-L as it collects cholesterol. Some of the cholesterol in HDL can be transferred to VLDL, IDL, and LDL, in fact, most of the cholesterol in IDL and LDL came from HDL in this manner. This is not bad as long as IDL and LDL are efficiently removed by the liver. Unfortunately, the liver is saturated with LDL at a level of 25 mg/dl (a level that most people have at birth) so that at the typical LDL levels seen in this country (120 to 140 mg/dl), much of this cholesterol is simply returned to the arteries (a bad thing). However, if HDL-L is functioning well, it will deliver this cholesterol to the liver instead of transferring it to IDL and LDL”
Understanding Lipoproteins
Click to access understanding-lipoproteins-old.pdf
4. — So how does the liver get saturated with LDL? —
First off, it seems the reason the Ch gets recycled is that there *isn’t enough to digest the meal*.
“Enterohepatic circulation
The bile salts present in the body are not sufficient to fully process the fats in a typical meal, thus they need to be recycled. This is achieved by the enterohepatic circulation. Specific transporters in the terminal ileum move bile salts from the lumen of the digestive tract to the intestinal capillaries. They are then transported directly to the liver via the hepatic portal vein. Hepatocytes take up bile salts from the blood, and increase the secretion of bile salts into the bile canaliculi, small passageways that convey bile into the larger bile ducts. 95% of the bile that is released to the small intestine is recycled via the enterohepatic circulation,while 5% of the bile salts are lost in the feces.”
http://courses.washington.edu/conj/bess/bile/bile.html
So this suggests:
a. LFHC diets probably don’t need so much bile, so there is no reason to recycle it.
b. If there is SO MUCH LDL in play in the average SAD diet, why isn’t there enough bile? Likely not enough taurine/glycine?
c. Recycling Ch is a normal process so …
d. There must be a way to prevent the bad-Ch from going back into circulation.
5. — This only applies to diets with lots of saturated fat —
And here is where it gets in to the fat wars!
a. LFHC: Not much bile needed. Plus they tend to be high-fiber diets, and bile gloms onto some fibers and is then not recyclable.
b. Coconut oil and fish fat: CO is technically saturated, but it doesn’t require much emulsifying. I noticed this in cleaning pans. Hardened beef or lamb fat requires major detergent. CO almost comes out with just hot water. Ditto for fish fat. Fish oil doesn’t require a lot of bile.
c. Beef and mutton fat: Tends to be tough to digest. Takes lots of bile. Now: under what circumstances is the bile recyclable?
6. — Sometimes Ch conjugates in a way it’s not recyclable —
So this is what happens with cats. If the diet has one type of protein, then the bile is recycled and the taurine reused. With another type of protein, the bile doesn’t get reused, and is degraded by bacteria.
So maybe that is in fact the usual case. The body wants to reuse Ch and Tau, but not bad-Ch. Maybe in the ideal situation, the bad-Ch gloms onto some other normal dietary factor and does not get reused, while the clean-Ch is reabsorbed along with the Tau as many times as is needed to digest a whole lot of fat.
——————–
“It could be we evolved an efficient system to cull out the corrupted Ch (using Tau?) that minimized the inflammatory process and thus the macrophage and/or high ApoB/LDL response. And why shouldn’t our bods immediately chuck it out? Our bods can easily make all the cholesterol it needs from the readily available Cs, Hs and Os at hand everywhere.”
EXACTLY! I’m thinking the liver might just chuck it all into the bile. And IF the bile hits some of whatever it is we traditionally ate is, the bad-Ch got glommed onto and went off to feed some bacteria. The good stuff got recycled.
I think with cats, the cat’s bile gets confused … oxidized meat isn’t something cats EVER encountered historically, so the combo of oxidized meat and bile works like oxidized bile and meat, and the result is none of the bile gets recycled. But bile plus raw meat … the oxidized fat part of either doesn’t get absorbed.
I also agree … our “traditional diet” was anything but pristine. A bit of oxidation was probably the least of the issues.
—————-
“I continue to find Tau very interesting, especially if it turns out we can’t always automatically make all we need via cysteine + methionine.”
This could be the answer to Denise’s question though. Perhaps we can make all the Tau we need for a LFHC diet (as long as there is some sulfur).
Maybe we mainly need more Tau when we get into HFLC territory, when the fats involved are the harder-to-digest ones. And maybe the meat needs to be more raw.
Or maybe (dare I say it!) we need more seafood in our diets …
heathertwist- Lots of great information in your recent posts, and very interesting; thanks! I was especially interested to read about the experiments on cats, and in addition to that it’s nice to know that sauteing my fish in olive oil won’t kill me, ha ha (because I do that sometimes too).
One thing I’m not sure I agree with though is the bile theory. The main reason is that I know people- (and this was true of myself too, back when I was on a low fat diet)- who have had bad issues with gallstones and gall bladder function while eating low fat. I’ve read a lot about gallstones, and there are two theories: one is the theory about too much fat in the diet- (which somehow gets “saturated” with cholesterol), the other theory is that sugar and refined flour cause problems with bile- (and I don’t remember the exact mechanism). Through my reading though it became clear that nobody really definitively knows (and some of the more professional people admitted “we don’t know”). I would question whether things like saturated fat in meat are “hard to digest”: for me, personally, animal fats and meat are about the easiest things to digest, and carbohydrates and sugars are the difficult things. Oddly enough, my digestion and my gall function both got much better after going low carb high fat. Some people say “use it or lose it”, so with that theory in mind, low fat diets may not be the best for optimal bile function (or digestive function) in my opinion. It’s personal, of course, but as I said I know many other people as well who had bad gall bladder function while eating low fat.
As for “recycling” bile, as with so many processes in the body (like cholesterol), it seems this is a normal function and not a pathology. Basically nothing in the body gets wasted, and everything gets reused if possible. Now your theory that damaged or oxidized cholesterol *should* leave the body (but doesn’t in some cases) is interesting; there might be something to that. I would also like to point out that the theory about “oxidized” cholesterol causing heart disease in the first place is still a theory as well. There are quite a few different theories out there, but not all experts agree on any one!
In any case, taurine does seem to be very important, and it does look look like there is a link, especially if giving taurine helps correct heart disease. There are also other nutrients that are equally important as well, like magnesium:
http://www.todaysgeriatricmedicine.com/archive/050613p30.shtml
It could be likely that people have the same ailment for different reasons, like different nutrient deficiencies that cause the same pathology. As we’ve talked about, certain B vitamins and homocysteine are another one.
Hey Morgana, @heathertwist. Guys I’m still reading your latest posts. In the meantime have you seen the Crash Course World History series of YouTube vids? I discovered it today and watched 5–6 episodes. Host John Green takes a fast-paced quirky approach which grows on me. Best of all, he consistently bucks the CW. I just watched his first vid, the Ag Rev, which lines up so much with what we discuss here, gratifying to see:
Eg “[To make a cheeseburger…] …then you gotta grow some wheat and process the living cr*p out of it till it’s whiter than Queen Elizabeth The First … should I be delighted or alarmed to live in this strange world of relative abundance?… and (Heather you’ll like this one) …by far the best hunting gig in the prehistoric world was fishing, which if you look at the prehistory of people populating the planet the tended to run for the shore and then stay there. Marine life was A) abundant and, B) relatively unlikely to eat you…”
Anyway, check it out if you have time. The Ag Rev’s 11min. –Bryan
” bad issues with gallstones and gall bladder function while eating low fat. I’ve read a lot about gallstones, and there are two theories: one is the theory about too much fat in the diet- (which somehow gets “saturated” with cholesterol), the other theory is that sugar and refined flour cause problems with bile- (and I don’t remember the exact mechanism).”
I was thinking about that too. Gall bladder problems are very much associated with celiac … when the gut gets inflamed, the opening of the gall bladder gets closed up.
Also, on a low-fat diet … I’m thinking the nature of the gall changes! There isn’t so much Ch to go into the gall, so it has more bilerubin? And on low-fat diets in the US, there is even less taurine than usual. Anyway, the gall bladder does more than just digest fats. It also dumps dead blood cell contents and toxins from the body. It probably requires a fair amount of fat to operate at peak condition (as does the rest of the body: even if one eats very, very, low fat, the body still needs fat and will manufacture it hopefully).
“I would question whether things like saturated fat in meat are “hard to digest”: ”
By hard to digest, I was just talking about the fact that saturated fat requires a fair bit of bile to break it up, before it can be absorbed. This is true. Our bodies are designed to handle it, if the system is working right. But if, say, you don’t have any bile at all … saturated fat just goes right on through. But MCT oil, at the other extreme, is absorbed right out of the stomach via the portal vein. Some people have a major hard time digesting saturated fats, so they use the easier to process fats (like MCT, or coconut oil).
“for me, personally, animal fats and meat are about the easiest things to digest, and carbohydrates and sugars are the difficult things. ”
So probably you have a nice acidic stomach and good bile acids! Which is good! I personally don’t digest fructose well (which is in a lot of starches too), which probably means I lack fructase, the enzyme needed to process fructose. Some people tend to get candida overgrowth too, in which case dextrose-based starches are iffy. But I used to lack stomach HCL and meat didn’t do well with me unless I took enzymes with the meal. See, just about everything is “a lot of work” to digest!
“As for “recycling” bile, as with so many processes in the body (like cholesterol), it seems this is a normal function and not a pathology.”
I agree. It does seem from the cat studies though, that the bile has a couple of different ways to act in the gut. If it conjugates in one way, it isn’t re-absorbed. So maybe that’s the methodology for “deciding” which Ch is reused.
There isn’t actually a controversy about the bile being a sort of “garbage dump” for the body. As far as I can tell, it is the ONLY way the body can get rid of non-water-soluble waste. What I haven’t seen is a description of what sorts out the “waste” from the “reusable stuff”.
But then, isn’t that what the gut does all the time? I mean, we eat all kinds of stuff … some is useful, some is a bit toxic. The cells that line our gut (supported by a LOT of nerve cells: more than in our brain I think) somehow decide what stuff is going into the bloodstream and what is going to feed the colonic bacteria.
So besides deciding which parts of last night’s pizza should be absorbed, the gut also gets to decide which parts of the bile were the contents of dead macrophages, and which are clean Ch and reusable Tau and Glycine.
“There are also other nutrients that are equally important as well, like magnesium”
Yay for magnesium! Actually one of the links I gave, listed the Tau AND magnesium-excretion levels. Places with lots of magnesium in the water do better, and that article also mentioned that aboriginal cultures tended to eat more nuts. And that soy products had more magnesium than some other modern foods (The Yuzu eat a fair bit of soy products and I’m guessing their water might be high-magnesium … volcanic soil is great stuff).
Arginine and glycine are a big deal too. Glycine is used to make bile also, instead Tau.
heathertwist- oh, thanks, you clarified things quite a lot there, so I may have originally misinterpreted a few things you had written about bile. That all makes sense then. I agree about the celiac problem; I started having terrible gall bladder pain when I was at my worst with celiac symptoms, but before I knew I was a celiac, so was still consuming a lot of gluten. At that time it was terrible; even eating low fat foods, and sometimes even drinking water made my gall bladder hurt! That slowly went away on a gluten free diet, but very, very slowly. And now I feel great, it’s like a miracle cure. As I had written though, I know of other people who had no gluten issues, but who also had gall bladder trouble while eating low fat, so that’s not the whole answer to the bile problem.
And like you, I also have some fructose issues. I can eat some fruits- (the ones that have an equal proportion of glucose to fructose, so basically the low FODMAP fruits); so I am lucky there, as some people can’t eat any. But there are many fruits that I have to avoid. I also have issues with soy, probably a cross reaction with gluten. Unfortunately it took me a few years after being gluten free to realize that all those things were issues for me. Actually, eating dried beans and lentils also cause problems. Funny enough, when I was plant-based low fat those were many of the foods I was eating all the time, which I guess explained my problems! I seem to be a person who was meant to eat meat and fat (and our beloved fish, shellfish and goat cheese of course). I guess I get my magnesium too because I love nuts of all kinds, and I also really like spinach and chard.
I agree that some waste material leaves the body through the bile, no argument there.
Heather, @morgana — again Heather, so interesting. Just a few things jump out at me:
What you say: “…on a low-fat diet … I’m thinking the nature of the gall changes! There isn’t so much Ch to go into the gall, so it has more bilerubin?…
And this: “… Anyway, the gall bladder does more than just digest fats. It also dumps dead blood cell contents [ie bilirubin, hemoglobin] and toxins from the body…”
First, if the bod perceives a need for more Ch, wouldn’t it just crank more out Ch? It’s got all the Cs Hs and Os right at hand.
Also, bilirubin is just the leftover detritus of old partly catabolized red blood cells and is water-soluble:
https://en.wikipedia.org/wiki/Bilirubin
RBC contents, almost exclusively hemoglobin, is also soluble in water:
Click to access h2625pis.pdf
so the bile salts won’t arrange round and cart away any of those RBC products to form micelles. Bile salts do that only for fat-soluble compounds.
I agree on the need to add more magnesium. When I diligently counted my nutrients (2008–2010), Mg was one of the harder ones for me to hit the RDI. Some dried herbs, esp basil and dill, are packed with Mg. I eat those most days. –Bryan
Yeah, I’m not sure at all why gall bladders have issues on a VLF diet. I’ve heard it a lot though. I know that when I did VLF my skin got super super dry and I actually got wrinkles … and I was in my early 30’s. So while your body can produce fats, sometimes I guess it chooses not to?
Or maybe the fat isn’t the issue at all! Shoot, the gallstones are MADE OF Ch … so obviously there IS Ch around. But the Ch is supposed to be in solution. If there is enough Tau, then the Ch is liquid (glommed onto the Tau, or glycine). It’s difficult to have a VLF diet with any large amount of meat or fish, and these days most of the VLF diets are vegan.
Also a lot of VLF diets feature whole wheat or purified wheat gluten, which adds another layer of issues if the bile gets blocked because of intestinal inflammation.
So there is a question: if you eat a VLF diet, have a healthy gut, AND have enough Tau, will you still get gallstones?
Morgana, @heathertwist — Morgana, many good points. And your experience:
“…my digestion and my gall function both got much better after going low carb high fat…”
mirrors mine. At least the overall digestion part. I can’t say specifically about my gallbladder.
For the ultimate cause our pathologies, my thoughts steer back to chronic inflammation, and the many and varied agents that may collude to drive it. Many factors quite apart from diet. –Bryan
Heather, looks like you put a lot of great stuff in here, thank you!
I have to spend more time on it, read your comments/proposals and links. –Bryan
Ah, well, I’ll probably ruin your weekend with yet another … !
It seems diabetics excrete taurine faster than non-diabetics! Possibly because of the diabetes itself.
“The final outcome of taurine homeostasis is through fecal excretion after deconjugation by the bacterial flora or renal excretion as intact molecules (19,21–23). In this study at similar half-life in both groups, the urinary excretion rate of taurine was higher in diabetic subjects. Because the kidneys regulate the body taurine pool, a high-taurine diet induces hypertaurinuria and reduces renal tubular uptake (24), and the opposite happens on a low-taurine diet”
“This is the first study to demonstrate that, after a taurine load, diabetic patients waste taurine more extensively in urine than matched control subjects and probably have a lower rate of net intestinal absorption.”
http://care.diabetesjournals.org/content/30/10/2652.full
I have no idea where this will land, but since I have a definition of LFHC I like, here’s a definition of HFLC from livestrong that sounds reasonable.
http://www.livestrong.com/article/360842-atkins-diet-proportion-fat-protein-on-induction/
70% fat, 20% protein, 10% carbs.
Hm. That Livestrong author, Agalee Jacob, her numbers look off.
http://www.livestrong.com/article/360842-atkins-diet-proportion-fat-protein-on-induction/
“…With less than 20g of carbohydrate a day in induction phase, this proportion corresponds to less than 10 percent of the daily calorie intake…”
Yeah. A LOT less than 10%. More like a few percent.
If 20g of your carbs came to 10% of your total kcals, you’d be eating only 800 kcals/day.
The math: 20g carbs x 4kcal/g = 80kcals from carbs = 10% of 800 total kcals
Yep! Definitely a weight loss diet!
If we went with the typical 2000 kcals/day, then the carbs come to 4% of the total (= 80/2000 kcals)
@heathertwist, thanks, and glad you’re trying the N=1 Japanese diet experiment. As for Japanese films, I’ve watched a lot of Kurosawa – have you seen Dersu Uzala and Dodes’ka Den?
Last night I found the paper the following comes from, but now can only find the linked article:
“Later, Keys studied the eating habits and coronary death rates of middle-aged Japanese–in Japan, Hawaii and California. The native Japanese get only 13% of their calories from fats. They eat a high-carbohydrate diet of rice, fish and vegetables, and have an average cholestrol count of 120. The Hawaiian Japanese, also eat fish, along with meat, eggs and dairy products–they get 32% of their calories from fats, and have an average cholesterol count of 183. The Los Angeles [Japanese] diet is typically American; they get 45% of their calories from fatty foods, and their average cholesterol count is 213. For every one heart attack in Japan, Keys notes, the Hawaiian Japanese have four, the Los Angeles Japanese have ten.”
http://www.happyhealthylonglife.com/happy_healthy_long_life/2010/12/ancel-keys.html
Thhq, that 1957 Keys et al report is garbage.
You can read it for yourself here, that Keys and Grande report that purports to compare CAD in Japanese nationals and American Issei, Nisei, etc:
http://www.ncbi.nlm.nih.gov/pmc/articles/PMC1551415/?page=1
For those compares, Keys and Grande fail to give us a sample rate. We don’t know the actual numbers of subjects studied. For all we know, they could base their observations just on a several people from each place.
They admit “Such large series of autopsy studies are all too few…”
Indeed for the LA cohort, Keys et al say this:
“**Comparable data are not available for Los Angeles**, but both severe atherosclerosis and coronary heart disease are unquestionably very common there among the Japanese whose mode of life is indistinguishable from that of the local Caucasians…”
Oh really?! This vaunted Ancel Keys bases a big part of his argument on an “impression?”
Well sure, why not? Wouldn’t surprise me if *everyone* in 1950s LA suffered higher rates of CAD and all-cause mortality. The LA basin was one of the most polluted places in the world:
http://www.marketplace.org/2014/07/14/sustainability/we-used-be-china/la-smog-battle-against-air-pollution
Even Keys et al speculated the same: “…both severe atherosclerosis and coronary heart disease are unquestionably very common there [in LA] among the Japanese whose mode of life is indistinguishable from that of the local Caucasians …”
Thhq if we go by Keys “methodology” here, we can compare Beijingers with the rural fat-chowing Swiss. And conclude that the high-carb diet causes more CVD and kills you seven years faster!
What I’m saying–what I’ve been saying over and over–macronutrient balances per se may have little or nothing to do with increased all-cause mortality rates in LA.
Indeed, Keys and Grande fail to furnish many parameters at all. We know nothing of the cohorts. For all we know, Keys et al compared rural Japanese farmers to urbanized Issei and Nisei, who suffer more pollution, do less physical work, and have less access to fresh healthy foods. We simply don’t know anything about these cohorts.
Again, this Keys and Grande is good for historical interest. But it is not science. It’s an example of the egregious self-serving trash we used to call science. And unfortunately too many people still do. –Bryan
Whatever Ancel did or didn’t do, the Japanese themselves have studied themselves a whole lot! I trust their studies more. The “happy family” and “low stress” meme has been around awhile, but I don’t think it holds very well. Esp. when it comes to how fast the virtues of “happiness” disappear as soon as they adopt a Western diet!
I just don’t think the culprit is fat. Fat is sort of a bystander … eating saturated fat uses up taurine, and the SAD is very low in taurine to begin with. High-fat diets that appear to work are also higher in taurine, which is what you see in, for example, France.
The initial observation that taurine (T) prevented stroke in stroke-prone
spontaneously hypertensive rats (SHRSP) led us to study the effects of T on cardiovascular
diseases (CVD), as well as the epidemiological association of T and
mortality rates, by using the data from WHO-coordinated Cardiovascular Disease
and Alimentary Comparison Study, which covered 61 populations in 25 countries.
In this study, 24 hour urine (24-U) samples were examined along with biomarkers
of CVD risk. The mortality rate from ischemic heart disease (IHD), which was lowest
among the Japanese compared to the populations of other developed countries,
was positively related to total serum cholesterol (TC) and inversely related to 24-U
taurine excretion (24-UT), as well as the n-3 fatty acid to total phospholipids ratio of
the plasma membrane, both biomarkers of seafood intake. Analysis of 5 diet-related
factors revealed that TC and BMI were positively associated with IHD mortality in
both genders while Mg and T were negatively associated with IHD mortality. TC
and sodium (Na) were negatively and positively associated with stroke mortality,
respectively. 24-UT was negatively associated with stroke mortality. These five diet related
factors explained 61 and 49% of IHD and stroke variances in male, 63 and
36% of IHD and stroke variances in female, respectively.
http://www.jbiomedsci.com/content/17/S1/S6
They studied a number of countries, and use urine excretion as the main criteria. No guessing as to what the people were eating! If you look at the charts, some of the countries that have low taurine levels are not the ones I’d expect.
Here is the kicker though: taurine also tends to lower cholesterol levels, by encouraging the liver to make more bile. It also is key to regulating blood sugar. So there is this correlation between T and low cholesterol, but the T is the cause, not the cholesterol. Likely ditto for diabetes.
This has also been tested by just giving people with heart issues more taurine … no happy family needed. There are a lot of studies on this over the last 20 years, mostly, it seems, in Japan. Unfortunately not double-blind studies I guess, on humans (it works nicely on mice and rats).
“The present review will address the potential beneficial actions of taurine in congestive heart failure, hypertension, ischemic heart disease, atherosclerosis and diabetic cardiomyopathy. There is a wealth of experimental information and some clinical evidence available in the literature suggesting that taurine could be of benefit in cardiovascular disease of different etiologies. However, double-blind long-term clinical trials need to be conducted before taurine can be unequivocally recommended as a nutritional intervention for the prevention and/or treatment of cardiovascular disease.”
http://www.ncbi.nlm.nih.gov/pmc/articles/PMC2586397/
Of course there are no double-blind studies about low-fat or high-fat diets too! Anyway, the huge difference in the Japanese diet compared to the American one is just the huge amount of fish they eat. And especially squid (dried squid are a common snack, and of course squid and octopus is in many food dishes). Also they tend to go for the oily “fishy” fish, like mackerel, rather than the bland cod or rockfish we prefer in the US, and they often eat the seafood raw, which preserves T content.
I haven’t seen Dersu Uzala but I should get it! Thanks! My favorite is still Tampopo. Talk about a carb fixation …
Hi Heather, @thhq:
Heather you may have already posted this, but just in case:
http://www.ncbi.nlm.nih.gov/pmc/articles/PMC3173217/
Taurine appears important enough, we form it via metabolites from CoA, that all-important Krebs Cycle enzyme that’s one of the first things we biochem folks have to memorize:
CoA → Cysteamine → Hypotaurine → Taurine
Not sure how much of this is spontaneous and enzymatically mediated.
Unless we can show that we make always scads of taurine from methionine/cysteine–thus to let us focus on foods high in those two AAs which we already routinely track–I’d really like to see USDA Nutrient Database and other orgs start to directly track taurine in foods.
About Japanese films, I saw Derzu Uzala twice, when it first came out in 1975, and a few years ago, and really really like it. It combines some intriguing survival techniques Derzu shows that Euro-Russian surveyor back the turn of the last cen when that part of the world was even wilder than now. It is very touching in the dear friendship the two men form, even though they come from vastly different places, and what happens in the ending (not to spoil it for you Heather). Seeing it again recently, its comparatively (to these days’ standard) low production quality stood out, but the message came through strong and sweet as ever. Iirc, it’s based on a true story. Kurosawa shot it in far eastern Siberia and was his only joint project with the Soviet Union.
–Bryan
@WBryanH Nice study, and no, I hadn’t run across it. Thanks!
I don’t know how the RDA on taurine is going to play out. Most animals DO synthesize it, and yet getting extra seems to be healing for mice and rats. And how much does a human need anyway? They were tracking taurine *excretion* which sounds like there was a whole lot of EXTRA taurine in the healthiest people.
Which reminds me of the old quip about vitamins: Americans have the most expensive pee in the world. But maybe it’s more like water … you need to ingest extra water … which just gets flushed out … to keep things cleared out in the body.
Seems like there are several ways to create taurine. One is based on methionene turning to cysteine:
http://ajpendo.physiology.org/content/302/10/E1292
http://www.jci.org/articles/view/72606
“Taurine increases IGF1 synthesis in hepatocytes and its action in osteoblasts to regulate bone mass. We next investigated the mechanisms through which taurine affects liver IGF1 synthesis downstream of GH to regulate bone mass. The taurine-mediated increase in IGF1 synthesis suggested that taurine was able to overcome the consequences of B12 deficiency in the liver. Analysis of metabolite levels in the liver showed that methionine levels in taurine-treated animals were rescued to the levels seen in WT animals (Figure 7A). Because MTR, the principle enzyme that synthesizes methionine in mammals, cannot function in the absence of B12, we looked at alternate pathways of methionine synthesis that are not dependent on B12 as a cofactor and could explain the increase in methionine synthesis in response to taurine.”
“Analysis of aged patients with B12 deficiency showed significantly decreased levels of taurine and osteocalcin (Supplemental Figure 8C). Further correlation analysis using all samples from aged subjects showed significant positive correlation between variation in serum B12 and taurine (R = 0.707; P = 0.001), B12 and osteocalcin (R = 0.946, P = 2.6 × 10–9), and taurine and osteocalcin (R = 0.699; P = 0.0012) levels (Figure 8, D–F). These data provide further support for a physiological role of B12 in regulating taurine synthesis and bone formation in humans. However, the human sample size in our studies was small; follow-up controlled clinical trials correlating the markers of the B12/taurine axis with bone formation using larger sample sizes would be needed.”
So the methionine synthesis version requires B12, and uses up methionine? And produces IGF1 and makes bones stronger. But it seems like this would prevent the methionine from being used to build tissues too. Humans don’t synthesize methionine though, I think. And oddly, high levels of methionine are in about the same foods that have high taurine … namely fish and eggs. Which makes you wonder where the vegans get it. It is in some vegies though, and esp. soy beans.
http://nutritiondata.self.com/foods-016084000000000000000.html
So maybe the Yuzus actually might synthesize a fair bit of taurine, along with IGF1 and that keeps them healthy? High levels of methionine isn’t associated with longevity, but rather the opposite … using up the methionine might be a good thing? There is B12 in Miso, which is part of the Yuzu diet.
Heather, you’re welcome! You bring up interesting Qs. Esp how do vegans manage it. Much as vegans’ exceptional sense of righteousness can wear on me, it’s fascinating to witness their grand experiment. 1- 3% of Americans are vegan at any given time–three to nine million people. Many seem to come and go:
http://nymag.com/scienceofus/2014/12/84-percent-of-vegetarians-go-back-to-eating-meat.html
or at least did 15yo. Still, this must include enough vegans dedicated for the long term we can do a big epidemiological study on and perform lots of clinical tests.
In general, I suspect we vastly underestimate our bods’ ability to purge and conserve as needed and make do and even do well with remarkably little. Eg the B12 in miso is remarkably small, like 0.2 µg per 275g cup:
https://www.google.com/search?q=B12+in+miso&oq=B12+in+miso&aqs=chrome.0.69i59j0l4.2226j0j7&sourceid=chrome&es_sm=93&ie=UTF-8
yet maybe that’s enough? Oh, but let’s not forget Yuzus get B12 from fish too.
I’m still trying to make sense of that JCL quote you gave. That for IGF1 synthesis, taurine can make up for a shortage of B12? Is that how you understand it?
Anyway, this jumped out at me: “Because MTR, the principal enzyme that synthesizes methionine in mammals…” Isn’t methionine essential, ie we have to ingest it? Or can out microbiome make it? I thought like you, we had to ingest it.
About what you say “…high levels of methionine are in about the same foods that have high taurine..” that makes sense to me if methionine is the main driver and sole essential precursor to taurine. The less methionine, possibly the less taurine you make. –Bryan
ps, Heather have you seen any of the Ryan Huxtable books on Taurine, eg, “Taurine in Nutrition and Neurology” and “Taurine in Health and Disease” (http://www.springer.com/us/book/9780306448126) That first tome I had a Google Books peek into and it looked quite interesting. Includes copy of researchers debating each other on taurine. –B
“You bring up interesting Qs. Esp how do vegans manage it. Much as vegans’ exceptional sense of righteousness can wear on me, it’s fascinating to witness their grand experiment. 1- 3% of Americans are vegan at any given time–three to nine million people.”
I agree it’s great that so many people experiment with diet. It would be unethical to put people on some of those diets, but if they do it willingly … !
But the answer of course is that many do NOT do well. Vegans in the US have all kinds of support in terms of special foods and supplements, and yet many “crash” after a couple of years.
So what is interesting are people like the Yuzus, who have managed this for generations and raised healthy children.
Discovery of Novel Sources of Vitamin B12 in Traditional Korean Foods from Nutritional Surveys of Centenarians
” Interestingly, we found that the prevalence of vitamin B12 deficient Korean centenarians was not higher compared with those from Western nations with animal-oriented traditional foods. We assumed that there might be some unveiled sources for vitamin B12 in the Korean traditional foods. Screening of vitamin B12 contents has revealed that some traditional soybean-fermented foods, such as Doenjang and Chunggukjang, and seaweeds contain considerable amounts of vitamin B12. Taken together, it can be summarized that the traditional foods, especially of fermentation, might be evaluated for compensation of the nutritional imbalance in the vegetable-oriented dietary pattern by supplying vitamin B12, resulting in maintenance of health status.”
http://www.hindawi.com/journals/cggr/2010/374897/
So yeah, the traditional Korean diet was also close to vegan, but the fermented foods and seaweed provide B12. B12 is ONLY made by microbes anyway … I guess fish get it from algae at the bottom of the food chain.
————-
As for the JCL link … I’m not sure I understand it either. It seems to indicate methionine CAN be synthesized (at least by these mice) but other sources say mammals can’t create it. Methionine though, is *the* growth regulator for raising chickens … if there is too much met in the diet, the chicken doesn’t eat so much, and stays small. If there is too little, the chicken is overly fat.
Anyway, this whole metabolic cycle seems both crucial and also way complex! It makes my head hurt!
I haven’t read the book, and at over $200, I doubt I will. My prediction though, is that in a few years this will be the “next big thing” and it will be on all the talk shows …
HAh! Heather, just scored both Huxtable books! Through our extended library loan system:
– Taurine in nutrition and neurology
– Taurine in health and disease
That’s a thousand pages on our oddball taurine.
omg
Oooh. Now THAT is a clever idea!
If the cable service offered a channel called “Taurine World” I’d subscribe to it. For a month anyway 🙂
You become a true addict when you go to the annual Taurine convention!
http://taurine2016.org/register/2016_met/regi/sub01.html
Heather! Are you going to it?
Lol! No, but it’s tempting. Actually I’m pretty sure in a few years it’ll be in every grocery store newspaper and I’ll be sick of hearing about it and off to something new. Like gluten. 15 years ago, avoiding it transformed my life, but no one else had heard of it.
On that channel. maybe I will see a remake of that classic 1970 Japanese-American WWII pic. With a third POV–that from ardent pescavores:
“Taurine! Taurine! Taurine!”
OK, I’ll stop now…
Is Taurine the Rodney Dangerfield of Amino Acids?
Do we fail to give this oddball AA the attention it deserves?
Heather, this post describes where I’m currently at on taurine.
Per this: http://www.news-medical.net/health/Taurine-Synthesis-and-Production.aspx
we make our taurine primarily (wholly?) from cysteine.
So where do we get cysteine? It’s one of our 21 proteogenic amino acids and appears to be semi-essential. We make cysteine from serine (non-essential) which snags an S from methionine (essential):
https://en.wikipedia.org/wiki/Cysteine
Thus, we should make sure to take in enough methionine.
Specifically, we make taurine via the cysteine sulfinic (sulfonic?) acid pathway, which is this:
http://ajpendo.physiology.org/content/293/1/E62
(scroll down to Fig 1)
1) Cysteine → 2) Cysteine Sulfinic Acid → 3) Hypotaurine → Taurine
Enzymes needed:
1) Cysteine → Cysteine Sulfinic Acid
Cysteine dioxygenase (CDO), https://en.wikipedia.org/wiki/Cysteine_dioxygenase
2) Cysteine Sulfinic Acid → Hypotaurine
Cysteine sulfinic acid decarboxylase (CSAD), http://www.ncbi.nlm.nih.gov/pubmed/17634260
3) Hypotaurine → Taurine
** can you get spontaneous oxidation of hypotaurine without an enzyme? You can find this Q debated in the book “Taurine in Nutrition and Neurology,” ed by Ryan J. Huxtable. Search on that Q string to get the mondo Google Books link.
So Heather, we need two enzymes–three max–to make taurine from one of our core amino acids cysteine. Which in turn may depend totally on our intake of methionine.
So one bunny hole I’d look at: how common or uncommon is it for us to fail to produce (enough of) those two enzymes, CDO and CSAD? E.g. due to gene variants?
Maybe researchers did this already and discovered few if any conditions to limit CDO and CSAD production. In which case, that folks like the USDA scientists don’t bother to assay for it for their nutrient database, since they essentially do that already using taurine’s proxy methionine.
Or maybe no-one’s really examined this after all. And thus we don’t know. And so maybe the USDA *should* include taurine on its nutrient lists.
Given what I know about this matter, methionine appears to be the sole essential precursor to taurine. Thus, I want to at least make sure I get plenty of *methionine* in my food. Here’s the USDA Nutrient Database filter on that (mg methionine per 100g food, from most to least) :
http://ndb.nal.usda.gov/ndb/nutrients/report/nutrientsfrm?max=25&offset=0&totCount=0&nutrient1=506&nutrient2=&nutrient3=&subset=0&fg=&sort=c&measureby=g
Near the top you find eggs, cod, sesame seeds, mollusks, spirulina, and certain cuts of New Zealand beef.
Heather, you might have a fruitful time with that Huxtable book. –Bryan
thhq- Like in other countries, different diets are eaten in the different regions of Japan. Here is a link describing the diet of the Okinawans, with comparisons as to what was different from the mainland. (I thought you might find it interesting, as they are meant to be the longest lived people in Japan):
http://nourishedkitchen.com/hara-hachi-bu/
@WBryanH – “It’s my sense that the “Blue Zone” and other very long-lived folks, they tend to limit *all* animal-sourced foods.”
Your sense is based on claims that are made. But I’d suggest you research it for yourself. The evidence leads to the opposite conclusion.
Thinking about Japan now, in relation to health and longevity….a couple apocryphal bits about several trips in the 1990’s….
First impression was that they smoked like fiends, everywhere and anywhere. It was like the national pastime.
Second impression is that there were established hierarchies of foods, best to worst. I observed this with rice, green tea and beef; but I’d guess it applied to other foods too. For rice, the best was Japanese farmed, American in the middle, and Thai at the bottom. Green tea I could never figure out. Beef was ordered from fattiest to leanest. Price differences were huge on all of these – maybe 10x difference top to bottom quality.
Comparing what I saw with what Keys and Kimura reported from the 1950’s and 60’s, here’s my guess on their habits.
Japanese farmers were probably smoking like fiends. For their high carb diet they were probably eating the cheapest industrial polished rice (the rice they grew would have been too valuable for them to eat – I think GT’s brown rice theory is pretty unlikely, unless you backdate to pre-1900), along with a lot of the Japanese traditional wheat noodles used in udon and ramen. This was probably doused with lots of soy sauce. Alcohol was probably beer, the standard beverage I saw a lot of at dinner. Meat was probably scarce, due to cost and traditional religious objections.
Keys and Kimura’s reported major causes of farmer mortality were stroke and stomach cancer. That would appear to fit high smoking and soy sauce habits, and possibly the very high cheap carb diet too.
Glad you guys liked Dersu. The Kurosawa films have a lot of tragic nobility. Dodes’ka Den is just tragic, but eerily abstract. Haven’t seen Tampopo, only heard of it.
This piece has a discussion of the relationship between Japanese heavy rice consumption and stomach cancer. I can’t imagine eating a kilogram of rice a day the way those farmers did.
Click to access 3254.full.pdf
The Japanese salt consumption of 10-15 kg per year is extreme. Americans eat about 3-4 grams per day and that’s considered high….but on an annual basis it’s only 10% of the average Japanese consumption.
Click to access 1543.full.pdf
That’s not counting the effect of all those cigarettes. We brought gift cigarette cartons on one of the trips and were criticized for bringing the strong American Marlboros instead of the kinder and gentler Japanese Mild 7’s. They liked the whiskey we brought better. The guy assigned to travel with us really enjoyed his, and left us with the impression that he’d finished the fifth overnight. I sat by him at dinner once and kept replenishing his empty sake cup…the result was almost as entertaining as karaoke…
thhq- I had a look at this link about rice intake and stomach cancer; however, to be honest, I am highly skeptical that white rice causes cancer. The authors of the study seemed to be speculating, and did not give a clear, logical reason as to why or how polished rice could cause stomach cancer. (They claimed that “rice stretched the walls of the stomach” which didn’t seem like a good explanation to me). And of course as we know, correlation does not equal causation. (Personally, if we’re going to speculate, I think heavy smoking makes more sense).
In her book “The Whole Soy Story”, Kaalya Daniels theorizes that the soy the Asians eat might be the issue- (though again, this is speculation). According to her, traditionally all soy products were heavily fermented- sometimes for years at a time!- to remove the toxic and difficult to digest substances. But apparently in recent years- even in places like Japan and China- they have started using shortcuts and adding elements to soy products so they are on the market faster- (for instance, traditionally soy sauce was fermented for a long time, whereas now they might add alcohol to it, taking out that important step). She claims that soy in its unfermented form can be toxic to the body, difficult to digest, and we know that it’s an endocrine disruptor. So, rather than the salt content or the rice content, the actual modern day preparation of soy could be the issue.
Of course, the incidence of stomach cancer is relatively high in some other countries as well, and places where they don’t traditionally eat soy or rice. (Like Poland). In the book “Missing Microbes”, the author suspects that this is due to gut microbes, most particularly H. Pylori. In countries where H. Pylori is higher, there is more risk for stomach cancer; however, at the same time, there is less of a risk for esophageal cancer; (according to him, a lack of H. Pylori can be an issue in esophageal cancer). In those countries where there is a relatively low incidence of stomach cancer (like the US), there is a higher risk for cancer of the esophagus, so it’s basically a “wash”. In any case, it’s a reminder that diet may not be the issue; there could be other issues, like the gut microbes found in various populations. Well, of course, people still don’t really know exactly what causes cancer, it’s basically guesswork based on correlations.
Gary Taubes’ main issue with white (polished) rice was due to the high glycemic index, which means that certain groups of people who are susceptible to those kinds of carbs would have problems, like metabolic issues, blood sugar problems, etc.
Morgana: Unfortunately, there is a very real and well-understood link between dried fish and cancer. It doesn’t even matter if the dried fish is dried without chemicals in the sun on a pristine beach. So in places like Kitava … where the food and the people are generally healthy … you still see this high level of stomach/esophagus/nose cancers. There are other methods of cooking fish that can do this too.
Click to access 956.full.pdf
The countries that eat a lot of dried fish happen to be the ones that also eat a lot of white rice, is what I think happens. There used to be a lot more nitrosamines in American/European foods too, but the FDA established rules about curing meats that drastically lowered the nitrosamine content, and stomach cancer rates dropped here.
I guess this is another point for eating very fresh, lightly cooked, or raw, fish (sushi!).
heathertwist- ah ya, the old “nitrosamine” debate. I’ve read a lot on the subject, and I’m not sure that there is enough proof that nitrosamines are the cause of stomach cancer (or any other cancer). Apparently the original paper was “debunked” and didn’t stand up to peer review (link below), and epidemiological studies always have confounding factors- (like maybe the high smoking in the Asian studies?) The authors of the link you posted even admitted there may be confounding factors to their study. In addition to that, the vegetables in the average diet have far more nitrates than smoked/dried fish or meat, and apparently, our saliva has more natural occurring nitrate than all these things combined. So for me this issue is by no means proven:
http://thedigestersdilemma.com/truth-nitrates/
According to what I’ve read, the greatest risk factor for stomach cancer is H. Pylori bacteria infection. I suspect that people in certain countries have a higher incidence of H. Pylori, and that gastric cancers may have a lot to do with gut bacteria. I find it hard to believe that traditional foods like smoked or dried fish would be an issue, although I guess I don’t know this for sure….maybe I’m going to research this a bit more now…..(since I do eat raw, salted herring which is a local specialty where I live).
I don’t recall the details offhand, but there are very specific types of nitrosamines that reliably cause cancer, and a lot of the studies are on rats. “Nitrates” per se aren’t the issue. And the amounts of nitrosamines in salted dried fish varies hugely depending on how the fish is dried. And then there is another huge variance depending on how the fish is cooked. Oddly, the biggest risk is to adults that were exposed as *children*. It doesn’t seem to be as much of an issue in adults.
The levels of N-Nitrosodimethylamine was from 0 to 400 micrograms/kg, depending on the fish. But a lot of the fish was fed as a weaning food, and that seems to increase the level of cancer later.
Click to access mono56-6.pdf
“Since Ho published his hypothesis in the early 1970s, eight case-control studies have
been conducted to investigate the association between consumption of salted fish and the
occurrence of NPC among Chinese living in different parts of the world and displaying
distinct risks for NPC. The evidence is derived from studies conducted among the very
high-risk Cantonese Chinese in Hong Kong (Geser et al., 1978; Yu et al., 1986) and
Guangzhou (Yu et al., 1989b), among southern Chinese in Guangx Autonomous Region,
who have intermediate rates of this disease (Yu et al., 1988), and among Chinese in Tianjin,
who have relatively low rates (Ning et al., 1990). ln addition, the association between
consumption of salted fish and NPC has been observed among southern Chinese living
outside of China or Hong Kong but who have maintained this custom (Henderson et aL.,
1976; Henderson & Louie, 1978; Armstrong et aL., 1983).”
This bit is nice because it describes many of the actual drying processes, which are different from country to country. The “aromatic nitrosamines” add to the flavor. Also note that in some of the processes, the guts are left intact (which increases histamine content) and the fish is left to rot some.
My thoughts on the brined/dried fish though are that a lot of it probably has the taurine leached out of it! When squid is dried, it has a white powder all over it … that is the taurine. Most of the dried squid I see is just plain dried squid … they lay it flat on screens to dry or put it on a spinner. It’s easier to eat as a snack too, because there are no bones.
I got some of the dried fish sold as bar snacks in Russia … they are pretty tasty but you are supposed to sit there and take off the skin and pick the meat from around the bones. Too much work in my book.
I like brined herring too though. I don’t know about the taurine content, but it’s loaded with good fats. My favorite though is cold-smoked mackerel. Yum! There doesn’t appear to be a lot of nitrosamines in non-dried non-broiled fish though.
heathertwist- thanks for that very thorough link! Very interesting…..I had never heard of a possible link before between dried fish and stomach cancer. The conclusion of the authors seemed to be that Chinese dried fish was carcinogenic, the others looked possible but inconclusive. If it’s more prevalent in people who ate dried fish as children, maybe it relates to gut bacteria in some way? Maybe a “mature gut” has more protection? Anyway, it’s something to delve into.
I wonder if there are groups of people who don’t eat smoked/dried fish, and still have a high stomach cancer prevalence? Or groups that do eat dried fish with low stomach cancer rates? Very curious indeed……
Thanks @morgana for the Okinawan link. I’ve probably read it before, but seeing it juxtaposed against the Japanese diet details the differences hit home. Especially the Japanese’ massive rice consumption. Piling on the salt appears to go hand-in-hand with the rice. I’m sure the Okinawans eat some miso, soy sauce and pickled vegetables but not like the people on the main islands.
thhq- I think a big difference was that the Okinawan diet was a nutrient dense diet. Reading about it, it sounded like good, wholesome foods to me; in fact, my mouth was watering and I felt hungry when I was reading that article! The foods described were things that I would enjoy eating- (although unfortunately, I have an intolerance to soy, even soy sauce….much as I love Japanese food). Contrast that with the farmer’s rice diet; I think the main problem is the white rice diet just isn’t very nutrient dense. It also doesn’t sound the least bit satisfying!- (maybe that’s why they smoke so much, and drink sake?) It’s hard for me to imagine how the Kempner rice diet that Denise describes worked so well for those people; but possibly, as many of them were obese and had metabolic issues, maybe they already had enough stores of nutrients in their bodies; i.e., maybe the rice diet was almost like fasting? (Which can also have beneficial effects, especially for certain groups of people). Anyway, that’s my theory about the Okinawan diet, it just sounds like a more satisfying diet with high quality, nutrient dense foods. My theory is that with the farmers, the rice “per se” was not the problem, but more the fact that too much nutrient poor rice was replacing other valuable foods.
@bryan, one man’s trash is another man’s treasure.
I related a first-person observation about the saturated soy oil Stable Flakes because I was shocked to discover that people eat it in their french fries. I thought that might interest people here. And it launched the discussion of Crisco, another dietary malefactor.
Finding out about the dietary uses of Stable Flakes wasn’t even why I went to Minneapolis. It was just an unpleasant observation I made while I was there. Yet you used that story to launch an ad hominem attack, accusing me of working in an unworthy profession, eating an evil diet and in cahoots with Monsanto. Where are you coming from? Slow down and read more carefully. Take your meds, man.
Regarding the Keys study of Japanese American CVD, same thing. It’s trash for you, it’s a useful observation for me. It brought to mind my overweight nisei dentist, who introduced me to National rice cookers and also (in the office banter) a heavy consumer of soy sauce. He died at age 74, from a stroke as I remember, but having had that experience I could identify with what the study said. Maybe his heart was perfect, maybe American fatty foods were not to blame, maybe it was all that salt and rice, but I was a witness to an N=1 in a population Keys observed. If you can’t get anything out of the 7 Nations study I can.
Regarding the Eade’s interview of GT I saw one other thing of interest beyond the Japanese diet details. GT talked about having to cut the 400,000 word manuscript of GCBC down for publication. When I was writing technical reports, I was trying to figure out how to compress a 4000 word report into a clear 100 word abstract for an audience who had to decide whether to risk their money on the results. A different kind of writing. I love reading dense prose, and I can appreciate GT trying to come across as clearly as he knows how, but I’ll be checking out War and Peace on the next trip to the library instead of GCBC.
Sure Thhq. What you say and how you feel and all that jazz.
About Ancel Keys and his work, the sooner we drop-kick it into the dustbin of history, the better.
At some point–in five years? In ten?–the grass-roots groundswell will grow large enough, enough people will have voted with their dollars to force Big Food to make fundamental changes no matter how many megabucks their lobbyists toss at the pols, our quickly growing “new” nutritional knowledge will settle down enough, the sheer amount of time will have passed enough–all to allow the ever-timid ever-trailing-edge US food and nutrition reg bodies to finally and firmly repudiate Keys’ shoddy self-serving work. To admit to the world they made a terrible mistake but that “we all learned valuable lessons from it and now we can move forward.” –Bryan
@morgana you’re right, it’s probably not the rice so much as all that salt and smoking while eating that causes stomach cancer. I used to have a picture of a conference table after a meeting. A full cup of green tea, an unopened pack of biscuits and an ashtray stuffed with butts. Anywhere, anytime, always that thick blue haze.
@bryan I usually check the morgue over at abebooks to find out who’s being kicked in the dustbin. 100 copies of GCBC for sale today, starting at $2.69. But if you want a copy of The Biology of Human Starvation, the price starts at $68.89 and goes up to $1200 for a clean copy.
If you want to kick Keys writings into the dustbin of history go right ahead. They’ll be landing in a dumpster already filled with copies of GCBC.
Thhq, thanks! I’ve been meaning to check the Best Seller ranks for books we’ve all been discussing.
Here they are, per Amazon.com:
#8,165 – Good Calories Bad Calories – Gary Taubes
#237,791 – How to eat well and stay well the Mediterranean way – Ancel Keys
#196,032 – The Biology of Human Starvation: Volume I – Ancel Keys
#1,452,411 – The Biology of Human Starvation: Volume II – Ancel Keys
–Bryan
Thhq, I’ll just let my previous comment stand. Won’t get drawn down that celeb personality road with you again 🙂
About what you say “…it doesn’t appear that the Omega 6 fat people are eating is harmful to their hearts or their longevity…” of course this is pure speculation. We can’t possibly say one way or the other. We can’t discuss simply “w6s” in isolation, but always in the w6/w3 ratios. And do we get them just in diet or in supps? And what kind of each in what amts, 18C (LA), 20C (AA) etc. and longer chains? My sense is that’s it’s generally very hard to get w6s & 3s in wacky ratios just through diet, but that’s me as usual peering through the ancestral lens. That said, it’d be interesting to study ancestral groups that get very low long-chain w3, like those who live far from the sea. Are they generally low on w6 too? Do they up-reg synthesis of long-chain w3 from ALA? Etc. –Bry
thhq- you’re making a huge generalization here! I, for one, was fat phobic for most of my adult life- unfortunately, as I became very unhealthy from this way of eating. I know very many Americans who are to this day still appalled by fat. Many of them appear fearful and uncomfortable when they see me eat my bacon….
Here in Europe, where I live now, people are far more relaxed about dietary fat. Just giving you my personal observations here.
Thhq, to clarify, what I said “My sense is that’s it’s generally very hard to get w6s & 3s in wacky ratios just through diet,” I meant to add *in whole ancestral foods* Veg/seed/legume oils, in addition to their hosts of other ills, give us way WAY too much w6. Jonathan thanks for reminding me of this. –Bry
And Thhq to add to the w6 part, how much w6 and w3 do we typically get? Both fats are very unstable and prone to oxidize, which sugg that the closer we stick to the min amts the better. Mary Enig in her book “Know Your Fats” suggs the balance back ~1900, just before mass avail of veg/seed/legume oils, was (going from memory here) 6–7gm/day w6 and 3–4g/day w3. That’s roughly a 2:1 ratio. And the absolute levels are modest. These omegas are essential FAs, the parent 18Cs absolutely essential, the longer chains conditionally so. But this suggs we typically don’t need much omega. –Bry
Thhq, what should we glean from your “random thinking” post?
Regarding diet and CVD, which of Key’s ideas is this supposed to validate? Besides “Trans-fat is bad for you?” A point few of us argue at this time.
That blogger you cite, Joseph Dixon, concludes:
“The data … shows [sic] convincingly that the efforts to lower total dietary fat, and especially to lower dietary saturated fat, were indeed successful in reversing the epidemic of deaths due to CHD that were observed by Ancel Keys and other scientists in the time after World War II.” That blogger cites Keys’ Seven-Country Study (7CS) to support his conclusion.
Trouble is thhq, 7CS *doesn’t actually say* what Citizen Blogger Dixon claims it says. See for yourself:
http://sevencountriesstudy.com/saturated-fat-and-coronary-heart-disease
“…among populations of the 7CS showed that the average *saturated fat intake*, average serum cholesterol level and 10-year CHD mortality rates in the 16 cohorts were strongly correlated.
Thhq, so where does that say “…efforts to lower total dietary fat…” like Dixon claims? Right. NOWHERE. At least not at the site I give above, which comes from one of the 7CS researchers.
Also, the study leads make clear: it’s purely correlative. “Correlation does not imply causation”–many of us have heard zillions of times. Further, Keys, for some reasons not clear to us, narrowed the original list down from 22 countries to this relatively small seven-country sample.
Then the study leads fail to break out very many confounders. E.g. calories in-calories out. Poorer nations eat closer to subsistence diets, thus overall lower calories regardless of calorie source. We see plenty of evidence to suggest calorie-restricted diets–HCLF, swampland, LCHF, etc–can be healthy.
And then the study leads fail to break out the *types* of dietary sat fats. We metabolize diff sat fats much differently. The shorter the sat fats, the more of them travel directly to the liver via the hepatic portal. Short- and medium-chain sat fats (2–12 carbons long), like those we find in butter and coconut, head more in our bods via that hepatic portal. Meanwhile the longer sat fats (14–22C), we have to load them into chylomicrons and send them into our serum via the lymph, which takes much longer.
Thhq, you assert this:
“Despite the obesity epidemic, and our massive increases in fat and carb consumption, our hearts have gotten healthier. This is a multi-factorial effort, involving better therapies, statins, reduced smoking…and diet. The last was Ancel’s part. Trans fats are more or less wiped out (even in the 50’s Keys hated margarine), and the fast food chains no longer deep fry with lard…”
Thhq, you simply can’t support your entire assertion. Could well be a slew of many other factors increased US life expectancies *despite* deleterious dietary changes. Also, fast-food chains may well have fried in veg oils since well before Keys’ work. Why not?–they’re cheap and have long shelf life. P&G invented Crisco (hydrogenated veg oil) in 1911. Per this New England Journal of medicine study:
http://www.nejm.org/doi/full/10.1056/NEJM199406303302620
“…It has been suggested that hydrogenated fats may be the main cause of our epidemic of cardiovascular disease, which began in the 1920s, shortly after hydrogenated fat was introduced…” People started cooking with them because these fats are cheap and you don’t have to fridge them. Why wouldn’t fast-food places used them from their beginning?
Btw thhq, what your say “…fast food chains no longer deep fry with lard.” Lard is not even primarily a sat fat, the type of fat Keys indicts. Lard has more mono fat than any other kind of fat.
Thhq, we face this slew of questions and unknowns even *before* we get into the fact that CVD risk does not encompass *all-cause* mortality or life expectancy. And that life expectancy does not describe *healthy* life expectancy. Which many nations with very varied foodways–including those relatively high on fat diets like in France and Switzerland–do better on all counts than the US. Citizens in those countries routinely live longer and more healthfully than those in the US, the richest and most powerful nation in the world.
http://apps.who.int/gho/data/node.main.688
There’s loads wrong with this whole picture. –Bryan
Not to mention cigarette smoking – Dr Dennis B Waddell pointed out to me that machine-made cigarettes became available in 1900 – he plotted cigarette consumption data from the USDA and CDC to 1995 against heart death data from the CDC and found the correlation to be very strong at 0.98, with no time lag. He wrote me “This goes against conventional theory as there is no time lag in the correlation and it is thought that the effect of smoking on coronary heart disease takes several years to manifest.” Anyway, this is a far stronger correlation than anything Keys came up with, or Yudkin for that matter. Seems to me that any who are set on substituting causation for correlation will look a hell of a lot less like a horse’s ass with cigarettes than with fat cholesterol sugar or trans fats, or even with all of them lumped together
I note that below @Jonathan. Focusing ONLY on the Nations study does not give the whole picture on why our longevity improved. Many factors changed.
The Seven Countries Study conclusions may well be largely, even *completely* wrong. Huge advancements in other areas–such as dramatic cuts in smoking rates, removing lead from fuel, huge reductions in industrial pollution reduction when the US brought in the EPA in 1970, increasing move away from fossil fuels, etc–may be the true contributors to lower CVD and longer lives. –Bryan
And the Nations study may not be relevant at all. But Ancel was part of the team. You and I weren’t. We can only observe and learn. I’m trying to learn why Ancel lived to be 100. His activity as a part of that team might be part of this.
I’ve also determined that Ancel had relatively long-lived parents, was very active, muscular but not a sportsman, weighed about 180 and was about 5’7″, and walked a lot. There are no doubt important factors too. But I can’t judge whether they are more important than cutting the dietary red meat, using lots of olive oil, and eating bread and pasta.
It’s interesting to look at longevity figures, but ultimately how much can they tell us? We all know about Jack LaLanne, how strong and fit he was, and how closely he monitored his diet, and which seemed to pay off because he lived to 96. Lesser known is his brother Norman, who lived to 97, and by one report at least Norman was not a “health nut.” According to that same source, the bros’ Mom lived to 94, but their Dad died at 50. We might suggest genes, but then there’s independent assortment at meiosis, which for almost certainly highly multi-factorial traits like innate potential for longevity, makes the genetic influence almost impossible to determine. –Bryan
Looking at ONE health nut doesn’t tell you much, but when you look at a lot of them you start seeing patterns!
Jack LaLanne impresses me not because he lived a long time, but because he was STRONG in old age. Ditto for the Japanese mountain people. They don’t just survive … they look young. Their skin and hearts are healthy. My Mom is 90 and sharp as a tack. But, she can barely walk, and has used a walker for the last 20 years or so. Her hands are totally messed up with arthritis, as are the hands of my sisters. I started getting the same issues, but then changed my diet.
It might be genes, but it’s also the case that Jack’s Mom was instrumental in changing his diet too:
LaLanne was addicted to sugar as a child, causing him to commit acts of violence, including setting his parents’ house on fire and attacking his brother with an axe. He was so weak his family physician recommended he be removed from school to rest and regain his strength. Around this time, he and his mother attended a lecture by Paul C. Bragg, a nutritionist who told LaLanne he was a human garbage can. LaLanne turned his life around with a strict diet and exercise …
http://www.imdb.com/name/nm0482364/bio
It wouldn’t be a big stretch to figure the brother changed his habits some too. At any rate, Jack was a sickly kid who turned around, so you can’t just blame genes.
The factor that makes such a huge difference in cats is taurine, and it’s really hard to know how much taurine is in cat food. I buy cat food that happens to be high in it. My cat is 18, and doing great. She also craves high-taurine foods (and goes nuts over taurine tablets!).
There is a high level of taurine in the Japanese diet. But although they eat a lot of fish in Finland, there is a low level of taurine in the Finnish diet and Finland has a high rate of heart disease. The main difference that I can see is that in Finland, fish is mostly brined and soaked, which takes out the taurine, and they don’t eat much squid or scallops. So just looking at macronutrient levels don’t tell you the actual nutrient levels.
And the person doing the diet may well not know why it’s working. Jack may have said “It works because there is no sugar!” but in fact it may have to do with his fish recipes. Terry Wahl’s diet isn’t too far off from Jack’s diet too. The famed “Mediterranean diet” may have less to do with olive oil and more to do with octopus and scallops.
So take a look at this!
Jack LaLanne on how to cook fish! He uses a Chinese recipe … “barely cook it” (he likes it on the raw side) and don’t boil it for heaven’s sake! … “all the goodness will boil away”.
Now the brother lived in Morro bay, and sold marine supplies … this was a major fishing port and a center of fishing everything. Also lots of Asian people cooking fish Asian style. Which is high-taurine fish.
I find Jack’s video amazing for the era. Right about that time my Dad was visiting near Morro bay, and saw this funny “rice cake” that he fell in love with. Turned out to be this weird thing called “sushi” which my Mom promptly learned to make (albeit not with raw fish, that would be TOO weird!). Jack was trying to please his sponsors too, so I’m not sure his TV diet was truly his private diet. For all I know he did eat his fish raw.
Heather, you’re very right. I meant to say “…it’s interesting to look at *n=1* longevity figures. Left out the n=1 part.
We may well be able to glean lessons from the longevity hot-spots, the “Blue Zones” like where live the Okinawans, Seventh Day Adventists in Loma Linda, certain Sardinians etc. But their totality of factors that contrib to their long lives go way beyond foodways, including rich social lives. Plus, anyone that old spend their first few formative decades before WWII before we inundated our enviro with novel chemicals. They had more chance to develop robust healthy energy metabolisms.
And no question Jack LaLanne looked very fit right up to near the end. So far I see at least two mortality causes we find in both the H-Gs and industrialized societies: osteoarthritis and reduced immune response. JL possibly minimized his osteo (or maybe even didn’t have much of it at all) because he exercised so diligently. We see amazing stories now about 80- and 90-something who remain incredibly fit through exercise. Recently heard about the 95yo runner, Orville:
http://www.runnersworld.com/newswire/a-95-year-old-record-setters-rules-to-run-by
And esp Ida, a 97yo who started running at 67! Wow. Never too late!
http://www.goodnewsnetwork.org/95yo-woman-sprinter-2/
But the reduced immunity–not sure why we seem programmed to lose it. Our thymus glands, key to us to produce T-cells, appear to shrink as we age no matter what we do. We gradually lose all those pathogen immune signatures we accumulated in our younger years. And so more often die from infections when we’re old.
So c’mon Great Minds–please figure this one out! –Bry
@heathertwist, the high CVD rates in Finland were inland, not on the coast. I was there once and had the delicious local delicacy reindeer hot pot: potato reindeer stew in a heavy brown gravy, with lingonberry sauce on the side. I don’t remember anything fishy in 2 weeks of being there. But they did enjoy their fresh sour wild berries!
“@heathertwist, the high CVD rates in Finland were inland, not on the coast. I was there once and had the delicious local delicacy reindeer hot pot: potato reindeer stew in a heavy brown gravy, with lingonberry sauce on the side. I don’t remember anything fishy in 2 weeks of being there. But they did enjoy their fresh sour wild berries!”
Aha! That makes more sense!
The thing I was reading measured taurine in urine, but didn’t analyze diet especially. I’m trying to put the two together. My usual thought is: sitting near the ocean, you eat fish! But that isn’t how history has worked. In Britain, fishing was replaced by dairying in a very short period of time, and their health suffered.
“In a previous study, carbon isotope testing of human bone from up to 5,000 years ago detected a rapid and complete change, both coastal and inland, from the marine and wild animal diet of the Late Mesolithic period. The attraction of farming was strong enough to cause the switch to eating the products of ‘domesticates’ at the onset of the Neolithic, Martin Richards suggested in Sharp shift in diet at onset of Neolithic.”
http://decodedpast.com/neolithic-peoples-loved-dairy-foods-rejected-fish/7155
Milk is actually fairly high in taurine, esp. raw milk, and esp. if from goats rather than cows. Not much in reindeer though! Anyway, CVD tracks with taurine consumption, and giving taurine supplements seems to reverse CVD.
Thhq you say: “But Ancel was part of the team. You and I weren’t.”
So what? How does that matter at all?
Being “a part of the team” doesn’t change a thing. Keys still put his name to a doc that concluded all dietary fat positively correlates to CVD. Which a growing body of new evidence, and my and many others’ n=1s refute. Keys’ conclusion, however much politics motivated it, however much it departs from his Seven Country Study findings, greatly contributed to untold numbers or people getting ill and dying terrible deaths much too soon. This is a largely silent but immense tragedy. –Bryan
Yes, it’s important that he was part of the team. Remember what I said about his incessant activity. Whether his contribution was ultimately important, whether he was wrong or right, he was ACTIVE, and that may be part of the key to his long life. For other nonagenarians like Julia Child and Colonel Sanders, their high levels of activity (mental and physical) seems to be part the explanation for their long lives.
Thhq, so what? Your statement could not be less relevant to the topic.
Did you forget we’re talking about CVD and dietary fat?
–Bryan
Did you forget that my interest here is longevity@Bryan?
I’m not interested in Keys CVD and dietary fat theories. I’m interested in why he lived so long. Same with Julia, The Colonel and Ferlinghetti.
Well, in terms of my “taurine theory”:
http://mbbnet.umn.edu/hoff/hoff_ak.html
“While in Yugoslavia in 1958, Keys and his wife corrected proofs of their book Eat Well and Stay Well, which became a best-seller/ Readers were advised to “eat less fat meat, fewer eggs and dairy products. Spend more time on fish, chicken, calves’ liver, Canadian bacon, Italian food, Chinese food, supplemented by fresh fruits, vegetables, and casseroles.” Margaret Keys supplied 200 low-fat recipes.”
Fish, liver, Italian food and Chinese food are all high-taurine foods.
“But life in Italy away from the cities is another matter. The Keys home is outside a fishing village. The townsfolk are friendly, and life is lived at a patient pace. “Just a few days before we left I went down with a big stack of mail and discovered I’d forgotten my wallet. The postmaster said, ‘Forget it, pay me some other time.’ We know everybody in town, though I’m sure I couldn’t tell you the names of 90 percent of the people, or maybe just their first names or nicknames. And people bring us things — a fish, a rabbit, a loaf of home-baked bread. They’re not rich.”
Hm. Living in a fishing village. Eat fish much? Probably octopus/squid/scallops too?
There appears to be little doubt that taurine makes human hearts more healthy. It’s not fat, it’s not carb, and it’s not even really a protein. But the main source is seafood, organ meats, and some dairy products (like goat cheese).
If you look at the infamous 7-countries study … Finland is very low in taurine (surprisingly) and Japan is very high. Mediterranean countries somewhere in the middle. Based on taurine in urine, which is the best way to measure it.
So here is the weird part: taurine lowers cholesterol in a very odd way. You need taurine to produce bile, and bile excretes cholesterol (and heavy metals and other gunk) out of your system. So your high-fish diet does lower your cholesterol, but not because it is low fat or has better fat. It just helps you make bile.
http://www.lifeextension.com/magazine/2013/6/The-Forgotten-Longevity-Benefits-of-Taurine/Page-01
heathertwist- all of this information about taurine is really interesting, and it makes sense. The sad thing is, why doesn’t anybody know about it?! Why are so many people on statins?! (Well, I know “why”, it’s just so wrong though),
Happily, I must be doing well with taurine, as I love goat cheese, eggs with runny yolk, and all kinds of fish and shellfish,,,,this is my diet!
Oh yeah, I eat nuts. In epidemiological studies nuts seem to be quite protective against heart disease as well. Any reason why? (No taurine in nuts, I assume).
Oooh, I love nuts too! Nuts have loads of good stuff in them, but one of the things is Vit E. I don’t recall where I read it, but Taurine, Arginine, Magnesium, and Vit E was the combo used to treat heart arrhythmia. I suspect those are the items that are just low in our diets these days. There is a lot of Vit E in fatty fish too, but how many people start the day with a slice of mackerel?
As for why we haven’t heard about this. Wow, I sure don’t know. I’ve seen the same thing happen with some other things though. One part of society knows a thing, and a whole lot of other people have simply never heard of it. Some people have suggested to me that “they” are keeping it a secret. But sheesh, it sure isn’t secret. 10 minutes of Googling will find all the info you could want. And yet I didn’t see it until a few days ago.
About 15 years ago I started using coconut oil, and everyone thought we were being really weird. I predicted CO would be a big deal soon. Well, not too soon, but these days my relatives are coming to us saying “Have you heard of this new oil? It’s called coconut oil!”. LOL! I expect Taurine is going to be one of the Next Big Things and the docs will be prescribing it.
Morgana, @Heather, on taurine, I admit I haven’t yet read through your links. But wanted to post this for you to nosh on.
Maybe it comes down to our bods’ levels of our two sulphur-containing amino acids, cysteine and methionine? Could it be the research comm never doubted our ability to synthesize enough taurine from those two AAs?
Per the below four links, cysteine is conditionally essential, methionine entirely so. We make some cysteine from methionine. We make taurine from cysteine/methionine:
https://en.wikipedia.org/wiki/Cysteine
https://en.wikipedia.org/wiki/Methionine
https://en.wikipedia.org/wiki/Taurine
http://bodyecology.com/articles/deficient_in_taurine.php
I went to the trusty USDA Nutrient Database and searched for our foods highest in cysteine and methionine (sorry for the long links):
Cysteine: http://ndb.nal.usda.gov/ndb/nutrients/report/nutrientsfrm?max=25&offset=0&totCount=0&nutrient1=507&nutrient2=&nutrient3=&subset=0&fg=&sort=c&measureby=g
Methionine:
http://ndb.nal.usda.gov/ndb/nutrients/report/nutrientsfrm?max=25&offset=0&totCount=0&nutrient1=506&nutrient2=&nutrient3=&subset=0&fg=&sort=c&measureby=g
Guess what’s at the top of the both lists? Eggs, seafood, meats!
IOW, maybe dietary levels of cysteine and methionine serve as a sufficiently robust proxy for taurine?
Btw, I search on “cystine” since the dbase doesn’t include “cysteine.” Cystine is two cysteines linked together per this:
https://en.wikipedia.org/wiki/Cystine
Did the dbase folks misspelled it, or cystine was the assayed pdt? Idk. –Bryan
Morgana, @heathertwist, to sum up my recent taurine/cysteine/methionine post to you, could be you saw the bennies from ramping up seafood due to the increased *cysteine and methionine* you take in. Just a thought. –Bryan
It could be … there are lots of factors for sure. My usual diet has lots of eggs, since we have chickens, so methionine and cysteine we have lots of. But for my taurine experiment, I started with taurine capsules, which makes it easy to measure what is going on. Then I switched to powder, which makes it easier to take, and added some arginine.
What I can say, subjectively, is that it makes a big difference! I get heart palpitations sometimes, and the taurine just stops them. I’m quite a bit stronger too, and am back to being able to haul a 40-lb bag of chicken food.
Now I’m adding some squid and more fish. Whole seafood has loads of other nutrients besides taurine and it is a nice snack. But a bit of a confounder when it comes to measuring the effect of taurine!
Thhq you say “I’m not interested in Keys CVD and dietary fat theories”
Oh no?
Is that why you said “…thinking about Ancel Keys positive contributions again….The whole reason for the Nations studies was to understand and reduce CVD mortality.”? (In that study, the Seven Countries Study, Keys correlates dietary sat fat with CVD.)
Why you said “Keys was interested in CVD mortality…so am I.” ?
Why you keep exhorting us to read Keys’ “Eat Well and Stay Well?” That monument to low-sat fat eating? Which came out the same time of his Seven Countries Study that correlated CVD and sat fat?
Why you said “Keys interest in heart health went way beyond population studies. His 1959 book Eat Well and Stay Well is essentially a practicum on how to eat and live in order to reduce CVD risk.”?
Why you said “This is where Keys was coming from. Direct observations of bad diets resulting in bad CVD outcomes.”?
Is that why you at least twice link us to Citizen Blogger Dixon, who claims to quote Keys here: “…the efforts to lower total dietary fat, and especially to lower dietary saturated fat, were indeed successful in reversing the epidemic of deaths due to CHD…”?
And on.
Thhq, sure thing. Whatever you say!
LOL!!!
–Bryan
Thhq, in this forum, you’ve often cast doubt on “Low-Carb High-Fat.”
Just curious: How do you define LCHF? Whose def do you go by?
Does your def even include percentages for the intake of the macronutrients (i.e. fat, protein, carbs)? If so, what are those percentages?
Thhq, I don’t ask rhetorical Qs here. I’d truly like to learn your operating def of LCHF. And from where you got your LCHF def.
Thanks –Bryan
@ heather, just picked up a tidbit on taurine and oysters….believe this was an Indian study….
“Taurine
The freely occurring β-sulphonic amino acid, taurine was estimated using high performance liquid chromatography. Figure 1 and Figure 2 show the chromatogram indicating the peak and retention time of taurine standard and taurine content in the oyster sample, respectively. The taurine content is high in oyster meat 243 mg/100 g (Table 6) which is significantly higher than that of fish 40–85 mg/100 g (Divakaran, 2006). The ratio of taurine to cholesterol is an important index in foods and higher ratio is beneficial to the consumer (Choi et al., 2006). Taurine:cholesterol ratio is 2.3 in oyster (Table 6). Among taurine’s many natural functions in living systems, is its hypocholesterolemic effect (Rijssenbeek et al., 2006). Taurine acts by conjugating bile acids that are formed from cholesterol synthesised in the liver and excreting them through bile. To replenish the excreted bile acids more endogenous cholesterol is converted to bile acids which results in lowering of cholesterol in the body. Thus taurine exhibits a hypolipidemic effect by stimulating hepatic bile acid synthesis from endogenous stores of cholesterol (Ogawa, 1996).”
http://www.sciencedirect.com/science/article/pii/S168742851400020X
The highest content taurine food I’ve found so far is cottage cheese at 1700mg per cup.
http://suppversity.blogspot.com/2010/08/taurine-from-foods-can-i-be-taurine.html
“Taurine:cholesterol ratio is 2.3 in oyster (Table 6). Among taurine’s many natural functions in living systems, is its hypocholesterolemic effect ”
Oh, and oysters taste SOOO much better than statins! (LOL!). Thanks for the link!
Whey is loaded with taurine, so a lot of those ancestral foods have it. I expect that’s why the switch from seafood to dairy worked ok in Europe. Most Americans don’t eat the high-whey foods these days though. Unless they are body-builders! Also there is more taurine in goat milk (like 20-40 times as much!) than cow milk. I can’t do either dairy myself, it gives me migraines, but sometimes I have goat cheese.
Click to access SRR08pre-pub.pdf
There is a sign on my doctor’s office that says basically, if you are diabetic he expects you must be on statins, period. He’s a smart and honest guy and I expect that it agrees with what he’s studied, but sheesh. That’s the best he knows.
The one caveat I have with shellfish though is the high iron content. In terms of diabetes, iron actually can cause diabetes and likely IS the cause of a lot of it. The shellfish work in the ancestral diet, and in the Asian diet, because the shellfish is paired with iron blockers … tea or seaweed or both. In other places, shellfish usually is paired with milk (clam chowder! Slices of cheese!) which also acts as an iron blocker. Or whole grains, which are big iron blockers. Chili blocks iron too. I sometimes just pop an IP6 if I feel the meal is just too irony. IP6 also blocks other heavy metals that shellfish sometimes accumulate.
Vit C makes iron hyper-absorbable though, so pairing oysters with oranges or tomatoes isn’t great.
One thing I’ve noticed since I’ve been taking taurine is that my poo is back to being very brown, even though I’m still doing the low-fat experiment and not eating beef or pork. My thoughts are yes, it just triggers your liver to produce plenty of bile, do a little house-cleaning maybe! However, with the taurine I’d think it gives your liver more of a choice in regulating the level in your blood, than the statins that just restrict production.
Costco sells big jars of pre-shucked oysters for a good price. Whenever we go there I get a big jar and we have an oyster-feast. But you can also just freeze them on a cookie sheet, which makes it easy to just toss a few into a soup or phad thai. The Asian store also sells mussels prepared just that way, frozen. Or frozen seafood mixes that have mussels, oysters, squid, octopus, and shrimp all mixed up. I just make my rice noodles however I like them, then toss in the seafood at the end so it doesn’t overcook. Cracking an egg into the hot mix makes an “egg flower” kind of effect too, and adds flavor.
Prompted by a cook at a Thai restaurant, I bought some “red curry paste”. It lasts forever in the fridge. You add a spoonful of that and some thickener (sweet rice flour is what I use, like Mochiko or just grind up some raw sticky rice) to your liquid, and some coconut milk, and you have instant Thai Red Curry. Nom! Apparently that is what they do in a lot of Thai places.
Thai kitchen makes it too, which is for sale pretty much everywhere. That gives you the chili iron-blockers plus all those good herbs. There is a Tom Yum paste too, which is similarly awesome. Thai kitchen is ok, but costs quite a bit more and seems less authentic than the more Asian versions. They are all pretty good though.
http://www.ncbi.nlm.nih.gov/pubmed/17116705
I love Thai food, but they never give you enough of the seafood part of it in my opinion.
@heathertwist I whipped up an old family recipe over the hodays for my mom. Eggost, or sweet egg cheese. A quart of buttermilk curdles three quarts of simmering milk mixed with half a dozen eggs and sugar. The curds are strained and squeezed (we throw out the sweet green whey) and eaten on the dry side, topped with some cinnamon. There must be a huge load of taurine in this, along with all the protein.
When the eggost is gone I’ll be eating more cottage cheese. A wonder food I’ve neglected for a few years.
The combination of cheese and oysters….grilled cheese-topped apalachicolas on the half shell…mmmm….anywhere, anytime, from the Florida panhandle to New Orleans….
There is probably a good shot of taurine in it, but it’s good to keep in mind that most of the taurine goes with the whey! That’s the problem with taurine. It’s water soluble, so as soon as you boil something, the taurine often goes with the water.
Cottage cheese is “curds and whey” so includes the whey. One reason it has more goodness, like taurine. I don’t know how to keep more whey in recipes though. I think Greek Yogurt adds whey to it. Or you can save your own whey:
http://blog.radiantlifecatalog.com/bid/62826/Homemade-Whey-vs-Protein-Powder-Rediscovering-nutrient-dense-foods
Whey has the lactoferrin too, which is good stuff!
Custards of various sorts were regarded as wonder foods of sorts in the old days. Great way to get protein and easy to feed a picky kid or a person who can’t chew well.
@ bryan here’s how I defined LCHF. This was adequate to get my blood sugar and T2 diabetes under control. I didn’t need to go any further than this, and after I had lost weight and started exercising I didn’t have to worry about it at all too keep blood tests, lipid sizes and level, and triglycerides at normal levels.
Click to access CountingCarbandMeal_EG.pdf
If you can follow this carb counting method, and I did for two months, calorie counting is child’s play.
If you want one of my snarky definitions of LCHF, it’s “a class of people that rejects calorie counting as satanic”. And that makes pretty good sense because Keys (aka satan, another fervently held belief of the LCHF community) promoted calorie counting for weight loss. He called it Scientific Reducing and describes it in detail in Eat Well and Stay Well. [No, I’m not typing the chapter out for you, and why would you trust me not to cheat?].
@morgana, thanks for the link.
@heather the taurine connection certainly is interesting! IMO, the easiest place for ancestrals to live was on the coast. I like to go on at length on why I think mollusks and crustaceans are key foods. Natural vitamin and mineral supplements!
Thhq, you realize you utterly fail to define LCHF for us in any way?
You routinely cast doubts on “LCHF.” Yet you can’t even tell us what it is.
I’m sorry. But that’s ridiculous.
–Bryan
I’ll try one more time and that’s it @bryan. Your dedication to LCHF has cured your problems, and you daily undergo the restrictions necessary to stay on LVHF. I used the linked method because I wanted to fix my diabetes yet still eat what I’ve always eaten. I didn’t want GT, Atkins, Eades, Cordain, Sisson or ketostix to dictate what I eat. I’ve supplied you with the low carb method I used to cure my diabetes. It has a wide range of nutrient combinations, with millions of meal possibilities, giving a very wide range of carb and fat levels. I used this method for six months, got my health back, and have maintained a healthy state for 8 years. I no longer use carb counting. I don’t need to.
In one sentence here’s my definition of LCHF:
Low enough carbs to fix the problem.
That’s what the answer to my problem (diabetes) looked like when I did it for two months in 2007. It brought my blood sugar down from 200 to 100 fasting in two weeks.
Thhq, again. You truly don’t have to try to explain anything you don’t want to explain. Please don’t force yourself on my account.
You tell me “…you daily undergo the restrictions necessary to stay on LVHF…” Oh really? I’ve made clear here that I love my food- and lifeway. My food has wonderful complex flavors and is completely satiating. With keto I can eat or not eat. I’m completely free of a schedule. I don’t “count” anything. Even my food bill dropped to an absurdly low level.
Thhq, I truly have never felt more liberated. If I suffer “restrictions,” I sure didn’t get that memo!
About the “linked method” Thhq what do you mean by that?
You say “I didn’t want GT, Atkins, Eades, Cordain, Sisson or ketostix to dictate what I eat.” Fine Thhq. Then don’t. Just please don’t inveigh against what those people and things offer *unless* you can give us credible evidence to back up what you say. That’s all I respectfully ask. Plus, what works for you doesn’t necessarily work for another person.
You say “I’ve supplied you with the low carb method I used to cure my diabetes. It has a wide range of nutrient combinations, with millions of meal possibilities, giving a very wide range of carb and fat levels…”
Thhq, can you see why I finally asked you to get done to brass tacks and *define* what you mean when you say “LCHF?” I don’t recall that your “low carb” method is all that low in carbs. But I’m willing to accept we can have different ideas what is “LCHF.”
So Thhq I repeat the Q: What’s *your* def of LCHF? You cited Cordain’s macro percentages. It seems reasonable to ask you for actual numbers. To simply say “Low enough carbs to fix the problem” is vague in the extreme. What protein % do you propose? What’s fat % do you propose? You completely ignore the HF portion of that equation.
Again Thhq, you can choose to answer this or not. It’s all the same to me.
Finally you never explain why one should leave “LCHF” once one “fixes the problem.” For me Hyperlipid’s Peter best sums up the matter:
http://high-fat-nutrition.blogspot.com/2014/11/the-p479l-gene-for-cpt-1a-and-fatty.html
“I’m always amazed by the concept that a ketogenic diet might be temporarily therapeutic but must be discontinued because it eventually becomes Bad For You. It reminds me so much of the converse concept that low fat diets, which might worsen every marker of health which people may care to look at, will deliver major benefits at some mythical future date.”
Again Thhq, please don’t bother to explain anything you don’t want to. All I say is that if you care to appear credible, you should at least know what exactly it is you judge. You rail against Good Calories Bad Calories. Yet you never read it. You rail against LCHF. Yet you can’t even define it.
You rail against things you don’t know. What are we supposed to think about what you say? –Bryan
Two months, six months whatever…I did the carb counting for two months to get the blood glucose levels normalized, then switched to calorie counting for weight loss for the next four months. Calorie counting did not restrict high glycemic foods, which were no longer raising my glucose tests. The high glycemic carbs supplied the calories I needed for my increasing use of exercise to generate 1000 calorie per day weight loss calorie deficits.
If you had been motivated by type two diabetes @bryan maybe you could understand what I’m saying. Carb counting moves a person away from eating high glycemic carbs to lower their blood sugar. This is done by changing the type of carb eaten, andy in most cases by also lowering the total number of calories eaten as well. It is not set up to do what you’re doing. Whether it raises dietary fat is up to you, and it can if you want it to, but that’s beside the point. It works without the HF, but not without the LC, and the LC doesn’t have to be lower than it needs to be to control blood sugar.
I’m sorry this isn’t black-and-white. It’s not simple to understand and execute, and I spent a lot of time digesting the pamphlet I linked and put it into practice. Meal planning, diary keeping, the whole deal. The only reason I succeded at it was because I was motivated to do it. The thought of diabetic ulcers on my feet – losing the ability to walk – scared me more than anything.
???
Thhq! I discussed my Type 2 Diabetes *dozens* of times here, which includes how I retreated from it. I discussed this with you!
You honestly don’t remember we talked about this?
Thhq, really, it’s OK if you can’t define LCHF for us. Just, if you would, please stop running down this mysterious thing you call “LCHF” when we have no concrete idea whatsoever you even mean by “LCHF.” That’s all.
And I’m really and truly glad you found a system that works for you to drive your T2D into remission. Whatever we discuss here **that’s the most important thing.** You did a wonderful thing for yourself and your family. –Bryan
@bryan over 35% fat is high fat. OK with that? Would you be happier if I said 60%? I’ll say that if you like. 80%? Great by me.
It’s not like I don’t understand what you do. But you seem to be completely incapable of understanding that for what I did the % fat in my diet was and is unimportant, and I’ve arrived at the same state of health as you.
There are different ways to control diabetes. LCHF was your method and it works. Counting carbs was mine and it works. I’m only persistent about this because I thought you might want to know how carb counting worked.
“…incapable of understanding…”
Thhq, I’d say that fits.
I can’t understand how you can assert “I’ve arrived at the same state of health as you” when you don’t do all the health measures/tests I do. And you don’t know my complete medical history.
I can’t understand why, when asked for the fat% for your def of LCHF, you suddenly think we’re talking about your own therapy diet.
I can’t understand why you persistently deride “LCHF” yet stoutly resist to define “LCHF” for us.
Thhq, I’d say to understand all that requires a special kind of understanding. One I don’t have.
Guilty as charged.
–Bryan
My gosh. Rivers of words have flowed on multiple topics here, and this is the first place I can find a relevant “Reply” hook. When will Part 2 of Minger’s article appear? A blank slate is needed.
Anyway, I’ve been collecting mollusks and cottage cheese. It’s high crab, clam and oyster season around here. Steamers in wine/garlic/butter, hangtown fry, smoked oyster snacks, crab salads and melts, and a half cup of cottage cheese every day. A superabundance of taurine. Maybe there’s been some sort of benefitn over the last month, but what I’m hoping for is long-term increases in shoulder and thigh muscle mass.
I just read through the N=1 reviews of people taking taurine supplements on webmd.
http://www.webmd.com/vitamins-supplements/ingredientreview-1024-TAURINE.aspx?drugid=1024&drugname=TAURINE
The reported benefits are reduced migranes, especially in conjunction with msg consumption. Also reduced palpitations and arrythmia in older people. I don’t have problems with these issues. But I wonder whether as we age, do we lose our ability to make adequate taurine?
You ask: “I wonder whether as we age, do we lose our ability to make adequate taurine?”
Thhq, that’s one of the many Qs we’ve been batting around. Per my 18 Jan post to Heather (search on “hypotaurine”), we make taurine from cysteine and methionine, two of our 20–23 proteinogenic amino acids, so super common. The conversion needs only two enzymes, three max. So seems on the face, we should have little prob to make all the taurine. But if this follows the usual biochem pattern, it’s likely more complex than that.
Maybe the taurine queen(s) will weigh in. –Bryan
Or maybe we just need more as we age. There seem to be benefits to extra taurine though, to all age groups. They are saying now that our ability to create it is “limited”. Anyway, we eat a fair bit of seafood, but my 21-year-old daughter reports that since she started taking T, she can be on her feet all day without her feet hurting. She used to come back from work barely being able to walk.
With all that seafood though, I doubt you would need extra. Plus if your diet is often like that, I’d think you have always had plenty. The people I wonder about are say, my inlaws, who believe fish is toxic and don’t like the smell of it in any case, and live off overcooked beef and potatoes. They are not aging well.
I’m looking forward to part 2 also! I fell down this verbose rabbit-hole when I tried following a very-low-fat diet as a response to part 1 … which led to a big difference in bile production it seemed … etc. etc.
“Fish is bad” sounds like the old midwestern malady. We ate a lot of lake trout and whitefish when we lived there, which were fresh when you could get them.
There’s tons of anecdotal evidence for taurine’s benefits as a bodybulding supplement, which is where I hope it leads. But with that group there’s no end of supplements, and it’s hard to tell what taurine does on its own. Interesting about the foot pain reduction, maybe it’ll do something for my tendinitis.
Jonathan, I’m with you here. I wouldn’t be surprised to learn cigs are the 900-pound gorilla of 20th cen enviro pathologies. When I was born (1960) just about everyone inhaled loads of cig smoke. Manufs jam all kinds of horrible stuff in their cigs, knowing they don’t have to reveal the ingreds:
http://www.lung.org/stop-smoking/smoking-facts/whats-in-a-cigarette.html?referrer=https://www.google.com/
The US made huge strides to get Americans to cut down/quit smoking. That one factor could way WAY overshadow all other efforts to make our enviro healthier–including our food and synthetic food-like substances. Jonathan, we started putting HFCS in edibles in 1975. Can anyone seriously infer from correlation that HFCS contributed to “steadily lowering CVD?” –Bryan
Lol – sadly, the cholesterophiles have done more with less!
Funny, what gets lost in all this, the Seven Country Study (iirc) correlates CVD only with *serum* cholesterol, not *dietary* cholesterol. But since dietary c’stol comes just from animal sourced food, many folks started to correlate dietary c’stol with CVD since it so often travels with sat fat. Even the gov’t put a recommended limit on it (300mg/day). But it’s set to lift that limit soon. –Bry
Should I hold my breath? Honestly Bryan these tossers have had their chance and failed miserably, yet almost nobody is paying attention – putting your faith in these guys coming right probably isn’t in your best interests
Jonathan, for sure, the wheels of change now turn. I feel similar, what you say “…almost nobody is paying attention.” Like I discuss elsewhere in this forum (search on “is today’s Crowd getting the upper hand?”), we see a fascinating new kind of split between the Authorities, the “Experts” and the Crowd Wisdom. E.g. on wheat. I don’t know that I’ve seen such a powerful popular movement away from anything like I see from wheat. This, despite gov’t/mainstream consensus science who endlessly intone their assurances that wheat/gluten only nourishes us and doesn’t hurt us. –Bryan
Ancel Keys smoked cigarettes and a pipe occasionally, but at some point quit…probably when he determined that it was unhealthful…
IMO there’s loads wrong with with living in an igloo and eating seals too @Bryan. Do like Keys and live out your belief. Hypothermia, 100% human-powered transportation, autophagy, semi starvation. The WHOLE Greenland circa 1900 package. Not just the selected dietary bits.
Living a healthy life to age 100 is the goal, not playing nih trump cards on each other.
Thhq. You do realize your response makes no sense? –Bryan
In view of what you expressed earlier in this thread about the healthiness of pre 1900 Inuits,
“I also haven’t heard of fasting issues in Inuit adults, and would like to learn how they adapt to fasting as Inuit grow older. Given their huge and harsh environment and often subsistence diet, it’s very hard to imagine the Inuit are always snacking all the time. It’s likely there were plenty of times they had to go hours or even days without eating anything.”
the easiest way to find out about those fasting issues would be to live the life. It makes perfect sense to me that you walk the walk. You need huge and harsh environment to run your N=1.
Like Ancel did in Italy. You couldn’t test the healthy country theory living in Minnesota in the 1950’s.
Thhq, what you say here is incorrect. My question about Inuit adult fasting didn’t relate at all to pre 1900 Inuits. (See your quote at post bottom.)
But since you brought it up, I *do* in fact “live the life.” To the extent practicable.
For example, I just finished an 88-hour (3-⅔ day) fast. I can honestly say it was fantastic. By around 50h, my whole body felt exquisitely finely tuned. I felt a heightened sensibility without undue sensitivity. I felt very calm and yet my thoughts flew along in a nice tight formation, and I made surprising and delightful cognitive connections. I felt this fine response in my toes, fingertips, my lips–everywhere.
I eat a LC diet just like the Inuit. I eat a lot of seafood, esp cold-water high w3 fish like salmon. AMAP, I source my foods organic/pesticide-free, locally, in season, and as herloom as possible, aligning with those common aspects of the ancestral Inuit diet.
And you know what Thhq? I learned firsthand a high-protein might not be disastrous after all! For four months (Aug–Nov 2007) I ate a very high protein diet, up to 300g per day, very similar to that which some ancestral Inuit ate at least episodically. I didn’t know about Inuit foodway at that time. I went high protein only because I HAD to cut carbs to lower BGs and I still lived in a stark and senseless terror that dietary fat would “clog my arteries sure as bacon grease clogs the sink drain.” During those four months, I got up to half my calories from protein. I felt fine and had plenty of energy, none of lassitude you hear about with the “rabbit starvation.” Only the diet *was* dull, a few friends mentioned my ammonia breath, and I had to pee 3–4x/night so my deep sleep suffered. By Nov I started ramping up the dietary fat with plenty of blood panels and never looked back.
It always mystifies me that people–you the latest, Duck Dodgers earlier–assert that somehow we can’t derive valuable lessons from other people’s foodways unless we take the “all or nothing” approach. It’s just plain silly to suggest that we need to move to the high north, live in igloos, and eat maktaaq, that we can’t take macronutrient cues from the Inuit. That if we do LCHF we’ll board the Cannonball Express to Horrible Death with evil yellow lipid paste oozing from our pores. I makes no sense to suggest it’s somehow “dishonest” if we dial down the protein in our LCHF, not to stay “true” to some mythical “pan-Inuit” diet that all these people all round the circum-Arctic purportedly ate. Just because (at least some) ancestral Inuit ate 50% fat/35% protein, doesn’t mean I won’t do just peachy on an 80% fat/15% protein diet. It’s been over 8.5 years, I’m 55, and I still do peachy on it! –Bryan
———————
Thhq’s quote:
“In view of what you expressed earlier in this thread about the healthiness of pre 1900 Inuits, [Bryan quote follows]:
‘I also haven’t heard of fasting issues in Inuit adults, and would like to learn how they adapt to fasting as Inuit grow older. Given their huge and harsh environment and often subsistence diet, it’s very hard to imagine the Inuit are always snacking all the time. It’s likely there were plenty of times they had to go hours or even days without eating anything.’ ”
Thhq, not even exactly sure where you got the pre 1900 Inuit thing from. But maybe when you asked me this?: “Guyenet’s information on traditional Inuits comes from the early 19th century… What do you know on this subject?” –B
What would be different about pre 1900 @Bryan? It needs to be pre-modern, and modeling it to Inuit life pre 1900 would probably do it. I don’t know what time frame you referred to in the comment I quoted, but earlier you spotted the oldest age survivors Guyenet cited from the early 19th century Russian census data. If you applied modern medical practice to that lifestyle you could very well live to 100. But don’t discount the effects of cold, upper body strength and maybe even frequent snacking – these could be on a par with any macronutrient effect. As with Keys, who could not possibly have guessed all the differences in living in Italy vs Minnesota, you have to live it out. Moving from a nation with polyunsaturates and canned peas to a nation with monounsaturates and fresh produce appears to have changed his diet. I lost a lot of weight living in France for 2 years, eating all I wanted of bread, pasta and desserts. 6 years later, having gained it all back in the USA eating the same way, it dawned on me that I needed to stop being so sedentary. Walking everywhere for transportation was the one of the biggest differences.
Thhq, they don’t need to be pre 1900. Pockets of Inuit lived ancestrally well after that including some that Bang and Dyerberg studied in the ‘70s in far northern Greenland. They too experienced “…the effects of cold, upper body strength…” as you say. About frequent snacking, I’m far from convinced that Inuit typically had to do this. No-one’s posted hard data on that for the entire cohort. That “68% have the ketone-deficiency gene” thing that supposedly drives frequent eating, that comes from researchers who gene-mapped only *25* First Peoples, possibly only a third of them–8 or 9–Yupik (Siberian Eskimo):
http://www.sciencedirect.com/science/article/pii/S0002929714004224
It’s a very small and localized sample. We can hardly generalize it to all the Yupik-Inuit scattered around the circum-Arctic. Sure we have anecdotal evidence of this in Alaskan and Canadian Inuit, but I haven’t seen data that tells how prevalent it is among them.
About their physical exertions being “…on a par with any macronutrient effect…” that may be true for some people, like you Thhq, but certainly not true for others, like me. I cycled 150-miles/day and ran half-marathons and still got love handles and T2D. For me the food matters hugely. And it may not just be macros, but other factors, like how the food’s processed and the endocrine disruptors and other toxins within it. Each person has to test him/herself with as many health metrics as available, and tailor the therapy accordingly. –Bryan
Ancel Keys didn’t ignore the Inuit diet. Here’s what he had to say about it in 1959 (Eat Well and Stay Well, pg 149):
“That brings us to the Eskimo, who is pictured as living entirely on seal fat and walrus blubber and seldom falling ill unless he is exposed to the infectious diseases of civilization. Actually, only very few Eskimos now eat the primitive arctic diet and nothing is known about their tendency to develop atherosclerosis and heart disease. The primitive Eskimo does not know his own age, but few of them attain the “ripe old age” of 50 years. Pneumonia, tuberculosis, and the accidents of hunting and fishing in the frozen North eliminate them before the age when coronary heart disease might be a problem. Moreover, the primitive Eskimoes never eat beef, pork or dairy products, and most of the fat they eat is of the highly unsaturated type in fish and marine mammals. Even the land mammals they eat, the caribou and reindeer, are not comparable to the meat animals of warmer regions. For example, the fat of the arctic land animals tends to have a low melting point, which suggests it is unusually low in saturated fats. So primitive Eskimoes teach us little.”
I don’t like his last comment, because I learned a lot reading this. Keys was preoccupied with CVD, and in that sense there’s not much to be learned. He’s onto something about the Inuit eating no dairy and lean meats, lower in saturated fats than beef and pork. This gets amplified by Cordain in his Paleo Diet.
Thhq, Keys took us down a dreadful path and the only time we should spend on him is for its historical lesson, to let us appreciate what is perhaps the most tragic example ever how Big (or at least Gov’t) Science in those early years, and how political process greatly perverted it, got things spectacularly wrong. Keys’ work, like his 1958 Seven Countries Study and the 1959 book you refer to, is outdated, woefully incomplete, and fell far short of rigor needed, resulting in wrong conclusions, esp the advice to reduce saturated fat. His work hopelessly lacks granularity–fails to “find the devil in the details”–in part because we simply lacked the knowledge to analyze the nutrients in proper detail. Keys concludes, in official reports he co-signed, e.g. this one:
Click to access 133.full.pdf
“…The reduction … of fat consumption…with substitution of poly-unsaturated for saturated fats, is recommended as a possible means of preventing atherosclerosis and decreasing the risk of heart attacks and strokes…”
Keys speaks only of “saturated fats” and “poly-unsaturated fats” and utterly fails to distinguish between the vast differences of the fats we find within. For example, our bods metabolize SCFAs like butyric acid (C4) much differently than longer chain SFAs like palmitic acid (C16) and stearic acid (C18). Same problem with the polys. Keys fails to discuss the diffs between w6 polys which are pro-inflammatory, and w3 polys which are anti-inflammatory. Plus, the Seven Countries Study is purely correlative and fails to take into account many confounders like the average energy each cohort expended. The Study covers the cals-in part, but not the cals-out part.
That above report to the AHA fails even to completely align with the results of Keys’ own Seven Countries Study, the latter in which he correlates CVD only with *saturated* fat. This shows that Keys not only promulgated broken science, he was willing to perjure himself.
I have to be very skeptical about what Keys said about anything at all, including the Inuit. Ignorance, and political and even pecuniary interests perverted his work. Keys apparently didn’t know about the far northern Greenland Inuit, from Qaanaaq and in that region, who lived largely ancestrally. Those Inuit that Bang and Dyerberg studied in the 70s. Those observations taught us a great deal. –Bryan
What did Keys say that contradicts Bang and Dyerberg? Keys has identified two low SFA sources of lower SFA ruminant fat – reindeer and caribou – which I’ll now be looking for at my grocery store.
Keys position on fats changed with time, and he eventually settled on olive oil as optimal. Yet even in 1959, Keys had a great disdain for both margarine and feedlot meat. That’s remarkably progressive I think. He was pointing us toward open range and grassfed as optimal animal fat sources.
Your zeal to discredit Keys’ dreadful path is only matched by my zeal to discredit GT’s. I remind you once again that my interest is in a path that ends at 100 years. GT’s contrarian views always seem point us back to Atkins well-traveled and fat-laden path.
You ask: “What did Keys say that contradicts Bang and Dyerberg?” Thhq, if you actually read my post, you wouldn’t need to ask this question. The answer’s already there.
You say: “Keys position on fats changed with time, and he eventually settled on olive oil as optimal. Yet even in 1959, Keys had a great disdain for both margarine and feedlot meat. That’s remarkably progressive I think. He was pointing us toward open range and grassfed as optimal animal fat sources.”
Thhq, Keys’ changing fat views being the case, why do you keep going back to his 1959 book?
You say: “Your zeal to discredit Keys’ dreadful path is only matched by my zeal to discredit GT’s. I remind you once again that my interest is in a path that ends at 100 years. GT’s contrarian views always seem point us back to Atkins well-traveled and fat-laden path.”
Sure Thhq. You’re certainly welcome to your opinions. And I applaud your longevity goal. Only, why stop at 100 years? –Bryan
Well, wbryanh, if I had read the 1970’s version (EH & SH the Mediterranean Way) I wouldn’t have found out anything about reindeer and caribou. In 1959 Keys was kinder and gentler towards meat than he was later on. There’s a great bone broth recipe in that book too…shades of Paleo things to come…
I dug a little deeper into Keys genealogy and discovered that his parents lived to their mid-70’s. I had been told that they were relatively long-lived, but had expected octogenarians at least. His uncle and cousin (Lon Chaney and Lon Chaney Jr.) weren’t particularly long-lived either. So genetics doesn’t look like a big factor in his longevity.
Thhq, about Cordain. In “The Paleo Diet” (2010) on page 11, he makes the ranges so wide for the three “diets” he compares:
Macronutrients: Protein / Carbs / Fat
Paleo Diet 19–35% / 22–40% / 28–47%
Typ US diet 15.50% / 49% / 34%
LC fad diets 18–23% / 4–26% / 51–78%
he renders their distinctions mostly meaningless.
He pretty much lost me at that point. –Bryan
Cordain’s Paleo Diet has six rules. Macronutrients fall where they may, based on eating unlimited fruits, non-starchy vegetables and lean meats.
Thhq, maybe you and I have diff ways to do math. But I don’t see six rules there. I see maybe three? –Bryan
Page 23 wbryanh. I thought you bought a copy. Three rules on what to eat, three rules on what not to eat.
Thhq, you say: “I thought you bought a copy…”
Sure. You may *think* that. But where do I say that? Right. Nowhere. I got it from the library.
I get to page 11 and see his macro balance ranges as broad as barns. When I saw that, in the category he derisively terms: “low-carb fad diets” that you can actually have a *higher* carb count (26%) that on the “Paleo Diet” he promotes (22%), well that was it. Back to the stacks with that puppy.
About the Six Rules, thhq, well *you’re* the one flogging Cordain’s book. If you don’t want bother to support your claims, that’s fine with me. Won’t give it another thought. –Bryan
One of the benefits of population studies is getting a very high view of a situation. I used multiple regression analysis, even on relatively small data sets, so that I could sort out important effects from trivial ones. The same applies to national studies. You don’t catch what you can’t measure (like the importance of Omega 6 vs Omega 3 ratio using 1950 measuring technology, or the paleoanthropology of as-yet undiscovered sites), but you can describe the broad observable effects, such as the high CVD rates in East Finland and lack of fresh fruits and vegetables in that diet versus Italy.
I’m finally reading The Paleo Diet. Other than the heavy emphasis on eating amounts of lean animal protein and the avoidance of grains, almost everything Cordain wrote is in accordance with Ancel Keys approach to healthy eating. It’s refreshing to read work by another enthusiastic and well educated academic researcher.
Practically nothing that Cordain wrote supports HFLC dieting. In fact he calls it out as being as unhealthy as vegan/vegetarian/SAD. According to his principles, the first law of thermodynamic is not suspended (though protein is an advantaged nutrient, it’s still calories in/calories out), ketosis is not mentioned (nor is it likely to occur on the Paleo diet), sodium is completely removed from the diet (throw away your salt shaker) along with most saturated fats (especially palmitic). Processed meats and butterfat are taboo. The accepted theories for heart disease are not scorned.
I couldn’t do it, though I can draw a lot of useful diet advice from this book, particularly eating more animal and seafood protein. But Cordain hasn’t convinced me give up my BLT and chips!
Really Thhq?! What you say here:
“Practically nothing that Cordain wrote supports HFLC dieting. In fact he calls it out as being as unhealthy as vegan/vegetarian/SAD…”
Got an actual Cordain quote for that?
Thhq, which version of The Paleo Diet are you reading? The 2002 ed? Or the Revised Paleo Diet book, pubbed in 2010?
If you’re going to source someone please make sure you at least get their *current* positions on the subject.
Per this interview (cue to 23:00):
http://www.dietdoctor.com/paleo-interview-with-professor-cordain
Cordain weighs in favor of dietary sat fats, or at least feels they are benign (in the absence of carbs). He says he reversed his formerly negative position on sat fats in 2004–2005.
Again, Thhq, please give us *actual quotes* OK? Not just your special spin on what other folks supposedly said.
I never got the idea that Cordian inveighs against LCHF. In this piece:
http://discovermagazine.com/2004/oct/inuit-paradox
That author gives this from Cordain, (albeit not shown in Cordian quotes)
“What’s equally striking, though, says Cordain, is that these meat-and-fish diets also exhibit a natural ‘protein ceiling.’ Protein accounts for no more than 35 to 40 percent of their total calories, which suggests to him that’s all the protein humans can comfortably handle.”
Thhq, please do the math here. Some ancestral Inuit eat virtually *no* carbs. If our protein intakes must peaks out at 35–40%, then that leaves 60–65% fat.
Hmm. 65% fat. 35% protein. Near zero carbs. Sure sounds like LCHF to me!
And nowhere I read Cordain to deem “the Inuit diet” an unhealthy foodway(s).
And Thhq please don’t trot out the tired vague totally unsubstantiated yada about how the “Inuit are different from us,” “We can’t use the Inuit foodway as a proxy, etc.” Been there done that. Ate the can of skin-and-bone salmon soaked in olive oil. –Bryan
You’re still not getting what I said about writing abstracts earlier @Bryan. Obviously you don’t trust my judgement, and you’re not going to trouble yourself picking up a copy of The Paleo Diet and reading it, but here we go with the long form. The pub date is 2011, if that makes a difference.
Regarding HFLC, Cordain is promoting his 19-35% protein, 22-40% carbohydrate, 28-47% Paleo Diet on Page 11. After the tabular comparison of Paleo, Typical US, and Low-carb fad diets he writes
“Modern low-carbohydrate weight-loss diets are really high-fat diets that contain moderate levels of protein. They don’t have the high levels of protein that our ancestors ate – the levels found in the Paleo Diet. Actually, compared with what our ancestors ate, the carbohydrate content of these modern weight-loss diets is far too low. Even worse, almost all of these low-carbohydrate diets permit unlimited consumption of fatty, salty processed meats (such as bacon, sausage, hot dogs, and lunch meats) and dairy products (cheeses, cream and butter) while restricting the consumption of fruits and vegetables. Cancer-fighting fruits and vegetables! This dietary pattern is drastically different from our ancestors.”
This particularly calls out Atkins and his acolytes with their processed foods, but Cordain is also not giving any support to salt in the diet (he goes on about this later), nor to a carbohydrate level below 22%.
I compressed this and abstracted it in one sentence, but it didn’t hurt me to read it again to verify that I had summarized it correctly the first time. Contrast that actual quote with the “quote” you cribbed from secondary sources and posted above:
“That author gives this from Cordain, (albeit not shown in Cordian quotes)
“What’s equally striking, though, says Cordain, is that these meat-and-fish diets also exhibit a natural ‘protein ceiling.’ Protein accounts for no more than 35 to 40 percent of their total calories, which suggests to him that’s all the protein humans can comfortably handle.”
Thhq, please do the math here. Some ancestral Inuit eat virtually *no* carbs. If our protein intakes must peaks out at 35–40%, then that leaves 60–65% fat.
Hmm. 65% fat. 35% protein. Near zero carbs. Sure sounds like LCHF to me!”
In future I’ll be taking my Cordain straight, without your chasers. Check your own math against Cordain’s published ranges for Paleo macros. 22-40% carb is not, as you calculated, near zero carbs.
Well, this is what I found online about the Paleo diet:
http://thepaleodiet.com/carbs-wreck-the-brain/#.VoHJy1Jl9DU
It’s not exactly anti-low carb/high fat, I would say.
@morgana, I got Cordain’s book as a gift. Now that I’m reading it I understand where he’s coming from in the blog link. He rejects cereals such as the spaghetti shown (Ground Rule #3). But if you’re not eating 22-40% carbs you’re not eating Paleo.
From Page 23, Ground Rule #2 of the Paleo Diet:
“All the fruits and nonstarchy vegetables you can eat.”
Get a copy and learn what the other five Ground Rules are.
Thhq, about what you say here “Obviously you don’t trust my judgement…” Please don’t take it personally, but no I *don’t* take your say-so–or anyone’s say-so. Nor should any of us. I ask for links from everyone. Even from people who feel the same or similar as I toward a given topic. Why should you get special treatment? Why should I trust you? I don’t even know who you are. And as far as what you say: “…you’re not going to trouble yourself picking up a copy of The Paleo Diet and reading it…” Thhq, uh-uh. That ain’t how it works. YOU make the claim, YOU supply the evidence. You shouldn’t spout claims and then expect us to do your work for you. That said, if I disagree with what you say, then of course it’s up to ME to do the rebuttal research. I make every effort to back up the claims I make with quotes and citations. That’s only fair, no?
Thhq, you continue to validate my “demanding” approach for genuine evidence. In the main, your quote fails to support what you say here:
“… In fact [Cordain] calls out [LCHF] as being as unhealthy as vegan/vegetarian/SAD…”
First, where does Cordain compare LCHF to “vegan,” “vegetarian,” or “SAD?” Right. NOWHERE. Did you simply invent that comparison? Cordain does rail against certain foods like “…fatty, salty processed meats (such as bacon, sausage, hot dogs, and lunch meats) and dairy products (cheeses, cream and butter)…” But he doesn’t call him SAD. Probably because not all charcuterie and dairy qualifies as SAD. Cordain fails to note the huge variety of quality and nutrition you find within these foods and their much diff health implications. E.g. an artisanal pastured-sheep cheese from the Pyrenees has a vastly different profile from a slices of Kraft processed cheese; uncured bacon from pasture-raised high-fat Mangalica hogs will be much diff from the mainstream nitrate-laden Smithfield strips from high-protein industrially-raised hogs.
Thhq, you asked me to “Check your own math against Cordain’s published ranges for Paleo macros.” I did. Guess what? Cordain’s “Paleo Diet” can come pretty close to LCHF. Even *be* LCHF in some people’s views.
Cordain’s “Paleo Diet” ratios–19–35% protein, 22–40% carbohydrate, 28%–47% fat, are too broad for us to apply any one characterization to them. However if you go with his fat/protein top-ends and carb bottom-end–which fits for foodways high in animal-sourced food–then you get this:
33% protein, 45% fat, 22% carb.
Thhq thus, yes, this *can* sidle up pretty close to LCHF. Here, fat *is* by far the dominant nutrient, carb the least. Esp if these percentages represent nutrient by weight. If he gives percents in weight, then this is quite close to LCHF–maybe even be LCHF–by calorie.
Thhq, I grant you that Cordain says “…the carbohydrate content of these modern weight-loss diets is far too low…” In your quote, Cordain fails to say why he consider such diets “too low” in carbs–which I assume means anything that falls below that bottom 22% end he cites for “Paleo Diets.” From what I’ve seen, I find Cordain’s message not entirely consistent between his revised Paleo Diet and what he said in interviews and what his Paleo Diet site bloggers say. I ordered his 2010 book and should get it in a few days. I’ll read it and see if he explains the “perils” of low-carb or if it simply doesn’t fit into his conception of a “paleo” diet. Which would be odd given the very low carb diets many of the ancestral circum-Arctic peoples ate. Stayed tuned. –Bryan
Read the book @bryan. I’m tired of typing it out for you, and I won’t do it anymore. I selected one paragraph to answer your question, and another sentence or two to answer Morgana. I mentioned that the paragraph I quoted is preceded by a table which shows the macros for Paleo, standard American, and fad low carb diets. The critique of veg diets occurs later, and as you might guess it concerns the low protein and the grains in those diets. There are also several N=1’s of ex-veg’s that switched to the Paleo Diet.
I like your spunk @Bryan. That should be good for longevity.
Regarding “rebuttal research”, you’re making it sound like what I did in high school debate. That’s not the same as the research I did as a career for 35 years. You have to understand that methodology in order to respond in a meaningful way to the likes of Keys, Guyenet and Cordain. If you disagree with them, and your point is important, it’s down to the lab to find out. This is much different from the jib-jab of debate. That’s only the preliminaries – what I call the obligatory literature dump. If you truly believe that the cholesterol CVD theory is incorrect, get up your money and prove it. A pile of nih trump cards doesn’t win in the real game of life. I’ll give GT and Attia credit for realizing this and organizing NuSI.
I’ll express another opinion and leave it to you to read the book to find out whether what I say is true. Cordain does not dismiss the Inuit diet, but the diet he created is a composite from many sources. HE set the floor at 22% carbs minimum, not me, and at a ceiling of 40% he’s pushing the carb level of the SAD (though much better carbs). As I quoted for Morgana, one of the basic principles of this diet is eating fruits and nonstarchy vegetables as libitum. He puts a lot of emphasis on eating low glycemic carbs, but in the recipe section he uses dates, pineapple, raspberries, oranges and wine. He also uses a lot of peppers and tomatoes, which I thought he was strongly against. Reading the book changed my perspective on Paleo in a lot of ways.
Thhq, you say “…I’m tired of typing it out for you, and I won’t do it anymore.”
Sure Thhq. Whatever you want and don’t want to do. Especially if you don’t especially care if people pay attention to you or not. If you want, you can persist to serve up your bias with dubious unsupported statements. If it’s mainly you yourself whom you serve, if mainly that you feel satisfied just to read, and get reinforcement from, your own words, if the rest of us don’t really matter, then what’s the problem right? You can regale us on your long research career and your globe-trotting life, but in the end what matters is the rigor, or lack thereof, with which you present your views, ideas and hypotheses. If you persist to fail to supply links and quotes to back up your claims, if you persist to misrepresent the occasional material you do quote, then what can you expect us to think? At least Duck Dodgers made more of an ostensible effort to supply evidence, however risible so much of that turned out to be, and occasionally his sources weren’t half-bad. Meanwhile you present certain figures like Ancel Keys, and to a lesser extent Guyenet and Cordain, almost in a hagiographic light, intimating these people are such Gods we should embrace their words and deeds with a child-like faith, to assume we can’t really understand what they did and why they did it. Well guess what Thhq? I’m here for real science or at least something that honestly aspires to be that. I’m here to learn what we do and don’t know. I’m here to bat around ideas. I’m not here to shop for latter-day dietary Gods to which we must genuflect and put implicit trust in.
Way I see it Thhq, you found the n=1 that works for you, at least measured by How You Feel and the far-from-comprehensive medical tests you get–even if it means you need to spend a chunk of your retirement counting the calories you eat and the miles you walk. And By God you’ll defend it no matter how much you need to deploy wearisome diversionary tactics and how much you need to shuck’n’jive in your pseudo-erudite-uncle manner seasoned with a dash or two of Grand/Father Knows Best. At bottom, Thhq, you fail to keep an open mind. You mainly want to promote The Way you’ve spent so much time living and nurturing, to reflexively defend it like you would any reasonably good or even merely tolerable spouse. But hey, you’ll get some takers. Whether or not they matter to you to begin with.
Thhq, about what you say “…it’s down to the lab to find out.” of course that’s silly. We can’t meaningfully lab-test the endlessly varying human experience, especially in our modern world with its innumerable novel inputs. Like I posted here in October:
“No study can account for the myriad inputs in our daily lives and our genetic diffs, esp for effects over the long term, over which chronic disease usu develops. Nor will they ever mean much until we greatly refine genetic testing and suss out what the genes actually do, AND if we can convince a meaningful sample of people to agree to live for years in completely and precisely controlled circumstances and submit to around-the-clock observation. Oh, and employ a really smart and completely unbiased research team to develop the methodology and conduct the experiment totally funded by unvested interests. Are you holding your breath for all of that? Neither am I.”
About the much abused and heavily co-opted term “paleo” I’ve minimized using it. Cordain’s “paleo” def includes macronutrient ranges wider than a three-ring circus tent.
Thhq, about what you say here: “If you truly believe that the cholesterol CVD theory is incorrect, get up your money and prove it.” This shows you don’t even understand the fundamentals of the evidence you cite. You fail to distinguish *dietary* and *serum* cholesterol which even that Head Deity in your near-earth pantheon of Nutrition Gods, Ancel Keys, carefully avoids to correlate. Thhq, it’s CVD and dietary *saturated fat*, remember?
And what you say/cite here Thhq, well it’s just all kinds of vague, even confused:
“Cordain does not dismiss the Inuit diet, but the diet he created is a composite from many sources. HE set the floor at 22% carbs minimum, not me, and at a ceiling of 40% he’s pushing the carb level of the SAD (though much better carbs). As I quoted for Morgana, one of the basic principles of this diet is eating fruits and nonstarchy vegetables as libitum. He puts a lot of emphasis on eating low glycemic carbs, but in the recipe section he uses dates, pineapple, raspberries, oranges and wine.”
Where to start with this mess? No-one ever said you set a 22% carb minimum. Why define yourself from something no-one ever accused you of? You say “better carbs” which promotes the same tired misconception that some carbs are somehow fundamentally diff from other carbs, like those people who parrot the “complex carbs” vs “simple carbs” trope without having the first clue what they’re nattering on about. Thhq, *carbs are carbs.* Period. What lets us respond differently to carbs is how these carbs are *packaged* in the food they come in. Will we absorb them instantaneously from refined synthetic food-like garbola like sugar water and Bisquick, kicking the BG/serum insulin roller-coaster into screaming overdrive? Or will they trickle into our systems from whole fruit and veg as our GIs slowly dismantles their fiber cages to let them out? As for the Cordain words you cite “…eating fruits and nonstarchy vegetables ad libitum…” well what kind of fruits are we even talking about? There a huge variation in the sugar and fiber contents of fruits. Chowing mangoes and pineapples all day long will seriously spike BGs, chowing raspberries much less so. Which leads to your next sentence: “…[Cordain] puts a lot of emphasis on eating low glycemic carbs, but in the recipe section he uses dates, pineapple, raspberries, oranges and wine…” What is that supposed to even mean? Again, we see sugar counts all over the map. Dates and pineapples are super high in fructose and sucrose, oranges less so, raspberries quite low in sugar and high in fiber. And wine–what kind of wine? Dry reds tend to be lowest in sugar. Sweet whites are much higher in sugar.
Thhq I agree with you on one thing: Gary Taubes and Dr Peter Attia creating NuSi: http://nusi.org/ That could be huge. –Bryan
thhq, wbryanh- Below is a link to an interview with Loren Cordain on Jimmy Moore’s show. He explains how he changed his stance on saturated fat (as new evidence came out), how hunter gatherers ate the fattiest parts of the animals (though wild animals are leaner than domesticated), that most hunter gatherers ate a high fat, moderate protein, low carb diet. He also talks about the Kitavans and Atkins; good interview to see where he is really coming from, and much that relates to this discussion:
http://www.thelivinlowcarbshow.com/shownotes/8592/722-dr-loren-cordain-responds-to-criticisms-of-paleo-by-wapfs-sally-fallon-morell/
Hi Morgana. Thanks for the Cordain interview with JM. I’m still digging into our oddball taurine because, as with you and Heather, I don’t get why we see so little on it. I’ll start to listen to the interview after. But honestly I may not stick with it.
I did get a copy of Cordain’s latest Paleo Diet (2010) and started to read it. He offers some good ideas and concepts, but it’s essentially flawed. My sense about Cordain is that he put himself into a macronutrient box–mainly over-critical of dietary fat–back when he pubbed his first Paleo Diet book in 2002. Now he’s trying to side-step his way out of that jam–even includes a mealy-mouth mea culpa on his former view on sat fat–but he’s not transitioning well. Cordain even contradicts himself in a fundamental way in his 2010 rev of Paleo Diet. I will soon post that contradiction for us. Cordain also appears to conflate macro balances and food quality (whole ancestral foods vs SAD). So far he gives no concrete hypothesis on why “low carb” is bad for us except that it necessarily means “high fat” and that we get so much of that fat from the SAD. I guess I shouldn’t be surprised these days I don’t hear much about him and his muddied message. –Bryan
2010 version. I don’t know why I have to quote blocks of it. This is tiring. I ‘ll do it but like I said about Eal Well and Stay Well READ THE BOOK YOURSELF.
Cordain defends high protein at higher levels than I like. It’s not high fat, definitely out of ketosis range levels of carbs, and it ends up being low calorie. Good for weight loss.
I’ll work on the rest later. Busy now.
I’m pretty much with thhq that molluscs were about our first ancestral food. The bonobos live in a swampy environment and eat swamp food, and the early hominids were mostly found in that same environment (along with turtles, shells, etc.). Super-easy food to catch and more importantly, no chewing! Chimps can eat meat, but it takes them hours to eat it. Snails you just swallow, and they are way easier to catch and don’t fight back much. However, there is also a lot of taurine in insects. You need lots of Omega 3 too, to build a big brain, and you’d get more of that in the swamp foods.
We CAN synthesize taurine, but it seems we don’t do it very well, and the populations that eat more taurine live longer. Yeah, one issue would be that the two precursors are also limited. Methionine in particular is problematic. If you eat too much methionine it is downright toxic, and it acts as an appetite suppressant. But also, in our ancestral diet, why bother? Maybe we are more like cats … there was always enough of the stuff around, and taurine isn’t toxic at all. Or hard to get, if you live by water and don’t mind eating bugs.
Probably there are two main reasons we haven’t heard much about it. One is that it has been assumed there is no need for the stuff, and it can be synthesized as needed. But two: the people that have discovered how necessary it is, all seem to be in Japan. There are a number of people beginning to talk about it now though, and there are plenty of studies.
http://www.springer.com/us/book/9780898383966
“The first Taurine Symposium organized by Dr. Ryan Huxtable and the late Dr. Andre Barbeau was held in Tucson, Arizona, in 1975. Since that auspicious event, nine international symposia on the role of taurine in biology have taken place. The locations for these meetings have been Tucson (two times), Rome, Philadelphia, Tokyo, Vancouver, Mexico City, Helsinki, and Florence. In 1977, due to the large number of scientists in Japan who were interested in the role of this unique amino acid in biological systems, we organized the Japanese Research Society on Sulfur Amino Acids with the encouragement and financial assistance of the Taisho Pharmaceutical Co., Ltd (Tokyo). Annual meetings have been held, and the membership has expanded from 78 to 414 in 1987; the number of presentations has increased during this time span from 29 to 74. The symposium in Tokyo in 1982, “Sulfur Amino Acids, Biochemical and Clinical Aspects” [1], was held to celebrate the 5th Annual Meeting of our Society. I would like to emphasize that in Japan we have an active Research Society especially directed to the study of sulfur amino acids. ”
The mystery to me though is: given that it is so necessary, how do vegans even survive? Cysteine and methionine aren’t easy to get on a vegan diet either. And yet there are these healthy vegans. I’m thinking there must be a “survival mode” where the gut hoards taurine because eggs/fish/etc. is now in short supply. That would include making sure to re-absorb bile when it is used, and to not use much bile to begin with. This would work mainly on a very low-fat diet.
But I’m also wondering if maybe there are bacteria in the gut that synthesize taurine? So then, as long as there is enough sulfur in the diet, the vegan person could get enough taurine to survive.
Click to access 2519.full.pdf
Taurine as a Constituent of a Bacterial Cell Wall
Heather, seems quite plausible to me as well that many (most?) of our H-G ancestors ate loads of shellfish, for the reasons you give in your last post. This Boing Boing piece even suggests shellfish saved the human race! Fun reading:
http://boingboing.net/2009/12/16/how-shellfish-saved.html
I can’t think of any other high-protein food so easy to harvest. We find ancient shell middens all over the world, going back possibly as early as 164kya.
http://archaeology.about.com/od/boneandivory/a/shellmidden.htm
About bonobos, I’ve want to look more into their fascinating culture. Who hasn’t seen at least few bonobo progs on the nature channels and been intrigued even a little heart-warmed by them? Many (most?) primate societies are brutally patriarchal, like chimps and baboons, which puts lots of stress on lower members, esp junior males. Bonobos seem almost unique in their matriarchal, relatively egalitarian society, and they enjoy near non-stop near-indiscriminate sex to resolve conflicts. That’s an approach perhaps not very adaptable to our civ, but bonobo society seems unusually harmonious 🙂 I’ve never heard of another species take the “make love not war” approach.
Per this report, the bonobo diet, mostly fruit, is even more plant-based than that of chimps:
Click to access Bonobo-Nutrition1.pdf
But as you suggest Heather, fin- and shellfish may occasionally creep onto their menu. From that link:
“The most significant animal food source for bonobos is invertebrates, such as insects, insect larvae, earthworms and millipedes …[But researchers] also observed bonobos eating mollusks. …bonobos are known to eat termites…Vertebrate prey species appear to be much less common in the bonobo diet. In addition to duikers (small antelopes), bonobos have been observed eating squirrels on several occasions … and, in one instance, a bat … also snakes and shrews. At Lomako and Wamba, bonobos have been observed feeding on unidentified organisms along the edge of a stream. The Bonobos’ rapid movements suggested that they were feeding on fish or shrimp …”
Bonobos might well eat more shellfish if they lived by the sea. But all live inland in the Congo River basin, all within The Democratic Republic of the Congo. Or maybe not? I googled for coastal primates that eat shellfish. Found nothing so far.
About taurine, I haven’t been able to find anything that discusses human in vivo conversion rates from cysteine/methionine to taurine. You say “We CAN synthesize taurine, but it seems we don’t do it very well…” Heather do any of your links address that conversion question? Any that suggest how well or poorly we make taurine? Can you point me to charts that show relative concentrations of taurine in diff creatures?
I also wonder–do the creatures that have more taurine have more cyst/meth too? Are the relative concentrations proportional?
Btw, this piece: http://jn.nutrition.org/content/136/6/1722S.long
concludes: “Although methionine was labeled as being the most toxic amino acid in relation to growth in animals, the evidence in humans does not point to serious toxicity, except at very high levels of intake.”
All that said and asked Heather, as you say we seem to see at least steady interest in taurine. Here’s the list of topics for the 19th International Taurine meeting. Maybe you’ll find some goodies:
http://www.taurine2014.meetings.pl/?action=search&category=317&node=317
Heather I like your graf here, sounds plausible to me. It proposes yet another way Mother Nature brilliantly accommodates for an unusual dietary nutrient balance:
“The mystery to me though is: given that it is so necessary, how do vegans even survive? Cysteine and methionine aren’t easy to get on a vegan diet either. And yet there are these healthy vegans. I’m thinking there must be a “survival mode” where the gut hoards taurine because eggs/fish/etc. is now in short supply. That would include making sure to re-absorb bile when it is used, and to not use much bile to begin with. This would work mainly on a very low-fat diet.”
That said, I question even the premise of “healthy vegans.” I hear over and over about these radiant creatures like I do about “wholehealthygrains.” But I’ve yet to see actual solid data on how healthy vegans truly are as a class. Some vegans may look healthy, but what are their blood panels numbers and results of other med tests? Who’s done extensive clinical tests on very large groups of vegans, like thousands, or even merely hundreds of them? I haven’t heard of any such studies. Anecdotally, I personally know only one (self-identified) vegan. He grew overweight and developed medical issues despite eating vegan since the 1990s. Cookies made with veg oil are vegan and he admits he has a weakness for them, so he’s not the best example. But maybe he’s not the worst either. On a vegan diet, food reward can go way low when the fast carbs/fructose are low, and satiety can go way low when the fast carbs/fructose are high. I’ve long wondered how many (most?) vegans navigate that conundrum in a hectic world full of chronic low-level stress that always slams our cortisol buttons.
About our gut flora synthesizing taurine, I google this and find nothing so far. I like your link about taurine in the bacterial cell wall. I don’t yet get a sense if we can get significant amounts of taurine–of any at all–from that subject gram-positive bacterial, B. subtilis. Curiously, I notice we get unusually high amts of B. subtilis in natto:
https://en.wikipedia.org/wiki/Bacillus_subtilis#In_humans
This Japanese fermented soybean dish is one of my faves–like a nicely barnyard-y cheese–and it’s the only way these days I eat soy, except occasionally as tofu. –Bryan
Well, to answer the last email first … I don’t think primates gave up eating shellfish. I think the primates who ate shellfish grew bigger brains and became us! But more to the point, they took over the coastland. Look at the coast in any country and what you see is a whole lot of human beings. Many of whom would happily eat a bonobo.
The aquatic ancestor website deals with some of these questions: http://aquatic-human-ancestor.org/evidence/diet.html . There’s a good chart in there of DHA sources too. But humans can’t live on an all-fish diet, and I’m guessing that is even more true for apes. The apes are used to a diet of mainly carbs, and there is precious little carb in ocean food!
Humans seem especially adapted for a specific diet that includes: 1. Lots of taurine
2. Enough Vitamin C that we don’t need to produce it. 3. Plus we don’t have uricase (apes do) so we tend to turn fructose into fat. 4. We have kidneys adapted to a high-salt diet. 5. We have less-dense muscles that make us far weaker than a chimp, but we can swim and they can’t. 6. We can hold our breath and dive. 7. Our lack of fur allows us to dry out more easily. 8. Our propensity to store skin fat makes us float more easily and keeps us from getting so cold in the water.
Probiscus monkeys can dive too (that big nose!) but they don’t have a digestive tract that handles much protein. Chimps like water, but they drown easily.
Anyway, bonobos and chimps are our cousins, not our ancestors. There seem to have been a whole lot of various hominids that filled that shoreline niche at one point. But if they remained on the shore, I’d guess they ended up being hairless swimmers and wind up interbreeding with the rest?
It’s the fat thing that bothers me the most. “Everyone knows” that fat people are unhealthy … fat causes inflammation and is implicated in heart disease and diabetes. But why? A fat hippo isn’t unhealthy, nor is a fat bear or a fat manatee or a fat penguin or a fat duck. Fat is designed to be a non-reactive insulator and energy store. Eating fat (or not eating fat) shouldn’t make much difference one way or the other, since our bodies “eat” our own fat and store our own fat all the time … getting fat from your diet isn’t that much different, chemically.
So the fact we are having this conversation about “how much fat to eat” simply doesn’t make any sense at all, if the fats are natural fats. If we eat a lot of fruit, we store fat just fine. We can live off fat just fine. High carb or low carb, your energy source is largely made of fat (plus some glucose and some ketones).
This is where taurine and bile are bringing it together for me. If you eat dietary fat, you need bile to digest it. But bile uses up taurine. If you don’t have the taurine, your body builds up waste products (including cholesterol). If you don’t have taurine, you also don’t handle glucose correctly, you go diabetic, and you start gaining fat, and your metabolism slows down. Bingo! Your water-hominid is now no longer adapted to running around in the savannah.
The thing about the Orkney sheep is that they adapted to seaweed within less than 200 years. And now they die if they eat nothing but grass, because their bodies hoard copper. So this adaption thing can be a trap of sorts!
The “healthy vegans” I am talking about are the ones in Denise’s article here. The Kempner patients, and the folks reversing heart disease on Esselstyn or Pritikins. And the Japanese mountain people, who are basically vegan (they do eat some fish). The diets DO seem to work, at least short term. It looks like having a good source of sulfur is part of it, and maybe eating low fat is part of it, and maybe having the right proteins such that you can synthesize taurine is part of it. But yeah, eating vegan is far more of a tightrope than eating Asian style is. The Japanese mountain people have proved that kids can grow up on that diet, but they also traditionally breast fed, probably for years (human milk is high in taurine). Plant DHA can be used for some people while others can’t process it well (another genetic thing: an adaptation to living inland).
I love bonobos too. There is an old story … a guy dies and is escorted to Hell. In Hell, everyone is seated at a table loaded with wonderful food. But each person has a 3-foot-long spoon strapped to their hands, so they can’t eat the food, and sit starving in front of the feast. Then he is taken to see Heaven. In Heaven, there is the same table, the same spoons. But everyone is feeding each other.
Heather, wow, thanks for all this!
Going down through your latest, line by graf…
“I don’t think primates gave up eating shellfish…” What does it mean? Seems like most primates don’t eat shellfish now, whether they once did or not. Do you mean we humans crowded them out? Not sure that’s the case. The world had vast empty stretches of coastline up till not so many centuries ago. Anyway, if you can clarify when you get a chance.
The enzyme uricase (aka urate oxidase): Heather, interesting, thanks! Uricase is new to me. Per its Wiki:
https://en.wikipedia.org/wiki/Urate_oxidase
we still have the gene to make it, just doesn’t function (maybe missense?) Makes me wonder if this is some variant that spread from misuse, like how we can lose amylase in our young years, and likely like how how we (relatively) recently lost the ability to manuf Vit C, and how some northern peoples lost some ability to produce ketones. I wonder what evol advantage we may have gained to lose the ability to metab uric acid down to allantoin + exhalables (CO2, H2O2) but instead must excrete it. Btw, found this link that looks how uric acid affects fructose to hepatic fat conversion, at least in rats:
http://www.ncbi.nlm.nih.gov/pmc/articles/PMC3781481/
In general your points about the diffs between us and the other primates are very interesting. Just a few more Qs on those:
– About our high-salt diet adaptation, how does that fit in here? To better cope with naturally high salt levels in seafood?
– Why can we swim but chimps can’t? True, their increased lean/fat mass may make them more dense and harder to float. But they have more muscle to help propel them through water and to stay afloat. Not sure how lean/fat mass ratios compare between chimps and macaques, but here’s a vid of a macaque foraging and swimming underwater and generally playing around and having a ball. Per this vid, they can hold their breath for up to 30sec:
– Your part about lower fat in non-human primates makes a lot of sense. Maybe that’s why we find the waterphilic macaques in the warm waters of Indochina and the islands south of it. Also in the Japan’s hot onsens.
What you say “Anyway, bonobos and chimps are our cousins, not our ancestors.” Just to clarify, I didn’t say they were our ancestors. When I asked “I wonder when our very early ancestors started to feed on seafood?” I meant our Hominin or even Homo ancestors. Much of the evidence shows us diverging from our primate cousins in inland places far from the coasts, so our super-early forebears had lesser or even very limited access to seafood. See Africa map of earlier Hominin fossil sites:
http://anthro.palomar.edu/hominid/australo_1.htm
So I imagine most of our early ancestors had to learn about eating seafood, esp shellfish only sometime after we split off and some eventually migrated to the coasts.
About what you say “It’s the fat thing that bothers me the most. ‘Everyone knows’ that fat people are unhealthy … fat causes inflammation and is implicated in heart disease and diabetes. But why? A fat hippo isn’t unhealthy…” I very much agree BF *per se* is not necessarily unhealthy. We know some high-BF% folks are plenty healthy (like Churchill living into his 90s?) But we need to drill more down into that, e.g. ratio of brown to white fat, abdominal vs dermal fat, etc.
About what you say “So the fact we are having this conversation about ‘how much fat to eat’ simply doesn’t make any sense at all…” AGREE!! I treat dietary fat as my main macro variable. I see fat–at least sat and mon fat–as our most benign and least oxidizing caloric nutrient. By default I eat almost negligible carbs, modest protein (~ 1–2g/kg body weight) and the rest fat. I ramped up protein and carbs only when I did lots of sustained resistance training, like when I went to the gym for 90–120min/session four days per week, when I constantly pushed muscle tissue to fail and routinely micro-rent it. In this case, I bumped up 1.5–2x the protein level, and went up to 100+g very fast carbs in the recovery meal <45min after the workout. But to live as I normally do, aerobically with just episodic forays into resistance, I vary mainly my fat intake for the calories I need for that day. Walk longer and farther than usual? Weather is colder than usual? Eat more fat.
What you say “your energy source is largely made of fat (plus some glucose and some ketones).” Yes I agree. And to hark back to our Inuit metab discussions, seems that those with the CPT1a deficiency do run high serum FFA/lower ketone levels. But what are typical serum FFA/ketone levels?
What you say “taurine and bile are bringing it together for me.” yes Heather, I’m with you. The logic makes sense to me.
About what you say “The ‘healthy vegans’ I am talking about are the ones in Denise’s article here. The Kempner patients, and the folks reversing heart disease on Esselstyn or Pritikins.”
Heather, I at least partly disagree with you here. The average post-treatment BG for the Kempner patient cohort was still diabetic at 155 mg/dL. You can take Neisy’s offer to send you the sheet that shows that. Plus, Pritikin, Esselstyn, McDougall, et al, while they pitch their progs as a permanent lifestyle change, it seems most patients do it only short-term. In any event, we don't truly know what these patients eat once they leave the clinic. My point still stands–we don’t have solid sufficient controlled long-term data on people living vegan. Looking at the long-term, it’s still mainly anecdotal.
About the Japanese mountain people and their vegan (near-vegan?) foodways, do you have link(s) for that? I’ve heard mention of them a bunch of times. But google gives me nothing so far.
Your Hell and Heaven dinner table story–LOVE IT!! LOL! Sharing and sharing!. First with my folks. 🙂 –Bryan
“Do you mean we humans crowded them out? Not sure that’s the case. The world had vast empty stretches of coastline up till not so many centuries ago. Anyway, if you can clarify when you get a chance.”
If you look at the worldwide distribution of humans, you’ll see most of them on the coasts. That’s been true for most of history. Now, look at the distribution of primates. Most of them are endangered, and living in protected areas. We crowd them out sure. And hunt them. And compete with them for food. You just don’t find humans and primates living anywhere close to each other. Monkeys seem to fare better, and even live in cities, but mostly it seems this happens when humans tolerate the monkeys for religious reasons.
Uricase is a really interesting thing. It seems to have to do with surviving famines. The lack of it causes humans to store sugar as fat easily, like a hibernating bear, and prevents the fat from being used for energy. Also makes us hoard uric acid, which leads to gout. I think it’s a kind of “hibernation switch” … it’s like a bear, they hoard fat when they eat fruit. It’s been awhile since I looked into it though.
http://eatingoffthefoodgrid.blogspot.com/2012/08/fructose-uric-acid-and-iron.html?q=gout
As for processing salt … we have kidneys similar to the ones on a camel. With camels, they live in places with not much water, and the water they find is often salty. So somewhere they learned to drink salty water. We did too. You can figure that was NOT while we were living in a rain forest! If you live near the coast though, there will be rivers exiting to the ocean. But the river near the ocean tends to be mixed with salt water, so I figure somewhere we learned to handle the salt.
For swimming … well, I guess some HAVE learned to swim, but it’s not what I’ve heard in the past:
http://www.sci-news.com/biology/science-chimpanzees-orangutans-swim-dive-01319.html
It seems to be rare though in the wild, and apparently chimps don’t often cross water they can’t walk through. If you look at the videos, the chimp just sinks by default … it learns to dive by hanging from ropes in the water.
“So I imagine most of our early ancestors had to learn about eating seafood, esp shellfish only sometime after we split off and some eventually migrated to the coasts.”
The commentary I’ve heard from the AAT folks is that while those skeletons were found inland, they are also buried with remains of turtles and crocs and other water food. Some of the shorelines may have been ocean or inland seas, and some were fresh water. But either way they were loaded with water food. Lucy, for example:
http://www.bbc.com/earth/story/20141127-lucy-fossil-revealed-our-origins
“Lucy herself may have been collecting eggs from a lake. Fossilised crocodile and turtle eggs were found near her skeleton, leading to suggestions that she died while foraging for them.”
“And to hark back to our Inuit metab discussions, seems that those with the CPT1a deficiency do run high serum FFA/lower ketone levels. But what are typical serum FFA/ketone levels?”
And does it matter? I guess if one has a problem handling glucose, minimizing glucose might be a good thing. But until fairly recently, most adult human beings on earth didn’t have much problem handling glucose. Diabetes was a rarity even when I was a kid. Diabetes was rare in China, even when people were living mostly on rice. Until they started eating “Western Food” and now the Chinese are getting epidemic rates of diabetes.
“Plus, Pritikin, Esselstyn, McDougall, et al, while they pitch their progs as a permanent lifestyle change, it seems most patients do it only short-term.”
It does seem that some people do it rather long term, and there are several cultures that are near vegan that have been that way for ages. The Japanese mountain people live the longest and have the best documentation. The village is called Yuzurihara. I have linked to it a couple of times.
http://www.livestrong.com/article/312974-yuzurihara-diet/
It’s not so much that I’d recommend living that way. But as Denise wrote far more convincingly … there IS plenty of evidence that this works, at least for some people. Dropping blood sugar down to 155 isn’t a cure, but it’s better than what it was. And more to the point, for me … the people actually lived. According to current thinking, that diet shouldn’t work at all. The Yuzurihara should all die from heart disease like the guys in Chad. *** Something *** is working in those cases.
Even if it’s only a short turn-around … like in the movie “Fat, sick and almost dead” … it’s worth looking into what the heck happened in the short run, that worked. And it’s worth figuring it out because I do NOT think the vegans are right in their explanation, which is basically “animal foods kill” (and they mean ALL animal foods!). The vegan diets that appear to have decent results are all exceedingly low-fat, is what I’m seeing.
Personally I have no desire to live off nothing but rice and vegies though. There are a few foods I’ve found problematic, but mostly nothing I’ve seen says we need to be either exceedingly high or low fat or avoid all animal foods or avoid all carbs. Go go gastronomy!
Presentation from Ancestral Health Symposium about humans eating shellfish
Remko Kuipers, PharmD, MD, PhD — Paleolithic Nutrition — Facts From the Floor
Thank you! That is a very nice video!
Here is the link more visibly (It showed up oddly in my mailbox):
Heather, @GTR, GTR, thank you for this vid. Just this moment finished watching it.
Remko Kuipers, PharmD, MD, PhD — Paleolithic Nutrition — Facts From the Floor
Learned some new ideas. Eg: natural selection stops not at *our* ability to reproduce but till our children reach the age *they* can reproduce. Meaning it selects for living not just to ~20–25, but ~40–50. Need to think more on that.
And Heather, it reflects what you say about early ancestors getting fin- and shellfish from lakes, riparian environments.
But should we aspire for 100+ nmol/L blood Vitamin D2 levels like those they measured in Hadza and Maasai? Hm. Need to look more into that. –Bryan
@wbryanh: I have no idea how much Vit D is ideal. I also don’t know how much of it ideally comes from the sun. What I noticed in my family is that my grandmothers got very little sun, esp. my fraternal grandmother, who was maybe a bit sun-phobic. But most woman of her time were pretty much covered head to foot and used a parasol and gloves when going outdoors. But she lived to be a healthy 96, with no cancer or heart disease at all, or even high blood pressure. For most of her life she had as much food as she wanted, and she was never obese either. So the question I’ve always had is: why wasn’t she dying from lack of Vit D? Why didn’t she have rickets at least?
The answer, I’m pretty sure, is that she ate a lot of fish and mushrooms. Herring was just sort of a staple snack. No one thought much about the fish … like in the video, it was sort of like “vegetables” … not really meat.
So when you talk about these tribal peoples: about half the Hadzabe were under 100, and the mean was 109. I don’t know what the mean is in Japan, but for elderly women who ate fish 4x a week or more, the range was 60-80 (way more than what was quoted in the video as what was considered “healthy” in Norway, which was 39?)
http://jn.nutrition.org/content/135/2/310.full
In at least one study, healthy levels of Vit D are considered 70-90
http://www.worldhealth.net/forum/thread/99358/vitamin-d-proven-more-effective-than-bo/?page=1
which isn’t far off from those tribal peoples. So maybe an average of 80-100 or so is about right? But what bothers me is the idea that if it is lower, you should just keep taking supplements until your Vit D levels are high enough. It smacks of the idea of keeping eating statins until your cholesterol goes down to a certain point. Do we even know that the supplements do the same thing as the whole source?
The IOM Institute of Medicine says 30 for vitamin D is adequate. Recently there have been more and more articles saying vitamin D supplementation has no benefit to our health, nor does it stop falls and broken bones. Sorry I do not have a reference, I do not file everything I read, but over the last year there has been more and more research saying this. As little as 10 minutes of sun a day on even a small area of exposed skin is enough for our bodies to produce all the vitamin D we need. The other misnomer is to call it a vitamin, it is a steroid hormone. All hormones need to be tightly regulated in the body, and vitamin D can be toxic if the levels are too high. Plus what is typically measured is 25D it is a proxy measurement for the active metabolite 1,25 D. It is not uncommon for people to have low levels of 25 D and very high levels of the active metabolite. This is seen a lot in people with chronic diseases. Again I do not file references, so for those who demand some proof, sorry you will have to do your own searching.
Thanks for this Rebecca. What you say here:
“…The other misnomer is to call [Vitamin D] a vitamin, it is a steroid hormone….”
brings up basic definitional Qs.
At least we might think they should be “basic.” It’s amazing how often the de jure and de facto authorities can’t agree seemingly basic defs. What defines ketosis? Glycolysis? For our discussion here, what defines a vitamin? What defines a hormone? Can a compound be both a vitamin and a hormone?
On page 373 of Lehninger Principles of Biochemistry Sixth Edition (2013)–a preeminent university text and Amazon top seller for biochem–we find:
“…vitamins [are] compounds that are essential to the health of humans and other vertebrates but cannot be synthesized by these animals and must therefore be obtained in the diet…”
And yet, in the very next graph, the book roundly contradicts itself! See here:
“ Vitamin D3…is normally formed in the skin from 7-dehydrocholesterol in a photochemical reaction driven by the uV component of sunlight…” (Btw, Lehninger fails to tell us *which* uV component. uV-A? uV-B? Both?)
This Wiki (https://en.wikipedia.org/wiki/Cholecalciferol), maintains:
“…cholecalciferol is synthesized by the body, and functions as a prehormone….”
Let’s move to B and K vitamins. That same Lehninger text defines “hormones” as:
“… small molecules or proteins that are produced in one tissue, released into the circulation, and carried to other tissues, where they act through receptors to bring about changes in cellular activities…”
This give evidence our gut flora make at least some our B and K vitamins:
http://www.clinicalnutritionjournal.com/article/S0261-5614(97)80252-X/abstract
We call these Bs and Ks “vitamins.” Yet we *do* produce them within our bods. Via interactions between our gut flora and tissues in our bods proper.
So does that make all of these vitamins hormones too?
All very interesting. –Bryan
BTW thank you for the links: they do look interesting. As far as saving humanity … I recall a quote that was supposedly from a Native American about the Pilgrims: “Only an idiot can starve next to the ocean”.
LOL! Heather dunno if “”Only an idiot can starve by the ocean” can stand up to Snopes’ scope, But I love it!
Btw, just visited here: http://eatingoffthefoodgrid.blogspot.com/
Glad you like the Grand Unified Theory for Macronutrient-Independent Euphagia!
I’ll read it closer later. But I see taurine figures high on the playbill 🙂 –Bryan
Heather, the seafood question keeps bugging me. Shellfish is such a terrific and easy-to-get source of protein and w3. It’s mineral-rich too and of course full of taurine. You’d think it’d be dead-easy for primates to find and eat shellfish. When we were kids we went to the beach with pails and trowels. In 20 minutes we dug up enough clams to feed the family.
Even so, for primates, to harvest and eat seafood seems the near-exclusive domain of people. Strangely, very few other primates seem to go for seafood. So far, I know of only the bonobos, and the crab-eating macaques of Indochina. Even for them, seafood’s usu a small part of their diet.
https://en.wikipedia.org/wiki/Crab-eating_macaque#Diet
Both primate species are uncommonly intelligent, and, curiously, both live in matrilineal and female-dominated groups. Macaques can use crude tools, e.g. a Macaque uses a rock to crack open a piece of shellfish (mussel?) (Bottom right corner):
Most non-human primates don’t even seem to like the water much. Besides bonobos and crab-eating macaques, the Japanese macaques are among the few that like the water. See them here basking in a steaming onsen, in this Daily Mail piece four images down:
http://www.dailymail.co.uk/news/article-2175085/Swimming-apes-reason-feel-healthier-sea.html
I haven’t been able to find any primates that like the ocean. Who are even willing to go to feed at the tidal pools during low tide.
I wonder why this is? What stops most of them from going after this rich and easily accessible nutrient bounty?
Are they afraid of the noisy waves and the rushing water? Yet even some sheep seem to overcome that fear. These Orkney Island sheep eat almost nothing but seaweed!:
http://www.orkney.com/about/explore-orkney/north-ronaldsay
And of course Alaskan brown bears stand near rushing river water chutes to snag salmon. And otters use rocks to crack open clams and mussels.
I wonder when our very early ancestors started to feed on seafood? What barriers did we have to overcome to let us to go to the water’s edge and harvest shellfish? That Daily Mail article linked above touches on the “Aquatic Ape” hypothesis, which says that ancestors of modern humans at some point adapted to a semi-aquatic existence.
https://en.wikipedia.org/wiki/Aquatic_ape_hypothesis
But that idea appeared never to gain traction. Anyway, why most primates pass up a wonderful easy-to-get nutrient source, it’s an interesting mystery. –Bryan
One of my muses is a 19th century s’klallam clam basket. It’s open-wove with heavy spruce ribbing, and could carry in the range of 100 lbs of clams. One recipe I’ve read was cooking in pits, blanketed with seaweed to steam them open. This takes out any need for tools, other than the digging sticks.
Regarding vitamin c, spruce buds are a very rich source. I haven’t looked into whether other leaves or seaweed, edible or inedible, contains vitamins.
I don’t think seaweed has much Vit C. But sure, spruce tea does. Also raw clams and fish. Same issues as the Inuit! Muktuk is about as much Vit C as OJ according to Discover Magazine:
http://discovermagazine.com/2004/oct/inuit-paradox
Lots of greens have Vit C though, and there was plenty of green stuff in Northern Europe. There is also a plant called Sea Buckthorn, which has one of the highest levels of Vit C of any plant, and also has some really good fats in it.
Cooking really wasn’t much of a challenge once people got fire. It was also common to line baskets with tar or a raw animal hide, and toss hot stones in it to boil the water. Or hang the hide over a fire. Burying food in a pit and making a fire on top was popular too. Or just setting the food next to the fire and letting it cook. They set this up locally to show how the first peoples cooked fish in the Northwest: they opened up the salmon on a stick, and stuck the stick in the ground next to the fire to let the radiant heat cook the fish.
But like I said, eating seafood raw or dried was (and is) common too.
Every once in a while I see the tightly-woven cooking baskets for sale but I’ve never landed one. I have a couple of storage baskets, the clam basket and a small imbricated berry basket ca 1850. Hunting for the baskets was a lot of fun. One guy in BC sold me two inexpensive ones and gave me an excellent book on Salish culture as it changed over from native to Western. Very sad. Their paleo-like existence was wiped out by a fever epidemic in the 1830’s. The fever was controllable by quinine, but there was not much quinine. 90% of them died, probably 100,000 people. [Having read this, I’m a bit skeptical of the health claims for the Paleo Diet. It can improve certain health conditions, but it won’t make you invincible].
Here’s a link to the Burke museum basket site.
http://www.burkemuseum.org/static/baskets/
Oh, those Salish baskets are amazing. I do a fair bit of “fiber arts” myself, including basketry, but never that finely.
I agree that eating Paleo isn’t a cure-all for sure. Yes, it certainly didn’t prevent the rest of the world from catching European diseases! You can also read the Lewis and Clark journals. Lewis did a fair bit of doctoring, and got a reputation with the Indians who came for healing. Lewis documented their illnesses.
Oddly he mentioned there were a lot of “rheumatoid” complaints. I find this odd, esp. as the Indians were mostly pretty young. And I think the folks on the coast (the salmon-eaters) were the most healthy. But none of them were unscathed by European germs.
I kind of think that a diet heavy on red meat (buffalo and deer, for instance) would be heavy in iron. Plus the neu5gc is just plain inflammatory for human beings.
where is part 2?
Remarkable read. You’re teaching me…
And there’s an error here: “Okinawans (12% of calories as fat)” The link you supply shows that they consumed 6% of calories as fat, being 12g of fat per day. NB their near contemporary Japanese, quoted in the same study consumed 8% of calories as fat.
Thank you for posting a link to the Esselstyn study, Neisy. I’ve read it and printed it. The first thing that jumped out at me was exclusion of all oils. There’s a fair body of evidence that oils, particularly seed oils, may be strongly implicated in cardiovascular disease. Exclusion of naturally oily foods like avocadoes may not have been significant, if commercially prepared seed oils are indeed the culprit.
There are other confounders, the same ones that plague all these vegan, lowfat interventions. Too many foods are excluded! In this latest Esselstyn paper, the study participants were forbidden not only animal products and even foods like avocadoes, but all processed products. that contained oil – that automatically cuts out a lot of sugar, starch, food gums, preservatives, stuff like titanium dioxide and the whole slew of weird chemicals to be found in the listing of, say, Pepperidge Farm Milano cookies or industrially-produced bread. Esselstyn says that participants were asked to exclude “sucrose, fructose, and drinks containing them, refned carbohydrates, fruit juices, syrups, and molasses). Subsequently, we also excluded cafeine and fructose.” He says that he considered subjects adherent if they excluded animal products, but he also emphasizes in-depth nutritional counselling. Just look at what they got:
A five-hour seminar
recipe handouts
books
video
strategies for plant food acquisition and preparation
testimonies
Ongoing phone counselling
Emotional support
This makes it highly unlikely that the participants were guzzling coffee, juices, sugary drinks, orprocessed foods. They were all over 60, and they were very sick people, all of them with CVD. They were scared to start with, and I bet the 5-hour seminar scared them even more.
Another confounder: this is a self-selected group. These people ASKED for a vegan diet. This was not a randomized trial. The group that stuck with it was highly motivated because they believed that a vegan fatfree diet would cure them. They’re likely to be super-responders. They were also on cardiac medication, so the diet may have potentiated the medication, or vice versa, or perhaps the removal of inflammatory foods like refined starches and sugars and industrial oils may have been an important factor.
91% of the participants were men. It would be instructive to know the sex of the non-adherers, and the sex of the non-adherers who experienced CVD events. The people who dropped out may have been sicker than the others to start with, and may well have had their unfortunate events even had they been adherent.
The typical western diet is a lousy referent, loaded with sick-making ingredients. It would be more meaningful to compare the Esselstyn and other vegan nutritionist studies against Blue Zoners, whose health and longevity are enviable. None is vegan, and none eats a fatfree diet.
I just don’t think there’s enough evidence to support either the extreme lowfat or the eradication of animal source foods as curative of heart disease. Further, there’s no evidence to support extrapolation of something that works for old, sick, men to entire populations.
But some positive side-effects are caused by low fat approach. Consider pan-frying. Conventionally it is done on oil, which allows to achieve temperatures like 190C or even more.
This causes toxic and carcinogenic substances to form, like acrylamide, HCA etc. Typical european pan is set at 190C – this is for example a temperature level that Tefal thermal indicators turn on, or non-regulated electric pans are set by default.
Esselstyn frying method is to fry on a thin layer of water. Meaning it cools things down to around 100C, at which the production of toxic products is reduced.
@suzannebick – “The typical western diet is a lousy referent, loaded with sick-making ingredients. It would be more meaningful to compare the Esselstyn and other vegan nutritionist studies against Blue Zoners, whose health and longevity are enviable. None is vegan, and none eats a fatfree diet.”
One needs to look at all of the evidence. There are healthy meat-eating populations in the West such as the present Mormons and earlier Rosetans. But there is even more healthy meat-eating populations in Asia, which includes Hong Kong residents who are among the longest lived and eat more beef than Americans. One complicating factor is the healthy user bias.
Denise, first of all, congratulations! Admitting your own mistakes and bias takes guts! But doing it, in front of the whole English speaking world to see, takes a lot more than guts! And show that you got the rare quality of integrity.
Second, I’m quite surprised by the summary of these findings, and look forward to keep learning about it, so keep at it girl!
Your wonderful way of writing makes one stick to it, even if you seem to surpass yourself at every new blog length, making one mustard new depths of visual strength to rival your panache!
here is a good rebuttal of some of Denise’s conclusions: https://intensivedietarymanagement.com/thoughts-on-the-kempner-rice-diet/
Dr. Ray Peat has a great article talking about diabetes and how it was once (successfully) treated by sugar.
http://raypeat.com/articles/articles/glucose-sucrose-diabetes.shtml
I think this makes sense in a lot of ways, the success of both low carb and low fat, especially with regards to the gut microbiota and metabolic endotoxemia. There is growing research that shows obesity might be caused by metabolic endotoxemia, which is effectively LPS translocating across the intestinal barrier.
1) LPS basically comes from gram negative bacteria, whichs increases on a high fat diet.
2) Chylomicrons are thought to be the transport mechanism for LPS which help them move across the intestinal barrier. These are composed mostly of triglycerides, which typically come from carbohydrates.
On a high fat diet, LPS will increase in the intestine but the body will be deprived of carbohydrates so the chylomicrons will be small – net effect is less LPS translocating across the barrier and lower metabolic endotoxemia.
On a high carbohydrate diet, LPS will be low but chylomicrons may increase – net effect is still less LPS translocating across the barrier.
In the swamplands both LPS and chylomicrons will both, which may increase the LPS translocation across the gut barrier.
Just an idea on how to make sense of some of this.
Thanks for putting the science first.
@wbryanh Gary Taubes has said a few times that he only believes about 70% of what he wrote in GCBC – that is, he’s since read more and researched more and now thinks some of the conclusions he reached were incorrect. I think GCBC is a great book, but the carbohydrate hypothesis probably only represents a small piece of the puzzle. That is, once insulin resistance and obesity kick in, a low carbohydrate, high fat diet *may* be the optimal one. But perhaps it’s better to focus on what causes the insulin resistance/obesity in the first place, since I don’t believe it’s even alluded to in GCBC, other than maybe the hypothesis that fructose is the causal agent. It may be something else entirely, like gut dysbiosis that leads to IR, which then makes a LCHF diet optimal. I don’t pretend to know. But I think it’s clear everyone is still learning, and the science still has a long way to go to figure out causality and if/how to reverse it.
One more defense of low fat. The ongoing discrediting of the NHANES self-reported data on macronutients, most recently by Mayo Clinic.
http://www.mayoclinicproceedings.org/article/S0025-6196(15)00319-5/abstract
The NHANES 1965-2000 trend showing increasing carbohydrate consumption is the major underpinning for Taubes assertion (in GCBC pgs 232 and ongoing) that carbs are responsible for the obesity crisis. The NHANES trend is completely the opposite of the 1970-2005 USDA trend based on food depletion, which indicates increasing fat consumption (from 34% to 50% of the American diet) as a more likely culprit.
In fairness to Taubes he didn’t know about NHANES inaccuracy 15 years ago. But it’s time for the assertions he made based on NHANES to be publicly retracted.
Big fat chance of that happening.
Thhq- Welcome back!
Actually, Gary Taubes did know about the inaccuracy of NHANES. He is a very scientific guy, and he mentioned that “food recall questionnaires” are highly inaccurate. Actually, anyone with half a brain can figure this out logically, and therefore I’m surprised this information is so widely used in studies and the like.
I did not see any evidence in the links you posted that fat consumption has gone up- (I’m not denying it though; it’s just that I don’t pay online for articles, so I may have missed something). What I can almost guarantee is that the type of fat people have been eating in recent years is worse than the traditional fats we used to use, which I’m sure is having an effect on the obesity crisis. Also, fat can “hide” in carbohydrate; this has been well documented; so when people eat lots of carbohydrates together with lots of fat, apparently they tend to eat more of both and consume more calories in general. (This doesn’t happen if you eat low carb, high fat). Fast food tends to be high in both, so that is one problem right there. In any case, there are many nuances.
It has been well documented that the world’s sugar consumption has steadily increased. Much of this is sugar added to foods- often to so-called “healthy foods”- that people aren’t even aware of. I think this is really unfair. In fact, there was a time when I was eating far more sugar than I realized, for this very reason. I didn’t get fat- (I exercise it off probably)- but I did have massive health problems. I don’t eat sugar anymore.
Hi Morgana, thhq! —
I agree, we should look warily at epidemiological studies with self-reported data. Including Keys’ Seven Countries Study which once we considered ground-breaking and central to the formation of US dietary policy in 1980. And now we increasingly understand that study’s severe limitations, if not its outright irrelevancy. Including Keys’ cherry-picking of the countries–7 of 22 he originally observed–to neatly fit his pre-determined conclusions to support his lipid hypothesis.
Based on how unavoidably weak and fallible nutrition studies are to date, no government should be in the biz to offer macro- and micronutrient-level dietary advice to its citizens. This, because we can’t sequester a sufficient sample of actual humans (like hundreds or thousands) for a sufficient period (like 20 years) to meaningfully measure them in a rigorous clinical fashion to correlate environmental inputs (esp diet) to their health and emerging disease.
This leaves us with our n = 1s and Aristotle’s conundrum of the “experts vs the wisdom of the crowd.” In this case our “experts” are those researchers, mainly with vested government and corporate interests, who create “consensus science” for their living. And the “crowd” is all of us, many of whom suffer from chronic disease, who experiment with different dietary paradigms, eg ancestral eating, and diligently observe ourselves to see how each model affects our health, and to share our experiences, like we do here on the web. In the end, each and every one of us can only truly find out for ourselves what will and won’t work, to record our environmental inputs in as much detail as possible and to seek the most and best health measures we can, as often as we can. In the main, the ream of conflicting “scientific” studies–including the Seven Countries Study–tells us little of value. –Bryan
Where did I mention Seven Nations @Bryan? I’m talking about One Nation With Two Contradictory Studies. Focus on that. We’re not talking about errors made in the 1950’s here.
Hi thhq. You’re right, you failed to mention the Seven Countries Study. You missed a golden opportunity to cite the best example ever for why people should finally dispense with the fools’ gold of epidemiological studies, which are based on the memory-based dietary assessment methods (M-BMs) as described in the Mayo report you posted. I cured your omission.
That Mayo link contains this:
“A Failed Research Paradigm
Epidemiologic studies suggest that almost any nutrient can be associated with a myriad of outcomes…”
Thhq, what better example of the fallibility of epidemiological studies than The Seven Countries Study? The US gov’t, much of the research community, hailed this dreadful contrivance as a landmark study. It became the single most influential evidence to guide the disastrous course of US dietary policy. It’s responsible for the shorter and sicker lives of untold millions of people.
Here thhq you say:
“I’m talking about One Nation With Two Contradictory Studies. Focus on that…”
Hm. So the first study is that giant epidemiological study that the Mayo report takes to task: NHANES. Already been there and focused on that.
Now about the other “study.” Here thhq you say:
“…The NHANES trend is completely the opposite of the 1970-2005 USDA trend based on food depletion, which indicates increasing fat consumption (from 34% to 50% of the American diet) as a more likely culprit…”
Sorry, thhq, but I couldn’t find that anywhere in that Mayo link you posted. Maybe you can actually give us an actual quote on that? Thanks. –Bryan
These government data banks are extraordinarily messy @brian, and nothing is apple-to-apples. I”m starting to see why the USDA food-depletion methodology is as open to criticism as NHANES. One of my sources of USDA data showing burgeoning fat consumption is linked here
http://www.nutritionaction.com/daily/fat-in-food/fats-and-oils-in-the-changing-american-diet/
where it’s expressed in lb/person per year. It increases from 33 to 48 lbs from 1970 to 2000, or 45%. If you compare this with the NHANES graph Taubes displays in GCBC (page 233) you see a decline in fat consumption over the same period, from 36% to 32% of total daily consumption. That’s the best I can make of it from the sources I have available. I can’t make heads or tails of how USDA sorts out food availability into estimated daily consumption, and you’d have to take it up with the Mayo researchers to see how they sorted it out.
Th unaddressed problem, as you mentioned re: 7 nations, is why anyone would trust the government data banks for formulating dietary guidelines. McGovern/Keys fell into the trap and created the food pyramid. Taubes should have known better, but plunged ahead and believed NHANES in creating his carb insulin assertion.
Thhq, what you say:
“These government data banks are extraordinarily messy … and nothing is apple-to-apples… I can’t make heads or tails of how USDA sorts out food availability into estimated daily consumption…”
It’s all you say and more. Especially the dismal lack of granularity, to the point of meaninglessness. Eg fat types. No epi study I’ve seen break down the fat beyond merely sat, mono, and poly. You’re lucky to get even that. Fat sub-subtypes matter hugely and no epi study ever breaks these out. And they should. Our bods respond much differently to short- and medium-chain sat fats (12:0 aka lauric acid and shorter) than to the long-chain sats like palmitic and stearic acids. About the polys, the omega-6/omega-3 balance likely matters hugely too. The sense is that a 4:1 ratio of 6s to 3s is about as high as you want to go, and when you stick to unprocessed foods–esp no legume/veggie/seed/nut oils–you’re hard-put to push it above that ratio. But when we look at that link you posted:
http://www.nutritionaction.com/daily/fat-in-food/fats-and-oils-in-the-changing-american-diet/
where do you see the big pop in fat use? Salad oils! Which are typically legume/veggie/seed/nut oils, fats that are highly processed into w-6 bombs, causing daily 6/3 ratios to soar to 20:1, 40:1, even 60:1. Over time these excessively high ratios may well stiffen our cell membranes, making them less permeable, restricting nutrient ingress and waste egress, laying the table for metabolic dysfunction.
We also see this woeful lack of granularity in Food Availability analyses, which also suffer from many other limitations, as the USDA itself readily discusses here:
http://www.ers.usda.gov/data-products/food-availability-(per-capita)-data-system/food-availability-documentation.aspx#limitations
This limitation especially jumped out at me:
“…more importantly, the **data may overstate the amount of food actually ingested by humans** by capturing substantial quantities of nonedible food portions and food lost through waste and spoilage in the home and marketing system…”
For example, thhq, just because we *buy* the fat doesn’t mean we *eat* the fat. There’s still plenty of folks who buy and cook the bacon, and toss out the rendered lard. Plus some fat types, like some polys go bad quickly, meanwhile carbs like sacks of rice and packages of pasta last virtually forever. So we may well see a much more fat waste than carb waste. Even though you may be buying more fat than carbs, you may actually be eating less of it than carbs because you waste so much more fat.
Bottom line thhq, epi and food availability studies may be interesting to read. They may give us ideas to think about. But we can’t rely on any of them at all for concrete dietary direction. –Bryan
Re: waste — the UN estimates that, worldwide, at least 33% of food is wasted (less waste would sure solve our much-ballyhooed “food shortage”). In the US, it’s even worse, close to 40% (http://www.fao.org/3/a-i4646e.pdf). Apparently, most “analyses” of the SAD do not account for this fact. Estimating consumption based on availability, or even what is purchased and taken out of the store, seems an iffy proposition.
@annie the raw USDA food data looks like this. I don’t even remember which of the multiple sites I found it on:
Year Fat g Carb g
1970 147 401 2000 191 505
Even without the protein, this is 3000-3500 calories per day just for fat and carbs. But USDA also reports total estimated dietary calories for men as 2450 in 1970 and 2618 in 2000. There’s a loss factor in between the raw and actual diet numbers. I have no idea what it is or where to find it.
>
Darn. Replying by e-mail mangled the table. I’ll try again
Year Fat g Carb g
1970 147 401
2000 191 505
Looking at just the raw numbers, fat consumption is up 44 x 9 = 396 cal/day, and carb consumption is up 104 x 4 = 416 cal/day. Almost exactly the same increase in both fat and carbs….looking remarkably like the fat/carb ratio of a Snickers candy bar…and the calories of 4 Snickers candy bars. I can’t imagine that those increases were due to eating more whole grains and grass-fed butter.
If you scale it, it looks like we were eating an extra 2-3 Snickers a day in 2000 that we weren’t eating in 1970.
That’s about the size of it…er super-size….er super reward…
Here’s the source of the USDA food availability macro data back to 1909. This is expressed in grams per day per person for each reporting year.
http://www.ers.usda.gov/media/179795/carbs_intake_d.html
This table underlies one of the graphs in this 2015 report.
http://www.ers.usda.gov/data-products/food-availability-(per-capita)-data-system/summary-findings.aspx
And here’s the 1970-2005 trends report.
Click to access eib33_1_.pdf
My problem with using this welter of information is filtering it to compare on same terms. In the 1970-2005 report especially, the data has been manipulated to create the report that some administrator or politician wanted, but not necessarily the report I want. For instance, look at Figure 1. The foods are expressed not as macronutrients, but as the groups that consittute the food pyramid (or My Pyramid as it was known at that time…who knows how this reconciles with the current My Plate protocol). [In fact, Figure 1 is really a Food Pyramid compliance diagram….we were eating too much grains, meat, eggs and nuts and not enough dairy, vegetables and fruit…naughty, naughty Americans! ] This twisted reporting makes it hard to report the numbers in any other way than what the author intended.
I just had some Tiim’s Potato Chips for lunch. The ratio of fat to carbs is 1.3. Even higher than a Snickers. This got me thinking about the NHANES underreporting problem. Snickers and potato chips are most likely the underreported foods. If they were included the dietary fat would go way up. Putting a lot of fat in processed food hugely increases the calories. People just don’t know that a 150 calorie serving of potato chips is 10-15 chips. Eating half a bag for a snack is easily 10x that. And what would someone report to NHANES, if they even bothered to report it?
Welcome back, wbryanh! You’ve been missed. In this post you wrote basically everything that I wanted to say, so you beat me to it.
Thhq- thanks for posting the links. It’s very interesting to see that refined grain consumption has gone up, more than any other food- (if we can believe the data, which, of course, we’ve talked about the shortcomings). Also fat consumption did go up, according to the graphs. Wbryanh- as you said, a lot of that might be crappy oils used for salad dressing, but some of it might be olive oil- (I wouldn’t put anything else on a salad!) Since there has been so much press in the media about the Mediterranean diet, it could be possible maybe (?) It is irritating that they don’t specify which oils have been used, it sure could tell us something! On the other hand, I’m sure that soy oil consumption has gone way up since the 70’s, especially for those who eat processed food, but even for those who eat bakery breads, pastries, and other treats, even ice cream. I don’t think soy oil was used that much when I was young; now it’s ubiquitous.
Of course, another gripe I have with this data is that I’m not sure how they separate various foods, since many foods consist of more than one element. As a for instance, I have seen people actually insist that sugar consumption has gone down because we buy fewer packages of table sugar than before- (since people don’t bake as much as they used to). But you have to take into consideration every other food that has sugar, and I’m not exactly sure how they do this, or if it’s even accurate. This goes for other food items and macronutrients as well.
Well hello. again. I assumed that both of you would answer the call to defend Good Calories Bad Calories from my mischief. So let’s start with the Mayo group’s statement about NHANES first.
“Given the overwhelming evidence in support of our position, we conclude that M-BM data cannot be used to inform national dietary guidelines and that the continued funding of M-BMs constitutes an unscientific and major misuse of research resources.”
This is unfortunately what Taubes has done. He has used NHANES’ M-BM to inform his own dietary guidelines. The first reference I can find to this is in “The Soft Science of Dietary Fat”:
“Since the early 1970s, for instance, Americans’ average fat intake has dropped from over 40% of total calories to 34%”
Click to access Science-The-soft-science-of-dietary-fat.pdf
Where did that 34% number come from? The numbers in the USDA 1970-2005 dietary assessment show the exact opposite of this (I’ll cite if you like but you can google it up as easily as I can). Their numbers, show that average fat intake had increased from 34% to 40% over the same period. And fat intake continues to increase to 50% of dietary calories in 2010.
http://www.nutritionaction.com/daily/fat-in-food/fats-and-oils-in-the-changing-american-diet/
As I’ve found increasingly typical of Taubes, he didn’t cite his source for the 34% number he causually threw out as fact in the 2001 paper. But he does cite NHANES as the source in GCBC, showing it in graphic form on Page 232:
https://books.google.com/books?id=XPJdM9POXGAC&pg=PA232&lpg=PA232&dq=taubes+nhanes+good+calories&source=bl&ots=kC2SS3S9jA&sig=gYn_34aQBEW2eBp5j1JRU1HtoaQ&hl=en&sa=X&ved=0ahUKEwjPk_-qiI7LAhVD42MKHdWaDPgQ6AEIPjAF#v=onepage&q=taubes%20nhanes%20good%20calories&f=false
And he cites NHANES as if it was a source of irrefutable fact. Read it yourself. Based on NHANES he concludes that the cause of the increase in obesity is either calories or carbs. And further, that because fat consumption according to NHANES has declined from 40% to 34% that fat consumption can be excluded as a cause.
This is not the work of a scientist. It’s not even the work of a competent investigative reporter, which is what Taubes actually is. He’s taken government statistics, which he knew at the time to be suspect, and used them to develop his carb insulin assertion. To be fair, Taubes didn’t know in 2001 that the 2005 USDA report would directly contradict the NHANES macronutrient numbers, nor that in 2013 that University of South Carolina would prove that the entire self-reported NHANES database is fraudulent (based on the self-reported consumption vs actual BMI impossibility). The recent Mayo report shows that the greater medical community is becoming aware of, and accepting, this.
I’ll cite another relevant section from the Mayo report:
“Trends in estimates of macronutrient consumption from population-level epidemiologic surveys (ie, M-BMs) exhibited statistically significant trends that were in opposition to those of USDA economic data for fat, carbohydrates, protein, and energy (ie, kilocalories per day) from the 1960s to the late 1980s. It should be apparent that US residents could not be simultaneously consuming more and less fat, protein, carbohydrates, and energy over time. The contradictory patterns and striking lack of correspondence between the 2 primary US nutrition surveillance tools suggest that 1 or more likely both protocols are invalid.”
So it’s not just me bearing bad news. They’re not saying that the USDA methodology is accurate either. But Taubes has a lot at stake if it is more correct than NHANES, and especially if NHANES is fraudulent. He has everything riding on the NHANES-derived carb insulin hypothesis, and nothing riding on USDA excess dietary fat being the true cause of the obesity crisis.
When I first noticed that 34% number in the 2001 paper, I wondered where it came from. This 2013 article by Colpo might interest you.
http://anthonycolpo.com/why-you-cant-trust-nhanes-or-gary-taubes-robert-lustig-to-accurately-report-calorie-carbohydrate-fat-intake-trends/
Fire away.
@heathertwist the two dried savories seaweed and tuna are used as a topping for the seafood omelet okonomiyaki, along with mayonnaise.
The quahogs I dig – along with the softshells, manilas, varnish clams and Pacific oysters – are not native mollusks. The native littlenecks, gapers and Olympia oysters are out there but much scarcer. So it’s more a Salish reenactment.
Clams are where you find them though, and I eat what I find. The quahog hardshell clams are the same as the ones you get in NYC’s Chelsea Market. The buckets I dig have everything from topneck size (which I eat as steamers) to cherrystones to full sized 4″ quahogs. I steam any of them to get the shells open, using white wine, butter, onions and garlic, and collect all of the liquid. The big tough clams I steam, shuck and mince whole, then refrigerate to use over the next few days. The reserved liquid I reduce, then add cream and some potato starch to thicken, and add chopped clams near the end to avoid overcooking (they’re still chewy no matter what I do). I use this for a white sauce on pasta.
I’m not much on oolican, or hooligan, or more commonly, smelt. They’re fun to net off the banks when they run in the rivers. But then you have to deal with them. They taste best smoked and seem to consist of waxy oil covered with fish skin. I can handle about two of them before my stomach feels like lead, then wonder what I’m going to do with the other two gallons in the bucket. I like pickled herring, but never have developed much taste for smelt.
I didn’t know so many of the shellfish are non-native. That is sad, albeit maybe inevitable (we are turning back into Pangea with all the easy travel). I haven’t tried oolichan but apparently it was THE oil for the natives. Boiled and stored in skins or whatever.
It’s hard to characterize the native diet in terms of macronutrients though. Seafood can be very high in oils, but they are different than the land-based oils and fats. And native foods have carbs, but they sure don’t digest the same as say, a loaf of bread. But probably more attention should be given to the kind of proteins too. Those yummy clams are just way, way different from a beef steak.
I’m glad you save the broth! That’s where the taurine tends to go. Dried fish and squid retains the taurine … on squid, the dried stuff on the outside is the taurine. Likely some other aminos too? Using dried fish, shellfish, and seaweed as a condiment/spice is brilliant … I started using it instead of parmesan and other cheeses, since I don’t get along with dairy much anyway.
That is a big part of the “Mediterranean diet” too. I know the focus has been on the olive oil and wine, but if you actually visit the area, a lot of the local cuisine focuses on stuff like shellfish, fish, and vegies. Only an idiot can starve next to the ocean! The meat and dairy tends to be fermented … sausages and cheeses. When I visited back 50 years ago, “bisteak” was not served much, and it was this tiny piece of beef.
Since the Salish didn’t have cooking pots for about 10,000 years, they weren’t boiling much of anything. The salmon was stored in a certain kind of basket that would hold about 100 pounds of dried fish, and I’d guess that the oolican/smelt was stored the same way. Based on a conversation with my Skokomish barber years ago, I think that a lot of big clams were smoked and dried too (he called smoked horseclams “Indian candy” – IMO probably more like Indian chewing gum). Most of the clams and oysters were fresh steamed under a blanket of seaweed, in a firepit.
Clam juice is hemolymph, not just salt water, and contains nutrients as well as the clammy flavor, so I try not to lose it in cooking. Reducing it with white wine, butter onions and garlic kicks it up a few notches flavor-wise, and the heavy cream mellows it out.
I once looked up a dinner menu Ancel and Margaret Keys ate in Italy late in life. After cocktails, they had bread, wine, fruit, and sauteed vegetables. The main dish was pasta with octopus sauce. When I lived on the French Atlantic coast, you got seafood any way you can imagine. Many of the dishes are rarely seen in the USA. Such as bar (small sea bass) grilled over smoky sarments (grape prunings) at the table. Brandade: reconstituted salt cod whipped up with potatoes and butter, best broiled in the oven with capers on top. Whole scallops right out of the shell. Moules frites were the French equivalent of English fish and chips for comfort food, with a big bowl of the mussels in the shell steamed in a sauce (Provencal was the white wine version, the curry cream was another favorite) next to a big bowl of frites. Soupe de poissons: a rich fish puree the consistency of bisque. I never had bouillabaise while I was there, because the restaurants on the Atlantic coast couldn’t get the proper Mediterranean fish needed to make it.
Nom! Somehow reading that menu, you don’t feel like he’s on a super-low-fat diet! If in fact he was trying to. And that is the thing. A really GOOD meal doesn’t need to look like a Snicker’s bar for fat and carbs. All that umami richness is just incredibly satisfying. And likely means you will eat a whole lot less.But umami is based largely on free amino acids. Drying fish increases the taurine content, and hence the umami.
https://books.google.com/books?id=vXIwSnmjJ4sC&pg=PA45&lpg=PA45&dq=taurine+umami&source=bl&ots=CyKIZM1gje&sig=KJ93EQF8PGbzptELa-5hNgOzpPE&hl=en&sa=X&ved=0ahUKEwjikZeGgpLLAhUT-2MKHUo1CIQQ6AEIRjAJ#v=onepage&q=taurine%20umami&f=false
So all that dried cod in the Mediterranean diet probably counts for a lot.
I wouldn’t rule out soups among the Salish though. Many of the tribal cultures DID make soups, mainly by hanging a skin from a tripod or lining a depression in the ground with one. Or using very, very tightly woven baskets. Or hollowed-out tree trunks. Then tossing in hot rocks to bring it to a boil. That is a surprisingly efficient way to make soup! You kind of wonder if that was the basis for “stone soup”. If you are working with an open fire, it’s a lot easier to deal with hot rocks than with open flame. If you pile hot rocks around, say, some meat wrapped in seaweed, you get cooked meat.
Soups and teas are mentioned a lot in the tribal cuisines of the Northwest.
Here is an old Salish story featuring stew:
https://books.google.com/books?id=kBAeRQKt6xsC&pg=PA135&lpg=PA135&dq=salish+stew&source=bl&ots=3tNj7rtuob&sig=xaIlOnxmcbj8B-vhM52MdSz2sGc&hl=en&sa=X&ved=0ahUKEwj8gc2diZLLAhVL6GMKHYnIDugQ6AEIXjAL#v=onepage&q=salish%20stew&f=false
I guess you are not an anthropology fan. You don’t need a pot (clay or metal) to boil foods. Aceramic peoples all over the world were boiling and steaming their food for tens of thousands of years w/o pots. You can do it is skin pouches (hide, bladder, stomach, etc.), in a wrap of leaves, in baskets or dug-out wooden bowls, in a pit, or in a depression in rock. Unlike frying, where you need higher temps (that might destroy your cooking vessel) and a goodly amount of oil, boiling/steaming only requires that you get the temp to 212 F (100 C) and use water or the natural juices of whatever you are going to cook. For a modern take on camp cooking w/o pots, see http://www.eattheweeds.com/mesolithic-cooking-it%E2%80%99s-the-pits-2/.
No, I’m not an anthropogist like Boas, and I should be reading more of this. But I’m not a tourist either, having lived 50 years of my life in Salish-land. My interest in clam-digging and oyster-picking is partly as a participant.
One of my favorite places to dig clams is Potlatch WA. It’s on the sunny reach at the bottom of Hood Canal. Wide open and warm, with lots of clams and oysters, and salmon running in the Skokomish River. The perfect place to hold a traditional Salish potlatch. Here’s a description of the kind of feasting that took place:
“Food at a potlatch must be abundant. Ideally the guests should not be able to finish what is served but should take the surplus home. “Traditional” foods are served, though what is traditional has been modified over time as introduced foods have become standard in the community. Salmon, dried for winter use, has been the prized and usually abundant principal food. Other dishes include berries, seaweed, and meat of mountain goats, elk, moose, bears, seals, small mammals, and halibut, all smoked or dried. Traditionally eulachon, a smelt abundant in early spring, were caught in large quantities and processed into a rich oil used as a sauce at every meal. Potlatches were noteworthy for the lavish outpouring of eulachon “grease,” to the point of ladling gallons into hearth fires until the flames roared to the roof. A description of Tsimshian feasts notes, “The foods that were most valued were those that were scarce, available only seasonally, required intensive labor (and entailed organization by a person of rank), ‘imported items’ (including European foods as they became available), grease, and anything preserved in grease” (Halpin and Seguin, 1990, p. 271).”
http://www.encyclopedia.com/topic/potlatch.aspx
Notice the importance of smoked and dried foods. Certainly there was some boiling of foods, but it was the exception rather than the rule. If you look at the cooking baskets they had (at the Burke), they don’t hold much, and rocks don’t stay hot for all that long. I think the reason that other basket types survived better is that cooking baskets are greasy, dirty, and unsanitary.
I’ve never done a proper pit smoke/roast. I use a 55 gallon drum with a fire basket in the bottom, which will burn for about 2 hours with the lid on, if loaded with a dense hardwood like white oak or apple. Temperature control is iffy (250-400F), and I end up with relatively dry meat which has lost almost all its fat into the fire below the racks. The flavor is so strongly smoky as to be peppery. No one likes to be around when I’m doing it…smoke can be fragrant in small amounts, but this is not a small amount of smoke…
“Notice the importance of smoked and dried foods. Certainly there was some boiling of foods, but it was the exception rather than the rule. ”
Yes, one of the things I’ve noticed in my forays into “ethnic eating” is that seafood-based cultures tend to do a whole lot less cooking … even if they have modern cooking equipment. In the Asian stores, there are whole sections of dried fish and shellfish. The dried fish has more umami than fresh fish, and so is used as a seasoning too. Dried bonito and dried kelp are THE main seasoning in Japanese soups. Fresh fish is more likely to be eaten raw, or very lightly cooked on a grill. Or in the Northwest, lashed to a board and stuck in the ground near the fire to smoke/cook.
Here is the thing though. It is commonly said that “modern civilization” started with growing grains. The logic is that grains can be stored and carried by an army, and therefore the army can eat on the march. Grains can be hoarded and taxed, and so kings and armies arise. It does in fact seem that the grain-eaters have done most of the invading and castle-building during history.
Problem with this logic I think though, is that dried fish and dried vegetables keep even better and are more nutritious grains! And they are lighter to carry. And you can live off fish and vegies, but a diet of all grains just isn’t complete. The Chinese railroad workers in the US were basically like an army, living in tents and on the road. They were noted for being healthier than the Irish railway workers, also imported for the task, who ate salted meat and bread/potatoes.
And the Chinese’s main food was dried oysters and dried vegetables, along with rice. Rice is a grain, but it’s also often just picked wild, and was eaten for a rather long time before “civilization”. Anyway, I’ve kept dried fish and vegies and rice in my food pantry for YEARS and they keep just fine. They don’t seem to go rancid either, even though fish oil alone is often noted for going rancid (oolichan grease appears to be an exception).
So one wonders why the Salish lived (apparently contentedly) with their dried stores and didn’t become like, say, the Maya with their temples or the Plains Indians with their raids. The Salish didn’t appear to have an issue with over-population either, even though they had plentiful food that was pretty easy to get. Further south, people lived off corn, and they DID get over-populated which seems to be what triggered some of the wars.
I’ve done my share of shoreline food-gathering, and it’s always amazed me at how easy it is … even on the over-populated dried-out coast of Los Angeles … to get a day’s worth of food. In the Northwest, there are huge patches of arrowroot in lakes, which can be easily gathered with one’s toes, so one could have “potatoes” with your fish! Lots of camas root too, and mushrooms.
The smoke probably preserved the Salish fish oil. I don’t know how they got the oil out of the fish and into storage containers (probably something like the cooking baskets), but someone like Eells or Boas might have that documented. I’ve read that oil from salmon was more highly regarded and used for perfume. Attar of Chinook #5.
California seafood. I’ve seen mossy looking crabs line-fished off the Manhattan pier, and always wondered about those Pismo clams, but most of my LA seafood experiences have been in Japantown eating sushi and sashimi. I’ve spent more time around Monterey eating local sanddabs and calamari. Some of the best I’ve ever had was at the little Monterey Fish House on the north side of town, far away from the tourist zone. Sicilian-style, in a rich red sauce, perfect for sopping up with local sourdough bread. Better than anything in San Francisco.
“Attar of Chinook #5.”
In the Asian stores, they sell something called “salmon bellies”, which are the bottom part of the salmon including the fins. I fry them up, coated in potato flour, to make a kind of fishy chichirone. The fins get crispy when fried. Actually the bones can get crispy too: the Japanese make them into “bone crackers”.
But you inspired me … what about taking those bellies and cooking them down slowly, extracting the oil? Salmon bellies are cheap, and mostly consist of salmon oil. Looks like the Salish extracted their oil by leaving the salmon in a wooden trough, out in the sun. As the fish decomposed, the oil ran out. So uh, yeah, it would be nice and “perfumy”!
https://books.google.com/books?id=fudyXm4KMpQC&pg=PA153&lpg=PA153&dq=salish+wooden+jar&source=bl&ots=m1LVaGJcZg&sig=yTUm-XfsYrZIH36zg6UYk7pr1Rw&hl=en&sa=X&ved=0ahUKEwjEsra9kpbLAhVBGGMKHcbgATQ4FBDoAQhkMA4#v=onepage&q=salish%20wooden%20jar&f=false
Looks like the natives stored the oil in things like seal bladders and kelp bladders. Stomachs were used for storage too, and the Inuit used whole seal skins (pull off the skin in one piece). That’s pretty much how sausage is made too … stuff the intestines with chopped meat, then hang it over a smoky fire. The meat ferments and you get … pepperoni!
But the Northwest folks were also excellent canoe-makers, and they made mini-canoes for stuff like gathering Wapatos. Absolutely waterproof. Here is a description of cooking in a log:
“Boiling is performed in a wooden Trough like an oblong box, by putting red hot stones into the liquor, a heap of which always compose the fire hearth, they put them in and out of the pot with a kind of wooden tongs. In this manner they boil all kinds of meat and make Soups, which even a European would relish …”
https://books.google.com/books?id=d2YRQYdQlT4C&pg=PA199&lpg=PA199&dq=salish+wooden+trough+cooking&source=bl&ots=O6PefqegqX&sig=uHpgiRmTSVdtbtH9wBnYLShEIN0&hl=en&sa=X&ved=0ahUKEwjE6uaqk5bLAhUM4mMKHdgJDVkQ6AEIHTAA#v=onepage&q=salish%20wooden%20trough%20cooking&f=false
I think much of their cooking was communal, so the fact it took a lot of work to make a big mess of food for dinner probably wasn’t a huge deal. They spit-roasted venison too, which takes a long time!
I used to cook with stones myself. I had a “cooking box” which was insulated (straw was used in the past, but mine was styrofoam I think). You put the heated stone in the bottom of the box, and place the container above it, and seal it up for the next 4 hours or so while it cooks slowly. I heated the stone on my stove and didn’t drop it IN the soup, but same idea. It works really well, and you don’t have to worry about burning the soup. Actually using a wooden trough would be very efficient: wood is a good insulator, and cedar would add a nice flavor to the soup. If the log is used often, it wouldn’t get moldy either.
They still make those long cedar log canoes, but now they stick big outboard motors on them. You can watch the Quinault tribe’s races at Taholah WA on the 4th of July every year while you eat your salmon and fry bread.
I’ve never collected wapatos or skunk cabbage roots (related to taro). I’ve dug the edible camas/fawn lilies (erythroneums)/rice roots (fritillaries), but only to plant in the garden for the flowers. The Lewisias are even more beautiful edibles – bitterroot is Idaho’s state flower – but harder to transplant. A lot of these wikld starches have oxalic acids or tannins that need to be soaked out. I tried soaking out white oak acorns once but never could make them edible despite many water changes.
I mostly render fat from ducks, roasting the raw meat stripped carcasses and skin in the oven at 400 F. You could probably render salmon bellies the same way, or just grill the fish in a pan with the skin on and collect the oil. Salmon doesn’t have as high a % oil as smelt (or ducks) though, and your yield is going to be pretty low. The redder the salmon meat the more oil it contains, and the pinks contain virtually no oil. It’s the high oil content that makes sockeye and chinook so tender and tasty.
This is what a Salish cooking basket typically looks like, though this one might have been for dry storage. Most baskets were made for collecting and storage rather than cooking. But coil baskets like this one can be made tight enough to hold water.
https://bcartifacts.com/shop/swsb101304-round-1890s-spruce-root-and-cedar-basket/
Gee, all this talk about food is making me hungry……
My reply showed up in the wrong place; the comment had to do with reading about the foods served at the potlach; sounded delicious!
Brilliant article, Denise. Hopefully in Part II you focus on the calculation that an all rice diet would have likely provided a lot of resistant starch. High white rice diets are probably just reproductions of the potato hack. If you’re eating rice all day, you don’t make a batch for each meal. You make a batch and you put it in the fridge and then you get a high RS diet…
According to Tim Steele’s RS FAQ:
So, an all rice diet, particularly if cooked/cooled, can be very high in RS3.
Even though there is hardly any amylose in freshly cooked rice, up to 10% of glycemic starch is believed to pass undigested to the colon and becomes RS—likely making these rice diets a high RS diet even without cooking/cooling.
The fact that you still poop when eating nothing but rice is proof that undigested starch is making its way to the colon.
It’s unlikely to be a coincidence that virtually all of the health benefits of these high rice diets mimic the exact same documented effects of increased RS intake.
Cheers and job well done!
Whenever Part 2 comes around, I’d be curious to get your take on Ray Cronise’s “Metabolic Winter”
http://online.liebertpub.com/doi/pdf/10.1089/met.2014.0027
He does his own, Joel Furhman-esque critique of the food pyramid, and instead suggest a food triangle.
Great post! I follow Swank’s Multiple Sclerosis diet, and have remained healthy and active!
Denise I like your cute style of writing. You’re like that 6th grade science teacher that tries to make science fun! But I think you went too far with that style of writing in this blog posting where it distracted from the content of your analysis and findings which was very compelling.
More re HDL quality:
http://www.sciencemag.org/news/2016/03/why-high-good-cholesterol-can-be-bad-news?utm_source=sciencemagazine&utm_medium=facebook-text&utm_campaign=goodbad-2900
Where is the second post????
I absolutely love that you added Rainbow Dash to the magic picture haha! Definitely made me smile. Thanks! 🙂
As someone who is on a plant-based diet, I love that you became more objective and “exposed” your previous biases (or at least some of them). I link people who are not sold on it here so that they can work through their own biases. I think it’s extremely helpful. But I’m a bit disappointed by passages like this one:
“For sure, there’s still plenty of stuff we could nitpick about this study (and his previous ones): there was no control group; the patients were abnormally motivated and self-selected (rather than reflective of the general heart-disease population, who might not be so inclined to give up steak forever)”
I think that the first nitpick that there’s no control group is kind of pointless, since we got to see exactly what happened when people strayed from the program. It sorts of act like a control group, doesn’t it?
Secondly, I fail to see what your second point has to do with the study itself. It’s really out of place and below your standards. Are we not studying the benefits of a low fat, whole foods plant-based diet and its relation to heart disease? What does it matter if a person is motivated or not? We wanted people to follow the diet so that we know if the diet works. The “general heart-disease population” won’t help us do that if they are more interested in dying than in eliminating meat – at last temporarily – to conduct an experiment. So why should we care about them for this study exactly, and how is this study hurt by not using them?
There’s this patronizing attitude among M.Ds. which has them assume that people won’t change their habits and they’re just wrong. Data shows that meat consumption has been dropping significantly in the US since 2011. There’s plenty of people who do not feel deprived by not eating steak anymore. We should never make statements like this that hint at the difficulty of giving up foods that cause diseases: people should be shown the evidence and make their own choices.
As someone who is on a plant-based diet, I love that you became more objective and “exposed” your previous biases (or at least some of them). I link people who are not sold on it here so that they can work through their own biases. I think it’s extremely helpful. But I’m a bit disappointed by passages like this one:
“For sure, there’s still plenty of stuff we could nitpick about this study (and his previous ones): there was no control group; the patients were abnormally motivated and self-selected (rather than reflective of the general heart-disease population, who might not be so inclined to give up steak forever)”
I think that the first nitpick that there’s no control group is kind of pointless, since we got to see exactly what happened when people strayed from the program. It sorts of act like a control group, doesn’t it?
Secondly, I fail to see what your second point has to do with the study itself. It’s really out of place and below your standards. Are we not studying the benefits of a low fat, whole foods plant-based diet and its relation to heart disease? What does it matter if a person is motivated or not? We wanted people to follow the diet so that we know if the diet works. The “general heart-disease population” won’t help us do that if they are more interested in dying than in eliminating meat – at last temporarily – to conduct an experiment.
And If you think you have a better diet that can reverse heart disease and is easier to follow, that’s great, but you don’t have to patronize people who do not feel deprived by not eating steak anymore. There’s plenty of them out there. People should be shown the evidence and make their own choices.
Also, the following comment about it having a “self-fulfilling prophecy” aspect rubs me the wrong way as well. Are we supposed to believe that if people were convinced that a diet of Twinkies and Jello could cure them of heart disease, that it would actually happen? I mean, if it did, holy crap, we’d have to re-engineer all of our drugs to be harmless placebos and work with hypnotherapists instead. But we all know that a strong belief isn’t going to reverse heart-disease, on any significant level. Denise, please!
When I was fed a high fat diet (Japanese eat lots of Animal products) I gained weight from 65 to 74KG. Then I felt like humans are not designed to eat fatty foods (because most other mammals eat mostly vegetarian with little protein from insects). I did notice that omnivorous animals preferred meat or fat, only during seasons plant based food was scarce. I became a fruitarian with inclusion of fish, and then became 62KG. My skin, hair, everything was shiny, flawless. Then became fruitarian and ate tons of fruit every day, to fulfill protein, became 56kg. Then continued to eat walnuts and peanuts, 1kg every day. I gained 2 kg of weight after 2 months. I noticed something peculiar. The body seems to prefer carbs for energy, and in current culture there’s no way fat will be used, and thought, you can focus on fat only and not gain weight, same for carbs. But mix those two and you get disease. I think vegetable oils, meat will destroy humanity. The human natural diet is vegetarian, with small fish, raw beans, nuts in the winter (parasites also dislike cold) and autumn, for spring and summer fruit, herbs. Year around vegetables and mushrooms. Sweet potato and cold stimulate adiponectin? Improving insulin response.
Any idea on when Part 2 will be posted?
Well done Denise – very interesting article which made me rethink what little I thought I already knew about diets and their effect on health. To be honest, I can’t see myself switching to an ultra low fat diet (unless perhaps I got MS), but a lot of people should not be shooting the messenger, but congratulating her on widening people’s knowledge. I wonder if NuSi would consider commissioning some studies on these sort of diets?
I asked Ray Peat about Swank’s diet and why he thinks it works, and he replied: “I think the cod liver oil and low iron (red meat) intake were helpful.”
After reading through your comments again, I see that Swank mentions meat reduction as a form of saturated fat reduction: “In recent years, this experience induced us to eliminate all meats and other sources of fat from the diet of many patients when first seen. “
So there you go, another hypothesis to consider! There’s always so many variables involved in each diet that it’s hard to say what does what, but good luck with your endeavours regardless. 🙂
Hi Denise, what you suggesting seems to tie in with what Dr Lustig says in his anti-sugar book, “Fat Chance”, namely that we evolved to eat mainly carbs (with loads of fibre) or mainly fat (meat, fish, coconuts etc) but not both together. He says that the liver has 2 pop-off valves (whatever they are!) one for carb (glucose) metabolism and one for fats. Of course this doesn’t seem to explain Dr Kempner’s success with diets including large amounts of sugar, but it does at least seems to agree with you that there are 2 ways of eating healthily.
What if the low-enough/high-enough fat threshold is yet another artifact of health-focused lifestyles?
I mean that the only people likely to be able and willing to maintain that low or that high a fat consumption in a cosmopolitan setting are also very likely to be health-conscious overall (exercise, no smoking, etc.). Conversely, those who cannot maintain such fat percentages in their diet are not only likely to be less careful eaters but less careful live-ers.
And for trial participants, were the control diets as strict and as demanding as the trial diets? Were the folks who abandoned the diets also sloppier about their eating habits and health overall?
I apologize for not scouring the 1500+ previous comments to see if anyone had discussed this.
I’m new to your blog, Denise, and finding much nourishment here. It’s rare and heartening to encounter a true skeptic, not to mention one with the analyitical skills, doggedness and humility required to walk the walk.
Bravo!
Just pointing out that 37% of the participants in the rice diet did not improve, or worsened.
I am sure I would be in that group, since I respond so spectacularly well to low carb. Lost weight, lowered A1C & blood pressure, and when I tried gluten free, my arthritis went from “waking me up in the night” to “almost vanished.”
I loved “Death by Food Pyramid” and was especially struck by the enzyme patterns described in the book. Food is truly not one size fits all, and we should be encouraging people to try new things.
Anything but the Standard American Diet. I think that has been shown to be bad for everyone.
Did you ever write a part 2?
“I think that the first nitpick that there’s no control group is kind of pointless, since we got to see exactly what happened when people strayed from the program. It sorts of act like a control group, doesn’t it?
Self-selected groups are pretty much the opposite of control groups. Ideally, you want your subject and control groups to reflect the general population, or, failing that, at least be as similar as possible. Letting people sort themselves out according to personal preference about what you’re trying to test for would in most cases guarantee that the groups aren’t similar and more or less nullify the value of the assay.
“…What does it matter if a person is motivated or not? We wanted people to follow the diet so that we know if the diet works.”
The problem with health-motivated nutrition subjects is that they are far more likely to be health-motivated in other aspects of their lives (exercise, furnishings, sleep, stress management, etc.), which will obscure the effect of diet alone on health. As the less disciplined drop out, your sample group now skews to the most motivated and disciplined members of the population. See the problem? Now it’s as difficult as possible to isolate the effect of diet. Denise has gone into this phenomenon in more detail elsewhere.
As to your conclusions about meat consumption, you can’t assume from the simple fact that a population is buying less meat that they are eating healthier, or even that they’re buying less by choice, informed or otherwise. Given that cheaper (and not necessarily better) foods are readily available, and that the majority of Americans have been getting poorer for some time, you’d need a lot more evidence to suggest that the drop in meat buying is caused by anything other than economics, or that the result is a healthier diet.
There is overwhelming evidence that changing habits is difficult. Pretending otherwise won’t help those who need to change their habits or those who try to help them.
robert e, these are all good points. Another confounder with a self-selected, highly-motivated group is the extent to which results may be due to the placebo effect, rather than the actual effectiveness of the diet. The test group really wanted this to work, so it did.
Is there Part 2?
Fabulous post, but alas, so CONFUSED now. I just want to know what to eat. I’m not so fond of the no-fat, or the all-fat. But the “swampy middle” doesn’t exactly seem promising. I’m also responsible for feeding my fellas, who tend to mutiny under, um, extreme circumstances. Sigh.
Denise, are you going to be writing a Part 2 on this? I loved this first part.
I find the discussion here very interesting.
I eat a low fat, fruit and plant-based diet with the occasional oysters, clams, mussels and the like, as well as insects which is mostly for entertainment value. I’ll eat other things if I’m interested in it, but it doesn’t happen really that often. I wake up and run five miles every morning, and will eat if I’m feeling hungry but this ends up being much less common than most people (who try to make me eat more).
I haven’t been sick in 3 years (I began this sorta thing at 14) , although I got a very bad whiplash injury a year back that gave me a severe TBI, and I was told that my life would probably never be the same and that I’d need drugs to “dull the effects” of the pain from nerve damage. My relatives got very concerned and tried to force me to eat, but, I wasn’t very hungry, so I just drank water for six days and my symptoms completely disappeared and I was able to get back to everything I’d done before, though it was cautious and incremental.
I’ve tried a high-fat diet to see the effects, and ketosis can be very powerful and almost a sort of “high” for me. However, it’s always felt like I’ve been manipulating my body, which I listen to very closely, and not really a sustainable thing over the long term.
Thanks for the great article Denise,
P.s. Are you still doing consulting? I’m interested. Also, I gave “Death by food pyramid” to all my relatives for Christmas 🙂 The title (and the content) is fantastic
Maybe what I’m going to mention has been discussed in the comments above, but there are just too many of them for me to wade through. If anybody is still reading these comments, including Denise, I hope someone will comment on the question that kept returning to me as I read this fascinating post.
The results Denise describes are indeed impressive, for instance with respect to MS. But Terry Wahls has also had impressive results with a very different approach. How can this be? The evidence presented in the studies here is irrefutable, but what’s the significance, when other approaches also work?
What is the hypothesized (or proven) mechanism of action for WHY people who eat rice and sugar cubes are healed of obesity, diabetes and heart disease? And how to explain the fact that many people have had phenomenal results treating the same issues through a Paleo approach instead?
Individual genetics? Is the concept of “essential nutrients” off the mark? Maybe for some people, fat is essential, for others, carbohydrate is? A particular cohort of sick people who all share the same symptoms need a certain diet, while a different cohort needs a different one. Is that where this research is heading?
I cannot tell you how thankful I am to have found this article. You kept apologizing for the length of the article but I found it hilarious and fascinatingly informative at the same time. Thank you so much for putting the time and effort in to put together something like this for those of us who have almost given up on figuring what what the hell is true or not in the nutrition world. There is so much conflicting (mis?)information out there that the more you learn the more it seems you don’t know. The rabbit hole is deep! I had begun to implicate fat intake with my insulin resistance but was sure I had to be wrong because everything I read and my own dr assured me that no it was the carbs that were the cillan and as long as I put down the beans and brown rice and picked up the bacon I would be on my way to good health. I truly believe that is wrong from personal experience. I learned so much in this article! There is so much misinformation regarding these people like pritikin!
Denise: Just a note on the “rice diet.” “The Salt Fix” talks about this and makes it appear (to me anyway) like a bunch of pseudo-scientific hooey.
You kick ass! Thank you for YOU!
I enjoyed reading that but was it a blog post or a book?
…and on that note, was that part 1 or volume 1?
Perhaps insulin sensitivity was not improved on ALL in the study because they had stored pufas that were being released as they lost weight…im curious to see the percentage of improved insulin sensitivity on those that lost no weight
Denise,
Thank you for an extraordinary article – which seems to turn much of what I learned from Dr Kendrick’s blog on its head – although you still seem to come out against the typical low fat Western diet.
I wonder if either the LCHF or the HCLF camp (or both?) might be observing a really powerful placebo effect. I mean, no diet can be blinded, and if a simple sugar pill can have appreciable power to heal, then perhaps an extremely intrusive diet of either type can trigger a more intensive response.
I can’t wait for part 2!
I loved this blog post! Is there a Part 2?
I read this entire page and loved all this fantastic information. I did Atkins and paleo for abt 5 yrs total years and 3 years ago quit to do a Matt Stone rest and refeed because I just could not do it any longer. Recently I came acrocc Kempner’s rice diet, McDougall and now your lovely looong post. I will never be vegan and probably never vegetarian but will be following low of a very low fat high starch approach now that I realize I am starting to feel better on it and that even moderate fat always makes me feel like I am never digesting my meals.
I’m sure you’ll never read this, but I just wanted to thank you for changing my mind about fat. I’ve been buying into the healthy fats propaganda for almost a decade, and while I think it can be good for some, it’s clearly not the best thing for my body. The worst blood sugar readings I ever had were on a low carb diet (my fasting glucose was always in the mid to high 90’s no matter how low I took my carbs). I ate low-carb paleo for almost two years, and while I did lose weight and get off my meds, my body was falling apart and I could not get my blood sugar to go down (and I couldn’t sleep, and I became agoraphobic, had internal bleeding, couldn’t think straight—yeah, LC was pretty destructive for me). I decided to go off the diet and just eat real food, but I could never drop the “good fat” mentality. As soon as I finished your article, I cut out all the extra fat I was eating, which really wasn’t hard, and within days my fasting blood sugar went down into the mid to low 80’s, where it has stayed as long as I keep the fat at about 10-12% (not counting the few times I tried to add in a supplement that made it go up). I’ve lost over 20 lbs and am now the lowest weight I’ve ever been in my adult life (126), and amazingly that happened without me even trying. I don’t count calories or fat grams or anything; I just eat healthy food and make sure I pick low-fat protein (except in the morning when I often eat fatty fish) and it all just falls into place. So thank you again for presenting this in such a logical way, and I am looking forward to part two whenever you get it up ❤
Great post. I am sorry I’ve only found it now. I recently came to a somewhat similar conclusion myself recently when I took on 14 day raw vegan diet challenge.
Being a 14 year low carb veteran I was not expecting the results I got. It causes me to look deeper.
While I still prefer my low carb life I now know that carbs don’t make you fat. Too much fat combined with too much fat make you fat.
Your chart on the magic points is right on the money as far as weight loss goes. I thought I was the only low carb advocate to see this. I guess you beat me. 🙂
That being said, I still wouldn’t say gorging in white flour and sugar are a great plan especially after reading the work of Weston A. Price. Physical degeneration linked with addition of sugar, white flour and sweetened jams alone was real and significant.
I wonder if the “squirrel” hypothesis written about here is at all relevant to the research and evidence that you have examined here, and of your working hypothesis. https://www.donteatforwinter.com/striking-similarity-signature-junk-food-autumnal-produce/
The blog’s fascinating finding is that the only two natural foods that have similar macronutrient profiles (high in BOTH fat and carb) to pretty much all modern industrial “junk food” are breastmilk (for infants who must gain weight to be healthy) and acorns (eaten only in autumn, by animals fattening up for winter). Isn’t that interesting? And a reason to reflect upon “autumn” style foods (which mix high fat ratios with high carb ratios) being consumed all year round, and the likely consequences…
Check out “The Starch Solution” by Dr. John McDougall.
Great post, part 2 still in the writing? somewhere in the next decade?
Just re-read this post for the millionth time. Fascinating stuff. Is part 2 on its way? I’ve been anxiously awaiting the sequel.
I wouldn’t hold my breath. Considering Denise hasn’t touched this web site in forever and she has disappeared from Youtube I don’t hold out much hope we’ll see part 2 or for that matter anything else from her. It could be that by publishing part one she has lost her following in the Primal/Ancestral group and the vegans have always hated her since she published he thoughts on the China Study. No one is interested in the truth. They just want confirmation of their own current program.
How sad. Pity because she was gaining a lot of genuine interest from people who have had enough of the radicals.
Part 2??? Please!!
Where i can find part 2?
Part 2 ?
I could follow your research and opinions blindly to the end of civilization. Love the verbiage, expressions, and laugh-out-loud punnines!
Research-honest
Relatability- top notch
Thanks for your passion, humility, and just existing!
I’ve been following the dietary debate in recent years. I thought it was already well understood and agreed upon that both low-carb/high-fat and high-carb/low-fat would allow fat loss or maintenance and affect metabolic health.
The greater point is about long-term health. There are essential fatty acids, but there are not essential carbohydrates. The body needs some glucose, of course, though it can get this from protein by way of gluconeogenesis.
The other thing is that the fat-soluble vitamins are essential to health. Although one could supplement these nutrients, one would still need adequate fat to go with them for the body to be able to use them.
One can entirely eliminate all starchy and sugary foods while remaining healthy. One could not do that in entirely eliminating fat and fat-soluble vitamins. That is to say a low-fat diet would still require adequate fat and fat-soluble vitamins. There is no such thing as too low-carb, even as there clearly is the problem of too low-fat.
That is what would be seen in the evidence. Low-fat diets are still including fat. There is no low-fat diet equivalent of a fatty carnivore diet where nearly all carbs are removed. So, it’s not exactly a good comparison.
This has not been my personal experience. For me, there is such a thing as too low carb, and I cannot eliminate all starchy/sugary foods and remain healthy. My body needs higher amounts of carbs to function optimally. I cannot possibly eat enough carbs if I don’t eat starches and some simple sugars (like maple syrup). Eating lchf left me with adrenal problems that almost hospitalized me. I had internal bleeding, blood sugar problems, hormonal imbalances, and, emotionally, I was completely debilitated. While a person’s body CAN make glucose through gluconeogenesis, it’s incredibly stressful for the body, going hand in hand with massive amounts of adrenaline production. If the body can’t keep up, it starts breaking itself down, eventually shutting down. Maybe YOU can eliminate all carbs from your diet and thrive, but I, and many others, cannot.
As for fat soluble vitamins, low fat has been shown to make nutrients more absorbable. (And no one is advocating no-fat, so that’s a moot argument.) Depending on the person, you only need about 5-15g of fat per meal to maximize nutrient absorption. While 15g at three meals a day would put a person over the strictest hclf recommendations, it’s still relatively low. It should be noted that nutrient absorption has been shown to decrease when eaten with high fat (over 35g) meals.
If lchf works for you, that’s great, but it doesn’t work for everyone. My health went downhill on lchf, but it improved drastically when I switched to hclf. I don’t like to speak in absolutes anymore. Different bodies require different amounts of macro and micronutrients. (And maybe different amounts at different times.) I encourage everyone to find what works for them.
This is the first time I’ve looked at this for 5 years. I still eat anything I feel like but count calories eating and exercising as I have been for 15 years. I have gained back 20 lbs of weight, but a lot of it was lost muscle from my initial crash 50 lb loss in 2007. I still like low carb as a diet strategy for fast weight loss, but it’s hard to stay on for 15 years, and not necessary after it has accomplished the purpose of weight loss, Yudkin style.
And with Yudkin and Keyes I agree wholeheartedly that it’s all about calories in and calories out being in balance. The macros are secondary, and there are better and worse foods to eat (aka Guyenet’s rewarding foods), but the important thing is not overeating for what you do in a day or you’ll get fat.
One problem is that few of us grew up on a healthy low-carb diet. So, most of us have already experienced decades of severe harm to our health from excess carbs. To what extent we can reverse metabolic syndrome and other health problems will vary to a great degree.
The challenge is that reversing what caused the problem won’t necessarily resolve the problem. Even if a low-carb diet might work well for most people if they grew up with it, the state of ill health caused by a lifetime of a high-carb diet might permanently alter what the body can handle.
Still, the point remains there is no such thing as an essential carbohydrate, as there are essential fatty acids and essential fat-soluble vitamins. No matter how many carbs you choose to eat or not to eat, the fact is that you could not survive without sufficient levels of fats and fat-soluble vitamins.
After 7 years, the same old nonsense about good food bad food continues.
Every food is essential if you need the calories. No one starves themself if they don’t have a stick of butter to eat. Ill health comes mainly from eating too much or too little of ANY food, not macronutrient ratios.
There is no point in glorifying potato chips, which is essentially what you are doing. You can survive quite nicely eating foods that are not composed of 50% fat like potato chips are. Keyes’ SAD diet is 15% protein, 35% fat, 50% carbs. You could get by with less fat than that and still have all you need. 10% fat would be plenty. There is nothing inherently good about eating fats beyond that, unless they supply calories that you need to survive.
I wrote another comment with a couple of links, but it disappeared after hitting post. Hopefully, it’s in moderation and Denise Minger will approve it. I’ll check back later to see if it reappears. For now, let me add another thought.
Macronutrient ratios matter for many reasons. For example, it is central to metabolic health. The body simply can only handle limited amounts of carbs. It’s similar with protein. Higher levels of animal fats, however, appears to have no known negative health effect. In fact, where fat is stored in animals tends to also be where micronutrients are stored. So, the issue of macronutrients and micronutrients is inseparable.
Macronutrient profiles also matter in other ways. Consider that carbs are the single greatest activator of mTOR. That is good for growth and is within evolutionary norms when carbs are eaten seasonally, but continuous high-carb consumption shortens lifespan. Yet some blame protein for mTOR upregulation. That is only true on a high-carb diet, though. As research shows, amino acids by themselves only elicit a small and short term mTOR uptick.
It’s a matter of degree David. 10% of total daily calories is SUFFICIENT to satisfy a person’s need for fat. The rest of the calories can be anything else, but a minimum of 15% protein would be desirable.
In Paleo times fat was very desirable but it was not available in any quantity. Open hearth cooking incinerates fat, resulting in a high protein diet which contains scant fat and carbs. But we survived on it. Probably 30% carb, 10% fat, 60% protein. Most of the carbs and fat came from nuts and fruit.
10% of fat as part of total daily calories on SAD is vastly greater than 10% of OMAD and calorie-restriction. In fact, 10% of former might be an even larger total fat intake than 30% of the latter. That is not a useful metric. The less one eats and the less often one eats the greater percentage of fat one will need to fulfill the body’s requirements of essential fatty acids and essential fat-soluble vitamins.
About the Paleolithic period, fat was both desirable and highly available, until the megafauna die-off. The megafauna were as blubbery as whales. And, as for food preparation, traditional people don’t generally overcook their meat as we do now because of our fears of microbes and parasites. Also, all of the excess fat was added to things like pemmican to be stored for later use and did not require cooking. Also, meat was often eaten raw, specifically as allowed to partly rot (i.e., high meat).
I am a late comer, but rediscovering what I once knew (low-fat is good) is such a relief. Of course! Humans didn’t evolve in the fat swampland, and people nowadays want to believe high fat is good because they like the taste of it and they don’t want to give it up. Bioindividualiity might account for a tiny percentage of the differences between people, but if you want to know how far from everyone else’s genetics you stray try eating a high fat diet for a while then get your cholesterol levels checked….good luck with that. Denise….i am so grateful to you. Gin Stephens mentioned you on a pod cast and it stirred up some interest. I’m going to jump in to find out about all your stuff. I want to know where I can donate. Thank you! You Rock!